Efficacy of Bioactive Glass Nanofibers Tested for Oral Mucosal Regeneration in Rabbits with Induced Diabetes
Abstract
:1. Introduction
2. Materials and Methods
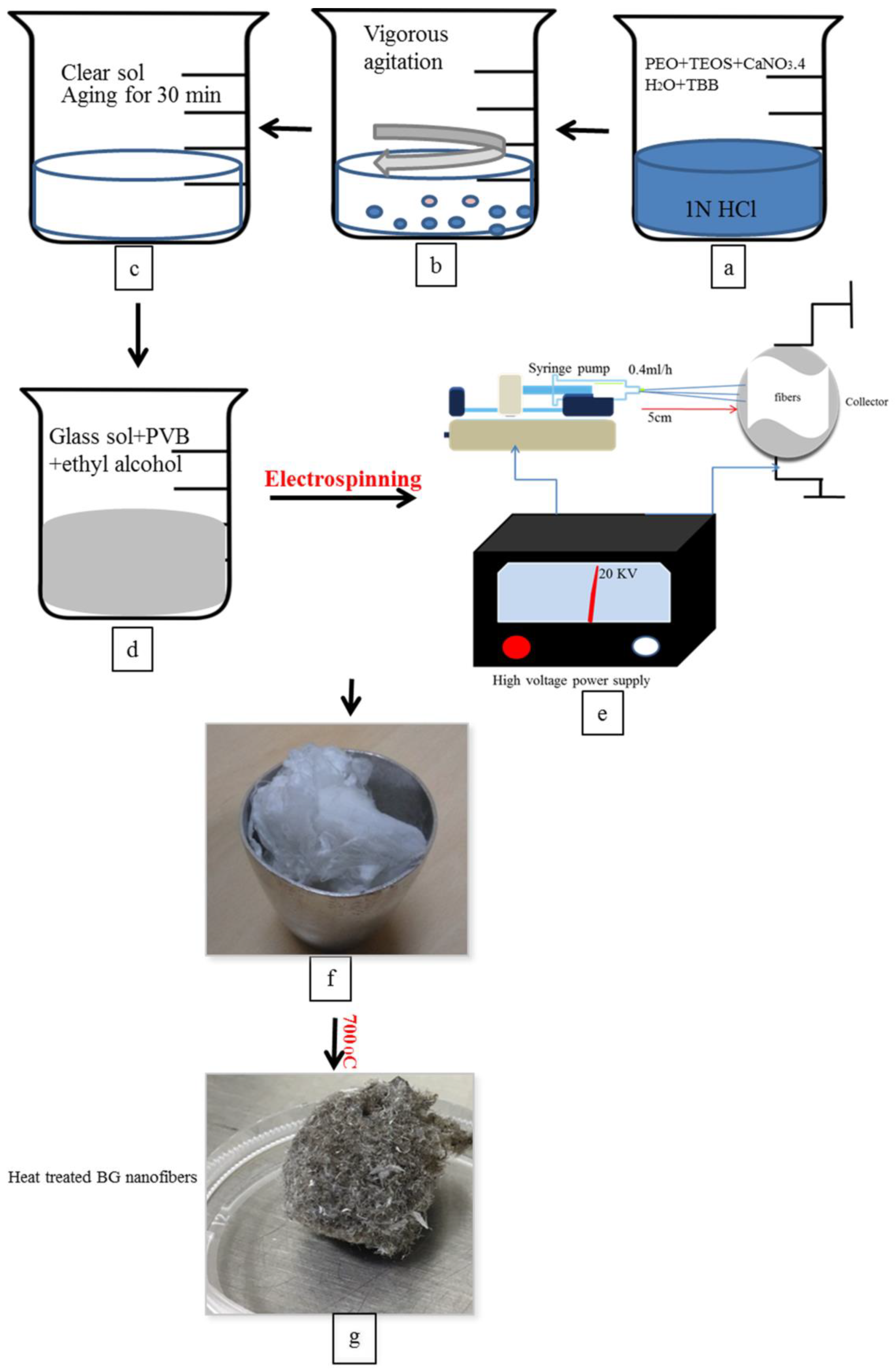
2.1. Preparation of Borate Bioactive Glass Nanofibers
2.2. Characterization of Glass Fibres
2.3. In Vitro Biodegradation
2.4. Sterilization of Glass Nanofibers
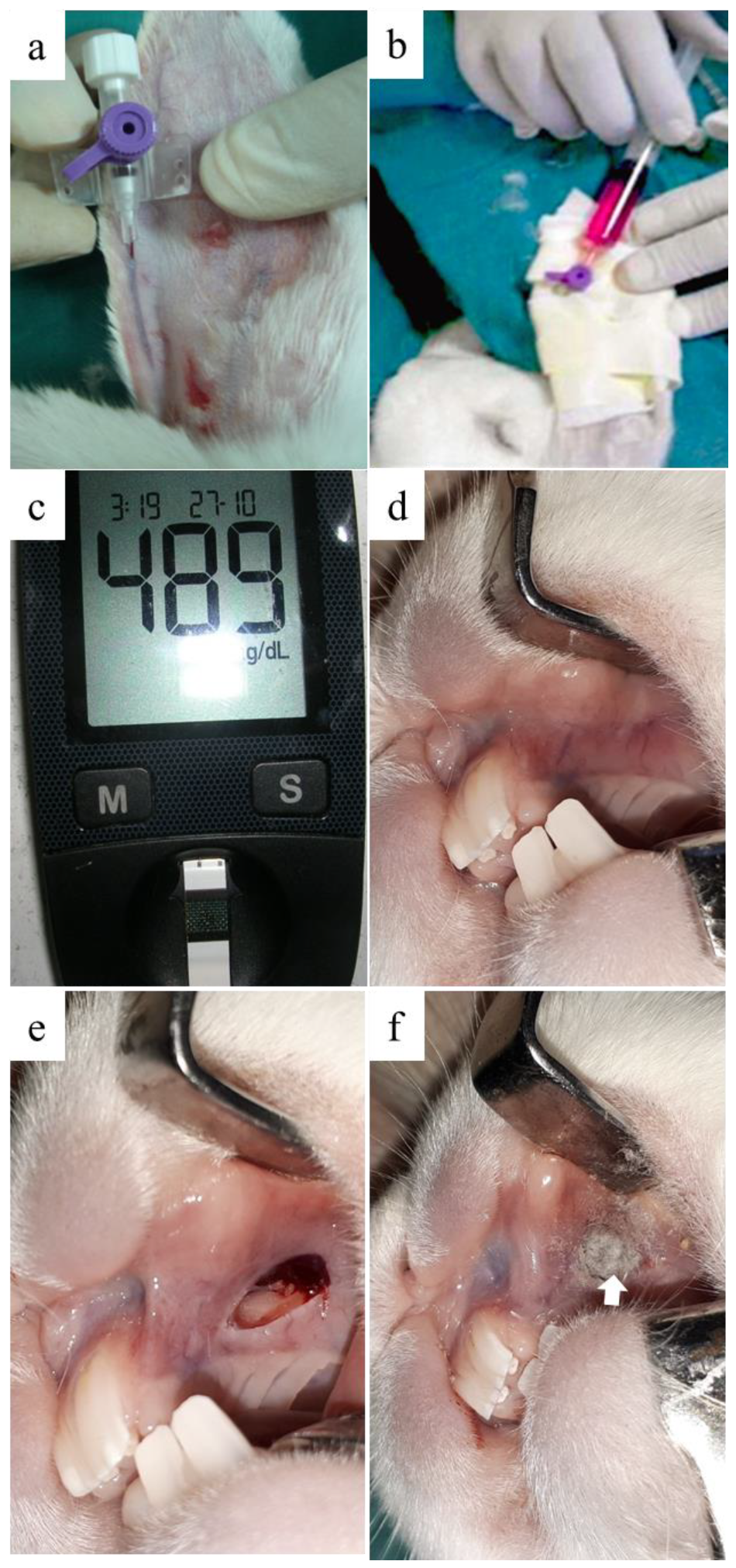
2.5. Oral Mucosal Wound Defect Creation in the Diabetic Animal Model
2.5.1. Animals
2.5.2. Chemical Induction of Diabetes Mellitus in the Animal Model
2.5.3. Surgical Procedure
2.6. Histological and Immunohistochemical Evaluation
2.6.1. Sample Collection for Histological Analysis
2.6.2. Immunohistochemistry
2.7. Statistical Analysis
3. Results
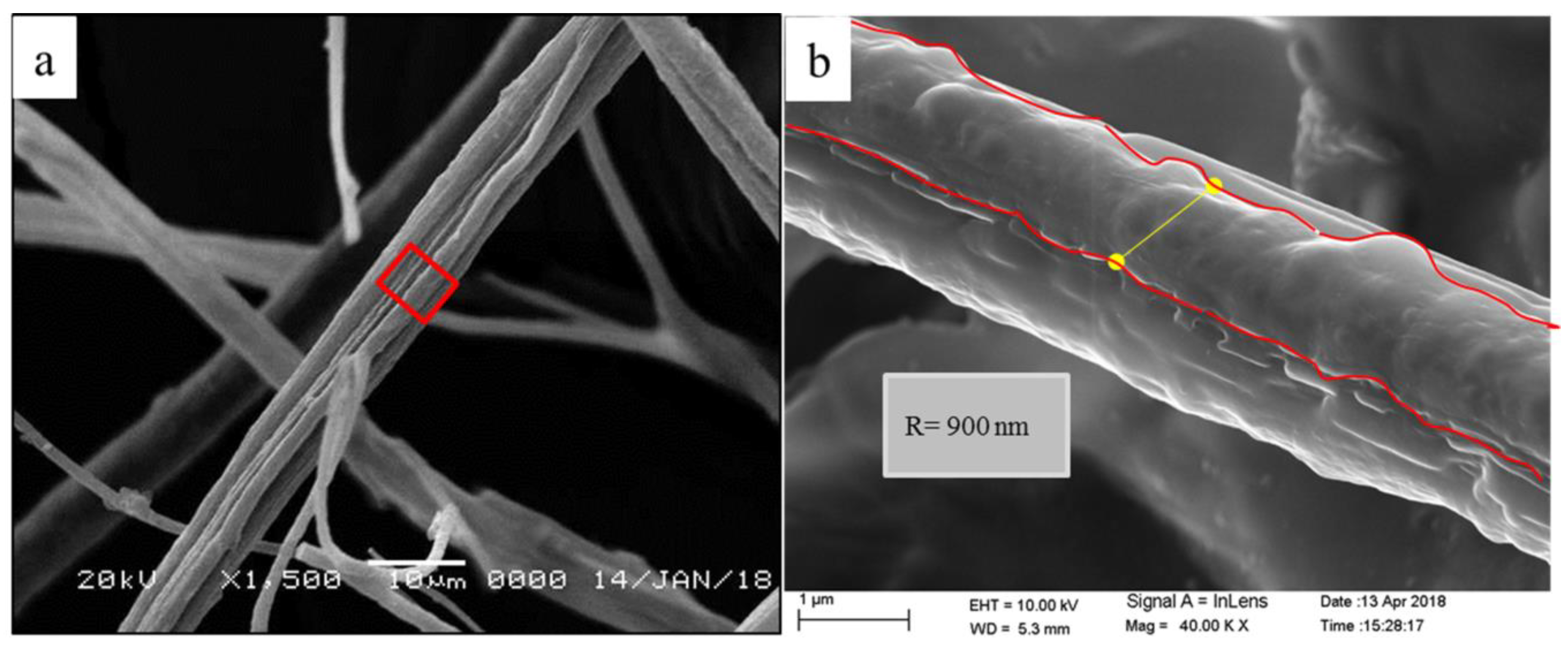
3.1. Characterization of Glass Fibers
3.1.1. X-ray Diffraction (XRD)
3.1.2. Morphological Analysis of the Glass Fibers
3.1.3. In-Vitro Biodegradation
3.2. Diabetic Induction in the Rabbit Animal Model
3.3. Effect of BGnf on the Full-Thickness Mucosal Wound
3.3.1. Macroscopic Observation
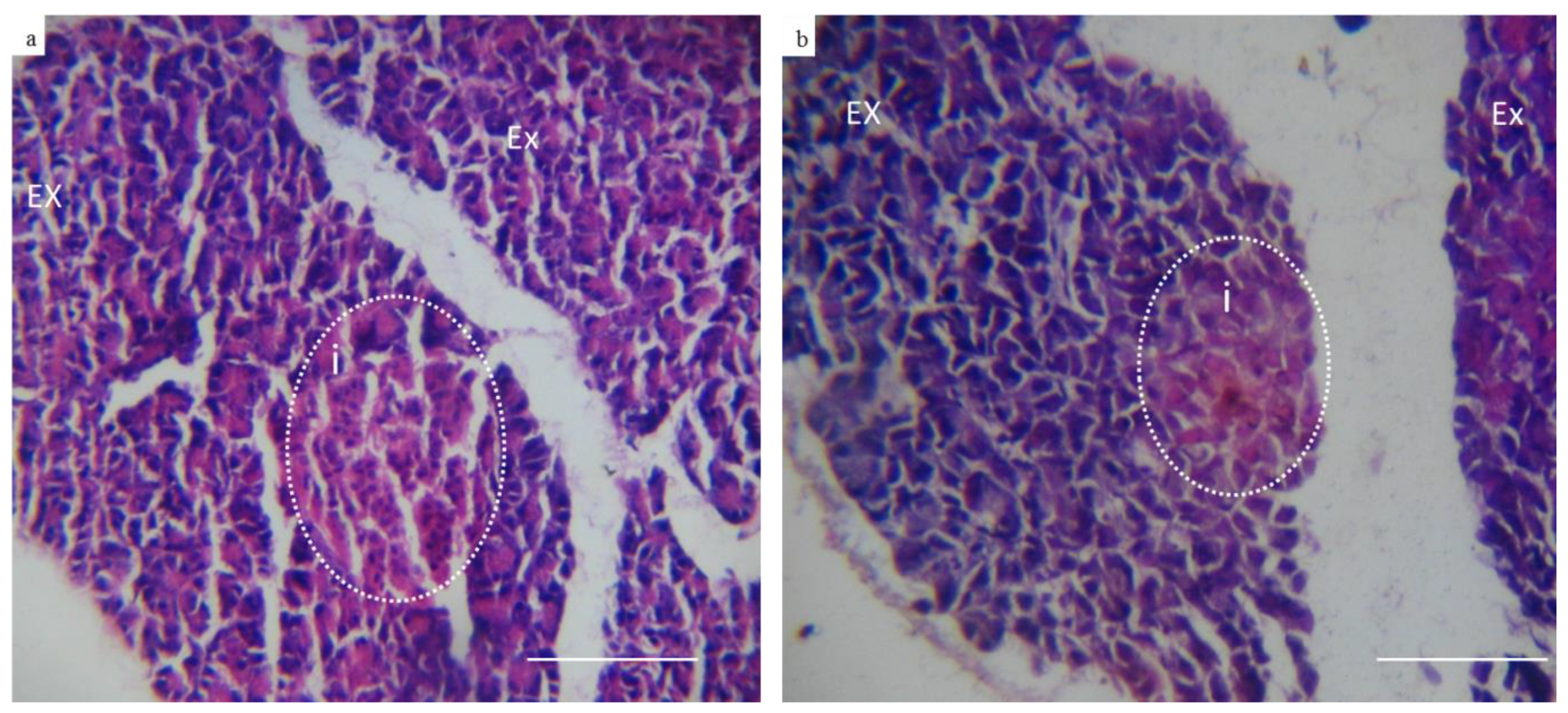
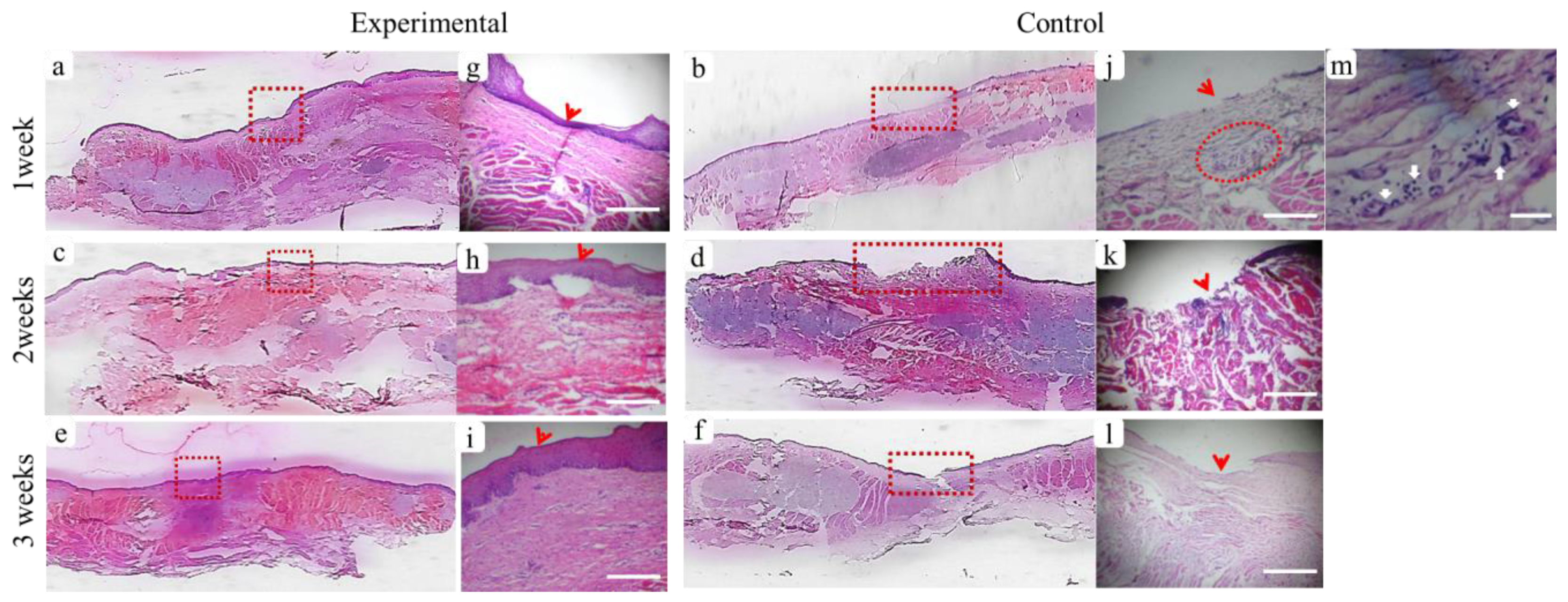
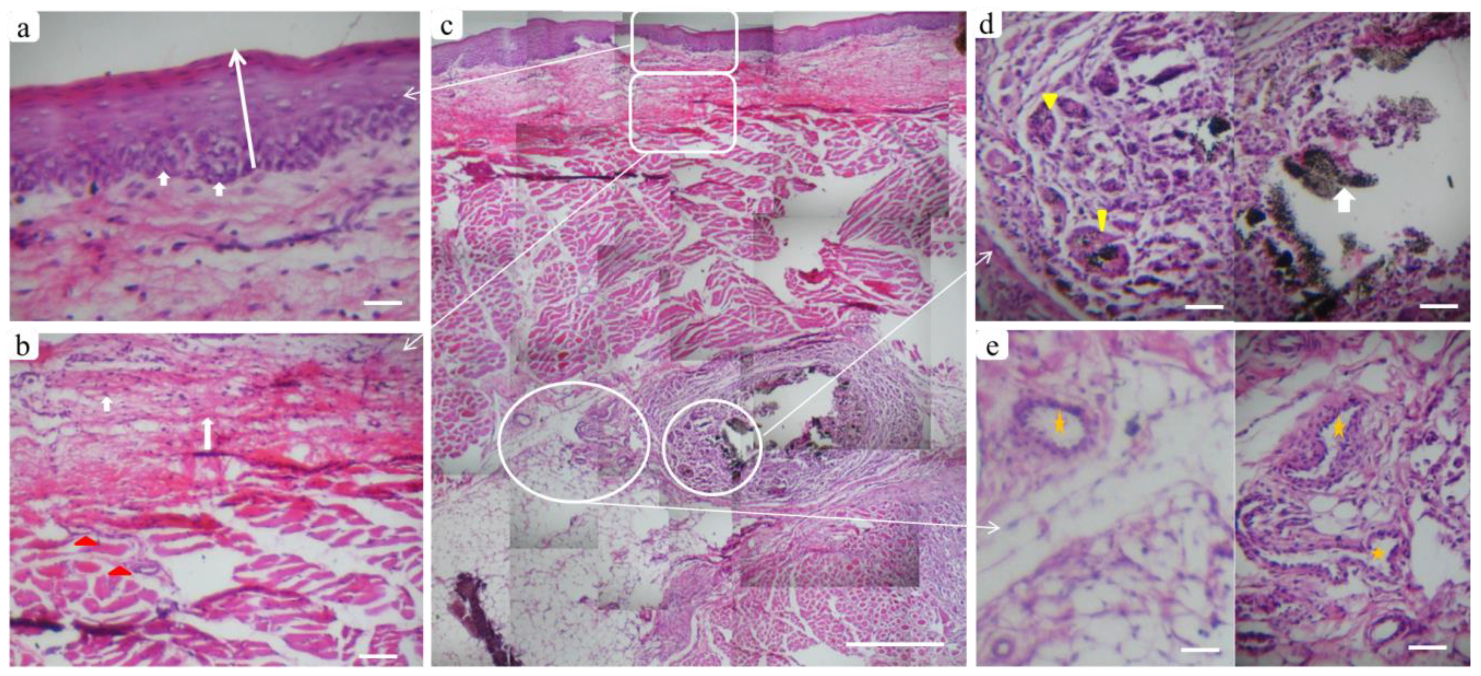
3.3.2. Histological Assessment
3.3.3. Immunohistochemical Analysis
- VEGF Expression
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Association, A.D. Diagnosis and classification of diabetes mellitus. Diabetes Care 2006, 29 (Suppl. 1), S43–S84. [Google Scholar]
- World Health Organization. Global Report on Diabetes. 2016. Available online: https://apps.who.int/iris/handle/10665/204871. (accessed on 7 April 2016).
- Hegazi, R.; El-Gamal, M.; Abdel-Hady, N.; Hamdy, O. Epidemiology of and Risk Factors for Type 2 Diabetes in Egypt. Ann. Glob. Health 2015, 81, 814–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saini, R.; Al-Maweri, S.A.; Saini, D.; Ismail, N.M.; Ismail, A.R. Oral mucosal lesions in non oral habit diabetic patients and association of diabetes mellitus with oral precancerous lesions. Diabetes Res. Clin. Pract. 2010, 89, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Dipietro, L.A. Factors affecting wound healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef]
