Hydro-Thermal Fatigue of Polymer Matrix Composite Biomaterials
Abstract
:1. Introduction
2. Material and Research Method
2.1. Materials
2.2. Method of Thermocycling
2.3. Methods for Investigating Strength
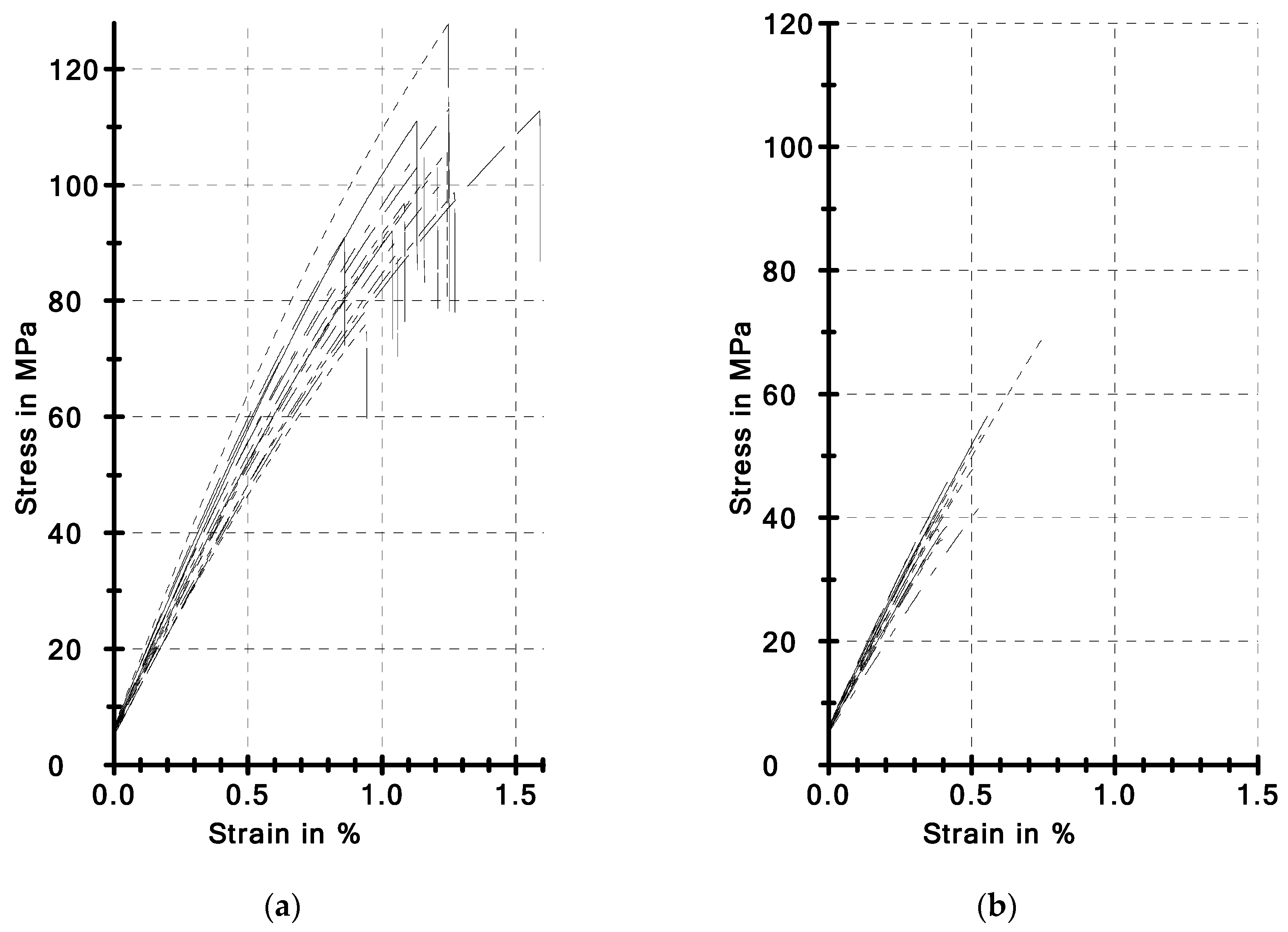
3. Results and Discussion
3.1. BFS and TFS Strength (Aging Only)
3.2. Impact of Thermocycling
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Willems, G.; Lambrechts, P.; Braem, M.; Celis, J.P.; Vanherle, G. A classification of dental composites according to their morphological and mechanical characteristics. Dent. Mater. 1992, 8, 310–319. [Google Scholar] [CrossRef]
- Braem, M.J.; Davidson, C.L.; Lambrechts, P.; Vanherle, G. In vitro flexural fatigue limits of dental composites. J. Biomed. Mater. Res. 1994, 28, 1397–1402. [Google Scholar] [CrossRef]
- Madej, M.; Ozimina, D.; Cwanek, J.; Styp-Rekowski, M. The analysis of tribological wear of polythene UHMW PE applied in biotribological systems. Tribologia 2010, 1, 61–76. [Google Scholar]
- Będziński, R. Experimental and numerical methods in biomechanics. Biocybern. Biomed. Eng. 2007, 27, 275–292. [Google Scholar]
- Pieniak, D. Initiation and tolerance of macro-damage of first ply (fbf) in a process of damaging of hybrid multi-ply structures due to reinforcement architecture. Adv. Mater. Sci. 2018, 18, 77–91. [Google Scholar] [CrossRef]
- Pieniak, D.; Niewczas, A. Phenomenological evaluation of fatigue cracking of dental restorations under conditions of cyclic mechanical loads. Acta Bioeng. Biomech. 2012, 14, 9–17. [Google Scholar] [PubMed]
- Eftekhari, M.; Fatemi, A. On the strengthening effect of increasing cycling frequency on fatigue behavior of some polymers and their composites: Experiments and modeling. Int. J. Fatigue 2016, 87, 153–166. [Google Scholar] [CrossRef]
- Kelly, J.R. Perspectives on strength. Dent. Mater. 1995, 11, 103–111. [Google Scholar] [CrossRef]
- Rodrigues, S.A., Jr.; Ferracane, J.L.; Bona, A.D. Flexural strength and Weibull analysis of a microhybrid and a nanofill composite evaluated by 3- and 4-point bending tests. Dent. Mater. 2008, 24, 426–431. [Google Scholar]
- Bechtold, J.; dos Santos, P.J.; Anido-Anido, A.; di Hipolito, V.; Alonso, R.C.B.; D’Alpino, P.H.P. Hardness, polymerization depth, and internal adaptation of Class II silorane composite restorations as a function of polymerization protocol. Eur. J. Dent. 2012, 6, 133–140. [Google Scholar] [Green Version]
