Strength–Durability Correlation of Osteosynthesis Devices Made by 3D Layer Manufacturing
Abstract
1. Introduction
2. Materials and Methods
2.1. Test Samples
2.2. Bending Test of Osteosynthesis Devices
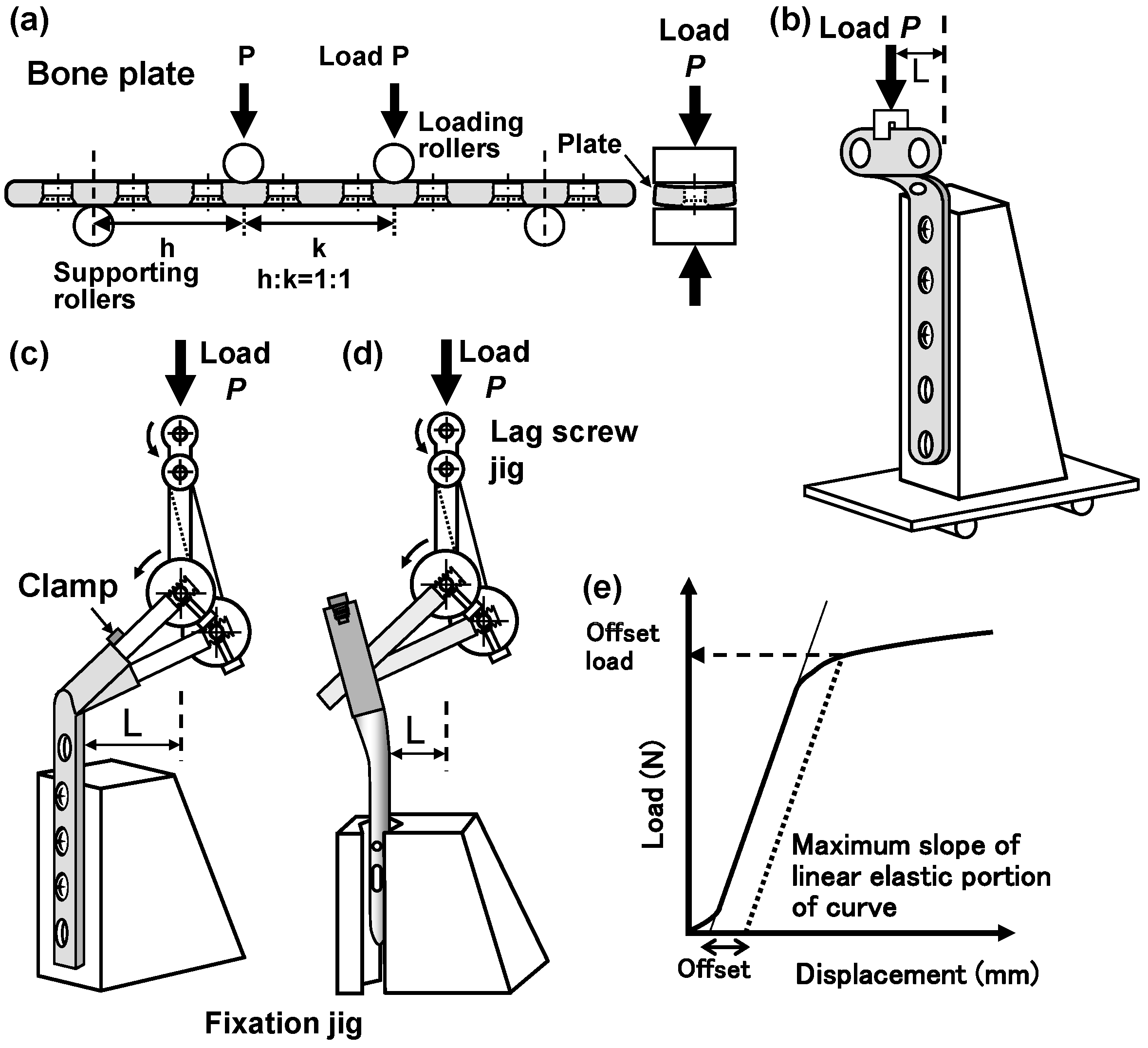
2.2.1. Four-Point Bending Tests
2.2.2. Compression Bending Tests
2.3. Durability Tests of Osteosynthesis Devices
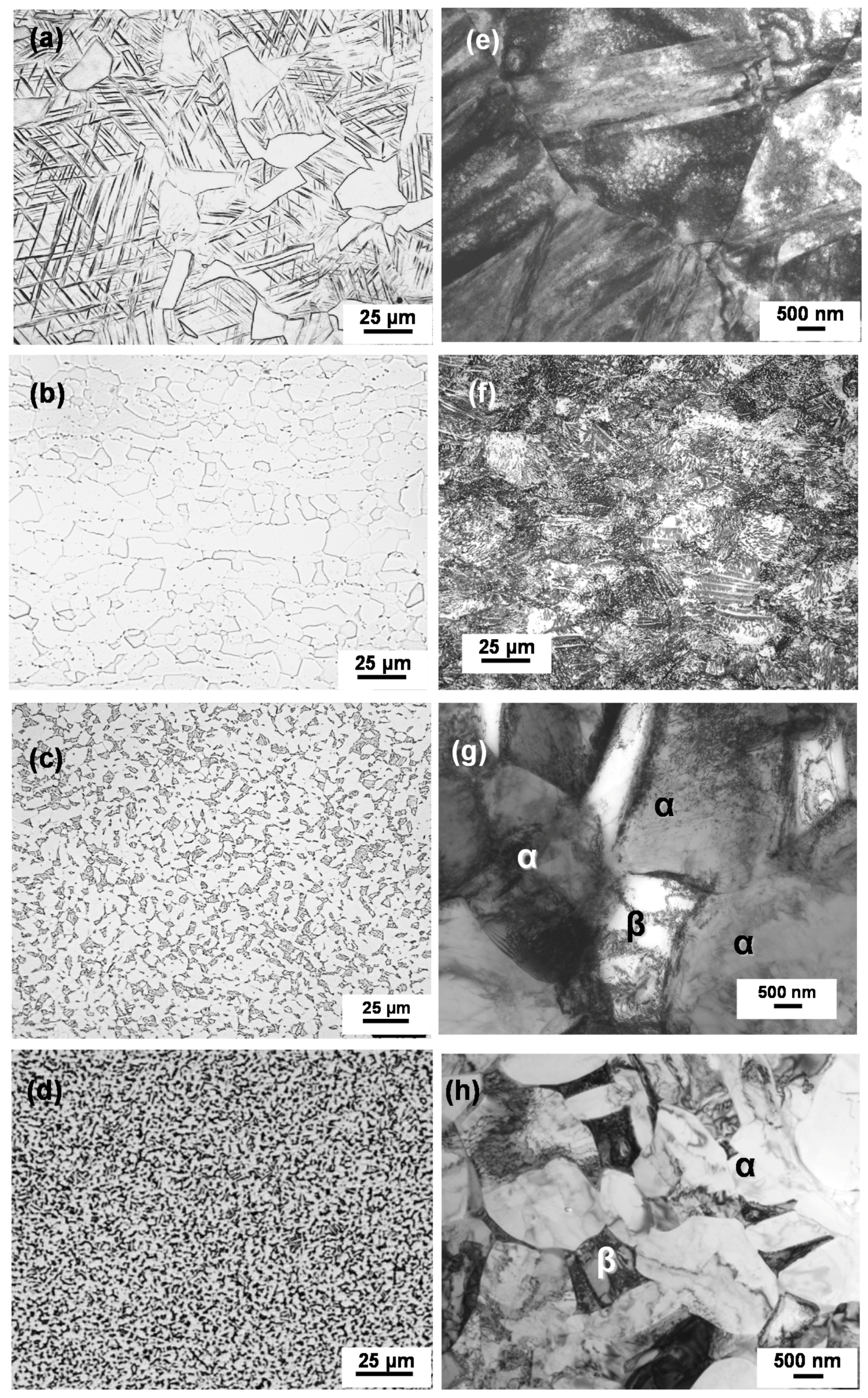
