Are Magnesium Screws Proper for Mandibular Condyle Head Osteosynthesis?
Abstract
:1. Introduction
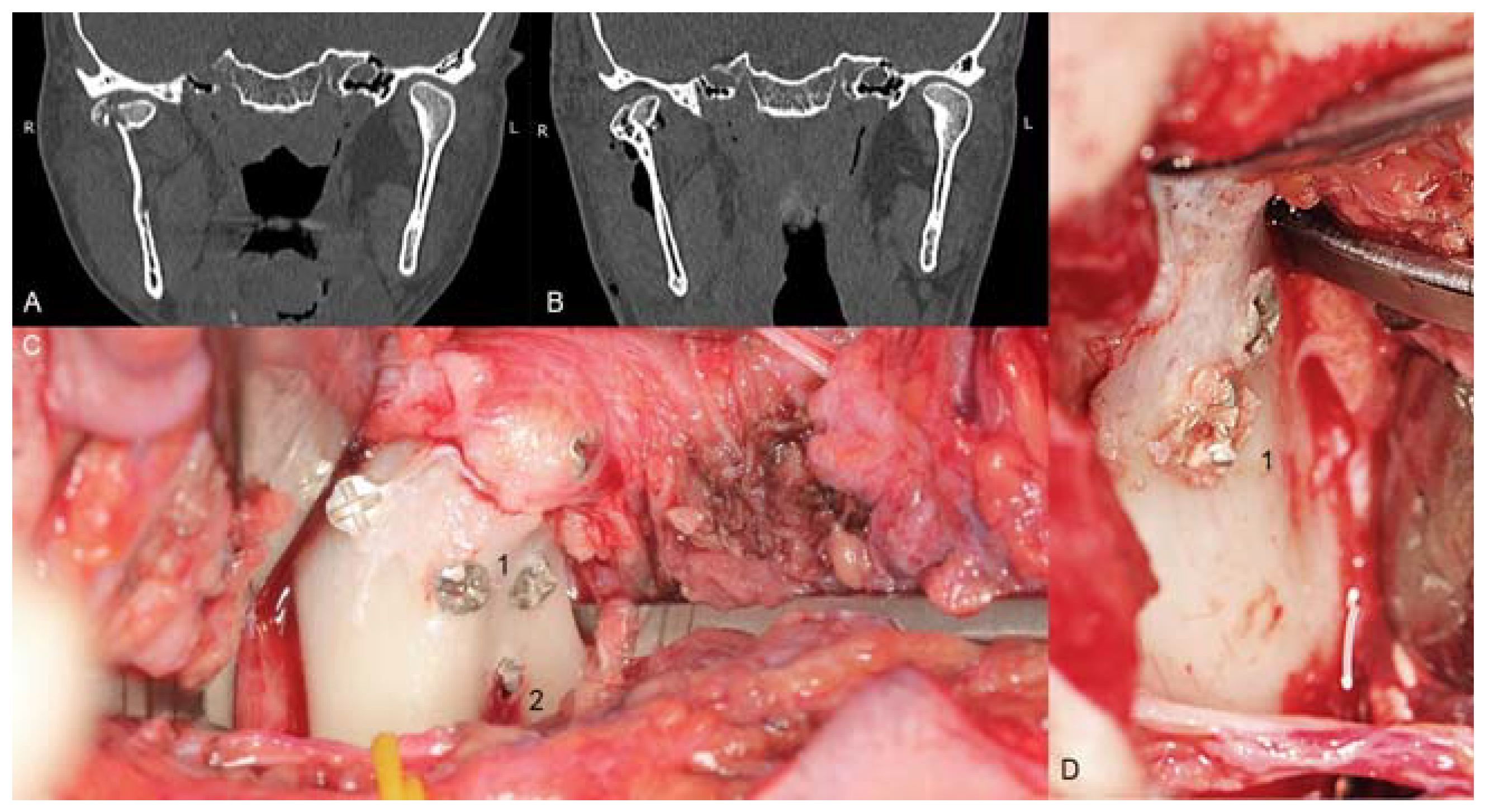
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Leonhardt, H.; Franke, A.; McLeod, N.; Lauer, G.; Nowak, A. Fixation of fractures of the condylar head of the mandible with a new magnesium-alloy biodegradable cannulated headless bone screw. Br. J. Oral Maxillofac. Surg. 2017, 55, 623–625. [Google Scholar] [CrossRef] [PubMed]
- Staiger, M.; Pietak, A.; Huadmai, J.; Dias, G. Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials 2006, 27, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Yu, X.; Wan, P.; Yang, K. Biodegradable materials for bone repairs: A review. J. Mater. Sci. Technol. 2013, 29, 503–513. [Google Scholar] [CrossRef]
- Zhao, D.; Feyerabend, F.; Lu, F.; Wang, J.; Li, J.; Qin, L. Current status on clinical applications of magnesium-based orthopaedic implants: A review from clinical translational perspective. Biomaterials 2017, 112, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Mazur, A.; Maier, J.; Rock, E.; Gueux, E.; Nowacki, W.; Rayssiguier, Y. Magnesium and the inflammatory response: Potential physiopathological implications. Arch. Biochem. Biophys. 2007, 458, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.; Li, K.; Han, Z.; Wang, E.; Xu, Z.; Liu, R.; Tian, Y. Degradable magnesium-based implant materials with anti-inflammatory activity. J. Biomed. Mater. Res. Part A 2012, 101, 1898–1906. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, G.W.; Zhai, Z.J.; Liu, L.N.; Li, H.W.; Yang, K.; Tan, L.L.; Wan, P.; Liu, X.Q.; Ouyang, Z.X.; et al. Antibacterial properties of magnesium in vitro and in an in vivo model of implant-associated methicillin-resistant staphylococcus aureus infection. Antimicrob. Agents Chemother. 2014, 58, 7586–7591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ren, L.; Lin, X.; Tan, L.L.; Yang, K. Effect of surface coating on antibacterial behawior of magnesium based metals. Mater. Lett. 2011, 65, 3509–3511. [Google Scholar] [CrossRef]
- Robinson, D.; Griffith, R.W.; Shechtman, D.; Evans, R.B.; Conzemius, M.G. In vitro antibacterial properties of magnesium metal against escherichia coli, pseudomonas aeruginosa and staphylococcus aureus. Acta Biomater. 2010, 6, 1869–1877. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, Z.; Smith, C.; Sankar, J. Recent advances on the development of magnesium alloys for biodegradable implants. Acta Biomater. 2014, 10, 4561–4573. [Google Scholar] [CrossRef]
- Liu, C.; Fu, X.; Pan, H.; Wan, P.; Wang, L.; Tan, L.; Wang, K.; Zhao, Y.; Yang, K.; Chu, P.K. Biodegradable Mg-Cu alloys with enhanced osteogenesis, angiogenesis, and long-lasting antibacterial effects. Sci. Rep. 2016, 6, 27374. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Z.J.; Qu, X.H.; Li, H.W.; Yang, K.; Wan, P.; Tan, L.L.; Ouyang, Z.X.; Liu, X.Q.; Tian, B.; Xiao, F.; et al. The effect of metallic magnesium degradation products on osteoclast-induced osteolysis and attenuation of NF-kappa B and NFATc1 signaling. Biomaterials 2014, 35, 6299–6310. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.A.; Indresano, T.; O’Ryan, F. Venous Thromboembolism in Oral and maxillofacial surgery: A review of the literature. J. Oral Maxillofac. Surg. 2011, 69, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Chapman, J.R.; Harrington, R.M.; Lee, K.M.; Anderson, P.A.; Tencer, A.F.; Kowalski, D. Factors affecting the pullout strength of cancellous bone screws. J. Biomech. Eng. 1996, 118, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Darvish, K.; Ilyas, A.M. Biomechanical analysis of second-generation headless compression screws. Injury 2012, 43, 1159–1165. [Google Scholar] [CrossRef] [PubMed]
- Baran, O.; Sagol, E.; Oflaz, H.; Sarikanat, M.; Havitcioglu, H. A biomechanical study on preloaded compression effect on headless screws. Arch. Orthop. Trauma Surg. 2009, 129, 1601–1605. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, R.; Evans, S.; Kosashvili, Y. Holding power of variable pitch screws in osteoporotic, osteopenic and normal bone: Are all screws created equal? Injury 2010, 41, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.A.; Kuiper, J.H.; Kelly, C.P. Biomechanical evaluation of a new composite bioresorbable screw. J. Hand Surg. 2006, 31, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Fiorillo, L.; Herford, A.; Crimi, S.; Bianchi, A.; D’Amico, C.; Laino, L.; Cervino, G. Bioactive titanium surfaces: Interactions of eukaryotic and prokaryotic cells of nano devices applied to dental practice. Biomedicines 2019, 7, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boffano, P.; Benech, R.; Gallesio, C.; Arcuri, F.; Benech, A. Current opinions on surgical treatment of fractures of the condylar head. Craniomaxillofacial Trauma Reconstr. 2014, 7, 92–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pilling, E.; Schneider, M.; Mai, R.; Loukota, R.; Eckelt, U. Minimally invasive fracture treatment with cannulated lag screws in intracapsular fractures of the condyle. J. Oral Maxillofac. Surg. 2006, 64, 868–872. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M. Comparison of compression screws used for mandible head fracture treatment—Experimental study. Clin. Oral Investig. 2019, 23, 4059–4066. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdel-Galil, K.; Loukota, R. Fixation of comminuted diacapitular fractures of the mandibular condyle with ultrasound-activated resorbable pins. Br. J. Oral Maxillofac. Surg. 2008, 46, 482–484. [Google Scholar] [CrossRef] [PubMed]
- Müller-Richter, U.; Reuther, T.; Böhm, H.; Kochel, M.; Kübler, A.C. Treatment of intracapsular condylar fractures with resorbable pins. J. Oral Maxillofac. Surg. 2011, 69, 3019–3025. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Deng, J.; Zhu, J.; Li, M.; Xia, B.; Xu, B. Computer-assisted virtual technology in intracapsular condylar fracture with two resorbable long-screws. Br. J. Oral Maxillofac. Surg. 2013, 51, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Windhagen, H.; Radtke, K.; Weizbauer, A.; Diekmann, J.; Noll, Y.; Kreimeyer, U.; Schavan, R.; Stukenborg-Colsman, C.; Waizy, H. Biodegradable magnesium-based screw clinically equivalent to titanium screw in hallux valgus surgery: Short term results of the first prospective, randomized, controlled clinical pilot study. Biomed. Eng. Online 2013, 12, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borys, J.; Maciejczyk, M.; Antonowicz, B.; Sidun, J.; Świderska, M.; Zalewska, A. Free radical production, inflammation and apoptosis in patients treated with titanium mandibular fixations-an observational study. Front. Immunol. 2019, 10, 2662. [Google Scholar] [CrossRef] [PubMed]