- Asmussen, E.; Peutzfeldt, A. Influence of UEDMA, BisGMA and TEGDMA on selected mechanical properties of experimental resin composites. Dent. Mater. 1998, 14, 51–56. [Google Scholar] [CrossRef]
- Fu, S.Y.; Feng, X.Q.; Lauke, B.; Mai, Y.W. Effects of particle size, particle/matrix interface adhesion and particle loading on mechanical properties of particulate-polymer composites. Compos. Part B Eng. 2008, 39, 933–961. [Google Scholar] [CrossRef]
- Gurumurthy, C.K.; Kramer, E.J.; Hui, C. Hydro-thermal fatigue of polymer interfaces. Hydro-thermal fatigue of polymer interfaces. Acta Mater. 2001, 49, 3309–3320. [Google Scholar] [CrossRef]
- Jakowluk, A. Procesy Pełzania i Zmęczenia w Materiałach; WNT: Warszawa, Poland, 1993; p. 483. (In Polish) [Google Scholar]
- Hales, R. Fatigue testing methods of elevated temperature. In Fatigue at High Temperature; Skelton, R.P., Ed.; Applied Science: London, UK, 1983; pp. 63–96. [Google Scholar]
- Lohbauer, U.; Belli, R.; Ferracene, J.L. Factors involved in mechanical fatigue degradation of dental resin composites. J. Dent. Res. 2013, 92, 584–591. [Google Scholar] [CrossRef]
- Milewski, G. Biomechanika w stomatologii zachowawczej. In Biomechanika, Tom XII; Będziński, R., Ed.; IPPT PAN: Warszawa, Poland, 2011; pp. 667–751. (In Polish) [Google Scholar]
- Kim, M.H.; Min, S.H.; Ferracane, J.; Lee, I.B. Initial dynamic viscoelasticity change of composites during light curing. Dent. Mater. 2010, 26, 463–470. [Google Scholar] [CrossRef]
- Ornaghi, B.P.; Meier, M.M.; Rosa, V.; Cesar, P.F.; Lohbauer, U.; Braga, R.R. Subcritical crack growth and in vitro lifetime prediction of resin composites with different filler distributions. Dent. Mater. 2012, 28, 985–995. [Google Scholar] [CrossRef]
- Ferracane, J.L. Hygroscopic and hydrolytic effects in dental polymer networks. Dent. Mater. 2006, 22, 211–222. [Google Scholar] [CrossRef]
- Finer, Y.; Santerre, J.P. The influence of resin chemistry on a dental composite’s biodegradation. J. Biomed. Mater. Res. A 2004, 69, 233–246. [Google Scholar] [CrossRef]