2.4. Room-Temperature Tensile Test and Microstructural Observation
2.5. Statistical Analysis
3. Experimental Results and Discussion
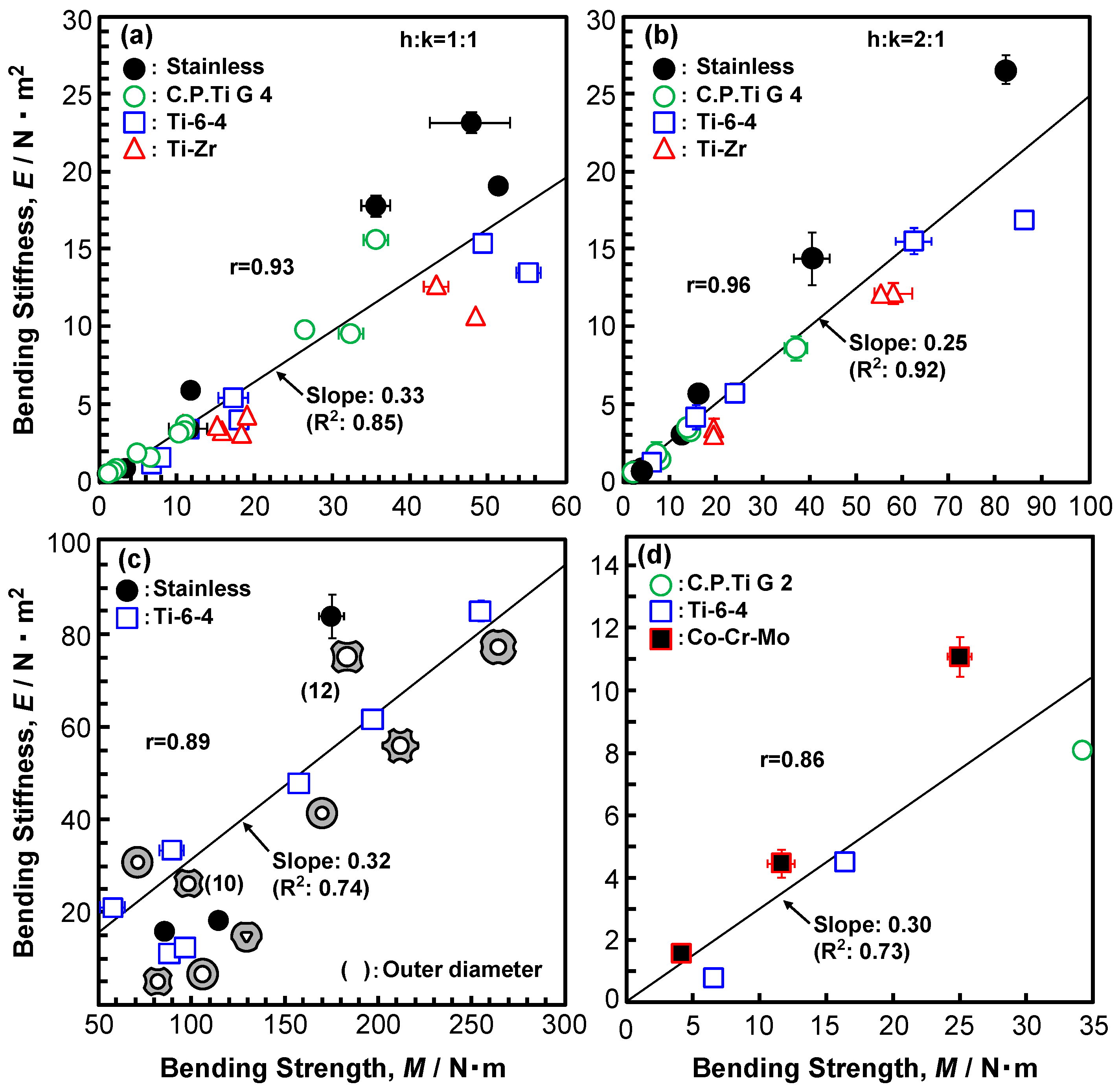
