Temperature Changes and SEM Effects of Three Different Implants-Abutment Connection during Debridement with Er:YAG Laser: An Ex Vivo Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples Collection
2.2. Sample Preparation
2.3. Surgical Procedure
2.4. Study Groups
2.5. Measurement Procedure
2.6. Scanning Electron Microscopy
2.7. Statistical Analysis
3. Results
3.1. Temperature Rise at Implant Level (P1 Thermocouple)
3.2. Temperature Rise at Abutment/Implant Level (P2 Thermocouple)
3.3. SEM Analysis
4. Discussion
5. Conclusions
- The Er:YAG laser debridement of two-piece and one-piece implants did not exceed the implant temperature by 10 °C at 100 mJ/30 Hz and 50 mJ/30 Hz;
- One-piece implants heat up faster than two-piece implants during Er:YAG laser irradiation at the implant’s collar area;
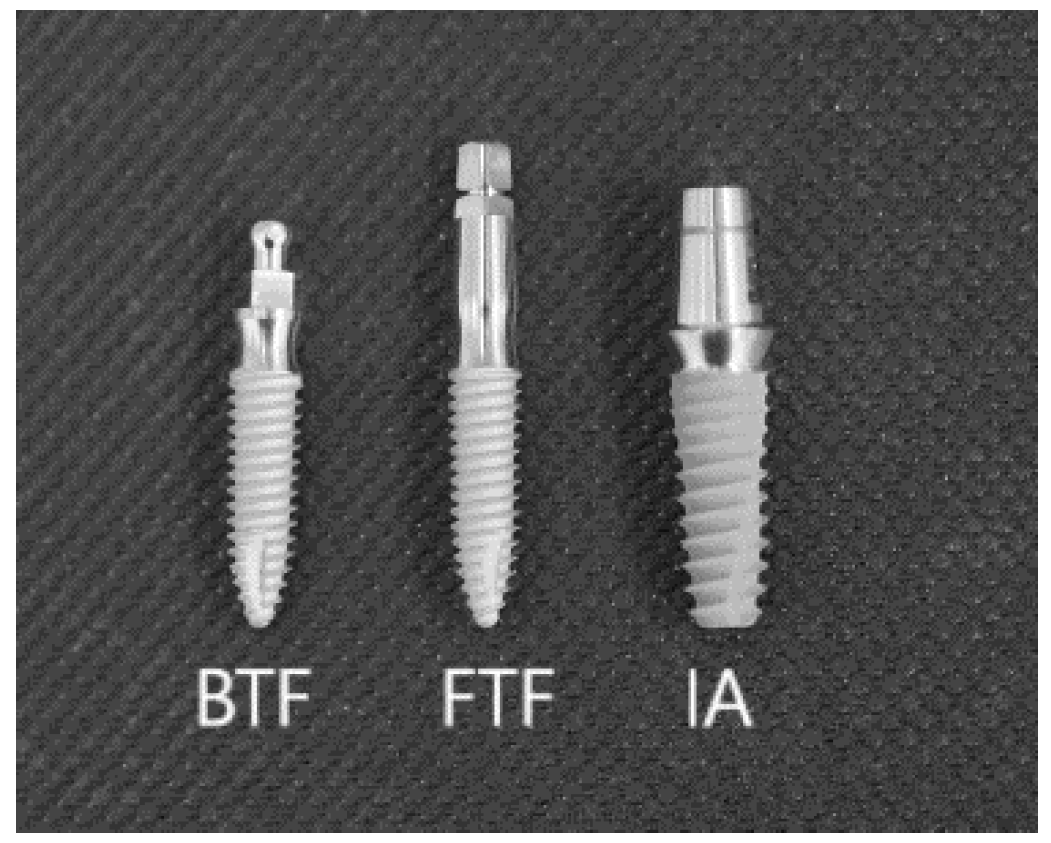
- Based on SEM analysis, the cracks and melting that occurred on the surface of two-piece implants were more pronounced compared to one-piece implants with the ball type fixture (BTF) and fix type fixture (FTF);
- Debridement of one-piece implants with a ball type fixture using Er:YAG laser at 200 mJ/30 Hz or more should be avoided. However, our findings should also be confirmed in the human in vivo model and using the implants of various manufactures.