- Politis, C.; Schoenaers, J.; Jacobs, R.; Agbaje, J.O. Wound Healing Problems in the Mouth. Front Physiol. 2016, 7, 507. [Google Scholar] [CrossRef] [Green Version]
- Xu, F.; Othman, B.; Lim, J.; Batres, A.; Ponugoti, B.; Zhang, C.; Alsadun, S. Foxo1 inhibits diabetic mucosal wound healing but enhances healing of normoglycemic wounds. Diabetes 2015, 64, 243–256. [Google Scholar] [CrossRef] [Green Version]
- Abiko, Y.; Selimovic, D. The mechanism of protracted wound healing on oral mucosa in diabetes. Rev. Bosn. J. Basic Med. Sci. 2010, 10, 186–191. [Google Scholar] [CrossRef]
- Vlassara, H.; Fuh, H.; Makita, Z.; Krungkrai, S.; Cerami, A.; Bucala, R. Exogenous advanced glycosylation end products induce complex vascular dysfunction in normal animals: A model for diabetic and aging complications. Proc. Natl. Acad. Sci. USA 1992, 89, 12043–12047. [Google Scholar] [CrossRef] [Green Version]
- Vincent, A.M.; Russell, J.W.; Low, P.; Feldman, E.L. Oxidative stress in the pathogenesis of diabetic neuropathy. Endocr. Rev. 2004, 25, 612–628. [Google Scholar] [CrossRef]
- Delamaire, M.; Maugendre, D.; Moreno, M.; Le Goff, M.C.; Allannic, H.; Genetet, B. Impaired leucocyte functions in diabetic patients. Diabet. Med. 1997, 14, 29–34. [Google Scholar] [CrossRef]
- Esposito, K.; Nappo, F.; Marfella, R.; Giugliano, G.; Giugliano, F.; Ciotola, M.; Giugliano, D. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: Role of oxidative stress. Circulation 2002, 106, 2067–2072. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gümüş, P.; Buduneli, N.; Çetinkalp, Ş.; Hawkins, S.I.; Renaud, D.; Kinane, D.F.; Scott, D.A. Salivary antioxidants in patients with type 1 or 2 diabetes and inflammatory periodontal disease: A case-control study. J. Periodontol. 2009, 80, 1440–1446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schramm, V.L., Jr.; Johnson, J.T.; Myers, E.N. Skin grafts and flaps in oral cavity reconstruction. Arch. Otolaryngol. 1983, 109, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Payne, C.E.; Sumfest, J.M.; Deshon, G.E., Jr. Buccal mucosal graft for hypospadias repairs. Tech. Urol. 1998, 4, 173–176. [Google Scholar]