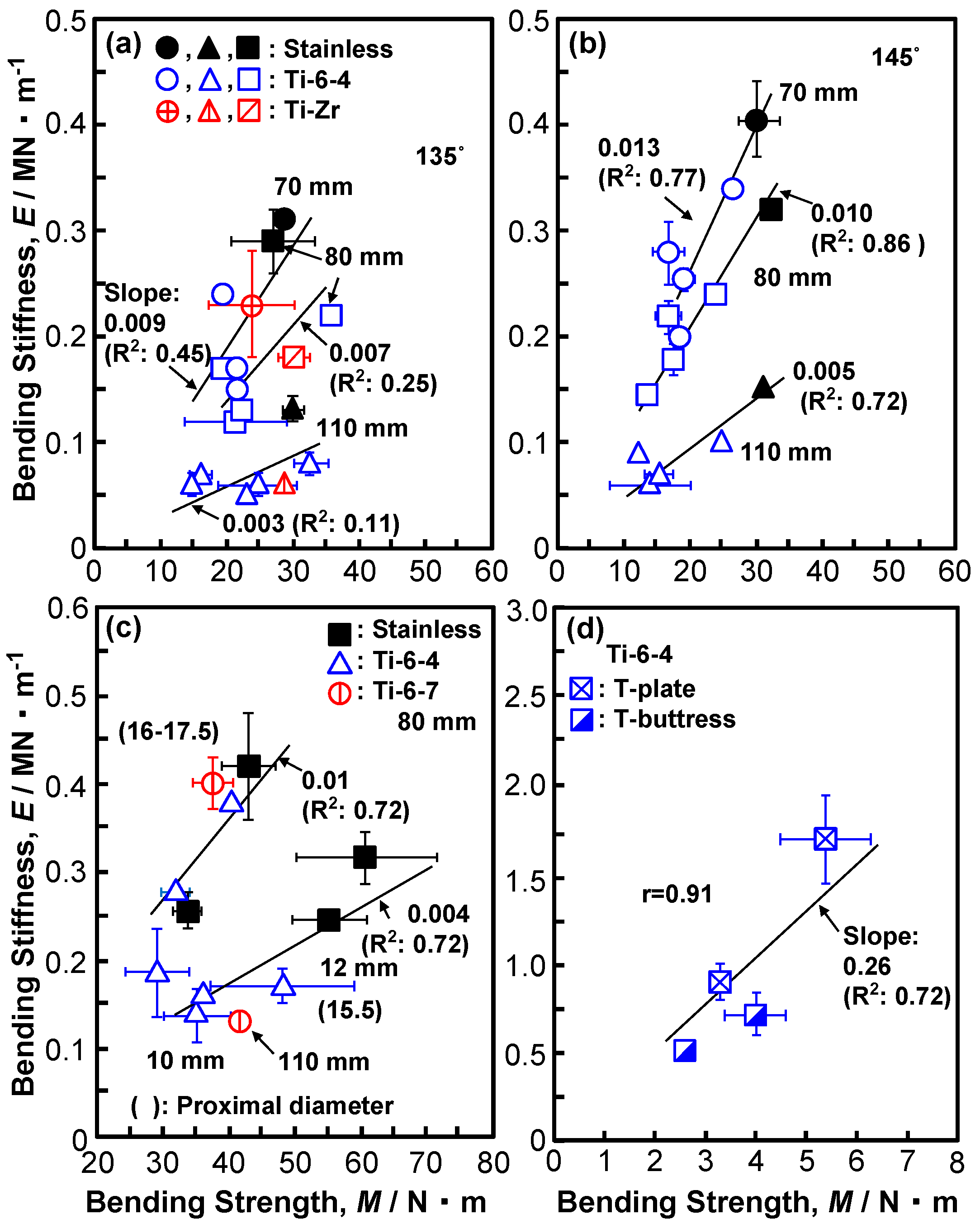
3.1. Bending Stiffness and Bending Strength of Osteosynthesis Devices
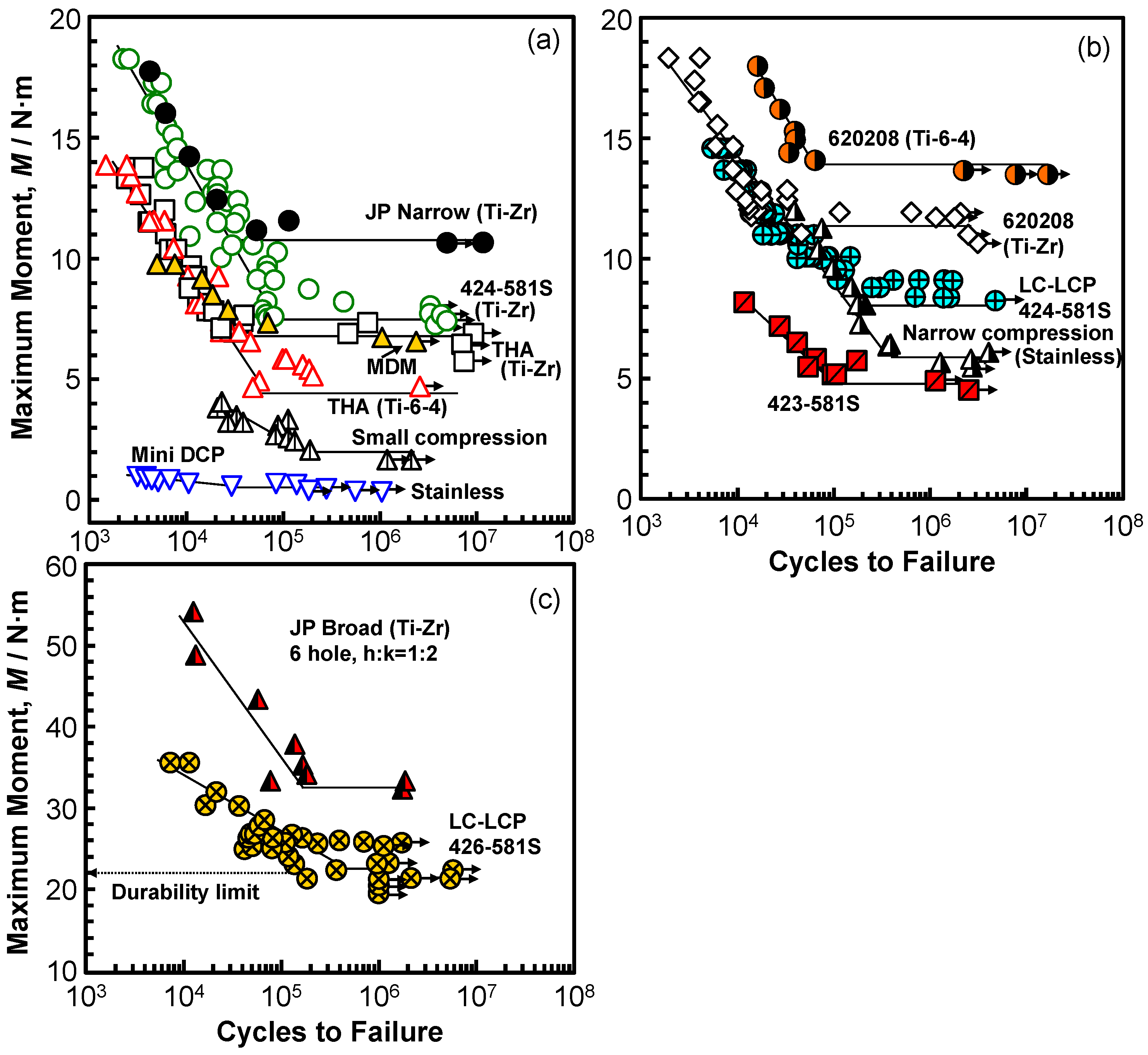
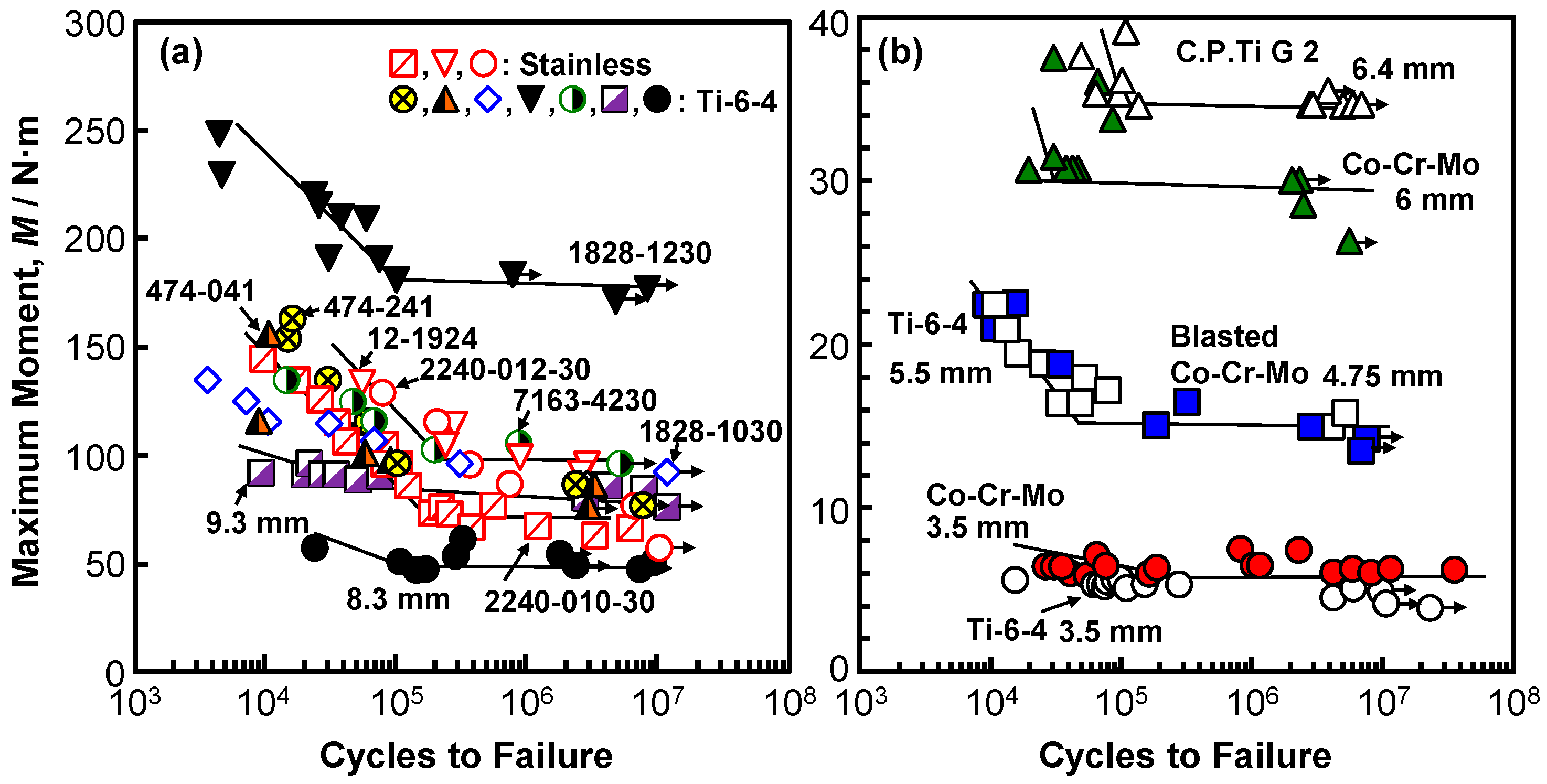