- Borys, J.; Maciejczyk, M.; Antonowicz, B.; Kretowski, A.; Waszkiel, D.; Bortnik, P.; Czarniecka-Bargłowska, K.; Kocisz, M.; Szulimowska, J.; Czajkowski, M.; et al. Exposure to Ti4Al4V titanium alloy leads to redox abnormalities, oxidative stress, and oxidative damage in patients treated for mandible fractures. Oxidative Med. Cell. Longev. 2018, 2018, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Borys, J.; Maciejczyk, M.; Antonowicz, B.; Kretowski, A.; Sidun, J.; Domel, E.; Dąbrowski, J.; Ładny, J.R.; Morawska, K.; Zalewska, A. Glutathione metabolism, mitochondria activity, and nitrosative stress in patients treated for mandible fractures. J. Clin. Med. 2019, 8, 127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- A Landes, C.; Kriener, S. Resorbable plate osteosynthesis of sagittal split osteotomies with major bone movement. Plast. Reconstr. Surg. 2003, 111, 1828–1840. [Google Scholar] [CrossRef] [PubMed]
- Bergsma, J. A 5-year in vitro and in vivo study of the biodegradation of polylactide plates. J. Oral Maxillofac. Surg. 1998, 56, 614–615. [Google Scholar] [CrossRef]
- Bergsma, E.J.; Rozema, F.R.; Bos, R.R.; De Bruijn, W.C. Foreign body reactions to resorbable poly(l-lactide) bone plates and screws used for the fixation of unstable zygomatic fractures. J. Oral Maxillofac. Surg. 1993, 51, 666–670. [Google Scholar] [CrossRef]
- Sheikh, Z.; Najeeb, S.; Khurshid, Z.; Verma, V.; Rashid, H.; Glogauer, M. Biodegradable materials for bone repair and tissue engineering applications. Materials 2015, 8, 5744–5794. [Google Scholar] [CrossRef] [PubMed]
- Rokkanen, P.U.; Böstman, O.; Hirvensalo, E.; Mäkelä, E.; Partio, E.K.; Pätiälä, H.; Vainionpää, S.; Vihtonen, K.; Törmälä, P. Bioabsorbable fixation in orthopaedic surgery and traumatology. Biomaterials 2000, 21, 2607–2613. [Google Scholar] [CrossRef]
- Leno, M.B.; Liu, S.Y.; Chen, C.-T.; Liao, H.-T. Comparison of functional outcomes and patient-reported satisfaction between titanium and absorbable plates and screws for fixation of mandibular fractures: A one-year prospective study. J. Cranio-Maxillofac. Surg. 2017, 45, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Bayat, M.; Garajei, A.; Ghorbani, K.; Motamedi, M.H.K. Treatment of mandibular angle fractures using a single bioresorbable miniplate. J. Oral Maxillofac. Surg. 2010, 68, 1573–1577. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H.; Han, H.-S.; Kim, Y.-C.; Lee, J.-Y.; Lee, B.-K. Stability of biodegradable metal (Mg–Ca–Zn alloy) screws compared with absorbable polymer and titanium screws for sagittal split ramus osteotomy of the mandible using the finite element analysis model. J. Cranio-Maxillofac. Surg. 2017, 45, 1639–1646. [Google Scholar] [CrossRef]
- Chocron, Y.; Azzi, A.J.; Cugno, S. Resorbable implants for mandibular fracture fixation. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2384. [Google Scholar] [CrossRef] [PubMed]