Author Contributions
Funding
Conflicts of Interest
References
- Matys, J.; Swider, K.; Flieger, R. Laser instant implant impression method: A case presentation. Dent. Med. Probl. 2017, 54, 101–106. [Google Scholar] [CrossRef]
- Atieh, M.A.; Alsabeeha, N.H.; Faggion, C.M., Jr.; Duncan, W.J. The frequency of peri-implant diseases: A systematic review and meta-analysis. J. Periodontol. 2013, 84, 1586–1598. [Google Scholar] [CrossRef] [PubMed]
- Świder, K.; Dominiak, M.; Grzech-Leśniak, K.; Matys, J. Effect of Different Laser Wavelengths on Periodontopathogens in Peri-Implantitis: A Review of In Vivo Studies. Microorganisms 2019, 7, 189. [Google Scholar] [CrossRef] [PubMed]
- Lindhe, J.; Meyle, J. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [PubMed]
- Boever, A.L.; Boever, J.A. Early colonization of non-submerged dental implants in patients with a history of advanced aggressive periodontitis. Clin. Oral Implants Res. 2006, 17, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Fürst, M.M.; Salvi, G.E.; Lang, N.P.; Persson, G.R. Bacterial colonization immediately after installation on oral titanium implants. Clin. Oral Implants Res. 2007, 18, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Leonhardt, Å.; Renvert, S.; Dahlén, G. Microbial findings at failing implants. Clin. Oral Implants Res. 1999, 10, 339–345. [Google Scholar] [CrossRef]
- Bassi, F.; Poli, P.P.; Rancitelli, D.; Signorino, F.; Maiorana, C. Surgical treatment of peri-implantitis: A 17-year follow-up clinical case report. Case Rep. Dent. 2015, 2015, 574676. [Google Scholar] [CrossRef]
- Aljateeli, M.; Fu, J.H.; Wang, H.L. Managing Peri-Implant Bone Loss: Current Understanding. Clin. Implant Dent. Relat. Res. 2012, 14, e109–e118. [Google Scholar] [CrossRef]
- Schwarz, F.; Sahm, N.; Bieling, K.; Becker, J. Surgical regenerative treatment of peri-implantitis lesions using a nanocrystalline hydroxyapatite or a natural bone mineral in combination with a collagen membrane: A four-year clinical follow-up report. J. Clin. Periodontol. 2009, 36, 807–814. [Google Scholar] [CrossRef]
- Claffey, N.; Clarke, E.; Polyzois, I.; Renvert, S. Surgical treatment of peri-implantitis. J. Clin. Periodontol. 2008, 35, 316–332. [Google Scholar] [CrossRef] [PubMed]
- Augthun, M.; Tinschert, J.; Huber, A. In vitro studies on the effect of cleaning methods on different implant surfaces. J. Periodontol. 1998, 69, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Louropoulou, A.; Slot, D.E.; Van der Weijden, F.A. Titanium surface alterations following the use of different mechanical instruments: A systematic review. Clin. Oral Implants Res. 2012, 23, 643–658. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Ferrari, D.; Popovski, K.; Hartig, B.; Becker, J. Influence of different air-abrasive powders on cell viability at biologically contaminated titanium dental implants surfaces. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 83–91. [Google Scholar] [CrossRef]
- Tastepe, C.S.; van Waas, R.; Liu, Y.; Wismeijer, D. Air powder abrasive treatment as an implant surface cleaning method: A literature review. Int. J. Oral Maxillofac. Implants 2012, 27, 1461–1473. [Google Scholar]