- Janda, R.; Roulet, J.F.; Latta, M.; Ruttermann, S. Water sorption and solubility of contemporary resin-based filling materials. J. Biomed. Mater. Res. Part B Appl. Biomater. 2007, 82, 545–551. [Google Scholar] [CrossRef]
- Leibrock, H.; Degenhart, M.; Behr, M.; Rosentritt, M.; Handel, G. In vitro study on the effect of thermo- and load-cycling on the bond strength of porcelain repair systems. J. Oral Rehabil. 1999, 26, 130–137. [Google Scholar] [CrossRef]
- Akin, H.; Ozdemir, A.K. Effect of corrosive environments and thermocycling on the attractive force of four types of dental magnetic attachments. J. Den. Sci. 2013, 8, 184–188. [Google Scholar] [CrossRef] [Green Version]
- Morresi, A.L.; D’Amarioa, M.; Capogreco, M.; Gatto, R.; Marzo, G.; D’Arcangelo, C.; Monaco, A. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing? A literature review. J. Mech. Behav. Biomed. 2014, 29, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, A.N.; Mitsui, F.H.O.; Ambrosano, G.M.B.; Marchi, G.M. Influence of adhesive systems and flowable composite lining on bond strength of class II restorations submitted to thermal and mechanical stresses. J. Biomed. Mater. Res. Part B Appl. Biomater. 2007, 80, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Walczak, A.; Niewczas, A.; Pieniak, D.; Gil, L.; Kozłowski, E.; Kordos, P. Temporary Stability of Compressive Strength of Flow and Universal Type LC PMCCS Materials. Adv. Mat. Sci. 2018, 18, 22–33. [Google Scholar] [Green Version]
- Pieniak, D.; Walczak, A.; Niewczas, A.M.; Przystupa, K. The effect of thermocycling on surface layer properties of light cured polymer matrix ceramic composites (PMCCs) used in sliding friction pair. Materials. 2019, 12, 2776. [Google Scholar] [CrossRef]
- Pieniak, D.; Kordos, P. Analysis of the degree of hydro-thermal fatigue damage of the surface layer of polymer-ceramic composites intended for operation in a biotribological node. Tribologia 2019, 2, 105–115. [Google Scholar] [CrossRef]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Karbhari, V.M.; Strassler, H. Effect of fiber architecture on flexural characteristics and fracture of fiber-reinforced dental composites. Dent. Mater. 2007, 23, 8. [Google Scholar] [CrossRef]
- ISO 4049–Dentistry—Polymer-Based Restorative Materials; International Organization for Standardization: Geneva, Switzerland, 2019.