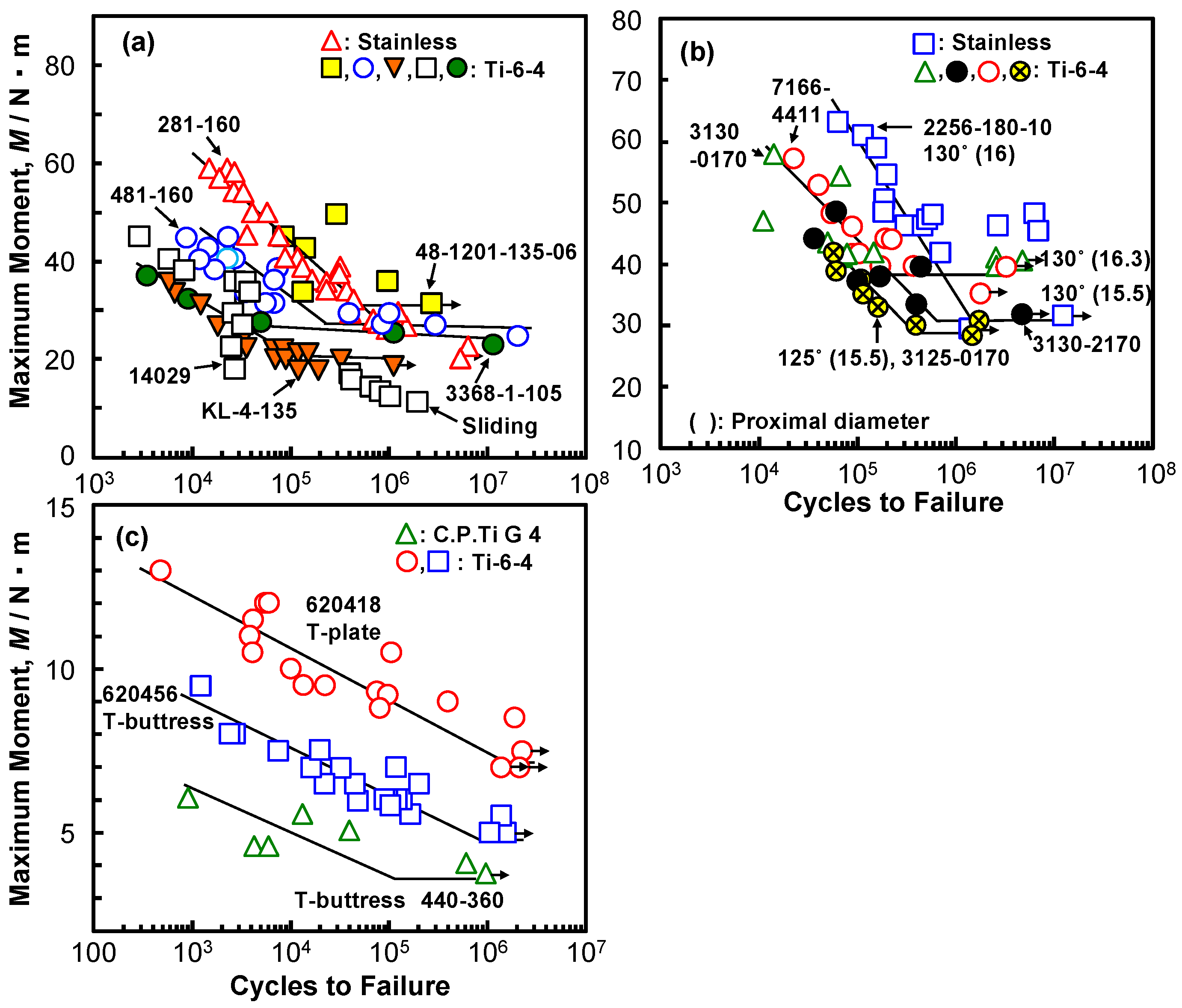
3.2. Durability of Osteosynthesis Devices
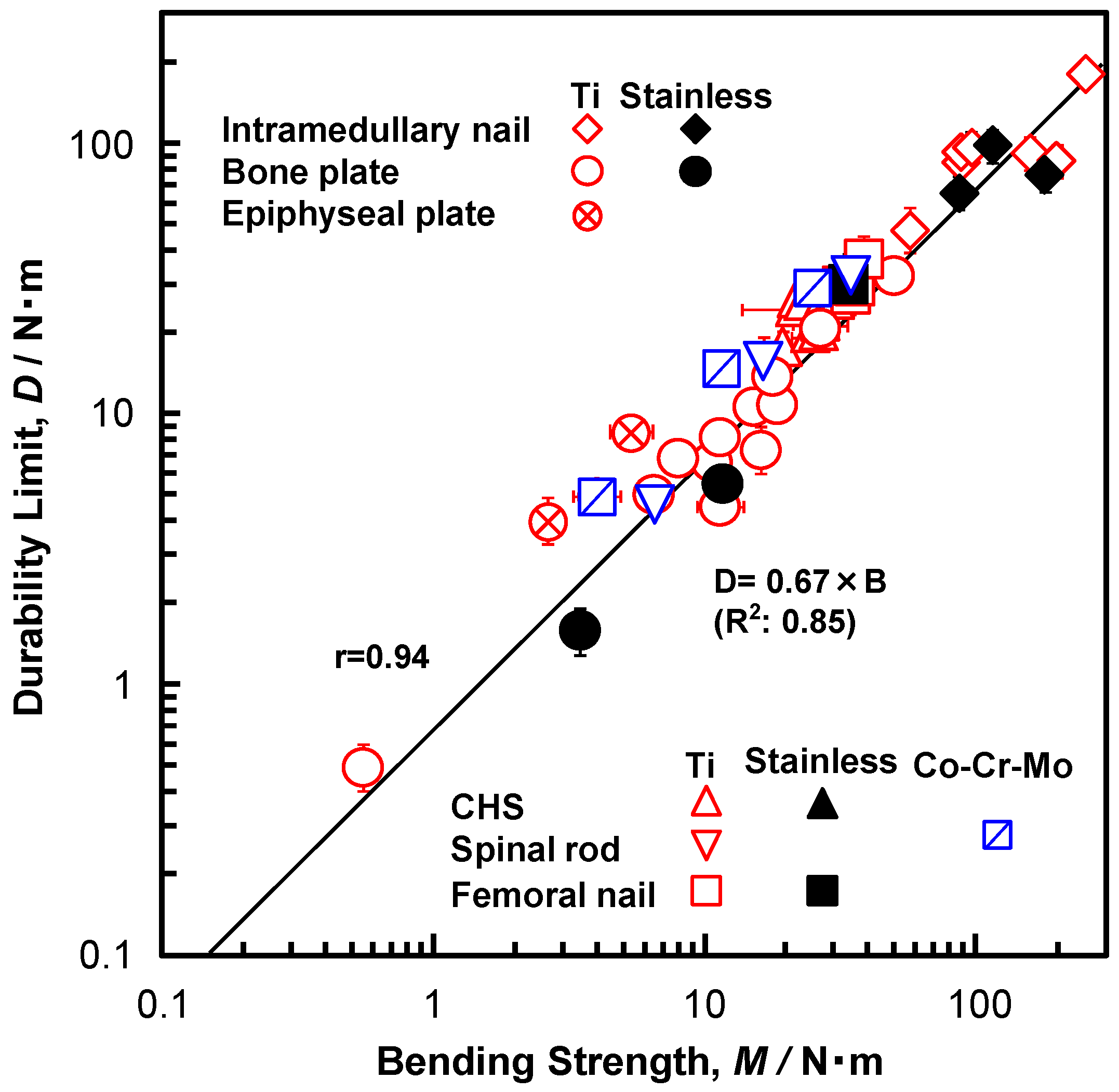
3.3. Relationship Between Durability Limit and Bending Strength
4. Conclusions
- 1.
