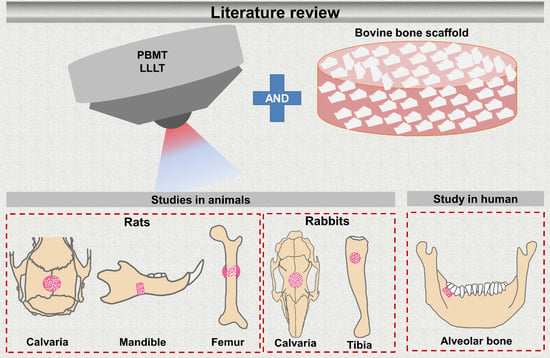
Photobiomodulation Therapy (PBMT) Applied in Bone Reconstructive Surgery Using Bovine Bone Grafts: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
- Use of bovine bone as a scaffold and PBMT in bone reconstructions;
- Human or animal studies;
- Publications in the English language only and which allowed full access to the text.
- Each included article should present data regarding: wavelength, output power, energy density, application protocol (points, frequency and days).
- Duplicate articles;
- Excluded because title was not related to aim;
- Did not use bovine bone;
- Use of other languages (not English);
- No access;
- Literature review;
- Data absence: wavelength (nm), output power (mW); energy density (J/cm2); quantity of radiation.
3. Results
3.1. Inclusion of Studies, Quality of Studies, and Test Subjects
3.2. Outcome Measures Used in the Included Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mester, E.; Szende, B.; Gartner, P. The effect of laser beams on the growth of hair in mice. Radiobiol. Radiother. 1968, 9, 621–626. [Google Scholar]
- Migliario, M.; Pittarella, P.; Fanuli, M.; Rizzi, M.; Renò, F. Laser-induced osteoblast proliferation is mediated by ROS production. Lasers Med. Sci. 2014, 29, 1463–1467. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, T.; Mitani, A.; Fukuda, M.; Mogi, M.; Osawa, K.; Takahashi, S.; Aino, M.; Iwamura, Y.; Miyajima, S.; Yamamoto, H.; et al. Irradiation with a low-level diode laser induces the developmental endothelial locus-1 gene and reduces proinflammatory cytokines in epithelial cells. Lasers Med. Sci. 2014, 29, 987–994. [Google Scholar] [CrossRef] [PubMed]
- AlGhamdi, K.; Kumar, A.; Moussa, N. Low-level laser therapy: A useful technique for enhancing the proliferation of various cultured cells. Lasers Med. Sci. 2012, 27, 237–249. [Google Scholar] [CrossRef]
- Rosso, M.; Buchaim, D.; Kawano, N.; Furlanette, G.; Pomini, K.; Buchaim, R. Photobiomodulation Therapy (PBMT) in Peripheral Nerve Regeneration: A Systematic Review. Bioengineering 2018, 5, 44. [Google Scholar] [CrossRef] [Green Version]
- Khadra, M.; Kasem, N.; Haanaes, H.; Ellingsen, J.; Lyngstadaas, S. Enhancement of bone formation in rat calvarial bone defects using low-level laser therapy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 693–700. [Google Scholar] [CrossRef]
- Angeletti, P.; Pereira, M.; Gomes, H.; Hino, C.; Ferreira, L. Effect of low-level laser therapy (GaAlAs) on bone regeneration in midpalatal anterior suture after surgically assisted rapid maxillary expansion. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e38–e46. [Google Scholar] [CrossRef]
- Morries, L.; Cassano, P.; Henderson, T. Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy. Neuropsychiatr. Dis. Treat. 2015, 20, 2159–2175. [Google Scholar]
- Pyo, S.; Song, W.; Kim, I.; Park, B.; Kim, C.; Shin, S.; Chung, I.; Kim, Y. Low-level laser therapy induces the expressions of BMP-2, osteocalcin, and TGF-β1 in hypoxic-cultured human osteoblasts. Lasers Med. Sci. 2013, 28, 543–550. [Google Scholar] [CrossRef]
- De Paiva, P.; Tomazoni, S.; Johnson, D.; Vanin, A.; Albuquerque-Pontes, G.; Machado, C.; Casalechi, H.; de Carvalho, P.; Leal-Junior, E. Photobiomodulation therapy (PBMT) and/or cryotherapy in skeletal muscle restitution, what is better? A randomized, double-blinded, placebo-controlled clinical trial. Lasers Med. Sci. 2016, 31, 1925–1933. [Google Scholar] [CrossRef]
- Rosso, M.P.D.O.; Rosa Júnior, G.M.; Buchaim, D.V.; German, I.J.S.; Pomini, K.T.; de Souza, R.G.; Pereira, M.; Favaretto Júnior, I.A.; Bueno, C.R.D.S.; Gonçalves, J.B.D.O.; et al. Stimulation of morphofunctional repair of the facial nerve with photobiomodulation, using the end-to-side technique or a new heterologous fibrin sealant. J. Photochem. Photobiol. B Biol. 2017, 175, 20–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pomini, K.; Buchaim, D.; Andreo, J.; Rosso, M.; Della Coletta, B.; German, Í.; Biguetti, A.; Shinohara, A.; Rosa Júnior, G.; Cosin Shindo, J.; et al. Fibrin sealant derived from human plasma as a scaffold for bone grafts associated with photobiomodulation therapy. Int. J. Mol. Sci. 2019, 20, 1761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brassolatti, P.; Bossini, P.; Oliveira, M.; Kido, H.; Tim, C.; Almeida-Lopes, L.; Retto Da Silva De Avó, L.; Araújo-Moreira, F.; Parizotto, N. Comparative effects of two different doses of low-level laser therapy on wound healing third-degree burns in rats. Microsc. Res. Tech. 2016, 79, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Arany, P. Craniofacial wound healing with photobiomodulation therapy: New insights and current challenges. J. Dent. Res. 2016, 95, 977–984. [Google Scholar] [CrossRef]