- Schramm, V.L., Jr.; Myers, E.N. How I do it—Head and neck A targeted problem and its solution. Skin graft reconstruction following composite resection. Laryngoscope 1980, 90 Pt 1, 1737–1739. [Google Scholar]
- Langer, R.; Vacanti, J.P. Tissue engineering. Science 1993, 260, 920–926. [Google Scholar] [CrossRef] [Green Version]
- Minuth, W.W.; Sittinger, M.; Kloth, S. Tissue engineering: Generation of differentiated artificial tissues for biomedical applications. Cell Tissue Res. 1998, 291, 1–11. [Google Scholar] [CrossRef]
- Del Bakhshayesh, A.R.; Asadi, N.; Alihemmati, A.; Nasrabadi, H.T.; Montaseri, A.; Davaran, S.; Abedelahi, A. An overview of advanced biocompatible and biomimetic materials for creation of replacement structures in the musculoskeletal systems: Focusing on cartilage tissue engineering. J. Biol. Eng. 2019, 13, 85. [Google Scholar] [CrossRef] [Green Version]
- Rahaman, M.N.; Day, D.E.; Bal, B.S.; Fu, Q.; Jung, S.B.; Bonewald, L.F.; Tomsia, A.P. Bioactive glass in tissue engineering. Acta Biomater. 2011, 7, 2355–2373. [Google Scholar] [CrossRef] [Green Version]
- Yu, Q.; Chang, J.; Wu, C. Silicate bioceramics: From soft tissue regeneration to tumor therapy. J. Mater. Chem. B 2019, 7, 5449–5460. [Google Scholar] [CrossRef]
- Hench, L.L. The story of Bioglass. J. Mater Sci. Mater. Med. 2006, 17, 967–978. [Google Scholar] [CrossRef] [PubMed]
- SJung, D.E.D. Conversion Kinetics of Silicate, Borosilicate, and Borate Bioactive Glasses to Hydroxyapatite. Phys. Chem. Glasses Eur. J. Glass Sci. Technol. Part B 2009, 50, 85–88. [Google Scholar]
- Jones, J.R. Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2013, 9, 4457–4486. [Google Scholar] [CrossRef] [PubMed]
- Miguez-Pacheco, V.; Hench, L.L.; Boccaccini, A.R. Bioactive glasses beyond bone and teeth: Emerging applications in contact with soft tissues. Acta Biomater. 2015, 13, 1–15. [Google Scholar] [CrossRef]
- Baino Francesco, N.G.; Miguez-Pachecob, V.; Boccaccinib, A.R.; Brovaron, C.V. Bioactive glasses: Special applications outside the skeletal system. J. Non-Cryst. Solids 2016, 432, 15–30. [Google Scholar] [CrossRef] [Green Version]