- The bending stiffness of bone plates, spinal rods, and intramedullary nail rods almost linearly increased with increasing four-point bending strength. The slopes of the straight lines [= (bending stiffness)/(bending strength)] for bone plates, spinal rods, and intramedullary nail rods were approximately 0.3 (R2 = 0.73–0.85).
- 2.
- With increasing the compression bending strength, the compression bending stiffness of CHSs, short femoral nails, and metaphyseal plates tended to increase linearly, depending on the cross-sectional shape.
- 3.
- The durability limit of various types of osteosynthesis devices linearly increased with increasing bending strength (r = 0.93). The relationship (durability limit at 106 cycles) = 0.67 × (bending strength) (N·m) (R2 = 0.85) was obtained by regression. This slope of 0.67 was close to the ratio of the fatigue strength to the tensile strength of the raw metals. The relationship for the highly biocompatible Ti-15Zr-4Nb-4Ta alloy was also linear.
- 4.
- The mechanical strength and ductility of specimens that were cut from various osteosynthesis devices were excellent and their microstructure consisted of fine structures, which are considered to be related to the excellent durability.
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| h | Distance between nearest supporting roller and loading roller in four-point bending test |
| k | Distance between two loading rollers in four-point bending test |
| L–D curve | Load–displacement curve obtained by four-point bending test or compression bending test |
| P | 0.2% Offset load in static bending test |
| M | Bending strength obtained by four-point bending test or compression bending test |
| E | Bending stiffness obtained by four-point bending test or compression bending test |
| M–N curve | Maximum bending moment vs number of cycles to failure on logarithmic scale |
References
- Okazaki, Y. On the effects of hot forging and hot rolling on the microstructural development and mechanical response of a biocompatible Ti alloy. Materials 2012, 5, 1439–1461. [Google Scholar] [CrossRef]
- Okazaki, Y.; Gotoh, E. Metal ion effects on different types of cell line, metal ion incorporation into L929 and MC3T3-E1 cells, and activation of macrophage-like J774.1 cells. Mater. Sci. Eng. C 2013, 33, 1993–2001. [Google Scholar] [CrossRef]
- Okazaki, Y.; Gotoh, E. Comparison of fatigue strengths of biocompatible Ti-15Zr-4Nb-4Ta alloy and other titanium materials. Mater. Sci. Eng. C 2011, 31, 325–333. [Google Scholar] [CrossRef]
- JIS T 7401-4. Titanium Materials for Surgical Implant Applications Part 4: Wrought Titanium 15-Zirconium 4-Niobium 4-Tantalum Alloy; Japanese Standards Association: Tokyo, Japan, 2009. [Google Scholar]
- US Food and Drug Administration. Technical Considerations for Additive Manufactured Medical Devices; US Food and Drug Administration: Concord, NH, USA, 2017.
- Okazaki, Y. Development trends of custom-made orthopedic implants. J. Artif. Organs 2012, 15, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Guidance on Evaluation of Customized Orthopedic Devices for Osteosynthesis; PFSB/ELD/OMDE (Yakushokuki) Notification 1215 No. 1 of the Director of Medical Devices and Regenerative Medicine Evaluation Division; Pharmaceutical Safety and Environmental Health Bureau: Tokyo, Japan, 2010.
- Ministry of Health, Labour and Welfare. Guidance on Evaluation of Orthopedic Customized Artificial Hip Joint Prosthesis; PFSB/ELD/OMDE (Yakushokuki) Notification 1207 No. 1 of the Director of Medical Devices and Regenerative Medicine Evaluation Division; Pharmaceutical Safety and Environmental Health Bureau: Tokyo, Japan, 2011.
- Ministry of Health, Labour and Welfare. Guidance on Evaluation of the Orthopedic Implants Manufactured by Additive Manufacturing Technology; Annex 3, Notification 0912 No. 2 of the Director of Medical Devices and Regenerative Medicine Evaluation Division; Pharmaceutical Safety and Environmental Health Bureau: Tokyo, Japan, 2014.
- Ministry of Health, Labour and Welfare. Guidance on Evaluation of Customized Orthopedic Devices Manufactured by Additive Manufacturing Technology with Medical Image Data Obtained from the Patient; Annex 3, Notification 0925 No. 1 of the Director of Medical Devices and Regenerative Medicine Evaluation Division; Pharmaceutical Safety and Environmental Health Bureau: Tokyo, Japan, 2015.