- de Oliveira, G.; Aroni, M.; Medeiros, M.; Marcantonio, E.; Marcantonio, R. Effect of low-level laser therapy on the healing of sites grafted with coagulum, deproteinized bovine bone, and biphasic ceramic made of hydroxyapatite and β-tricalcium phosphate. In vivo study in rats. Lasers Surg. Med. 2018, 50, 651–660. [Google Scholar] [CrossRef]
- Zhang, L.; Xing, D.; Gao, X.; Wu, S. Low-power laser irradiation promotes cell proliferation by activating PI3K/Akt pathway. J. Cell. Physiol. 2009, 219, 553–562. [Google Scholar] [CrossRef]
- Khadra, M.; Lyngstadaas, S.; Haanaes, H.; Mustafa, K. Effect of laser therapy on attachment, proliferation and differentiation of human osteoblast-like cells cultured on titanium implant material. Biomaterials 2005, 26, 3503–3509. [Google Scholar] [CrossRef]
- Lopes, C.; Pacheco, M.; Silveira, L.; Cangussú, M.; Pinheiro, A. The effect of the association of near infrared laser therapy, bone morphogenetic proteins, and guided bone regeneration on tibial fractures treated with internal rigid fixation: A Raman spectroscopic study. J. Biomed. Mater. Res. A 2010, 94, 1257–1263. [Google Scholar] [CrossRef]
- Aykol, G.; Baser, U.; Maden, I.; Kazak, Z.; Onan, U.; Tanrikulu-Kucuk, S.; Ademoglu, E.; Issever, H.; Yalcin, F. The Effect of Low-Level Laser Therapy as an Adjunct to Non-Surgical Periodontal Treatment. J. Periodontol. 2011, 82, 481–488. [Google Scholar] [CrossRef]
- Kim, Y.; Song, W.; Kim, S.; Kim, G.; Hwang, D.; Shin, S.; Kim, U.; Kim, J.; Chung, I. Expression of receptor activator of nuclear factor -κB ligand, receptor activator of nuclear factor -κB, and osteoprotegerin, following low-level laser treatment on deproteinized bovine bone graft in rats. Lasers Med. Sci. 2009, 24, 577–584. [Google Scholar] [CrossRef]
- Da Silva, J.P.; da Silva, M.A.; Almeida, A.P.; Lombardi Junior, I.; Matos, A.P. Laser therapy in the tissue repair process: A literature review. Photomed. Laser Surg. 2010, 28, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Cunha, M.; Esper, L.; Sbrana, M.; Oliveira, P.; Valle, A.; Almeida, A. Effect of Low-Level Laser on Bone Defects Treated with Bovine or Autogenous Bone Grafts: In Vivo Study in Rat Calvaria. BioMed Res. Int. 2014, 2014, 104230. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.; de Magalhães Júnior, E.; Magalhães, C.; Ferreira, C.; Marques, A.; Pinheiro, A. New bone formation around implants inserted on autologous and xenografts irradiated or not with IR laser light: A histomorphometric study in rabbits. Braz. Dent. J. 2013, 24, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Basso, F.; Turrioni, A.; Soares, D.; Bagnato, V.; Hebling, J.; de Souza Costa, C. Low-level laser therapy for osteonecrotic lesions: Effects on osteoblasts treated with zoledronic acid. Support. Care Cancer 2014, 22, 2741–2748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yildirimturk, S.; Sirin, Y.; Soluk Tekkesin, M.; Gurler, G.; Firat, D. The effects of low-level laser therapy on the healing of bone defects in streptozotocin-induced diabetic rats: A histological and morphometric evaluation. J. Cosmet. Laser Ther. 2017, 19, 397–403. [Google Scholar] [CrossRef]
- Leja, C.; Geminiani, A.; Caton, J.; Romanos, G. Thermodynamic effects of laser irradiation of implants placed in bone: An in vitro study. Lasers Med. Sci. 2013, 28, 1435–1440. [Google Scholar] [CrossRef]
- Caran, E.; Barone, T.; Barone, J.; Lopes, N.; Alves, M.; França, C. Facial reconstruction surgery 10 years after treatment for hemangiopericytoma: Planning considerations and clinical outcomes. J. Cosmet. Laser Ther. 2014, 16, 201–204. [Google Scholar] [CrossRef]
- Malard, O.; Espitalier, F.; Bordure, P.; Daculsi, G.; Weiss, G.; Corre, P. Biomaterials for tissue reconstruction and bone substitution of the ear, nose and throat, face and neck. Expert Rev. Med. Devices 2007, 4, 729–739. [Google Scholar] [CrossRef]
