Dental Aerosol as a Hazard Risk for Dental Workers
Abstract
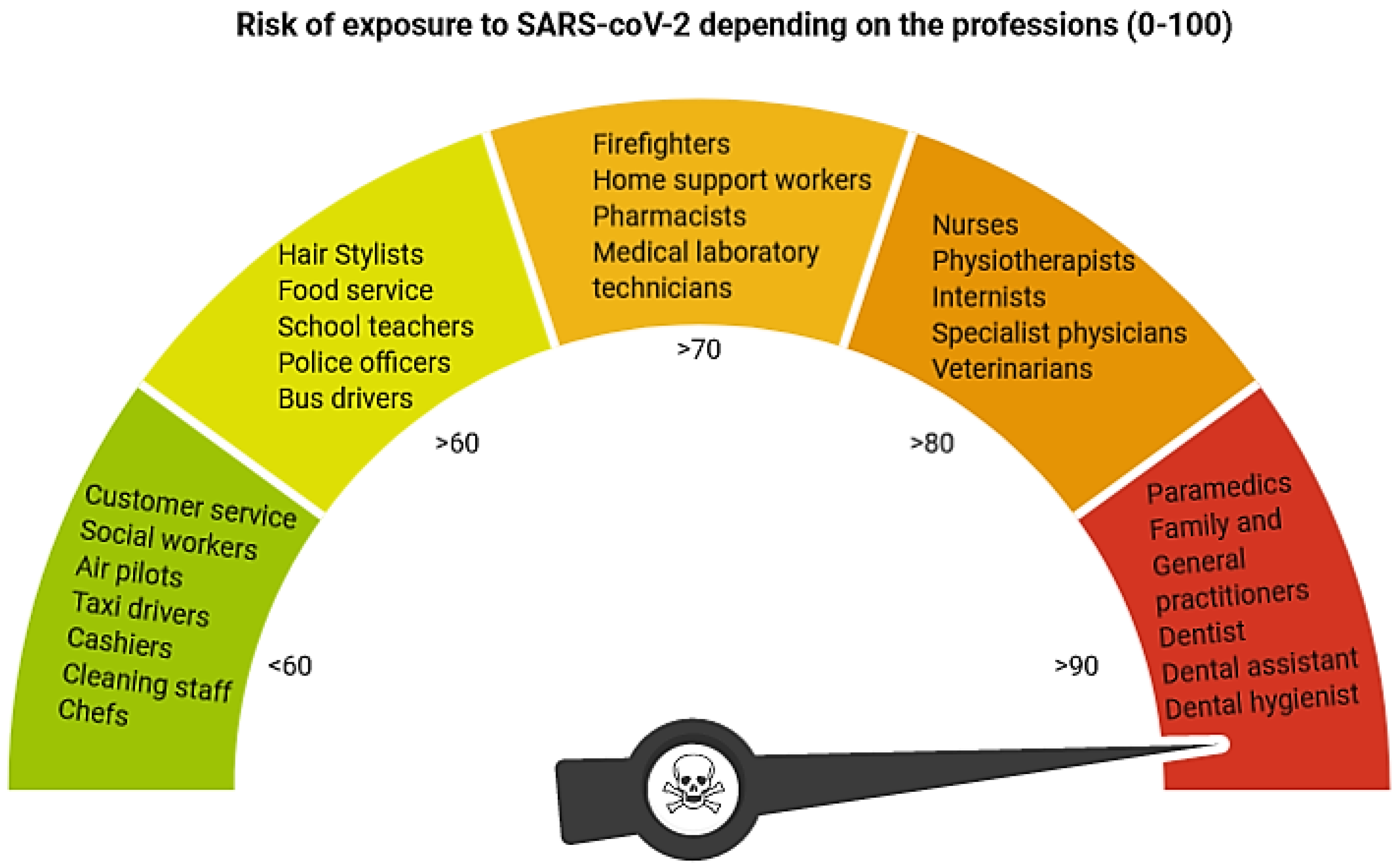
1. Introduction
2. Materials and Methods
2.1. Measurement Method
2.2. The Office Air Standardization
2.3. Suction Systems
- Saliva ejector EM15 (Monoart® Euronda, Vicenza, Italy);
- High volume evacuator EM19 EVO (Monoart® Euronda, Vicenza, Italy);
- Saliva ejector EM15 (Monoart® Euronda, Vicenza, Italy) with an extraoral vacuum (MAcURAY PRO, KTMAX Inc., Seoul, Korea);
- High volume evacuator EM19 EVO (Monoart® Euronda, Vicenza, Italy) with an extraoral vacuum (MAcURAY PRO, KTMAX Inc., Seoul, Korea);
- Zirc evacuator Mr. Thirsty One-step® (Loser, Zirc, Buffalo, USA);
- Customized high volume evacuator (white)—designed and prepared by the authors;
- Customized high volume evacuator (black)—designed and prepared by the authors.
