Tribomechanical Comparison between PVA Hydrogels Obtained Using Different Processing Conditions and Human Cartilage
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Materials Preparation
Hydrogels
Human Cartilage
2.2.2. Materials Characterization
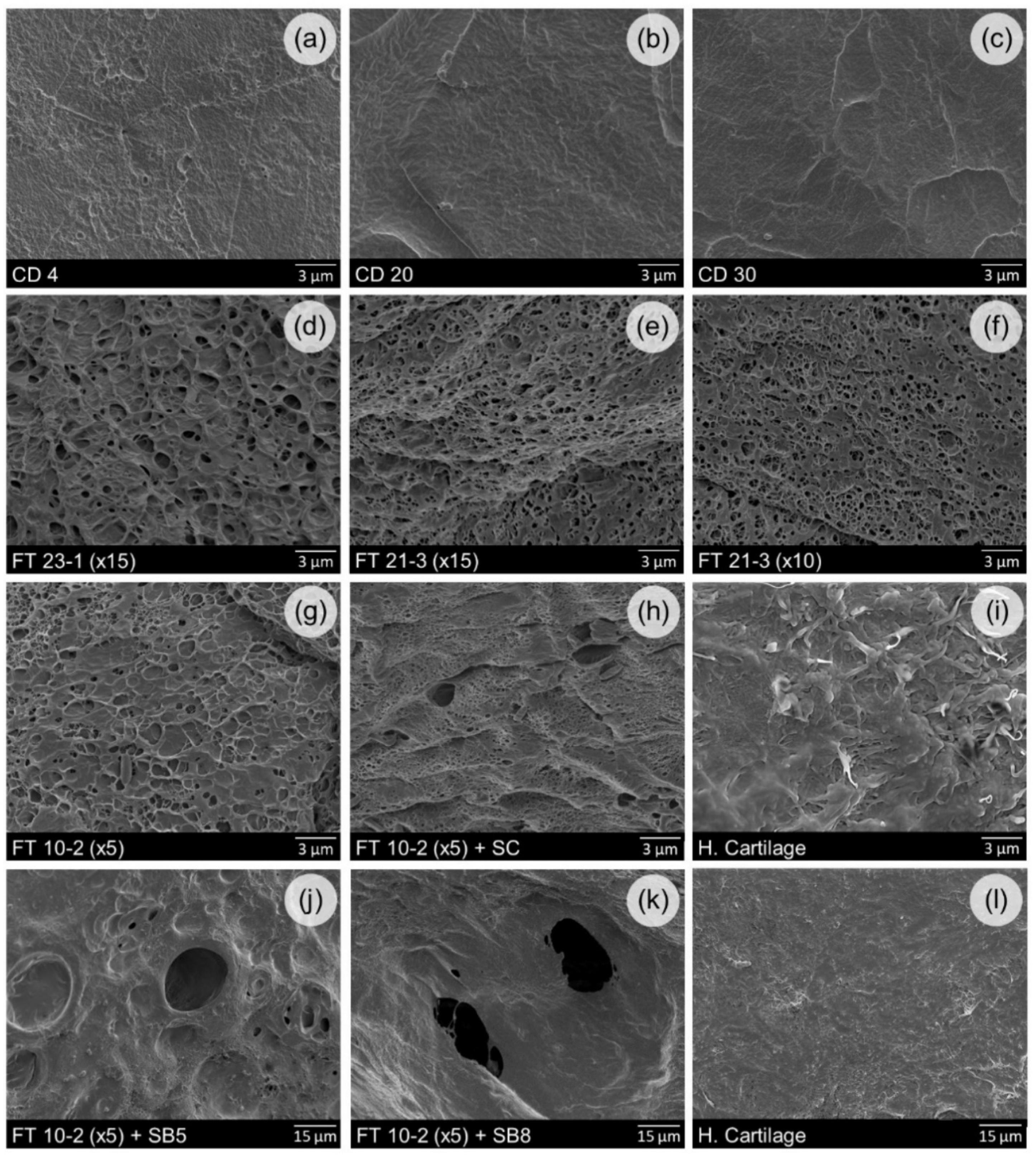
Surface Morphology
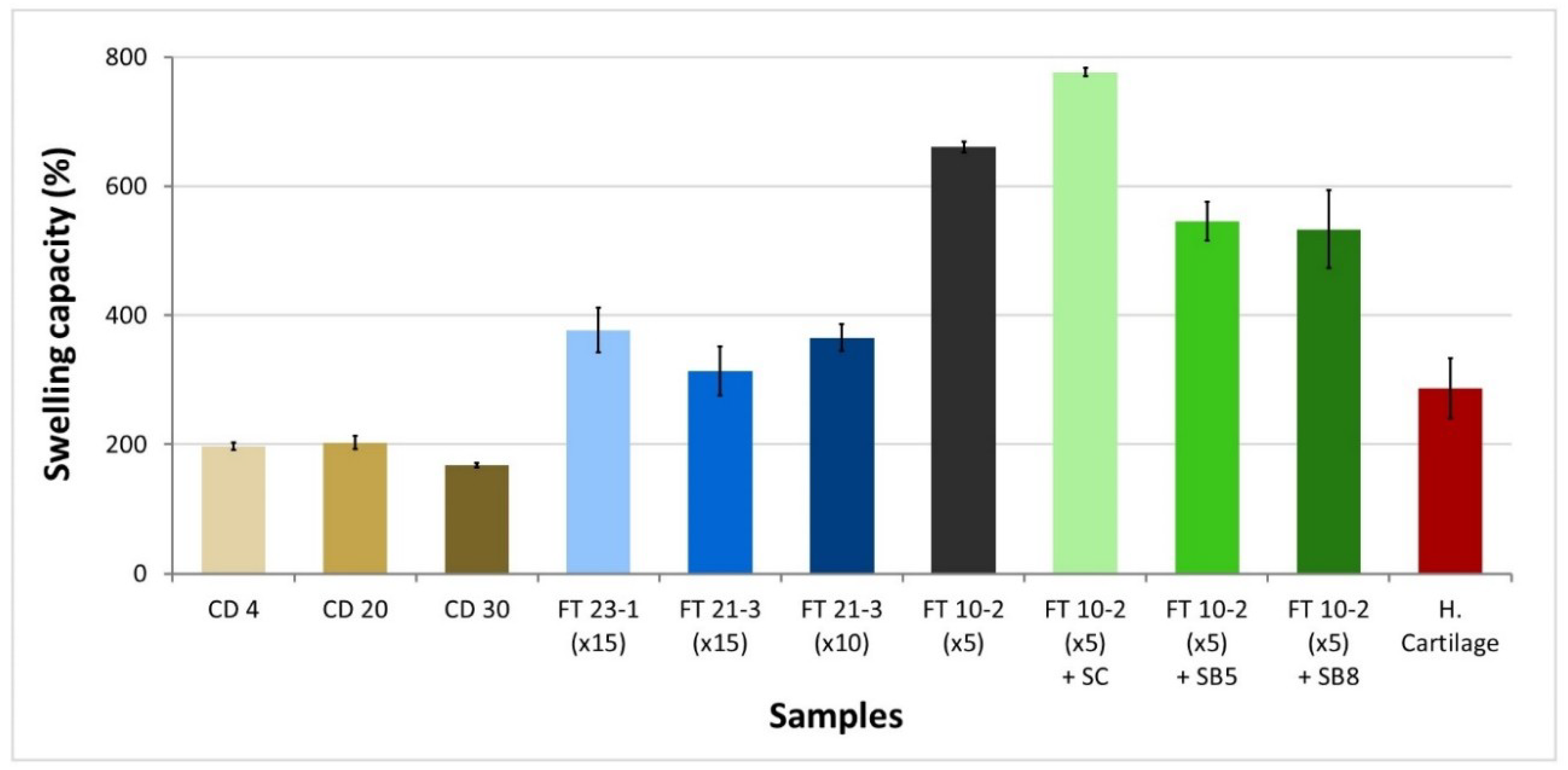
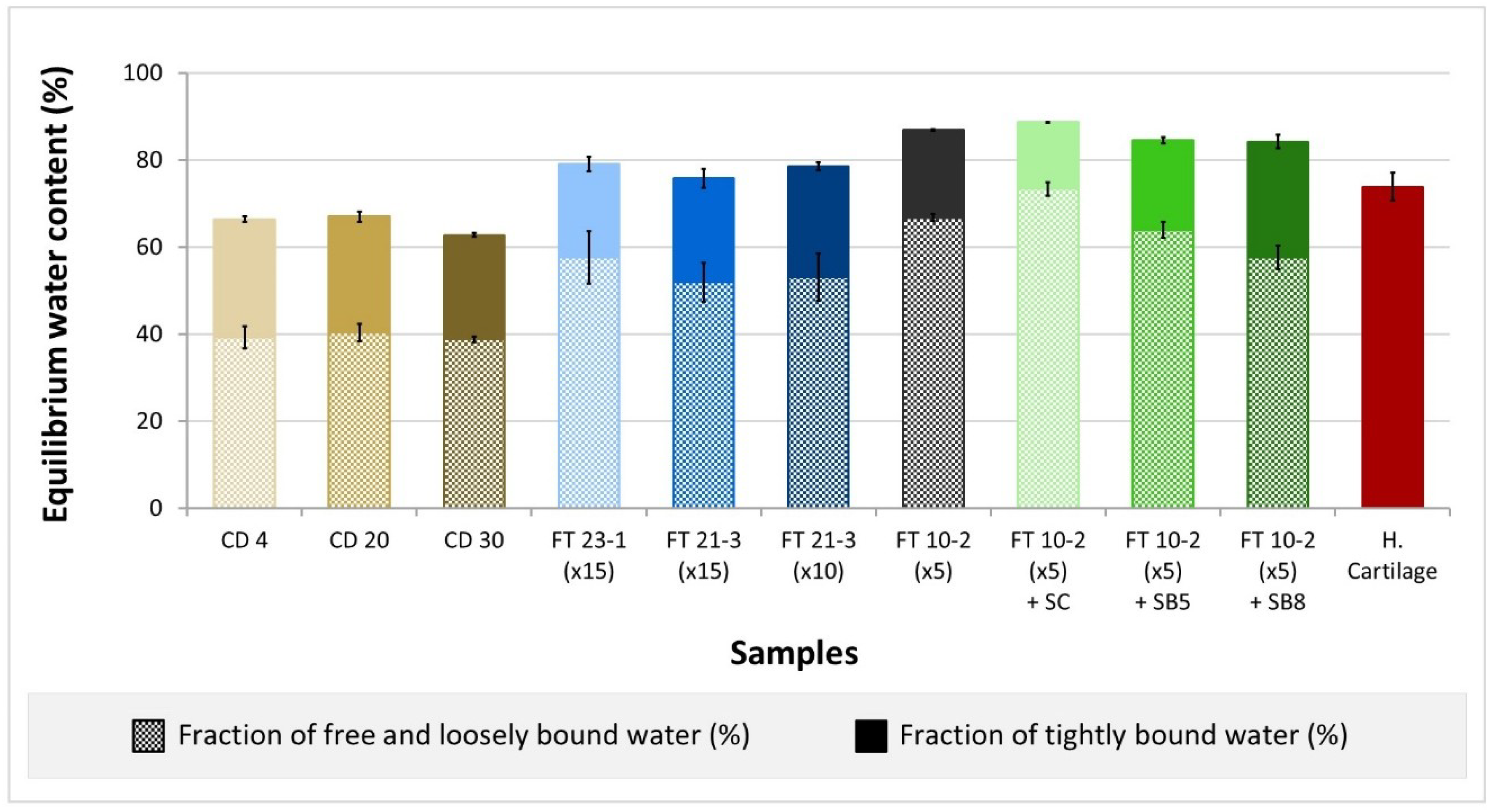
Water Uptake
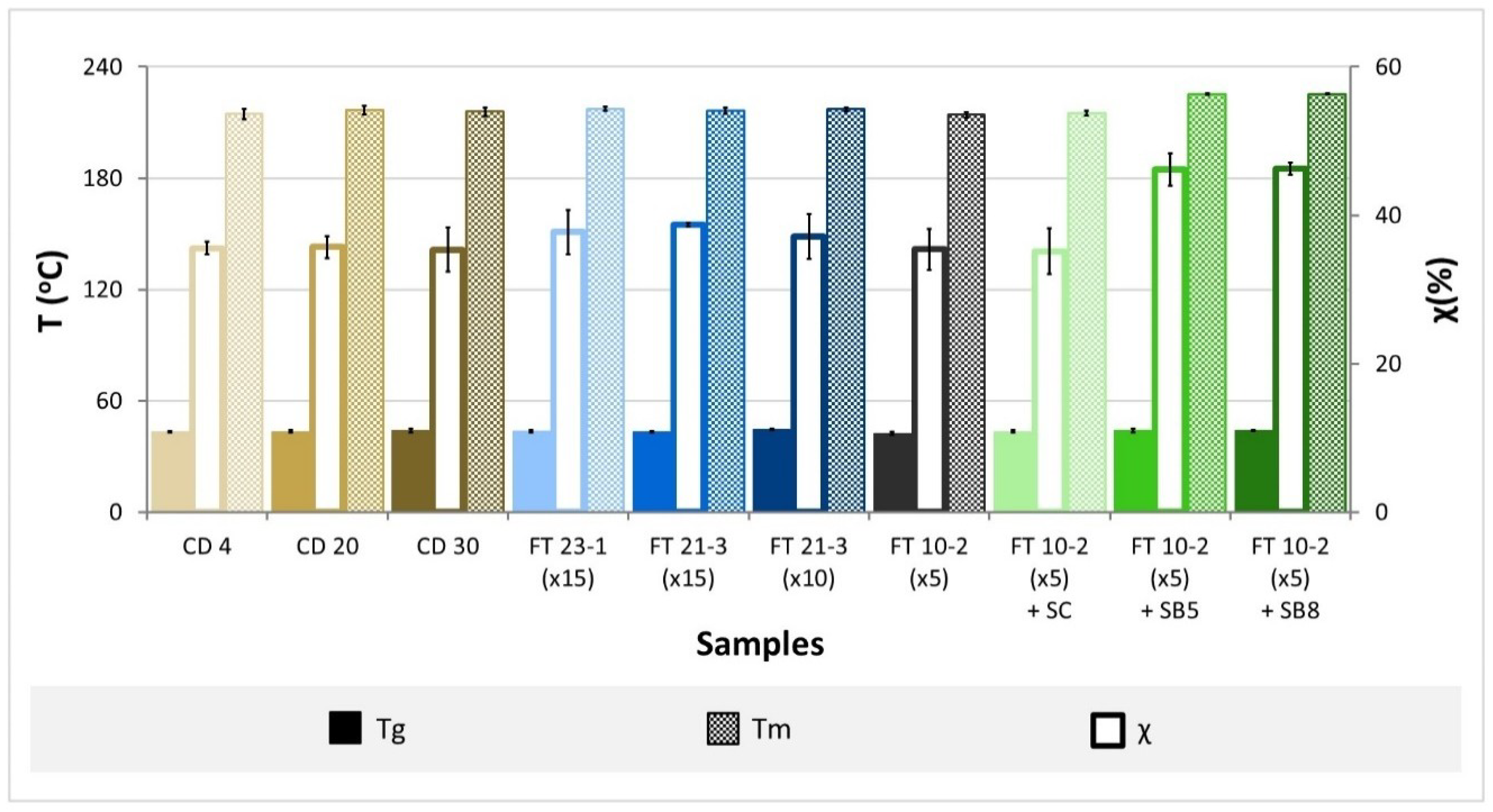
Thermotropic Behavior
Mechanical Properties
Tribological Behavior
3. Results and Discussion
3.1. Surface Morphology
3.2. Water Uptake
3.3. Thermotropic Behavior
3.4. Mechanical Properties
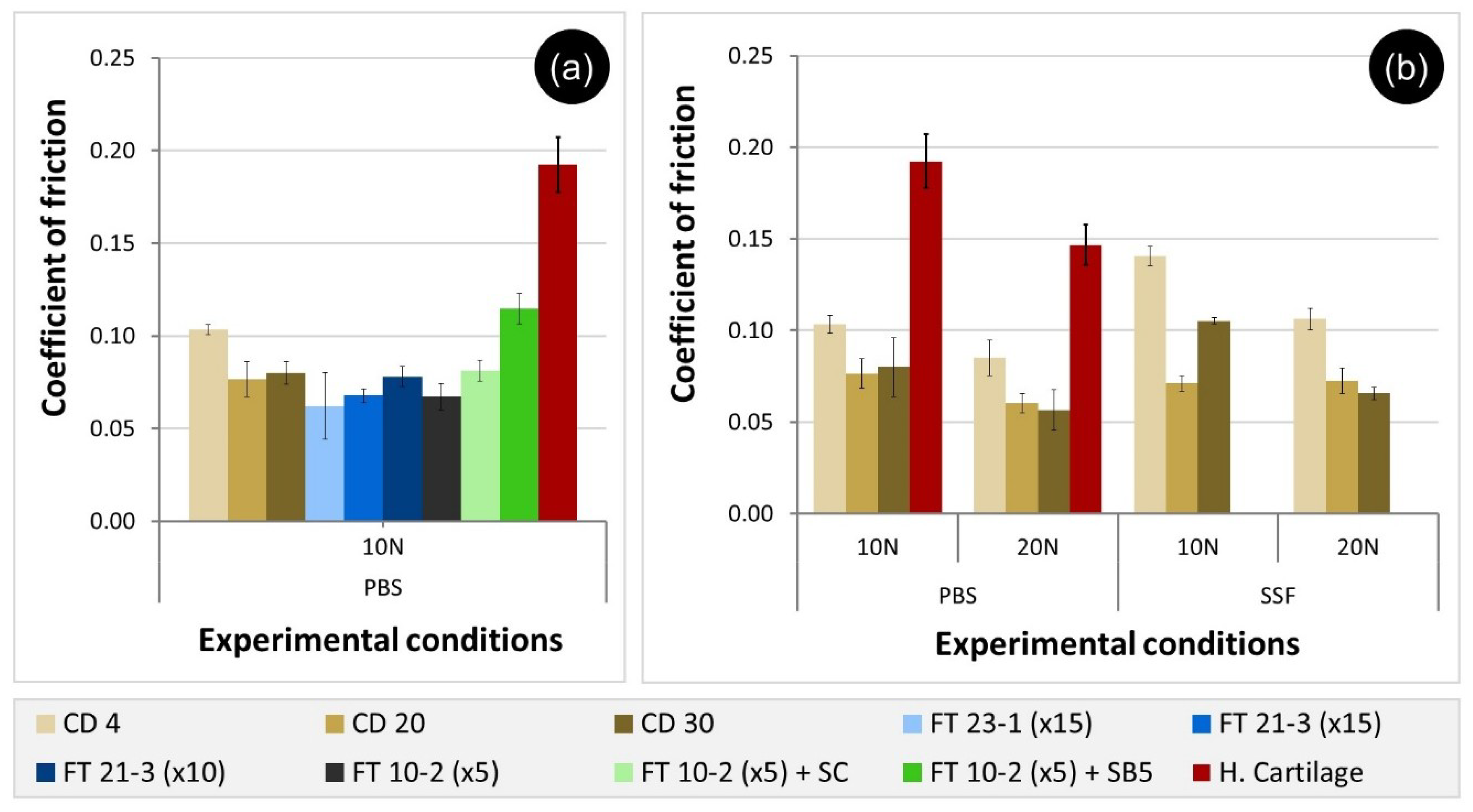
3.5. Tribological Behavior
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fox, S.A.J.; Bedi, A.; Rodeo, S.A. The Basic Science of Articular Cartilage: Structure, Composition, and Function. Sport. Heal. A Multidiscip. Approach 2009, 1, 461–468. [Google Scholar]
- Karuppal, R. Current concepts in the articular cartilage repair and regeneration. J. Orthop. 2017, 14, A1. [Google Scholar] [CrossRef]
- Redman, S.; Oldfield, S.; Archer, C. Current strategies for articular cartilage repair. Eur. Cells Mater. 2005, 9, 23–32. [Google Scholar] [CrossRef]
- Rönn, K.; Reischl, N.; Gautier, E.; Jacobi, M. Current Surgical Treatment of Knee Osteoarthritis. Arthritis 2011, 2011, 454873. [Google Scholar] [CrossRef]
- Vyas, D.; Rabuck, S.J.; Harner, C.D. Allograft Anterior Cruciate Ligament Reconstruction: Indications, Techniques, and Outcomes. J. Orthop. Sport. Phys. Ther. 2012, 42, 196–207. [Google Scholar] [CrossRef]
- Han, Y.; Li, X.; Zhang, Y.; Han, Y.; Chang, F.; Ding, J. Mesenchymal Stem Cells for Regenerative Medicine. Cells 2019, 8, 886. [Google Scholar] [CrossRef]