- Orsi, P.; Landim-Alvarenga, F.; Justulin, L.; Kaneno, R.; De Assis Golim, M.; Dos Santos, D.; Creste, C.; Oba, E.; Maia, L.; Barraviera, B.; et al. A unique heterologous fibrin sealant (HFS) as a candidate biological scaffold for mesenchymal stem cells in osteoporotic rats. Stem Cell Res. Ther. 2017, 8, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Lienemann, P.; Metzger, S.; Kiveliö, A.; Blanc, A.; Papageorgiou, P.; Astolfo, A.; Pinzer, B.; Cinelli, P.; Weber, F.; Schibli, R.; et al. Longitudinal in vivo evaluation of bone regeneration by combined measurement of multi-pinhole SPECT and micro-CT for tissue engineering. Sci. Rep. 2015, 5, 10238. [Google Scholar] [CrossRef] [Green Version]
- Buchaim, R.; Rosso, M.; Andreo, J.; Buchaim, D.; Okamoto, R.; Rodrigues, A.; Shinohara, A.; Roque, J.; Roque, D.; Rosa Junior, G.; et al. A New Anionic Bovine Tendon as Scaffold for the Repair of Bone Defects: A Morphological, Histomorphometric and Immunohistochemical Study A New Anionic Bovine Tendon as Scaffold for the Repair of Bone Defects: A Morphological, Histomorphometric and Imm. Br. J. Med. Med. Res. 2015, 10, 1–11. [Google Scholar] [CrossRef]
- Fellah, B.; Gauthier, O.; Weiss, P.; Chappard, D.; Layrolle, P. Osteogenicity of biphasic calcium phosphate ceramics and bone autograft in a goat model. Biomaterials 2008, 29, 1177–1188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasouli Ghahroudi, A.; Rokn, A.; Kalhori, K.; Khorsand, A.; Pournabi, A.; Pinheiro, A.; Fekrazad, R. Effect of low-level laser therapy irradiation and Bio-Oss graft material on the osteogenesis process in rabbit calvarium defects: A double blind experimental study. Lasers Med. Sci. 2014, 29, 925–932. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.; Cruess, R. Bone and cartilage transplantation surgery. J. Bone Jt. Surg. Am. 1982, 64, 270–279. [Google Scholar] [CrossRef]
- Stauropoulos, A.; Kostopoulos, L.; Nyengaard, J.; Karring, T. Deproteinized bovine bone (Bio-Oss) and bio active glass (Biogram) arrest bone formation when used as an adjust to guided tissue regeneration (GTR): An experimental study in the rat. J. Clin. Periodontol. 2003, 7, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, S. Low Level Laser Therapy in the Treatment of Intra-Osseous Defect- A Case Report. J. Clin. Diagn. Res. 2016, 10, 10–12. [Google Scholar] [CrossRef]
- Havlucu, U.; Bölükbaşı, N.; Yeniyol, S.; Çetin, Ş.; Özdemir, T. Effects of Light-Emitting Diode Photobiomodulation Therapy and BioOss as Single and Combined Treatment in an Experimental Model of Bone Defect Healing in Rats. J. Oral Implantol. 2014, 41, e110–e117. [Google Scholar] [CrossRef]
- Fernández-Bodereau, E.; Dedossi, G.; Asencio, V.; Fernández-Domínguez, M.; Gehrke, S.; Aragoneses, J.; Calvo-Guirado, J. Comparison of different bone filling materials and resorbable membranes by means of micro-tomography. A preliminary study in Rabbits. Materials 2019, 12, 1197. [Google Scholar] [CrossRef] [Green Version]
- Leventis, M.; Fairbairn, P.; Mangham, C.; Galanos, A.; Vasiliadis, O.; Papavasileiou, D.; Horowitz, R. Bone healing in rabbit calvaria defects using a synthetic bone substitute: A histological and micro-CT comparative study. Materials 2018, 11, 4. [Google Scholar] [CrossRef] [Green Version]
- Pomini, K.T.; Andreo, J.C.; De Rodrigues, A.C.; De Gonçalves, J.B.O.; Daré, L.R.; German, I.J.S.; Rosa, G.M., Jr.; Buchaim, R.L. Effect of low-intensity pulsed ultrasound on bone regeneration biochemical and radiologic analyses. J. Ultrasound Med. 2014, 33, 713–717. [Google Scholar] [CrossRef] [Green Version]
- Santos, C.; Pimenta, C.; Nobre, M. A estratégia PICO para a construção da pergunta de pesquisa e busca de evidências. Rev. Lat. Am. Enferm. 2007, 15, 508–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liberati, A.; Altman, D.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.; Ioannidis, J.; Clarke, M.; Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Santinoni, C. dos S.; Oliveira, H.F.F.; Batista, V.E. de S.; Lemos, C.A.A.; Verri, F.R. Influence of low-level laser therapy on the healing of human bone maxillofacial defects: A systematic review. J. Photochem. Photobiol. B Biol. 2017, 169, 83–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. referred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Luca, R.; Todea, C.; Duma, V.; Bradu, A.; Podoleanu, Ag. Quantitative assessment of rat bone regeneration using complex master-slave optical coherence tomography. Quant. Imaging Med. Surg. 2019, 9, 782–798. [Google Scholar] [CrossRef]