2.4. Dental Procedures
- Treatment of caries class I with the round diamond bur (#014) with a high-speed handpiece W&H Synea TA-98LC (W&H, Bürmoos, Austria) and all seven suction modalities (Figure 4A–G). Working parameters: 200,000 RPM (revolutions per minute), water cooling: 30 mL/min;
- Treatment of caries class I with the round rose bur (#014) with a low-speed handpiece W&H Synea TA-98LC (W&H, Bürmoos, Austria) and saliva ejector EM15 or high volume evacuator EM19 EVO. Working parameters: 15,000 RPM (revolutions per minute), water cooling: 30 mL/min;
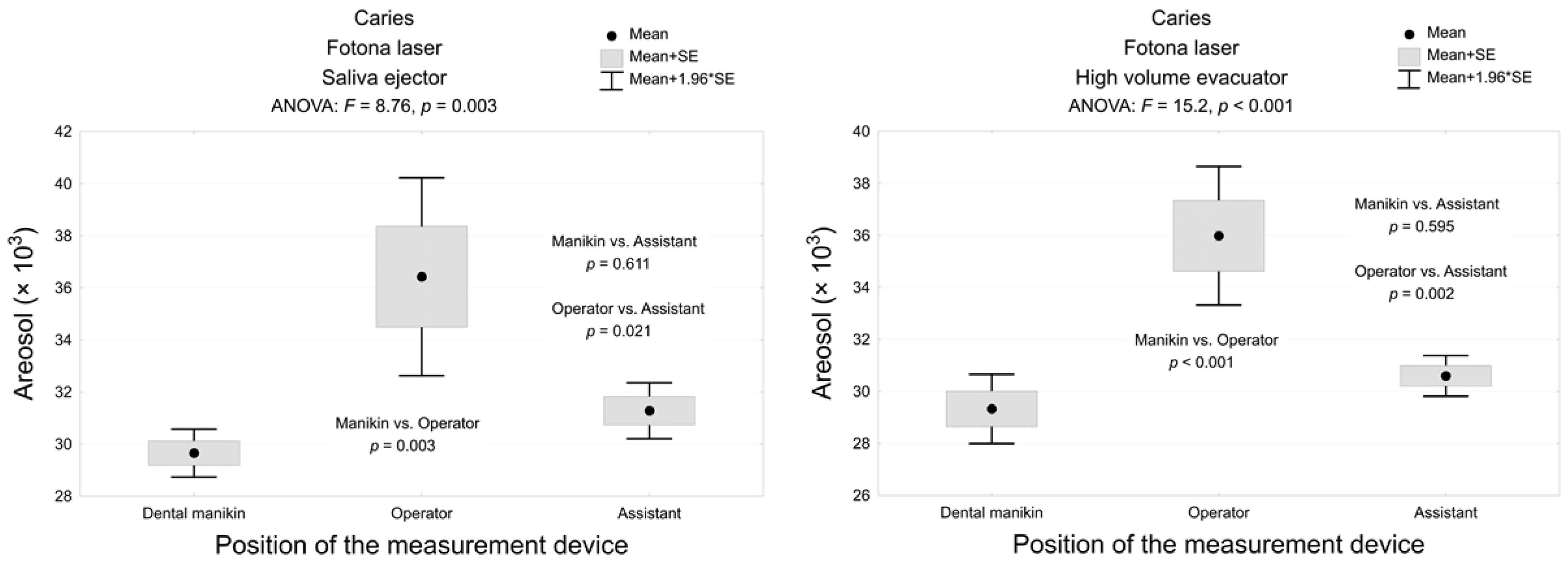
- Treatment of caries class I with 1 mm diameter sapphire tip with a handpiece H14 of Er:YAG laser (LightWalker, Fotona, Slovenia) and saliva ejector EM15 or high volume evacuator EM19 EVO. Laser parameters: energy 300 mJ, frequency 20 Hz, power 6 W, water/air coolant 6/4;
- Tooth polishing with silicone rubber dental bur (Kenda AG, Vaduz, Liechtenstein) with a low-speed handpiece W&H Synea TA-98LC (W&H, Bürmoos, Austria) at 1000 and 10,000 RPM (revolutions per minute) and saliva ejector EM15 or high volume evacuator EM19 EVO. Water cooling: 30 mL/min;
- Dental calculus removal using ultrasound scaler HW-3H (Woodpecker Medical Instrument Co., Ltd., Guilin, China) and saliva ejector EM15 or high volume evacuator EM19 EVO at a power of 30%, water cooling: 40 mL/min.