- Wang, C.; Feng, N.; Chang, F.; Wang, J.; Yuan, B.; Cheng, Y.; Liu, H.; Yu, J.; Zou, J.; Ding, J.; et al. Injectable Cholesterol-Enhanced Stereocomplex Polylactide Thermogel Loading Chondrocytes for Optimized Cartilage Regeneration. Adv. Healthc. Mater. 2019, 8, 1900312. [Google Scholar] [CrossRef]
- Zhang, J.; Dong, S.; Sivak, W.N.; Sun, H.B.; Chang, P. Stem Cells in Cartilage Diseases and Repair 2018. Stem Cells Int. 2018, 2018, 454873. [Google Scholar] [CrossRef]
- Murakami, T.; Yarimitsu, S.; Nakashima, K.; Sakai, N.; Yamaguchi, T.; Sawae, Y.; Suzuki, A. Biphasic and boundary lubrication mechanisms in artificial hydrogel cartilage: A review. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2015, 229, 864–878. [Google Scholar] [CrossRef]
- Rey-Rico, A.; Madry, H.; Cucchiarini, M. Hydrogel-Based Controlled Delivery Systems for Articular Cartilage Repair. Biomed. Res. Int. 2016, 2016, 1215263. [Google Scholar] [CrossRef]
- Katta, J.K.; Marcolongo, M.; Lowman, A.; Mansmann, K.A. Friction and wear behavior of poly(vinyl alcohol)/poly(vinyl pyrrolidone) hydrogels for articular cartilage replacement. J. Biomed. Mater. Res. Part A 2007, 83, 471–479. [Google Scholar] [CrossRef]
- Hassan, C.M.; Peppas, N.A. Structure and Applications of Poly (vinyl alcohol) Hydrogels Produced by Conventional Crosslinking or by Freezing/Thawing Methods. In Biopolymers PVA Hydrogels, Anionic Polymerisation Nanocomposites; Advances in Polymer Science; Springer: Heidelberg/Berlin, Germany, 2000; Volume 153, pp. 37–65. [Google Scholar]
- Kumar, A.; Han, S.S. PVA-based hydrogels for tissue engineering: A review. Int. J. Polym. Mater. Polym. Biomater. 2017, 66, 159–182. [Google Scholar] [CrossRef]
- Moreau, D. Design and Characterization of Hydrogel Films and Hydrogel-Ceramic Composites for Biomedical Applications. Ph.D. Thesis, PSL Research University, Paris, France, 2016. [Google Scholar]