- Bergendal, T.; Forsgren, L.; Kvint, S.; Löwstedt, E. The effect of an airbrasive instrument on soft and hard tissues around osseointegrated implants. A case report. Swed. Dent. J. 1989, 14, 219–223. [Google Scholar]
- Mengel, R.; Buns, C.-E.; Mengel, C.; Flores-de-Jacoby, L. An in vitro study of the treatment of implant surfaces with different instruments. Int. J. Oral Maxillofac. Implants 1998, 13, 91–96. [Google Scholar]
- Matys, J.; Botzenhart, U.; Gedrange, T.; Dominiak, M. Thermodynamic effects after Diode and Er: YAG laser irradiation of grade IV and V titanium implants placed in bone-an ex vivo study. Preliminary report. Biomed. Tech. (Berl.) 2016, 61, 499–507. [Google Scholar] [CrossRef]
- Park, J.B.; Jang, Y.J.; Koh, M.; Choi, B.K.; Kim, K.K.; Ko, Y. In vitro analysis of the efficacy of ultrasonic scalers and a toothbrush for removing bacteria from resorbable blast material titanium disks. J. Periodontol. 2013, 84, 1191–1198. [Google Scholar] [CrossRef]
- Rühling, A.; Kocher, T.; Kreusch, J.; Plagmann, H.C. Treatment of subgingival implant surfaces with Teflon®-coated sonic and ultrasonic scaler tips and various implant curettes. An in vitro study. Clin. Oral Implants Res. 1994, 5, 19–29. [Google Scholar] [CrossRef]
- Wilson, V. An insight into peri-implantitis: A systematic literature review. Prim. Dent. Care 2013, 2, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Koka, S.; Han, J.; Razzoog, M.E.; Bloem, T.J. The effects of two air-powder abrasive prophylaxis systems on the surface of machined titanium: A pilot study. Implant Dent. 1992, 1, 259–265. [Google Scholar] [CrossRef] [PubMed]
- McCollum, J.; O’Neal, R.B.; Brennan, W.A.; Van Dyke, T.E.; Horner, J.A. The effect of titanium implant abutment surface irregularities on plaque accumulation in vivo. J. Periodontol. 1992, 63, 802–805. [Google Scholar] [CrossRef] [PubMed]
- Zablotsky, M.H.; Wittrig, E.E.; Diedrich, D.L.; Layman, D.L.; Meffert, R. MFibroblastic growth and attachment on hydroxyapatite-coated titanium surfaces following the use of various detoxification modalities. Part II: Contaminated hydroxyapatite. Implant Dent. 1992, 1, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Matys, J.; Jurczyszyn, K.; Ziółkowski, P.; Dominiak, M.; Brugnera, A.J., Jr.; Romeo, U. Histological and Thermometric Examination of Soft Tissue De-Epithelialization Using Digitally Controlled Er:YAG Laser Handpiece: An Ex Vivo Study. Photomed. Laser Surg. 2018, 36, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Romeo, U.; Russo, C.; Palaia, G.; Lo Giudice, R.; Del Vecchio, A.; Visca, P.; Migliau, G.; De Biase, A. Biopsy of different oral soft tissues lesions by KTP and diode laser: Histological evaluation. TSWJ 2014, 2014, 761704. [Google Scholar] [CrossRef]
- Romeo, U.; Del Vecchio, A.; Palata, G.; Tenore, G.; Visca, P.; Maggiore, C. Bone damage induced by different cutting instruments: An in vitro study. Braz. Dent. J. 2009, 20, 162–168. [Google Scholar] [CrossRef]
- Matys, J.; Flieger, R.; Tenore, G.; Grzech-Leśniak, K.; Romeo, U.; Dominiak, M. Er: YAG laser, piezosurgery, and surgical drill for bone decortication during orthodontic mini-implant insertion: Primary stability analysis—An animal study. Lasers Med. Sci. 2018, 33, 489–495. [Google Scholar] [CrossRef]