- Gerbi, M.; Miranda, J.; De Arruda, J.; Moreno, L.; Carneiro, V.; Brasilino, N.; Menezes, R.; Brugnera, A.; Pinheiro, A. Photobiomodulation Therapy in Bone Repair Associated with Bone Morphogenetic Proteins and Guided Bone Regeneration: A Histomorphometric Study. Photomed. Laser Surg. 2018, 36, 581–588. [Google Scholar] [CrossRef]
- Bosco, A.; Faleiros, P.; Carmona, L.; Garcia, V.; Theodoro, L.; de Araujo, N.; Nagata, M.; de Almeida, J. Effects of low-level laser therapy on bone healing of critical-size defects treated with bovine bone graft. J. Photochem. Photobiol. B Biol. 2016, 163, 303–310. [Google Scholar] [CrossRef]
- Gerbi, M.; Marques, A.; Ramalho, L.; Ponzi, E.; Carvalho, C.; Santos, R.; Oliveira, P.C.; Nóia, M.; Pinheiro, A.L.B. Infrared laser light further improves bone healing when associated with bone morphogenic proteins: An in vivo study in a rodent model. Photomed. Laser Surg. 2008, 26, 55–60. [Google Scholar] [CrossRef]
- Márquez Martínez, M.; Pinheiro, A.; Ramalho, L. Effect of IR laser photobiomodulation on the repair of bone defects grafted with organic bovine bone. Lasers Med. Sci. 2008, 23, 313–317. [Google Scholar] [CrossRef]
- Pinheiro, A.; Gerbi, M.; Ponzi, E.; Ramalho, L.; Marques, A.; Carvalho, C.; Santos, R.; Oliveira, P.; Nóia, M. Infrared laser light further improves bone healing when associated with bone morphogenetic proteins and guided bone regeneration: An in vivo study in a rodent model. Photomed. Laser Surg. 2008, 26, 167–174. [Google Scholar] [CrossRef]
- Marquez de Martinez Gerbi, M.; Barbosa Pinheiro, A.; de Assis Limeira, F., Jr.; Marzola, C.; Pedreira Ramalho, L.; Arruda Carneiro Ponzi, E.; Olveira Soares, A.; Bandeira de Carvalho, L.; Vieira Lima, H.; Oliveira Goncalves, T.; et al. Assessment of bone repair associated to the use of organic bovine bone and membrane irradiated with 830nm. Lasers Dent. IX 2003, 4950, 156. [Google Scholar]
- de Assis Limeira, F., Jr.; Barbosa Pinheiro, A.; Marquez de Martinez Gerbi, M.; Pedreira Ramalho, L.; Marzola, C.; Carneiro Ponzi, E.; Soares, A.; Bandeira de Carvalho, L.; Vieira Lima, H.; Oliveira Gon‡alves, T.; et al. Assessment of bone repair following the use of anorganic bone graft and membrane associated or not to 830-nm laser light. Lasers Dent. IX 2003, 4950, 30. [Google Scholar]
- Pinheiro, A.; Limeira Júnior, F.; Gerbi, M.; Ramalho, L.; Marzola, C.; Ponzi, E. Effect of low level laser therapy on the repair of bone defects grafted with inorganic bovine bone. Braz. Dent. J. 2003, 14, 177–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinheiro, A.; Limeira, F.; Gerbi, M.; Ramalho, L.; Marzola, C.; Ponzi, E.; Soares, A.; De Carvalho, L.; Lima, H.; Gonçalves, T. Effect of 830-nm Laser Light on the Repair of Bone Defects Grafted with Inorganic Bovine Bone and Decalcified Cortical Osseous Membrane. J. Clin. Laser Med. Surg. 2003, 21, 383–388. [Google Scholar] [CrossRef]
- Zhang, K.; Wang, S.; Zhou, C.; Cheng, L.; Gao, X.; Xie, X.; Sun, J.; Wang, H.; Weir, M.D.; Reynolds, M.A.; et al. Advanced smart biomaterials and constructs for hard tissue engineering and regeneration. Bone Res. 2018, 6. [Google Scholar] [CrossRef]
- Henkel, J.; Woodruff, M.; Epari, D.; Steck, R.; Glatt, V.; Dickinson, I.; Choong, P.; Schuetz, M.; Hutmacher, D. Bone Regeneration Based on Tissue Engineering Conceptions—A 21st Century Perspective. Nat. Publ. Gr. 2013, 1, 216–248. [Google Scholar] [CrossRef] [Green Version]
- Rocha, L.; Goissis, G.; Rossi, M. Biocompatibility of anionic collagen matrix as scaffold for bone healing. Biomaterials 2002, 23, 449–456. [Google Scholar] [CrossRef]
- Gomes, P.; Fernandes, M. Rodent models in bone-related research: The relevance of calvarial defects in the assessment of bone regeneration strategies. Lab. Anim. 2011, 45, 14–24. [Google Scholar] [CrossRef]
- Li, Y.; Chen, S.; Li, L.; Qin, L.; Wang, X.; Lai, Y. Bone defect animal models for testing efficacy of bone substitute biomaterials. J. Orthop. Transl. 2015, 3, 95–104. [Google Scholar] [CrossRef] [Green Version]
- Venken, K.; Calleweart, F.; Boonem, S.; Vanderschueren, D. Sex hormones, their conseptors and bone health. Osteoporos. Int. 2008, 19, 1517–1525. [Google Scholar] [CrossRef]