- Bray, J.C.; Merrill, E.W. Poly (vinyl alcohol) hydrogels. Formation by electron beam irradiation of aqueous solutions and subsequent crystallization. J. Appl. Polym. Sci. 1973, 17, 3779–3794. [Google Scholar] [CrossRef]
- Shi, Y.; Xiong, D.; Zhang, J. Effect of irradiation dose on mechanical and biotribological properties of PVA/PVP hydrogels as articular cartilage. Tribol. Int. 2014, 78, 60–67. [Google Scholar] [CrossRef]
- Bodugoz-Senturk, H.; Choi, J.; Oral, E.; Kung, J.H.; Macias, C.E.; Braithwaite, G.; Muratoglu, O.K. The effect of polyethylene glycol on the stability of pores in polyvinyl alcohol hydrogels during annealing. Biomaterials 2008, 29, 141–149. [Google Scholar] [CrossRef]
- Kumar, A.; Mishra, R.; Reinwald, Y.; Bhat, S. Cryogels: Freezing unveiled by thawing. Mater. Today 2010, 13, 42–44. [Google Scholar] [CrossRef]
- Liu, Y.; Geever, L.M.; Kennedy, J.E.; Higginbotham, C.L.; Cahill, P.A.; McGuinness, G.B. Thermal behavior and mechanical properties of physically crosslinked PVA/Gelatin hydrogels. J. Mech. Behav. Biomed. Mater. 2010, 3, 203–209. [Google Scholar] [CrossRef]
- Sasaki, S.; Suzuki, A. Factors influencing the swelling and elution properties of poly (vinyl alcohol) cast gels. Polym. Adv. Technol. 2016, 27, 318–324. [Google Scholar] [CrossRef]
- Kawanishi, K.; Komatsu, M.; Inoue, T. Thermodynamic consideration of the sol-gel transition in polymer solutions. Polymer 1987, 28, 980–984. [Google Scholar] [CrossRef]
- Tai, B.C.U.; Du, C.; Gao, S.; Wan, A.C.A. Synthetic Poly (Vinyl Alcohol)—Based Membranes for Cartilage Surgery and Repair. Biotechnol. J. 2017, 12, 1700134. [Google Scholar] [CrossRef]
- Coluccino, L.; Gottardi, R.; Ayadi, F.; Athanassiou, A.; Tuan, R.S.; Ceseracciu, L. Porous Poly (vinyl alcohol)—Based Hydrogel for Knee Meniscus Functional Repair. ACS Biomater. Sci. Eng. 2018, 4, 1518–1527. [Google Scholar] [CrossRef]