- Hahnel, S.; Dowling, A.H.; El-Safty, S.; Fleming, G.J.P. The influence of monomeric resin and filler characteristics on the performance of experimental resin-based composites (RNCs) derived from a commercial formulation. Dent. Mater. 2012, 28, 416–423. [Google Scholar] [CrossRef]
- Walczak, A.; Pieniak, D.; Niewczas, A.; Niewczas, A.M.; Kordos, P. Study of Ceramic-Polymer Composites Reliability Based on the Bending Strength Test. J. KONBiN 2015, 35, 169–178. [Google Scholar] [CrossRef]
- Niewczas, A.M.; Pieniak, D.; Ogrodnik, P. Reliability analysis of strength of dental composites subjected to different photopolymerization procedures. Eksploat. Niezawodn. 2012, 14, 249–255. [Google Scholar]
- Palin, W.M.; Fleming, G.J.P.; Marquis, P.M. The reliability of standardized flexure strength testing procedures for light-activated resin-based composite. Dent. Mater. 2005, 21, 911–919. [Google Scholar] [CrossRef] [PubMed]
- St-Georges, A.J.; Swift, E.J.; Thompson, J.Y.; Heymann, H.O. Irradiance effects on the mechanical properties of universal hybrid and flowable hybrid resin composites. Dent. Mater. 2003, 19, 406. [Google Scholar] [PubMed]
- ISO 6872 – Dentistry—Ceramic Materials; International Organization for Standardization: Geneva, Switzerland, 2015.
- Braem, M.; Lambrechts, P.; Van Doren, V.; Vanherle, G. The impact of composite structure on its elastic response. J. Dent. Res. 1986, 65, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, F.; Kawano, Y.; Braga, R.R. Contraction stress related to composite inorganic content. Dent. Mater. 2010, 26, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Ong, J.L.; Okuno, O. The effect of filler loading and morphology on the mechanical properties of contemporary composites. J. Prosthet. Dent. 2002, 87, 642–649. [Google Scholar] [CrossRef]
- Antunes, P.V.; Ramahlo, A.; Carrihlo, E.V.P. Mechanical and wear behaviours of nano and microfilled polymeric composite: Effect of filler fraction and size. Mater. Des. 2014, 61, 50–60. [Google Scholar]
- Ikejima, I.; Nomoto, R.; McCabe, J.F. Shear punch strength and flexural strength of model composites with varying filler volume fraction, particle size and silanization. Dent. Mater. 2002, 19, 206–211. [Google Scholar] [CrossRef]
- Ivanisevic, A.; Lainovic, T.; Blazic, L.; Vilotic, M. Influence of Light-curing Mode on the Mechanical Properties of Dental Resin Nanocomposites. Proc. Eng. 2014, 69, 921–930. [Google Scholar] [Green Version]
- Walker, M.P.; Haj-Ali, R.; Wang, Y.; Hunziker, D.; Williams, K.B. Influence of environmental conditions on dental composite flexural properties. Dent. Mater. 2006, 22, 1002–1007. [Google Scholar] [CrossRef]
- Adabo, G.L.; dos Santos Cruz, C.A.; Fonseca, R.G.; Vaz, L.G. The volumetric fraction of inorganic particles and the flexural strength of composites for posterior teeth. J. Dent. 2003, 31, 353–359. [Google Scholar] [CrossRef]