- Andreu, V.; Mendoza, G.; Arruebo, M.; Irusta, S. Smart Dressings Based on Nanostructured Fibers Containing Natural Origin Antimicrobial, Anti-Inflammatory, and Regenerative Compounds. Materials 2015, 8, 5154–5193. [Google Scholar] [CrossRef]
- Ma, W.; Yang, X.; Ma, L.; Wang, X.; Zhang, L.; Yang, G.; Gou, Z. Fabrication of bioactive glass-introduced nanofibrous membranes with multifunctions for potential wound dressing. RSC Adv. 2014, 4, 60114–60122. [Google Scholar] [CrossRef]
- Saha, S.; Bhattacharjee, A.; Rahaman, S.H.; Ray, S.; Marei, M.K.; Jain, H.; Chakraborty, J. Prospects of antibacterial bioactive glass nanofibers for wound healing: An in vitro study. Int. J. Appl. Glass Sci. 2020, 11, 320–328. [Google Scholar] [CrossRef]
- Deliormanl, A.M. Preparation and in vitro characterization of electrospun 45S5 bioactive glass nanofibers. Ceram. Intern. 2015, 41, 417–425. [Google Scholar] [CrossRef]
- William, C.; Lepry, S.S.L.L.; Aldo, R.; Boccaccini Showan, N.N. Acellular Bioactivity of Sol-Gel Derived Borate Glass-Polycaprolactone Electrospun Scaffolds. Biomed. Glasses 2016, 2, 88–98. [Google Scholar]
- Tsigkou, O.; Jones, J.R.; Polak, J.M.; Stevens, M.M. Differentiation of fetal osteoblasts and formation of mineralized bone nodules by 45S5 Bioglass conditioned medium in the absence of osteogenic supplements. Biomaterials 2009, 30, 3542–3550. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Chen, S.; Shi, H.; Xiao, H.; Ma, Y. In vitro study of improved wound-healing effect of bioactive borate-based glass nano-/micro-fibers. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 55, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Dai, Z.; Ronholm, J.; Tian, Y.; Sethi, B.; Cao, X. Sterilization techniques for biodegradable scaffolds in tissue engineering applications. J. Tissue Eng. 2016, 7, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Council, N.R. Guide for the Care and Use of Laboratory Animals, 8th ed.; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Mapara, M.; Thomas, B.S.; Bhat, K.M. Rabbit as an animal model for experimental research. Dent. Res. J. (Isfahan) 2012, 9, 111–118. [Google Scholar]