- Peppas, N.A.; Merrill, E.W. Differential scanning calorimetry of crystallized PVA hydrogels. J. Appl. Polym. Sci. 1976, 20, 1457–1465. [Google Scholar] [CrossRef]
- Guan, L.; Xu, H.; Huang, D. The investigation on states of water in different hydrophilic polymers by DSC and FTIR. J. Polym. Res. 2011, 18, 681–689. [Google Scholar] [CrossRef]
- Suzuki, A.; Murakami, T. High-Strength Poly (Vinyl Alcohol) Hydrogels for Artificial Cartilage. In Encyclopedia of Biocolloid and Biointerface Science 2V Set; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2016; pp. 269–270. [Google Scholar]
- Holloway, J.L.; Lowman, A.M.; Palmese, G.R. The role of crystallization and phase separation in the formation of physically cross-linked PVA hydrogels. Soft Matter 2013, 9, 826–833. [Google Scholar] [CrossRef]
- Perfetti, G.; Jansen, K.M.B.; Wildeboer, W.J.; Hee, P.V.; Meesters, G.M.H. Characterization of physical and viscoelastic properties of polymer films for coating applications under different temperature of drying and storage. Int. J. Pharm. 2010, 384, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, E.; Komiya, S.; Sasaki, S.; Xing, J.; Bando, Y.; Hirashima, Y.; Sugiyama, M.; Suzuki, A. Effects of preparation temperature on swelling and mechanical properties of PVA cast gels. Soft Matter 2012, 8, 8129–8136. [Google Scholar] [CrossRef]
- Murakami, T.; Yarimitsu, S.; Sakai, N.; Nakashima, K.; Yamaguchi, T.; Sawae, Y.; Suzuki, A. Superior lubrication mechanism in poly(vinyl alcohol) hybrid gel as artificial cartilage. Proc. Inst. Mech. Eng. Part J J. Eng. Tribol. 2017, 231, 1160–1170. [Google Scholar] [CrossRef]
- Murakami, T.; Sakai, N.; Yamaguchi, T.; Yarimitsu, S.; Nakashima, K.; Sawae, Y.; Suzuki, A. Evaluation of a superior lubrication mechanism with biphasic hydrogels for artificial cartilage. Tribol. Int. 2015, 89, 19–26. [Google Scholar] [CrossRef]