- Valderrama, P.; Wilson, T.G., Jr. Detoxification of implant surfaces affected by peri-implant disease: An overview of surgical methods. Int. J. Dent. 2013, 2013, 749680. [Google Scholar] [CrossRef]
- Taniguchi, Y.; Aoki, A.; Mizutani, K. Optimal Er: YAG laser irradiation parameters for debridement of microstructured fixture surfaces of titanium dental implants. Lasers Med. Sci. 2013, 28, 1057–1068. [Google Scholar] [CrossRef]
- Takasaki, A.A.; Aoki, A.; Mizutani, K.; Kikuchi, S.; Oda, S.; Ishikawa, I. Er: YAG laser therapy for peri-implant infection: A histological study. Lasers Med. Sci. 2007, 22, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Bieling, K.; Nuesry, E.; Sculean, A.; Becker, J. Clinical and histological healing pattern of peri-implantitis lesions following non-surgical treatment with an Er: YAG laser. Lasers Surg. Med. 2006, 38, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, F.; Hasan, I.; Kunert-Keil, C.; Götz, W.; Gedrange, T.; Spassov, A.; Schweppe, J.; Gredes, T. Experimental and histological investigations of the bone using two different oscillating osteotomy techniques compared with conventional rotary osteotomy. Ann. Anat. Anat. Anz. 2012, 194, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, A.R.; Albrektsson, T. Temperature threshold levels for heat-induced bone tissue injury: A vital-microscopic study in the rabbit. J. Prosthet. Dent. 1983, 50, 101–107. [Google Scholar] [CrossRef]
- Eriksson, A.R.; Albrektsson, T.; Magnusson, B. Assessment of bone viability after heat trauma. A histological, histochmeical and vital microscopic study in the rabbit. Scand. J. Plast. Reconstr. Surg. 1984, 18, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Sculean, A.; Rothamel, D.; Schwenzer, K.; Georg, T.; Becker, J. Clinical evaluation of an Er:YAG laser for nonsurgical treatment of peri-implantitis: A pilot study. Clin. Oral Implants Res. 2005, 16, 44–52. [Google Scholar] [CrossRef]
- Kreisler, M.; Al Haj, H.; d’Hoedt, B. Temperature changes at the implant-bone interface during simulated surface decontamination with an Er: YAG laser. Int. J. Prosthodont. 2002, 15, 582–587. [Google Scholar]
- Kreisler, M.; Kohnen, W.; Marinello, C.; Götz, H.; Duschner, H.; Jansen, B.; d’Hoedt, B. Bactericidal effect of the Er: YAG laser on dental implant surfaces: An in vitro study. J. Periodontol. 2002, 73, 1292–1298. [Google Scholar] [CrossRef]
- Geminiani, A.; Caton, J.G.; Romanos, G.E. Temperature increase during CO2 and Er: YAG irradiation on implant surfaces. Implant Dent. 2011, 20, 379–382. [Google Scholar] [CrossRef]
- Leja, C.; Geminiani, A.; Caton, J.; Romanos, G.E. Thermodynamic effects of laser irradiation of implants placed in bone: An in vitro study. Lasers Med. Sci. 2013, 28, 1435–1440. [Google Scholar] [CrossRef]
- Trisi, P.; Berardini, M.; Falco, A.; Vulpiani, M.P. Effect of Temperature on the Dental Implant Osseointegration Development in Low-Density Bone: An In Vivo Histological Evaluation. Implant Dent. 2015, 24, 96–100. [Google Scholar] [CrossRef]