- Russel, W.M.D.; Burch, R.L. The Rinciples of Human Experimental Technique; UFAW Methuen & Co.: London, UK, 1959; ISBN 0900767782 9780900767784. [Google Scholar]
- Lenzen, S. The mechanisms of alloxan- and streptozotocin-induced diabetes. Diabetologia 2008, 51, 216–226. [Google Scholar] [CrossRef] [Green Version]
- Gorus, F.K.; Malaisse, W.J.; Pipeleers, D.G. Selective uptake of alloxan by pancreatic B-cells. Biochem. J. 1982, 208, 513–515. [Google Scholar] [CrossRef] [Green Version]
- Elsner, M.; Tiedge, M.; Guldbakke, B.; Munday, R.; Lenzen, S. Importance of the GLUT2 glucose transporter for pancreatic beta cell toxicity of alloxan. Diabetologia 2002, 45, 1542–1549. [Google Scholar]
- Wang, J.; Wan, R.; Mo, Y.; Zhang, Q.; Sherwood, L.C.; Chien, S. Creating a long-term diabetic rabbit model. Exp. Diabetes Res. 2010, 2010, 289614. [Google Scholar] [CrossRef]
- Oh, N.H.; Kim, E.Y.; Paek, J.; Kook, Y.A.; Jeong, D.M.; Cho, I.S.; Nelson, G. Evaluation of stability of surface-treated mini-implants in diabetic rabbits. Int. J. Dent. 2014, 2014, 838356. [Google Scholar] [CrossRef] [Green Version]
- Muthuraman, P.; Senthilkumar, R.; Srikumar, K. Alterations in beta-islets of Langerhans in alloxan-induced diabetic rats by marine Spirulina platensis. J. Enzyme Inhib. Med. Chem. 2009, 24, 1253–1256. [Google Scholar] [CrossRef] [Green Version]
- Levin, M.P.; Tsaknis, P.J.; Cutright, D.E. Healing of the oral mucosa with the use of collagen artificial skin. J. Periodontol. 1979, 50, 250–253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu Xiangliang, C.N.; Wang, E. Application of an acellular dermal matrix to a rabbit model of oral mucosal defects. Exp. Ther. Med. 2018, 15, 2450–2456. [Google Scholar]
- Bancroft, J.D.; Gamble, M. (Eds.) Theory and Practice of Histological Techniques, 5th ed.; Churchill Living Stone: New York, NY, USA, 2002. [Google Scholar]
- Karen Petrosyan, R.T.; Daisy, J. Sensitivity of a Novel Biotin-Free Detection Reagent (Powervision+™) for Immunohistochemistry. J. Histotechnol. 2002, 25, 247–250. [Google Scholar] [CrossRef]