- Marrella, A.; Lagazzo, A.; Dellacasa, E.; Pasquini, C.; Finocchio, E.; Barberis, F.; Pastorino, L.; Giannoni, P.; Scaglione, S. 3D Porous Gelatin/PVA Hydrogel as Meniscus Substitute Using Alginate Micro-Particles as Porogens. Polymers 2018, 10, 380. [Google Scholar] [CrossRef]
- Kumar, B.Y.S.; Isloor, A.M.; Kumar, G.C.M. Viscoelastic Behavior of HAp Reinforced Polyvinyl Alcohol Composite Hydrogel for Tissue Engineered Articular Cartilages. In Advances in Polymer Composites: Mechanics, Characterization And Applications, Proceedings of the Second International Conference on Polymer Composites (ICPC 2018), Surathkal, India, 15–16 December 2018; Kumar, G.C.M., Doddamani, M.R., Eds.; American Institute of Physic: College Park, MD, USA, 2019; p. 20062. [Google Scholar]
- Miao, T.; Miller, E.J.; McKenzie, C.; Oldinski, R.A. Physically crosslinked polyvinyl alcohol and gelatin interpenetrating polymer network theta-gels for cartilage regeneration. J. Mater. Chem. B 2015, 3, 9242–9249. [Google Scholar] [CrossRef]
- Draghi, L.; Resta, S.; Pirozzolo, M.G.; Tanzi, M.C. Microspheres leaching for scaffold porosity control. J. Mater. Sci. Mater. Med. 2005, 16, 1093–1097. [Google Scholar] [CrossRef] [PubMed]
- Lozinsky, V.I.; Okay, O. Basic Principles of Cryotropic Gelation. In Polymeric Cryogels: Macroporous Gels with Remarkable Properties; Okay, O., Ed.; Springer International Publishing: Basel, Switzerland, 2014; Volume 263, pp. 49–101. [Google Scholar]
- Patachia, S.; Florea, C.; Friedrich, C.; Thomann, Y. Tailoring of poly (vinyl alcohol) cryogels properties by salts addition. Express Polym. Lett. 2009, 3, 320–331. [Google Scholar] [CrossRef]
- Gottardi, R.; Hansen, U.; Raiteri, R.; Loparic, M.; Düggelin, M.; Mathys, D.; Friederich, N.F.; Bruckner, P.; Stolz, M. Supramolecular Organization of Collagen Fibrils in Healthy and Osteoarthritic Human Knee and Hip Joint Cartilage. PLoS ONE 2016, 11, e0163552. [Google Scholar] [CrossRef] [PubMed]