- Oury, F. A crosstalk between bone and gonads. Ann. N. Y. Acad. Sci. 2012, 1260, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Fernandez de Grado, G.; Keller, L.; Idoux-Gillet, Y.; Wagner, Q.; Musset, A.; Benkirane-Jessel, N.; Bornert, F.; Offner, D. Bone substitutes: A review of their characteristics, clinical use, and perspectives for large bone defects management. J. Tissue Eng. 2018, 9, 2041731418776819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cardaropoli, G.; Araujo, M.; Hayacibara, R.; Sukekava, F.; Lindhe, J. Healing of extraction sockets and surgically produced—Augmented and non-augmented—Defects in the alveolar ridge. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Obradovic, R.; Kesic, L.; Pesevska, S. Influence of low-level laser therapy on biomaterial osseointegration: A mini-review. Lasers Med. Sci. 2009, 24, 447–451. [Google Scholar] [CrossRef]
- Marques, L.; Holgado, L.A.; Francischone, L.A.; Ximenez, J.P.B.; Okamoto, R.; Kinoshita, A. New LLLT protocol to speed up the bone healing process—Histometric and immunohistochemical analysis in rat calvarial bone defect. Lasers Med. Sci. 2015, 30, 1225–1230. [Google Scholar] [CrossRef]
- Pinheiro, A.; Gerbi, M. Photoengineering of bone repair processes. Photomed. Laser Surg. 2006, 24, 47–49. [Google Scholar] [CrossRef]
- Vladimirov, Y.; Osipov, A.; Klebanov, G. Photobiological principles of therapeutic applications of laser radiation. Biochemistry 2004, 69, 81–90. [Google Scholar] [CrossRef]
- Brugnera, A.; dos Santos, A.; Bologna, E.; Ladalardo, T. Atlas of Applied Laser Therapy to Clinical Dentistry.; Quintessence Editoria LTDA: São Paulo, Brazil, 2006. [Google Scholar]
- Rabie, A.; Chay, S. Clinical applications of composite intramembranous bone grafts. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 375–383. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, S.; Hwang, D.; Kim, S.; Kwon, Y.; Shin, S.; Kim, U.; Kim, J.; Chung, I. Effect of low-level laser treatment after installation of dental titanium implant-immunohistochemical study of RANKL, RANK, OPG: An experimental study in rats. Lasers Surg. Med. 2007, 39, 441–450. [Google Scholar] [CrossRef]
- Basford, J. Low intensity laser therapy: Still not an established clinical tool. Lasers Surg. Med. 1995, 16, 331–342. [Google Scholar] [CrossRef]
- Torroni, A.; Marianetti, T.; Romandini, M.; Gasparini, G.; Cervelli, D.; Pelo, S. Mandibular reconstruction with different techniques. J. Craniofac. Surg. 2015, 26, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Scheyer, E.; Heard, R.; Janakievski, J.; Mandelaris, G.; Nevins, M.; Pickering, S.; Richardson, C.; Pope, B.; Toback, G.; Velásquez, D.; et al. A randomized, controlled, multicentre clinical trial of post-extraction alveolar ridge preservation. J. Clin. Periodontol. 2016, 43, 1188–1199. [Google Scholar] [CrossRef] [PubMed]




| Authors | Type of Laser (Manufacturer) | Wavelength (nm)/Spot Beam (cm2) | Output Power (mW) | Energy Density (J/cm2) | Quantity of Radiation | Bovine Bone | Therapeutic Variables | Irradiation Site (Defect) | Evaluation Time | Outcome Measures |
|---|---|---|---|---|---|---|---|---|---|---|
| Luca et al., 2019 [45] | GaAlAs (IRRADIA Mid-Laser Stockholm, Suécia) | 808/- | 450 Frequen-cy of 3800 Hz | 2/1.9 J per session | 4 points around the defect plus 1 central point. 17 s/point. Started IP, repeated every 48 h, until the established sacrifice day. | BBG | CM | Rat calvaria (5 mm Ø) | 14, 21 and 30 days post-surgery. | By CMS/SS-OCT quantitative analysis in 30 days, BBG + PBMT with higher volume bone formation (27.11%, p ≤ 0.05). Histological analysis (by MT) shows new bone around the particles, osteoid lamellae delimited by osteoblasts. |
| Pomini et al., 2019 [12] | GaAlAs (Laserpulse IBRAMED, Amparo, SP, Brazil) | 830/0.11 | 30 | 6 | 4 points in contact area, 24 s/point. Started IP, repeated every 48 h, three times a week until euthanasia. | DBBm | FS | Rat calvaria (8 mm Ø) | 14 and 42 days post-surgery. | Histomorphometric analysis quantified higher bone volume density between both periods (5.6 to 10.64, p < 0.05) for the FS + DBBm + PBMT group and presence of the particles seen in the µCT. In the histological analysis (HE), the new bone started from the defect edges and there was more evidence of trabecular formation in the irradiated group FS + DBBm. Association of PBMT with xenograft and fibrin sealant had beneficial effects on bone repair. |