- Thapa, N.; Prayson, M.; Goswami, T. A failure study of a locking compression plate implant. Case Stud. Eng. Fail. Anal. 2015, 3, 68–72. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, A.; Joshi, G.R.; John, J.T. Retrospective study of implant failure in orthopaedic surgery. Med. J. Armed Forces India 2006, 62, 70–72. [Google Scholar] [CrossRef]
- Rotne, R.; Bertollo, N.; Walsh, W.; Dhand, N.K.; Voss, K.; Johnson, K.A. Influence of plate–bone contact on cyclically loaded conically coupled locking plate failure. Injury 2014, 45, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, D.G.; Brenkel, I.J. The supracondylar intramedullary nail in elderly patients with distal femoral fractures. Injury 1999, 30, 475–484. [Google Scholar] [CrossRef]
- Bucholz, R.W.; Ross, S.E.; Lawrence, K.L. Fatigue fracture of the interlocking nail in the treatment of fractures of the distal part of the femoral shaft. J. Bone Joint Surg. 1987, 69, 1391–1399. [Google Scholar]
- Hahn, D.; Bradbury, N.; Hartley, R.; Radford, P.J. Intramedullary nail breakage in distal fractures of the tibia. Injury 1996, 27, 323–327. [Google Scholar] [CrossRef]
- Ruiz, A.L.; Kealey, W.D.C.; McCoy, G.F. Implant failure in tibial nailing. Injury 2000, 31, 359–362. [Google Scholar] [CrossRef]
- Bhat, A.K.; Rao, S.K.; Bhaskaranand, K. Mechanical failure in intramedullary interlocking nails. J. Orthop. Surg. 2006, 14, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Aggerwal, S.; Gahalot, N.; Saini, U.C.; Bali, K. Failure of intramedullary femoral nail with segmental breakage of distal locking bolts: A case report and review of the literature. Chin. J. Trauma 2011, 14, 188–192. [Google Scholar]
- Yang, J.S.; Sponseller, P.D.; Thompson, G.H.; Akbarnia, B.A.; Emans, J.B.; Yazici, M.; Skaggs, D.L.; Shah, S.A.; Slari, P.; Poe-Kocher, C. Growing rod fractures: Risk factors and opportunities for prevention. Spine 2011, 36, 1639–1644. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Neo, M.; Fujibayashi, S.; Ito, H.; Takemoto, M.; Nakamura, T. Mechanical implant failure in posterior cervical spine fusion. Eur. Spine J. 2012, 21, 328–334. [Google Scholar] [CrossRef]
- Heiney, J.P.; Barnett, M.D.; Vrabec, G.A.; Schoenfeld, A.J.; Baji, A.; Njus, G.O. Distal femoral fixation: A biomechanical comparison of trigen retrograde intramedullary (i.m.) nail, dynamic condylar screw (DCS), and locking compression plate (LCP) condylar plate. J. Trauma 2009, 66, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Kasimatis, G.B.; Lambiris, E.; Tyllianakis, M.; Giannikas, D.; Mouzakis, D.; Panagiotopoulos, E. Gamma nail breakage: A report of four cases. J. Orthop. Surg. 2007, 15, 368–372. [Google Scholar] [CrossRef]
- Najibi, S.; Lemos, M.; Fehnel, D. Mechanical failure of the long gamma nail in two proximal femur fractures. Iowa Orthop. J. 2010, 30, 205–210. [Google Scholar]
- Gaebler, C.; Stanzl-Tschegg, S.; Tschegg, E.K.; Kukla, C.; Menth-Chiari, W.A.; Wozasek, G.E.; Heinz, T. Implant failure of the gamma nail. Injury 1999, 30, 91–99. [Google Scholar] [CrossRef]
- Wee, J.L.H.; Sathappan, S.S.; Yeo, M.S.W.; Low, Y.P. Management of Gamma nail breakage with bipolar hemi-arthroplasty. Singap. Med. J. 2009, 50, e44–e47. [Google Scholar]
- Maes, M.; Deboer, Y.; Brabants, K. Failure of the titanium trochanteric Gamma nail in ununited metastatic fractures. Acta Orthop. Belg. 2012, 78, 552–557. [Google Scholar] [PubMed]
- Cruz-Sánchez, M.; Torres-Claramunt, R.; Alier-Fabregó, A.; Martínez-Díaz, S. Salvage for nail breakage in femoral intramedullary nailing. Injury 2015, 46, 729–733. [Google Scholar] [CrossRef] [PubMed]
- Tomás-Hernández, J.; Núñez-Camarena, J.; Teixidor-Serra, J.; Guerra-Farfan, E.; Selga, J.; Porcel, J.A.; Andrés-Peiró, J.V.; Molero, V. Salvage for intramedullary nailing breakage after operative treatment of trochanteric fractures. Injury 2018, 49, S44–S50. [Google Scholar] [CrossRef] [PubMed]
- Gervais, B.; Vadean, A.; Raison, M.; Brochu, M. Failure analysis of a 316L stainless steel femoral orthopedic implant. Case Stud. Eng. Fail. Anal. 2016, 5–6, 30–38. [Google Scholar] [CrossRef]
- Okazaki, Y.; Ishii, D.; Ogawa, A. Spatial stress distribution analysis by thermoelastic stress measurement and evaluation of effect of stress concentration on durability of various orthopedic implant devices. Mater. Sci. Eng. C 2017, 75, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, D.C.; Doornink, J.; Madey, S.M.; Bottlang, M. Relative stability of conventional and locked plating fixation in a model of the osteoporotic femoral diaphysis. Clin. Biomech. 2009, 24, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Kanchanomai, C.; Phiphobmongkol, V.; Muanjan, P. Fatigue failure of an orthopedic implant—A locking compression plate. Eng. Fail. Anal. 2008, 15, 521–530. [Google Scholar] [CrossRef]
- Hoffmeier, K.L.; Hofmann, G.O.; Mückley, T. Choosing a proper working length can improve the lifespan of locked plates. A biomechanical study. Clin. Biomech. 2011, 26, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Snow, M.; Thompson, G.; Turner, P.G. A mechanical comparison of the locking compression plate (LCP) and the low contact-dynamic compression plate (DCP) in an osteoporotic bone model. J. Orthop. Trauma 2008, 22, 121–125. [Google Scholar] [CrossRef]
- Schüller, M.; Drobetz, H.; Redl, H.; Tschegg, E.K. Analysis of the fatigue behaviour characterized by stiffness and permanent deformation for different distal volar radius compression plates. Mater. Sci. Eng. C 2009, 29, 2471–2477. [Google Scholar] [CrossRef]