- Johnstone, S.; Logan, R.M. Expression of vascular endothelial growth factor (VEGF) in normal oral mucosa, oral dysplasia and oral squamous cell carcinoma. Int. J. Oral. Maxillofac. Surg. 2007, 36, 263–266. [Google Scholar] [CrossRef]
- Zhao, S.; Li, L.; Wang, H.; Zhang, Y.; Cheng, X.; Zhou, N.; Zhang, C. Wound dressings composed of copper-doped borate bioactive glass microfibers stimulate angiogenesis and heal full-thickness skin defects in a rodent model. Biomaterials 2015, 53, 379–391. [Google Scholar] [CrossRef]
- Buchberger, B.; Follmann, M.; Freyer, D.; Huppertz, H.; Ehm, A.; Wasem, J. The importance of growth factors for the treatment of chronic wounds in the case of diabetic foot ulcers. GMS Health Technol. Assess. 2010, 6. [Google Scholar] [CrossRef]
- Squier, C.A.; Kremer, M.J. Biology of oral mucosa and esophagus. J. Natl. Cancer Inst. Monogr. 2001, 29, 7–15. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.G.; Eun, H.C. Differences between fibroblasts cultured from oral mucosa and normal skin: Implication to wound healing. J. Dermatol. Sci. 1999, 21, 176–182. [Google Scholar] [CrossRef]
- Turabelidze, A.; Guo, S.; Chung, A.Y.; Chen, L.; Dai, Y.; Marucha, P.T.; Di Pietro, L.A. Intrinsic differences between oral and skin keratinocytes. PLoS ONE 2014, 9, e101480. [Google Scholar] [CrossRef]
- Szpaderska, A.M.; Walsh, C.G.; Steinberg, M.J.; DiPietro, L.A. Distinct patterns of angiogenesis in oral and skin wounds. J. Dent. Res. 2005, 84, 309–314. [Google Scholar] [CrossRef]
- Brand, H.S.; Veerman, E.C. Saliva and wound healing. Chin. J. Dent Res. 2013, 16, 7–12. [Google Scholar] [PubMed]
- Zaura, E.; Keijser, B.J.; Huse, S.M.; Crielaard, W. Defining the healthy “core microbiome” of oral microbial communities. BMC Microbiol. 2009, 9, 259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, J.; Macewan, M.R.; Ray, W.Z.; Liu, W.; Siewe, D.Y.; Xia, Y. Radially aligned, electrospun nanofibers as dural substitutes for wound closure and tissue regeneration applications. ACS Nano 2010, 4, 5027–5036. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Liu, W.; MacEwan, M.R.; Yeh, Y.C.; Thomopoulos, S.; Xia, Y. Nanofiber membranes with controllable microwells and structural cues and their use in forming cell microarrays and neuronal networks. Small 2011, 7, 293–297. [Google Scholar] [CrossRef] [Green Version]