| Gerbi et al., 2018 [46] | GaAlAs (Thera Lase Surgery; DMC Equipamentos, São Carlos, SP, Brazil) | 830/0.28 | 40 | 4 | 4 points applied in contact around the defect and was repeated every other day for 15 days, total of 7 sessions. | OmB | BMP + collagen Binder + bovine biological membrane | Rat femur (3mm Ø) | 15 and 30 days post-surgery. | By histomorphometric analysis the OmB + PBMT group exhibited a larger area of newly formed bone tissue (21.11%, p < 0.05), demonstrating the efficacy of bone photobiomodulation in 30 days. Picrosirus and HE analysis show trabecular bone and complete cortical repair. |
| de Oliveira et al., 2018 [15] | GaAlAs (Therapy XT, DMC São Carlos-SP, Brazil) | 808/0.02 | 100 | 354/ point Total energy 28 J | 4 points in contact area, 10 s/point. Started IP, repeated every 48 h for 13 days, 7 sessions in total. | DBB | HA/βTCP + Teflo capsule, peripheral ring | Rat mandibular branch (Four holes of 0.5 mm Ø were made 6 mm from each other to form the edges of a square, the region was scarified). | 30, 60 and 90 days post-surgery | Quantitative analysis by µCT: 90 days, higher PBMT effect on the amount of mineralized tissue associated with DBB (±63%, p ≤ 0.05) compared to non-biostimulated groups. Histomorphometry showed greater amount of new bone in the DBB + PBMT group (±25%, p ≤ 0.05). Lower amount of biomaterial in the PBMT, DBB (±30%, p ≤ 0.05). Immunohistochemi-cal analysis showed increased ALP in the irradiated DBB (45%, p < 0.05) group. |
| Bosco et al., 2016 [47] | GaAlAs (Bio Wave; Kondortech Equipment Ltd., São Carlos-SP, Brazil) | 660/0.07 | 35 | 30.85/ point total energy of 19.44 J | 8 points in contact area plus 1 central point in the scanning procedure. 72 s/point, 1 application IP. | IBBG | - | Rat calvaria (10 mm Ø) | 30 and 60 days post-surgery | Histomorphometric analysis showed that the IBBG/PBMT group had the largest newly formed bone area (7.39 to 9.44, p < 0.05), and histological analysis (HE) showed a large osteoid matrix area, osteoblasts and newly formed bone around the particles at 60 days. No statistical difference for particle resorption at 30 (21.98 ± 4.10) and 60 (27.20 ± 6.39) days. PBMT can improve bone formation, but did not speed up the resorption of biomaterial particles. |
| Cunha et al., 2014 [22] | GaAlAs (Thera Lase DMC São Carlos-SP, Brazil) | 780/0.05 | 100 | 210 6J per point | 4 points in contact area plus 1 central point, 60 s/point. Application IP. | IBBG | - | Rat calvaria (5 mm Ø) | 30 days post-surgery | Histomorphometric analysis showed that the group (IBBG + PBMT) presented the largest area of bone neoformation with 48.57% (p < 0.05) and smallest area of remaining particles (16.74%, p < 0.05). In the histological analysis (HE) presence of osteoid matrix with bone formation leading to the center of the defect, and parallel collagen fibers around the particles. PBMT benefited bone healing and particle resorption. |
| Havlucu et al., 2014 [37] | LED OsseoPulse (Biolux Research Ltd, Vancouver, Canada) | 618/- | 20 mW/cm2 | 24 total/ session | 20 min of total application in contact with the area. Started 24 h after surgery and followed in this interval for 7, 14 and 21 days. | DBB | - | Rat femur (two defects of 3 mm Ø each) | 8, 15 and 22 days post-surgery | By histomorphometric analysis in the DBB + PBMT group, all animals presented new bone tissue average >60% (p < 0.01), less inflammation (<30%, p < 0.01) and remaining particles less than 30%, p < 0.05) at 3 weeks. Histologically (HE), newly formed bone trabeculae with active osteoblasts were around the particles and reconstructed the defect. |
| Rasouli Ghahroudi et al., 2014 [33] | Diode laser (Giga com, China) | 810/- | 300 | 4 | Applied around the surgical area IP and followed by ten applications (every other day) for the next 20 days. | IBB | - | Rabbit calvaria (Four defects 8 mm Ø each) | 28 and 56 days post-surgery | A histomorphometric group of DBB + PBMT group had the highest mean of new bone formation, 41.83 and 47% at weeks 4 and 8, respectively, with statistically significant differences (p < 0.05) and an inflammation index <25% in 66.7% of the animals. Coinciding with the bone tissue presented in histology (HE), altering the auxiliary PBMT in bone healing. |