- Heiney, J.P.; Battula, S.; O’Connor, J.A.; Ebraheim, N.; Schoenfeld, A.J.; Vrabec, G. Distal femoral fixation: A biomechanical comparison of retrograde nail, retrograde intramedullary nail, and prototype locking retrograde nail. Clin. Biomech. 2012, 27, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Schüller, M.; Herndler, S.; Weninger, P.; Jamek, M.; Redl, H.; Tschegg, E.K. Stiffness and permanent deformation of extra-articular distal tibia fractures treated with unreamed small diameter intramedullary nailing. Mater. Sci. Eng. C 2008, 28, 1209–1216. [Google Scholar] [CrossRef]
- Steinberg, E.L.; Blumberg, N.; Dekel, S. The fixion proximal femur nailing system: Biomechanical properties of the nail and a cadaveric study. J. Biomech. 2005, 38, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Cheung, G.; Zalzal, P.; Bhandari, M.; Spelt, J.K.; Papini, M. Finite element analysis of a femoral retrograde intramedullary nail subject to gait loading. Med. Eng. Phys. 2004, 26, 93–108. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Agarwal, A.K.; Jayaswal, A.; Goel, V. Smaller interval distractions may reduce chances of growth rod breakage without impeding desired spinal growth: A finite element study. Spine Deform. 2014, 2, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Yettram, A.L.; Yao, M.S.; Procter, P. Finite element analysis of a Gamma nail within a fractured femur. Med. Eng. Phys. 1998, 20, 677–683. [Google Scholar] [CrossRef]
- Feerick, E.M.; Kennedy, J.; Mullett, H.; FitzPatrick, D.; McGarry, P. Investigation of metallic and carbon fibre PEEK fracture fixation devices for three-part proximal humeral fractures. Med. Eng. Phys. 2013, 35, 712–722. [Google Scholar] [CrossRef] [PubMed]
- ASTM F 382-14. Standard Specification and Test Method for Metallic Bone Plates; ASTM International: West Conshohocken, PA, USA, 2014. [Google Scholar]
- ASTM F1264-16. Standard Specification and Test Methods for Intramedullary Fixation Devices; ASTM International: West Conshohocken, PA, USA, 2016. [Google Scholar]
- JIS T 0312. Testing Methods for Bending Properties of Metallic Osteosynthesis Devices; Japanese Standards Association: Tokyo, Japan, 2009. [Google Scholar]
- ISO 9585: 1990. Implants for Surgery—Determination of Bending Strength and Stiffness of Bone Plates; International Organization for Standardization: Geneva, Switzerland, 1990. [Google Scholar]
- ASTM F384-17. Standard Specifications and Test Methods for Metallic Angled Orthopedic Fracture Fixation Devices; ASTM International: West Conshohocken, PA, USA, 2017. [Google Scholar]
- JIS T 0313. Testing Methods for Compression Bending Properties of Metallic Osteosynthesis Devices; Japanese Standards Association: Tokyo, Japan, 2009. [Google Scholar]
- JSME S 002. Standard Method of Statistical Fatigue Testing; The Japan Society of Mechanical Engineers: Tokyo, Japan, 1981. [Google Scholar]
- JSMS-SD-06-08. Standard Evaluation Method of Fatigue Reliability for Metallic Materials—Standard Regression Method of SN Curves; JSMS Committee on Fatigue and Reliability Engineering: Tokyo, Japan, 2008. [Google Scholar]
- Okazaki, Y. Comparison of fatigue properties and fatigue crack growth rates of various implantable metals. Materials 2012, 5, 2981–3005. [Google Scholar] [CrossRef]

| Alloy | σ0.2%PS /MPa | σUTS/MPa | T.E.(%) | R.A.(%) |
|---|---|---|---|---|
| Bone plate | ||||
| C.P. Ti G 4 | 650 ± 13 | 700 ± 7 | 21 ± 2 | 56 ± 3 |
| Ti-6-4 | 873 ± 26 | 949 ± 6 | 24 ± 2 | 34 ± 7 |
| Stainless | 877 ± 17 | 994 ± 14 | 21 ± 1 | 81 ± 3 |
| Ti-Zr | 848 ± 2 | 915 ± 3 | 21 ± 2 | 55 ± 3 |
| Spinal rod | ||||
| C.P. Ti G 2 | 322 ± 16 | 431 ± 9 | 35 ± 3 | 68 ± 1 |
| C.P. Ti G 4 | 597 ± 1 | 755 ± 1 | 34 ± 2 | 54 ± 1 |
| Ti-6-4 | 848 ± 4 | 1003 ± 3 | 20 ± 2 | 46 ± 4 |
| Co-Cr-Mo | 846 ± 10 | 1315 ± 9 | 36 ± 2 | 27 ± 1 |
| Intramedullary nail | ||||
| Ti-6-4 | 874 ± 50 | 985 ± 3 | 19 ± 1 | 34 ± 3 |
| Stainless | 790 ± 54 | 1100 ± 17 | 26 ± 4 | 66 ± 3 |
| CHS | ||||
| Ti-6-4 | 917 ± 35 | 966 ± 31 | 19 ± 2 | 45 ± 8 |
| Stainless | 971 ± 48 | 1009 ± 63 | 15 ± 2 | 72 ± 5 |
| Short femoral nail | ||||
| Ti-6-4 | 873 ± 79 | 973 ± 9 | 20 ± 2 | 36 ± 4 |
| Ti-6-7 | 862 ± 18 | 952 ± 8 | 21 ± 1 | 36 ± 4 |
| Stainless | 864 ± 109 | 1101 ± 57 | 21 ± 1 | 78 ± 2 |
| High-N stainless | 1229 ± 8 | 1300 ± 5 | 14 ± 1 | 33 ± 2 |
| Epiphyseal plate | ||||
| C.P. Ti G 4 | 456 ± 32 | 719 ± 4 | 27 ± 2 | 51 ± 1 |
| Ti-6-4 | 967 ± 17 | 1066 ± 12 | 16 ± 1 | 42 ± 6 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okazaki, Y.; Gotoh, E.; Mori, J. Strength–Durability Correlation of Osteosynthesis Devices Made by 3D Layer Manufacturing. Materials 2019, 12, 436. https://doi.org/10.3390/ma12030436
Okazaki Y, Gotoh E, Mori J. Strength–Durability Correlation of Osteosynthesis Devices Made by 3D Layer Manufacturing. Materials. 2019; 12(3):436. https://doi.org/10.3390/ma12030436
Chicago/Turabian StyleOkazaki, Yoshimitsu, Emiko Gotoh, and Jun Mori. 2019. "Strength–Durability Correlation of Osteosynthesis Devices Made by 3D Layer Manufacturing" Materials 12, no. 3: 436. https://doi.org/10.3390/ma12030436
APA StyleOkazaki, Y., Gotoh, E., & Mori, J. (2019). Strength–Durability Correlation of Osteosynthesis Devices Made by 3D Layer Manufacturing. Materials, 12(3), 436. https://doi.org/10.3390/ma12030436