- Beun, S.; Glorieux, T.; Devaux, J.; Vreven, J.; Leloup, G. Characterization of nanofilled compared to universal and microfilled composites. Dent. Mater. 2007, 23, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Hickel, R. Investigations on mechanical behaviour of dental composites. Clin. Oral Investig. 2009, 13, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Leinfelder, K.F.; Bayne, S.C.; Swift, E.J., Jr. Packable composites: Overview and technical considerations. J. Esthet. Dent. 1990, 11, 234–249. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Zellweger, G.; Zappini, G. The relationship between physical parameters and wear of dental composites. Wear 2007, 263, 1138–1146. [Google Scholar] [CrossRef]
- Shalaby, W.S.; Salz, U. Polymers for Dental and Orthopedic Applications; CRC Press: Boca Raton, FL, USA, 2007; p. 440. [Google Scholar]
- Sideridou, I.; Karabela, M.M.; Vouvoudi, E.C. Physical properties of current dental nanohybrid and nanofill light-cured resin composites. Dent. Mater. 2011, 27, 598–607. [Google Scholar] [CrossRef]
- Mair, L.H.; Stolarski, T.A.; Vowles, R.W.; Lloyd, C.H. Wear: Mechanisms, manifestations and measurement. Rep. Workshop J. Dent. 1996, 24, 141–148. [Google Scholar]
- Kawano, F.; Ohguri, T.; Ichikawa, T.; Matsumoto, N. Influence of thermal cycles in water on flexural strength of laboratory-processed composite resin. J. Oral Rehabil. 2001, 28, 703–707. [Google Scholar] [CrossRef]
- Weir, M.D.; Moreau, J.L.; Levine, E.D.; Strassler, H.E.; Chow, L.C.; Xu, H.H.K. Nanocomposite containing CaF2 nanoparticles: Thermal cycling, wear and long-term water-aging. Dent. Mater. 2012, 28, 642–652. [Google Scholar] [CrossRef]
- Wang, J.; Kochan, O.; Przystupa, K.; Su, J. Information-Measuring System to Study the Thermocouple with Controlled Temperature Field. Meas. Sci. Rev. 2019, 19, 161–169. [Google Scholar] [CrossRef]
- Moraes, J.S.; Sostena, M.M.D.S.; Grandini, C.R. The Glass Transition Temperature in Dental Composites. In Ceramic and Polymeric Composites for Various Uses; Cuppoletti, J., Ed.; InTech: London, UK, 2011; pp. 669–684. [Google Scholar]
- Souza, R.O.; Ozcan, M.; Michida, S.M.; de Melo, R.M.; Pavanelli, C.A.; Bottino, M.A.; Soares, L.E.; Martin, A.A. Conversion degree of indirect resin composites and effect of thermocycling o their physical properties. J. Prosthodont. 2010, 19, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Ulker, M.; Ozcan, M.; Sengun, A.; Ozer, F.; Belli, S. Effect of artificial aging regimens on the performance of self etching adhesives. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 93, 175–184. [Google Scholar] [PubMed]