| Lopes et al., 2010 [18] | Diode Laser Unit, (Kondortech, São Carlos-SP, Brazil) | 790/0.5 | 40 | 4/point | 4 points applied transcutaneously around the area. Started IP, repeated every 48 h, per 15 days | LOBB | IRF + Biomaterial (LOBB + Collagen + BMP + Decalcified cortical osseous membrane) | Rabbit tibia (complete bone fracture, 5 mm) | 30 days post-surgery | Raman spectroscopy demonstrated that biomaterial associated PBMT was effective in improving bone healing due to increased CHA levels. Highest group average IRF + biomaterial + PBMT (9316%, p = 0.05). PBMT was effective in improving bone healing. |
| Kim et al., 2009 [20] | GaAlAs (500DPSS, LVI Technology, Seoul, Korea) | 808/0.01 | 96 power density of 830 mW/cm2 | 8.3/point | 3 points applied in contact, 10 s/point. Started IP, repeated every 24 h, per 7 days. | DBB | - | Rat calvaria (2.7 mm Ø) | 7, 14 and 21 days post-surgery. | The results of immunohistochemical analysis showed that RANKL expression (>50%, p = 0.199), OPG expression (>75%, p = 0.035) and RANK expression (<50%, p = 0.020) in the experimental group had a significant increase from 7 to 21 days. At 21 days of expression in osteoid formation and bone density in histology (Goldner’s trichrome). |
| Gerbi et al., 2008 [48] | Thera Lase, DMC Equipamentos, São Carlos, SP, Brazil | 830/0.28 | 40 | 4/point | 4 points applied in contact around the defect, begun immediately after suturing and was repeated every other day, for 15 days. | OLDBB | Biomaterial (OLDBB + collagen gel + BMP) | Rat femur (2 mm Ø) | 15, 21 and 30 days post-surgery. | Qualitative analysis (HE and Sirius red) showed an increased collagen fibers (at 15 and 21 days) and amount of well-organized bone trabeculae at 30 days in laser irradiated animals. PBMT associated with biomaterial showed positive biomodulatory. effects. |
| Márquez Martínez et al., 2008 [49] | Thera Lase, DMC Equipamentos/São Carlos, SP, Brazil, | 830/0.28 | 40 | 4/point | 4 points applied in contact around the defect and was repeated every other day, for 2 weeks. | OBB | - | Rat femur (3 mm2 cavity) | 15, 21 and 30 days post-surgery. | Qualitative analysis (HE and Picrosirus) at 30 days—higher amount of collagen fibers, evident osteoblastic activity and mature bone formation, with complete repair of the defect in group OBB + PBMT. |
| Pinheiro et al., 2008 [50] | DMC Equipamentos, São Carlos, SP, Brazil | 830/0.28 | 40 | 4/point | 4 points applied in contact around the defect and was repeated every other day, for 15 days. | OLDBB | Biomaterials (Collagen gel + BMP + bone resorbable decalcified cortical bone membrane) | Rat femur (2 mm2 cavity) | 15, 21 and 30 days post-surgery. | Qualitative analysis (HE and Sirus red) showed that biomaterials + membrane-associated PBMT developed collagen fibers, accelerated cortical bone repair, and developed the Haversian system. |
| Marquez de Martinez Gerbi et al., 2003 [51] | DMC Equipamentos, São Carlos, SP, Brazil | 830/0.28 | 40 | 4/point | 4 points applied in contact around the defect and was repeated every other day, for 15 days, total of 7 sessions. | OBB | Decalcified cortical osseous membrane | Rat femur (3mm2 cavity) | 15, 21 and 30 days post-surgery. | Qualitative histological analysis (HE and Picrosirus) showed positive effect of PBMT at 15 days with evident amounts of collagen fibers, osteoblastic activity and evident bone neoformation and complete repair of the defect. Positive effects of PBMT independent of organic bone or membrane. |
| de Assis Limeira Júnior et al., 2003 [52] | Thera Lase, DMC Equipamentos, São Carlos, SP, Brazil | 830/0.28 | 40 | 4/point | 4 points applied in contact around the defect and was repeated every other day for 15 days, total of 7 sessions. | IBB | Decalcified bovine cortical osseous membrane | Rat femur (3mm2 cavity) | 15, 21 and 30 days post-surgery. | Qualitative analysis (HE and Picrosirius) showed that the level of bone neoformation did not change much until day 30 in most groups except for the PBMT + IBB + membrane group, where bone neoformation was most evident between days 21 and 30, with dense and well organized neoformed bone trabeculae and the conclusion of cortical repair. |