- Changoor, A.; Nelea, M.; Méthot, S.; Tran-Khanh, N.; Chevrier, A.; Restrepo, A.; Shive, M.S.; Hoemann, C.D.; Buschmann, M.D. Structural characteristics of the collagen network in human normal, degraded and repair articular cartilages observed in polarized light and scanning electron microscopies. Osteoarthr. Cartil. 2011, 19, 1458–1468. [Google Scholar] [CrossRef] [PubMed]
- Noh, T.; Bando, Y.; Ota, K.; Sasaki, S.; Suzuki, A. Tear force of physically crosslinked poly (vinyl alcohol) gels with different submicrometer-scale network structures. J. Appl. Polym. Sci. 2015, 132, 41356. [Google Scholar] [CrossRef]
- Holloway, J.L.; Spiller, K.L.; Lowman, A.M.; Palmese, G.R. Analysis of the in vitro swelling behavior of poly (vinyl alcohol) hydrogels in osmotic pressure solution for soft tissue replacement. Acta Biomater. 2011, 7, 2477–2482. [Google Scholar] [CrossRef]
- Pavelka, M.; Roth, J. Articular Cartilage. In Functional Ultrastructure; Springer: Vienna, Austria, 2010; pp. 294–295. [Google Scholar]
- Gupta, S.; Pramanik, A.K.; Kailath, A.; Mishra, T.; Guha, A.; Nayar, S.; Sinha, A. Composition dependent structural modulations in transparent poly (vinyl alcohol) hydrogels. Colloids Surf. B Biointerfaces 2009, 74, 186–190. [Google Scholar] [CrossRef]
- Nkhwa, S.; Lauriaga, K.F.; Kemal, E.; Deb, S. Poly (vinyl alcohol): Physical Approaches to Designing Biomaterials for Biomedical Applications. Conf. Pap. Sci. 2014, 2014, 403472. [Google Scholar] [CrossRef]
- Tranoudis, I.; Efron, N. Water properties of soft contact lens materials. Contact Lens Anterior Eye 2004, 27, 193–208. [Google Scholar] [CrossRef]
- Murakami, T.; Yarimitsu, S.; Nakashima, K.; Yamaguchi, T.; Sawae, Y.; Sakai, N.; Suzuki, A. Superior lubricity in articular cartilage and artificial hydrogel cartilage. Proc. Inst. Mech. Eng. Part J J. Eng. Tribol. 2014, 228, 1099–1111. [Google Scholar] [CrossRef]