- Plaass, C.; Ettinger, S.; Sonnow, L.; Koenneker, S.; Noll, Y.; Weizbauer, A.; Reifenrath, J.; Claassen, L.; Daniilidis, K.; Stukenborg-Colsman, C.; et al. Early results using a biodegradable magnesium screw for modified chevron osteotomies. J. Orthop. Res. 2016, 34, 2207–2214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Tan, L.; Yu, X.; Etim, I.P.; Ibrahim, M.; Yang, K. Mechanical properties of magnesium alloys for medical application: A review. J. Mech. Behav. Biomed. Mater. 2018, 87, 68–79. [Google Scholar] [CrossRef]
- Neff, A.; Mühlberger, G.; Karoglan, M.; Kolk, A.; Mittelmeier, W.; Scheruhn, D. Stabilität der osteosynthese bei gelenkwalzenfrakturen in klinik und biomechanischer simulation. Mund- Kiefer- Und Gesichtschirurgie 2004, 8, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M. Small-diameter compression screws completely embedded in bone for rigid internal fixation of the condylar head of the mandible. Br. J. Oral Maxillofac. Surg. 2018, 56, 74–76. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Swiniarski, J. Treatment of high fracture of the neck of the mandibular condylar process by rigid fixation performed by lag screws: Finite element analysis. Dent. Med. Probl. 2017, 54, 223–228. [Google Scholar] [CrossRef] [Green Version]
- Kolk, A.; Neff, A. Long-term results of ORIF of condylar head fractures of the mandible: A prospective 5-year follow-up study of small-fragment positional-screw osteosynthesis (SFPSO). J. Cranio-Maxillofac. Surg. 2015, 43, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Skroch, L.; Fischer, I.; Meisgeier, A.; Kozolka, F.; Apitzsch, J.; Neff, A. Condylar remodeling after osteosynthesis of fractures of the condylar head or close to the temporomandibular joint. J. Cranio-Maxillofac. Surg. 2020, 48, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Snahnicanova, Z.; Loderer, D.; Sokol, J.; Staško, J.; Lasabova, Z.; Kubisz, P.; Simurda, T. Fibrinogen martin: A novel mutation in FGB (Gln180Stop) causing congenital afibrinogenemia. Semin. Thromb. Hemost. 2016, 42, 455–458. [Google Scholar] [CrossRef] [Green Version]




| Screw Type | Thread Diameter | Core Diameter | Thread Pitch | Material | Appearance |
|---|---|---|---|---|---|
| Magnesium (Mg20 screw) | 2.2 mm | 1.5 mm | 0.7 mm | MgYREZr |  |
| Titanium (W screw) | 1.7 mm | 1.1 mm | 0.7 mm | Ti6Al7Nb |  |
| Polymer (Absorbable screw) | 2.5 mm | 1.9 mm | 1.0 mm | PLGA |  |
| Parameter | Axial Pull-Out Force [N] | Maximal Torque [N·cm] | |||
|---|---|---|---|---|---|
| Polymer | Titanium | Magnesium | Titanium | Magnesium | |
| Average ± standard deviation | 138 ± 26.49 | 340 ± 15.92 | 399 ± 7.49 | 19 ± 0.82 | 16 ± 1.00 |
| Minimum | 80 | 317 | 387 | 18 | 14 |
| Maximum | 157 | 363 | 411 | 20 | 17 |
| Range | 77 | 46 | 24 | 2 | 3 |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozakiewicz, M. Are Magnesium Screws Proper for Mandibular Condyle Head Osteosynthesis? Materials 2020, 13, 2641. https://doi.org/10.3390/ma13112641
Kozakiewicz M. Are Magnesium Screws Proper for Mandibular Condyle Head Osteosynthesis? Materials. 2020; 13(11):2641. https://doi.org/10.3390/ma13112641
Chicago/Turabian StyleKozakiewicz, Marcin. 2020. "Are Magnesium Screws Proper for Mandibular Condyle Head Osteosynthesis?" Materials 13, no. 11: 2641. https://doi.org/10.3390/ma13112641