| Pinheiro et al., 2003 [53] | Thera Lase, DMC Equipamentos, São Carlos, SP, Brazil | 830/0.28 | 40 | 4/point | 4 points applied transcutaneouslyStarted IP, repeated every 48 h, total of 7 sessions. | IBB | - | Rat femur (3mm2 cavity) | 15, 21 and 30 days post-surgery. | Histological qualitative analysis (HE and Picrosirius) showed that IBB + PBMT at 21 days obtained increased amount of bone neoformation and collagen fibers around the graft. At 30 days still presence of dense collagen fiber graft. PBMT had beneficial effects associated with inorganic bovine bone. |
| Pinheiro et al., 2003 [54] | Thera Lase, DMC Equipamentos, São Carlos, SP, Brazil | 830/0.28 | 40 | 4 | 4 points applied transcutaneously Started IP, repeated every 48 h, total of 7 sessions. | IBB | Decalcified cortical osseous membrane | Rat femur (3mm2 cavity) | 15, 21 and 30 days post-surgery. | Histological qualitative analysis (HE and Picrosirius) showed that at 30 days IBB + membrane + PBMT there was more pronounced, well-organized bone formation with dense trabeculae around the graft particles, the cortical repair was complete. All groups irradiated with more collagen fibers. PBMT accelerated bone repair. |
| Authors | Type of Laser (Manufacturer) | Wavelength (nm)/Spot Beam (cm2) | Output Power (mW) | Energy Density (J/cm2) | Quantity of Radiation | Bovine Bone | Irradiation Site | Evaluation Time | Outcome Measures |
|---|---|---|---|---|---|---|---|---|---|
| Bhardwaj, 2016 [36] | GaAlAs | 810/- | 100 | 4/point | 5 min in contact with the internal margins of the flap and then 10 min without contact on the defect. Application for 5 days consecutively (outer surfaces of buccal and lingual flaps) | DBM | Treatment of intraosseous defects. Alveolar bone between 44 and 45. | 30, 60 and 90 days post-surgery | By radiological measurement PBMT + DBM showed good results in clinical insertion level (CAL) gain of 4 mm, linear bone gain of 2.5 mm, bone filling of 37% and reduction of defect angle from 68° to 32°, showing a positive treatment result. Safe treatment to approach periodontal regeneration. |
| Authors | Quantitative Analyzis | Measurements Results |
|---|---|---|
| Luca et al., 2019 [45] | CMS/SS-OCT | Bone volume formation: 27.11% |
| Pomini et al., 2019 [12] | Histomorphometric | Bone volume density: 10.64% |
| Gerbi et al., 2018 [46] | Histomorphometric | Bone volume density: 21.11% |
| de Oliveira et al., 2018 [15] | HistomorphometricµCT Immunohistochemistry | Bone volume density: ±25% Mineralized tissue: ±63% ALP (45%) |
| Bosco et al., 2016 [47] | Histomorphometric | Bone volume density: 9.44% |
| Cunha et al., 2014 [22] | Histomorphometric | Bone volume density: 48.57% |
| Havlucu et al., 2014 [37] | Histomorphometric Histopathological | Bone volume density: >60% Inflammation: <30% |
| Ghahroudi et al., 2014 [33] | Histomorphometric Histopathological | Bone volume density: 47% Inflammation: <30% |
| Lopes et al., 2010 [18] | Raman spectroscopy | CHA level: 9316% |
| Kim et al., 2009 [20] | Immunohistochemistry | RANKL (>50%), OPG (>75%), RANK (<50%) |
| Bhardwaj, 2016 [36] | Radiological for CAL | Linear bone gain: 2.5 mm and reduction of defect angle: 32° |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosso, M.P.d.O.; Buchaim, D.V.; Pomini, K.T.; Coletta, B.B.D.; Reis, C.H.B.; Pilon, J.P.G.; Duarte Júnior, G.; Buchaim, R.L. Photobiomodulation Therapy (PBMT) Applied in Bone Reconstructive Surgery Using Bovine Bone Grafts: A Systematic Review. Materials 2019, 12, 4051. https://doi.org/10.3390/ma12244051
Rosso MPdO, Buchaim DV, Pomini KT, Coletta BBD, Reis CHB, Pilon JPG, Duarte Júnior G, Buchaim RL. Photobiomodulation Therapy (PBMT) Applied in Bone Reconstructive Surgery Using Bovine Bone Grafts: A Systematic Review. Materials. 2019; 12(24):4051. https://doi.org/10.3390/ma12244051
Chicago/Turabian StyleRosso, Marcelie Priscila de Oliveira, Daniela Vieira Buchaim, Karina Torres Pomini, Bruna Botteon Della Coletta, Carlos Henrique Bertoni Reis, João Paulo Galletti Pilon, Getúlio Duarte Júnior, and Rogério Leone Buchaim. 2019. "Photobiomodulation Therapy (PBMT) Applied in Bone Reconstructive Surgery Using Bovine Bone Grafts: A Systematic Review" Materials 12, no. 24: 4051. https://doi.org/10.3390/ma12244051
APA StyleRosso, M. P. d. O., Buchaim, D. V., Pomini, K. T., Coletta, B. B. D., Reis, C. H. B., Pilon, J. P. G., Duarte Júnior, G., & Buchaim, R. L. (2019). Photobiomodulation Therapy (PBMT) Applied in Bone Reconstructive Surgery Using Bovine Bone Grafts: A Systematic Review. Materials, 12(24), 4051. https://doi.org/10.3390/ma12244051