- Gaharwar, A.; Schexnailder, P.; Schmidt, G. Nanocomposite Polymer Biomaterials for Tissue Repair of Bone and Cartilage. In Nanobiomaterials Handbook; CRC Press: Boca Raton, FL, USA, 2011; pp. 1–28. [Google Scholar]
- Akizuki, S.; Mow, V.C.; Müller, F.; Pita, J.C.; Howell, D.S.; Manicourt, D.H. Tensile properties of human knee joint cartilage: I. Influence of ionic conditions, weight bearing, and fibrillation on the tensile modulus. J. Orthop. Res. 1986, 4, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.-S.; Xiong, D.-S.; Chen, X.-L. Friction Behavior of Poly (Vinyl Alcohol) Gel Against Stainless Steel Ball in Different Lubricant Media. J. Tribol. 2008, 130, 031802. [Google Scholar] [CrossRef]
- Kosukegawa, H.; Fridrici, V.; Kapsa, P.; Sutou, Y.; Adachi, K.; Ohta, M. Friction Properties of Medical Metallic Alloys on Soft Tissue—Mimicking Poly (Vinyl Alcohol) Hydrogel Biomodel. Tribol. Lett. 2013, 51, 311–321. [Google Scholar] [CrossRef]
- Li, F.; Su, Y.; Wang, J.; Wu, G.; Wang, C. Influence of dynamic load on friction behavior of human articular cartilage, stainless steel and polyvinyl alcohol hydrogel as artificial cartilage. J. Mater. Sci. Mater. Med. 2010, 21, 147–154. [Google Scholar] [CrossRef]
- Covert, R.J.; Ott, R.D.; Ku, D.N. Friction characteristics of a potential articular cartilage biomaterial. Wear 2003, 255, 1064–1068. [Google Scholar] [CrossRef]
- Li, F.; Wang, A.; Wang, C. Analysis of friction between articular cartilage and polyvinyl alcohol hydrogel artificial cartilage. J. Mater. Sci. Mater. Med. 2016, 27, 87. [Google Scholar] [CrossRef]