- Xu, H.; Lv, F.; Zhang, Y.; Yi, Z.; Ke, Q.; Wu, C.; Chang, J. Hierarchically micro-patterned nanofibrous scaffolds with a nanosized bio-glass surface for accelerating wound healing. Nanoscale 2015, 7, 18446–18452. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.W.; Kim, H.K.; Knowles, J.C. Production and potential of bioactive glass nanofibers as a next generation biomaterial. Adv. Funct. Mater. 2006, 16, 1529–1535. [Google Scholar] [CrossRef]
- Huang, W.; Day, D.E.; Kittiratanapiboon, K.; Rahaman, M.N. Kinetics and mechanisms of the conversion of silicate (45S5), borate, and borosilicate glasses to hydroxyapatite in dilute phosphate solutions. J. Mater Sci. Mater. Med. 2006, 17, 583–596. [Google Scholar] [CrossRef]
- Wray, P. Cotton candy’ that heals: Borate glass nanofibers look promising. Ceram. Bull. 2011, 90, 25–29. [Google Scholar]
- Lansdown, A.B. Calcium: A potential central regulator in wound healing in the skin. Wound Repair Regen. 2002, 10, 271–285. [Google Scholar] [CrossRef]
- Naseri, S.; Lepry, W.C.; Nazhat, S.N. Bioactive glasses in wound healing: Hope or hype? J. Mater. Chem. B 2017, 5, 6167–6174. [Google Scholar] [CrossRef]
- Zhai, W.; Lu, H.; Chen, L.; Lin, X.; Huang, Y.; Dai, K.; Chang, J. Silicate bioceramics induce angiogenesis during bone regeneration. Acta Biomater. 2012, 8, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Kargozar, S.; Baino, F.; Hamzehlou, S.; Hill, R.G.; Mozafari, M. Bioactive Glasses: Sprouting Angiogenesis in Tissue Engineering. Trends Biotechnol. 2018, 36, 430–444. [Google Scholar] [CrossRef] [PubMed]
- Dzondo-Gadet, M.; Mayap-Nzietchueng, R.; Hess, K.; Nabet, P.; Belleville, F.; Dousset, B. Action of boron at the molecular level: Effects on transcription and translation in an acellular system. Biol. Trace Elem. Res. 2002, 85, 23–33. [Google Scholar] [CrossRef]