- Seimenis, I.; Sarafianou, A.; Papadopoulou, H.; Papadopoulou, T.R.J. Shear bond strength of three veneering resins to a Ni-Cr alloy using two bonding procedures. J. Oral Rehabil. 2006, 33, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Curtis, A.R.; Palina, W.M.; Fleming, G.J.P.; Shortall, A.C.C.; Marquis, P.M. The mechanical properties of nanofilled resin-based composites: The impact of dry and wet cyclic pre-loading on bi-axial flexure strength. Dent. Mater. 2009, 25, 188–197. [Google Scholar] [CrossRef]
- Yu, B.; Liu, D.; Liu, F.; He, J. Preparation and characterization of light-cured dental resin without methacrylate monomers derived from Bisphenol A. Adv. Polym. Tech. 2014, 33, 214–217. [Google Scholar] [CrossRef]
- Wang, Y.; Lee, J.J.; Lloyd, I.K.; Wilson, O.C., Jr.; Rosenblum, M.; Thompson, V. High modulus nanopowder reinforced dimethacrylate matrix composites for dental cement applications. J. Biomed. Mater. Res. A. 2007, 82, 651–657. [Google Scholar] [CrossRef]
- Soderholm, K.J. Fracture of dental materials. In Applied Fracture Mechanics; Belov, A., Ed.; InTech: Rijeka, Croatia, 2012; pp. 111–142. [Google Scholar]
- Sideridou, I.; Achilias, D.S.; Kyrikou, E. Thermal expansion characteristics of light-cureddental resins and resin composites. Biomaterials 2004, 25, 3087–3097. [Google Scholar] [CrossRef]
- Bełzowski, A. Metoda oceny stopnia uszkodzenia kompozytów polimerowych. Kompozyty 2002, 2, 4. [Google Scholar]






| Parameter | Name of Materials | ||
|---|---|---|---|
| Filtek Z550 (Abbreviation—Z550) | Ex-nano(G) | Ex-Flow(G) | |
| Manufacturer | 3M ESPE (USA) | – | – |
| Type | Nanohybrid composite | Nano composite | Semi-liquid composite |
| Matrix | BIS-GMA, UDMA, BIS-EMA, PEGDMA, TEGDMA | BIS-GMA, UDMA, TEGDMA | BIS-GMA, UDMA, TEGDMA |
| Filler | SiO2 20 nm, ZrO2/SiO2 5–20 nm, (0.6–1.4 mm clusters) | The inorganic filler particles consist of barium aluminum bore glass and highly dispersed silicon dioxide. | The inorganic filler particles comprise silica, dental glass (strontium aluminum-boron-silicate glass) |
| Content of Filler Molecules (wt.%) | 82% | 82% | 74% |
| Quantity | FBI | dL (FBI) | FFract | dL (FFract) | W (FBI) | W(FFract) | h |
|---|---|---|---|---|---|---|---|
| Unit | N | mm | N | mm | Nmm | Nmm | mm |
| Material | Z550 | ||||||
| nTC = 0 | |||||||
| 154.00 | 0.10 | 59.90 | 0.10 | 10.70 | 10.80 | 1.44 | |
| Std.dev. | 24.60 | 0.00 | 9.50 | 0.00 | 3.72 | 3.73 | 0.065 |
| ν | 15.97 | 22.14 | 15.86 | 21.93 | 34.81 | 34.50 | 4.53 |
| nTC = 10,000 | |||||||
| 129.00 | 0.10 | 49.00 | 0.10 | 8.21 | 8.51 | 1.31 | |
| Std.dev. | 36.70 | 0.00 | 15.40 | 0.00 | 3.92 | 3.65 | 0.074 |
| CV | 28.42 | 26.01 | 31.34 | 21.25 | 47.76 | 42.86 | 5.66 |
| Material | Ex-nano(G) | ||||||
| nTC = 0 | |||||||
| 156.00 | 0.20 | 60.40 | 0.20 | 12.39 | 12.53 | 1.26 | |
| Std.dev. | 10.60 | 0.00 | 4.17 | 0.00 | 1.30 | 1.30 | 0.057 |
| CV | 6.80 | 6.81 | 6.90 | 6.72 | 10.47 | 10.37 | 4.51 |
| nTC = 10,000 | |||||||