- Cohen, O.; Gabay, E.; Machtei, E.E. Cooling profile following prosthetic preparation of 1-piece dental implants. J. Oral Implantol. 2010, 36, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Flieger, R.; Dominiak, M. Assessment of Temperature Rise and Time of Alveolar Ridge Splitting by Means of Er:YAG Laser, Piezosurgery, and Surgical Saw: An Ex Vivo Study. BioMed Res. Int. 2016, 2016, 9654975. [Google Scholar] [CrossRef] [Green Version]
- Matys, J.; Dominiak, M.; Flieger, R. Energy and Power Density: A Key Factor in Lasers Studies. J. Clin. Diagn. Res. 2015, 9, ZL01–ZL02. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Rothamel, D.; Sculean, A.; Georg, T.; Scherbaum, W.; Becker, J. Effects of an Er:YAG laser and the Vector ultrasonic system on the biocompatibility of titanium implants in cultures of human osteoblast-like cells. Clin. Oral Implants Res. 2003, 14, 784–792. [Google Scholar] [CrossRef]
- Schwarz, F.; Sculean, A.; Romanos, G.; Herten, M.; Horn, N.; Scherbaum, W.; Becker, J. Influence of different treatment approaches on the removal of early plaque biofilms and the viability of SAOS2 osteoblasts grown on titanium implants. Clin. Oral Investig. 2005, 9, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Sennhenn-Kirchner, S.; Schwarz, P.; Schliephake, H.; Konietschke, F.; Brunner, E.; Borg-von Zepelin, M. Decontamination efficacy of erbium:yttrium-aluminium-garnet and diode laser light on oral Candida albicans isolates of a 5-day in vitro biofilm model. Lasers Med. Sci. 2009, 24, 313–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sennhenn-Kirchner, S.; Klaue, S.; Wolff, N.; Mergeryan, H.; Borg von Zepelin, M.; Jacobs, H.G. Decontamination of rough titanium surfaces with diode lasers: Microbiological findings on in vivo grown biofilms. Clin. Oral Implants Res. 2007, 18, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Fontana, C.R.; Kurachi, C.; Mendonca, C.R.; Bagnato, V.S. Microbial reduction in periodontal pockets under exposition of a medium power diode laser: An experimental study in rats. Lasers Surg. Med. 2004, 35, 263–268. [Google Scholar] [CrossRef]
- Monzavi, A.; Shahabi, S.; Fekrazad, R.; Behruzi, R.; Chiniforush, N. Implant surface temperature changes during Er: YAG laser irradiation with different cooling systems. J. Dent. (Tehran) 2014, 11, 210–215. [Google Scholar]
- Kamel, M.S.; Khosa, A.; Tawse-Smith, A.; Leichter, J. The use of laser therapy for dental implant surface decontamination: A narrative review of in vitro studies. Lasers Med. Sci. 2014, 29, 1977–1985. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Hadzik, J.; Dominiak, M. Schneiderian Membrane Perforation Rate and Increase in Bone Temperature During Maxillary Sinus Floor Elevation by Means of Er: YAG Laser—An Animal Study in Pigs. Implant Dent. 2017, 26, 238–244. [Google Scholar] [CrossRef] [PubMed]





| Study Groups | Handpiece | Distance (mm) | Energy (mJ) | Frequency (Hz) | Power (W) | Spot (mm) | Fluence (J/cm2) | Time (s) | Power Density (W/cm2) | Cooling (mL) |
|---|---|---|---|---|---|---|---|---|---|---|
| G1 | Laser-in-Handpiece | contact | 50 | 30 | 1.5 | 0.8 | 9.95 | 60 | 298.5 | 30 |