- Serro, A.P.; Colaço, R.; Saramago, B. Effect of Albumin Adsorption on Biotribological Properties of Artificial Joint Materials. In Proteins at Interfaces III State of the Art; Horbett, T.A., Brash, J.L., Norde, W., Eds.; ACS Symposium Series; Oxford University Press: Oxford, UK, 2012; Volume 1120, pp. 497–523. [Google Scholar]

| Cast-Drying | Freeze-Thawing | |||||
|---|---|---|---|---|---|---|
| Samples | Drying Temperature (°C) | Samples | Freezing Time/Cycle (h) | Thawing Time/Cycle (h) | Number of Cycles | Pore-Forming Agent |
| CD 4 | 4 | |||||
| CD 20 | 20 | |||||
| CD 30 | 30 | |||||
| FT 23-1 (×15) | 23 | 1 | 15 | - | ||
| FT 21-3 (×15) | 21 | 3 | 15 | - | ||
| FT 21-3 (×10) | 21 | 3 | 10 | - | ||
| FT 10-2 (×5) | 10 | 2 | 5 | - | ||
| FT 10-2 (×5) + SC | 10 | 2 | 5 | NaCl (1:6 w/w) * | ||
| FT 10-2 (×5) + SB5 | 10 | 2 | 5 | NaHCO3 (5:1 w/w) * | ||
| FT 10-2 (×5) + SB8 | 10 | 2 | 5 | NaHCO3 (8:1 w/w) * | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, A.S.; Seidi, O.; Ribeiro, N.; Colaço, R.; Serro, A.P. Tribomechanical Comparison between PVA Hydrogels Obtained Using Different Processing Conditions and Human Cartilage. Materials 2019, 12, 3413. https://doi.org/10.3390/ma12203413
Oliveira AS, Seidi O, Ribeiro N, Colaço R, Serro AP. Tribomechanical Comparison between PVA Hydrogels Obtained Using Different Processing Conditions and Human Cartilage. Materials. 2019; 12(20):3413. https://doi.org/10.3390/ma12203413
Chicago/Turabian StyleOliveira, Andreia Sofia, Oumar Seidi, Nuno Ribeiro, Rogério Colaço, and Ana Paula Serro. 2019. "Tribomechanical Comparison between PVA Hydrogels Obtained Using Different Processing Conditions and Human Cartilage" Materials 12, no. 20: 3413. https://doi.org/10.3390/ma12203413
APA StyleOliveira, A. S., Seidi, O., Ribeiro, N., Colaço, R., & Serro, A. P. (2019). Tribomechanical Comparison between PVA Hydrogels Obtained Using Different Processing Conditions and Human Cartilage. Materials, 12(20), 3413. https://doi.org/10.3390/ma12203413