| 93.90 | 0.10 | 36.50 | 0.10 | 5.13 | 5.19 | 1.31 | |
| Std.dev. | 14.30 | 0.00 | 5.85 | 0.00 | 1.50 | 1.50 | 0.071 |
| CV | 15.23 | 14.10 | 16.03 | 13.92 | 29.23 | 28.94 | 5.42 |
| Material | Ex-flow(G) | ||||||
| nTC = 0 | |||||||
| 114.00 | 0.10 | 44.20 | 0.10 | 8.80 | 8.88 | 1.24 | |
| Std.dev. | 19.00 | 0.00 | 7.22 | 0.00 | 2.75 | 2.75 | 0.055 |
| CV | 16.67 | 15.51 | 16.33 | 15.29 | 31.30 | 30.93 | 4.43 |
| nTC = 10,000 | |||||||
| 81.30 | 0.10 | 31.80 | 0.10 | 4.41 | 4.45 | 1.24 | |
| Std.dev. | 12.40 | 0.00 | 4.93 | 0.00 | 1.31 | 1.31 | 0.063 |
| CV | 15.28 | 17.29 | 15.51 | 17.06 | 29.77 | 29.49 | 5.08 |
| Quantity | Ef | σfM | εfM | σfB | εfB | WfM | WfB |
|---|---|---|---|---|---|---|---|
| Unit | MPa | MPa | % | MPa | % | Nmm | Nmm |
| Material | Z550 | ||||||
| nTC = 0 | |||||||
| 6730 | 71.2 | 1.1 | 62.9 | 1.1 | 4.75 | 4.76 | |
| Std.dev. | 1120 | 16.8 | 0.3 | 16.8 | 0.3 | 2.24 | 2.25 |
| CV | 16.65 | 23.66 | 24.76 | 23.66 | 24.76 | 47.24 | 47.24 |
| nTC = 10,000 | |||||||
| 9990 | 59.4 | 0.7 | 53.0 | 0.7 | 2.36 | 2.37 | |
| Std.dev. | 1700 | 20.6 | 0.3 | 14.4 | 0.3 | 1.51 | 1.52 |
| CV | 17.04 | 34.66 | 48.94 | 27.12 | 48.76 | 64.16 | 64.20 |
| Material | Ex-nano (G) | ||||||
| nTC = 0 | |||||||
| 9910 | 99.5 | 1.1 | 78.4 | 1.1 | 6.41 | 6.43 | |
| Std.dev. | 1010 | 14.9 | 0.2 | 8.97 | 0.2 | 2.01 | 2.01 |
| CV | 10.19 | 14.97 | 19.54 | 11.44 | 19.53 | 31.31 | 31.27 |
| nTC = 10,000 | |||||||
| 9030 | 44.4 | 0.5 | 44.4 | 0.5 | 1.19 | 1.19 | |
| Std.dev. | 753 | 9.38 | 0.1 | 9.40 | 0.1 | 0.55 | 0.55 |
| CV | 8.34 | 21.11 | 23.45 | 21.18 | 23.36 | 46.21 | 46.08 |
| Material | Ex-flow (G) (N = 15) | ||||||
| nTC = 0 | |||||||
| 9190 | 54.4 | 0.5 | 54.4 | 0.5 | 1.65 | 1.65 | |
| Std.dev. | 517 | 9.86 | 0.1 | 9.86 | 0.1 | 0.6 | 0.6 |
| CV | 5.63 | 18.12 | 16.99 | 18.12 | 16.99 | 36.17 | 36.17 |
| nTC = 10,000 | |||||||
| 7980 | 21.5 | 0.2 | 21.5 | 0.2 | 0.30 | 0.30 | |
| Std.dev. | 605 | 2.98 | 0.0 | 3.02 | 0.0 | 0.09 | 0.09 |
| CV | 7.58 | 13.85 | 21.87 | 14.08 | 21.46 | 30.64 | 30.04 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pieniak, D.; Przystupa, K.; Walczak, A.; Niewczas, A.M.; Krzyzak, A.; Bartnik, G.; Gil, L.; Lonkwic, P. Hydro-Thermal Fatigue of Polymer Matrix Composite Biomaterials. Materials 2019, 12, 3650. https://doi.org/10.3390/ma12223650
Pieniak D, Przystupa K, Walczak A, Niewczas AM, Krzyzak A, Bartnik G, Gil L, Lonkwic P. Hydro-Thermal Fatigue of Polymer Matrix Composite Biomaterials. Materials. 2019; 12(22):3650. https://doi.org/10.3390/ma12223650
Chicago/Turabian StylePieniak, Daniel, Krzysztof Przystupa, Agata Walczak, Agata M. Niewczas, Aneta Krzyzak, Grzegorz Bartnik, Leszek Gil, and Paweł Lonkwic. 2019. "Hydro-Thermal Fatigue of Polymer Matrix Composite Biomaterials" Materials 12, no. 22: 3650. https://doi.org/10.3390/ma12223650