| G2 | Laser-in-Handpiece | contact | 100 | 30 | 3 | 0.8 | 19.89 | 60 | 593.7 | 30 |
| G3 | Laser-in-Handpiece | contact | 200 | 30 | 6 | 0.8 | 39.79 | 60 | 1193,7 | 30 |
| G4 | Scaler | contact | - | 20 | 4 | 0.9 | - | 60 | - | 30 |
| Study Groups | Thermocouple P1∆Ta (°C) IA (I) (Mean ± SD) | Thermocouple P1∆Ta (°C) FTF (I) (Mean ± SD) | Thermocouple P1∆Ta (°C) BTF (I) (Mean ± SD) | P Value |
|---|---|---|---|---|
| Group 1 | 1.55 ± 0.55 | 1.07 ± 0.27 + | 0.86 ± 0.46 *+ | IA vs. FTF, BTF p < 0.05 FTF vs. BTF p > 0.05 |
| Group 2 | 3.62 ± 0.74 * | 4.42 ± 0.38 * | 2.37 ± 1.37 + | IA, FTF vs. BTF p < 0.01 IA vs. FTF p > 0.05 |
| Group 3 | 6.54 ± 0.96 * | 5.04 ± 0.96 *+ | 4.35 ± 0.54 *+ | IA vs. FTF, BTF p < 0.0004 FTF vs. BTF p > 0.05 |
| Group 4 | 1.15 ± 0.54 | 1.57 ± 0.27 + | 2.43 ± 0.23 + | IA vs. FTF vs. BTF p < 0.05 |
| P value | G1 vs. G2, G3 p < 0.0002 G4 vs. G2, G3 p < 0.0002 G1 vs.G4 p > 0.05 | G1 vs. G2, G3 p < 0.0002 G4 vs. G2, G3 p < 0.05 G1 vs. G4 p > 0.05 | G1 vs. G2, G3, G4 p < 0.0003 G2 vs. G3 p < 0.0002 G3 vs. G4 p < 0.0002 G2 vs. G4 p > 0.05 |
| Study Groups | Thermocouple P2∆Ta (°C) IA (A) (Mean ± SD) | Thermocouple P2∆Ta (°C) FTF (A) (Mean ± SD) | Thermocouple P2∆Ta(°C) BTF (A) (Mean ± SD) | P Value |
|---|---|---|---|---|
| Group 1 | 0.95 ± 0.55 * | 3.47 ± 0.27 *+ | 2.40 ± 0.35 + | IA vs. FTF vs. BTF p < 0.05 |
| Group 2 | 2.55 ± 0.58 | 5.50 ± 0.89 *+ | 3.12 ± 0.74 + | FTF vs. IA, BTF p < 0.0002 FTF vs. BTF p < 0.0002 |
| Group 3 | 5.86 ± 0.46 * | 7.62 ± 0.74 *+ | 10.67 ± 1.14 *+ | IA vs. FTF vs. BTF p < 0.05 |
| Group 4 | 2.00 ± 0.89 | 2.13 ± 0.23 | 2.97 ± 0.27 + | BTF vs. IA, FTF p < 0.003 FTF vs. BTF p < 0.003 IA vs. FTF p > 0.05 |
| P value | G1 vs. G2, G3, G4 p < 0.002 G2 vs. G3 p < 0.0002 G3 vs. G4 p < 0.0002 G2 vs. G4 p > 0.05 | G1 vs. G2 vs. G3 vs. G4 p < 0.0002 | G3 vs. G2, G4 p < 0.0002 G1 vs. G3 p < 0.0002 G1 vs. G2, G4 p > 0.05 G2 vs. G4 p > 0.05 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matys, J.; Romeo, U.; Mroczka, K.; Grzech-Leśniak, K.; Dominiak, M. Temperature Changes and SEM Effects of Three Different Implants-Abutment Connection during Debridement with Er:YAG Laser: An Ex Vivo Study. Materials 2019, 12, 3748. https://doi.org/10.3390/ma12223748
Matys J, Romeo U, Mroczka K, Grzech-Leśniak K, Dominiak M. Temperature Changes and SEM Effects of Three Different Implants-Abutment Connection during Debridement with Er:YAG Laser: An Ex Vivo Study. Materials. 2019; 12(22):3748. https://doi.org/10.3390/ma12223748
Chicago/Turabian StyleMatys, Jacek, Umberto Romeo, Krzysztof Mroczka, Kinga Grzech-Leśniak, and Marzena Dominiak. 2019. "Temperature Changes and SEM Effects of Three Different Implants-Abutment Connection during Debridement with Er:YAG Laser: An Ex Vivo Study" Materials 12, no. 22: 3748. https://doi.org/10.3390/ma12223748
APA StyleMatys, J., Romeo, U., Mroczka, K., Grzech-Leśniak, K., & Dominiak, M. (2019). Temperature Changes and SEM Effects of Three Different Implants-Abutment Connection during Debridement with Er:YAG Laser: An Ex Vivo Study. Materials, 12(22), 3748. https://doi.org/10.3390/ma12223748