- Zhou, T.; Sui, B.; Mo, X.; Sun, J. Multifunctional and biomimetic fish collagen/bioactive glass nanofibers: Fabrication, antibacterial activity and inducing skin regeneration in vitro and in vivo. Int. J. Nanomed. 2017, 12, 3495–3507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simons, M.C.; Ben-Amotz, R. The Use of Borate-based Biological Glass for the Treatment of Full-thickness Wounds in Six Dogs. J. Vet. Med. Res. 2017, 4, 1108–1113. [Google Scholar]
- Lin, Y.; Brown, R.F.; Jung, S.B.; Day, D.E. Angiogenic effects of borate glass microfibers in a rodent model. J. Biomed. Mater. Res. A 2014, 102, 4491–4499. [Google Scholar] [CrossRef]




| Time (h) | BGnf Ionic Extract (ppm) | |
|---|---|---|
| Si | Ca | |
| 24 h | 41.25 ± 0.94 | 25.15 ± 1.28 |
| 48 h | 60.36 ± 1.05 | 27.36 ± 1.45 |
| 72 h | 67.35 ± 1.58 | 30.25 ± 1.07 |
| Total N. | Diabetic Induction | Study Groups | N | % | ||
|---|---|---|---|---|---|---|
| Condition | N | % | ||||
| 16 New Zealand white rabbits | Induced | 12 | 75.0 | Experimental | 6 | 37.5 |
| Failed | 1 | 6.25 | Control | 6 | 37.5 | |
| Died | 3 | 18.75 | Total | 12 | 75 | |
| Number | Percentage of VEGF Expression of BGnf Treated and Control Groups at 1 and 3 Weeks | |||
|---|---|---|---|---|
| One week | Three weeks | |||
| BGnf | Control | BGnf | Control | |
| Nu of analyzed Fields | 12 | 12 | 12 | 12 |
| Mean ± SD | 14.08 ± 3.88 | 3.92 ± 0.221 | 18.48 ± 1.458 | 16.81 ± 1.65 |
| Sig. (2 tailed) P | 0.0001 * | 0.0064 * | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elshazly, N.; Khalil, A.; Saad, M.; Patruno, M.; Chakraborty, J.; Marei, M. Efficacy of Bioactive Glass Nanofibers Tested for Oral Mucosal Regeneration in Rabbits with Induced Diabetes. Materials 2020, 13, 2603. https://doi.org/10.3390/ma13112603
Elshazly N, Khalil A, Saad M, Patruno M, Chakraborty J, Marei M. Efficacy of Bioactive Glass Nanofibers Tested for Oral Mucosal Regeneration in Rabbits with Induced Diabetes. Materials. 2020; 13(11):2603. https://doi.org/10.3390/ma13112603
Chicago/Turabian StyleElshazly, Noha, Abdelaziz Khalil, Manal Saad, Marco Patruno, Jui Chakraborty, and Mona Marei. 2020. "Efficacy of Bioactive Glass Nanofibers Tested for Oral Mucosal Regeneration in Rabbits with Induced Diabetes" Materials 13, no. 11: 2603. https://doi.org/10.3390/ma13112603