2.5. Statistical Analysis
3. Results
3.1. High Volume Evacuators Significantly Reduced the Aerosols during Caries Removal with the Use of a High-Speed Handpiece. The New Custom-Designed High Volume Evacuators and the Zirc® Evacuator Proved to be the Most Effective
3.2. High Volume Evacuator Significantly Reduced the Aerosols during Caries Removal with the Use of a Low-Speed Handpiece. The Low-Speed Handpiece Produced Less Aerosols than a High-Speed Turbine
3.3. Er:YAG Laser Significantly Reduced the Aerosols during Caries Removal as Compared with Classical Rotary Handpieces
3.4. Polishing the Tooth with Silicone Rubber Dental bur with a Low-Speed Contra-Angle Generated the Highest Amount of Aerosol Particles
3.5. Ultrasonic Scaling Generated Less Aerosols then Caries Removal and Tooth Polishing Using Conventional Rotary Handpieces and Traditional Suction Systems (Saliva Ejector and High Volume Evacuator)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- AFL. As Albertans Return to Work, Who Is at the Highest Risk of Exposure to the Novel Coronavirus? Available online: https://www.afl.org/as_albertans_return_to_work_who_is_at_the_highest_risk_of_exposure_to_the_novel_coronavirus (accessed on 10 August 2020).
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef]
- Miller, R.L. Characteristics of Blood-Containing Aerosols Generated by Common Powered Dental Instruments. Am. Ind. Hyg. Assoc. J. 1995, 56, 670–676. [Google Scholar] [CrossRef] [PubMed]
- Harrel, S.K.; Molinari, J. Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. J. Am. Dent. Assoc. 2004, 135, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Bentley, C.D.; Burkhart, N.W.; Crawford, J.J. Evaluating spatter and aerosol contamination during dental procedures. J. Am. Dent. Assoc. 1994, 125, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Coulthard, P. Dentistry and coronavirus (COVID-19)—Moral decision-making. Br. Dent. J. 2020, 228, 503–505. [Google Scholar] [CrossRef] [PubMed]
- Micik, R.E.; Miller, R.L.; Mazzarella, M.A.; Ryge, G. Studies on Dental Aerobiology: I. Bacterial Aerosols Generated during Dental Procedures. J. Dent. Res. 1969, 48, 49–56. [Google Scholar] [CrossRef]
- Garden, J.M.; Kerry O’Banion, M.; Bakus, A.D.; Olson, C. Viral disease transmitted by laser-generated plume (aerosol). Arch. Dermatol. 2002, 138, 1303–1307. [Google Scholar] [CrossRef]
- Garden, J.M.; O’Banion, M.K.; Shelnitz, L.S.; Pinski, K.S.; Bakus, A.D.; Reichmann, M.E.; Sundberg, J.P. Papillomavirus in the Vapor of Carbon Dioxide Laser-Treated Verrucae. J. Urol. 1989, 141, 223–224. [Google Scholar] [CrossRef]
- Hughes, P.S.H.; Hughes, A.P. Absence of human papillomavirus DNA in the plume of erbium:YAG laser-treated warts. J. Am. Acad. Dermatol. 1998, 38, 426–428. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Nowicka, J.; Pajączkowska, M.; Matys, J.; Szymonowicz, M.; Kuropka, P.; Rybak, Z.; Dobrzyński, M.; Dominiak, M. Effects of Nd:YAG laser irradiation on the growth of Candida albicans and Streptococcus mutans: in vitro study. Lasers Med. Sci. 2019, 34, 129–137. [Google Scholar] [CrossRef]
- Flieger, R.; Gedrange, T.; Grzech-Leśniak, K.; Dominiak, M.; Matys, J. Low-Level Laser Therapy with a 635 nm Diode Laser Affects Orthodontic Mini-Implants Stability: A Randomized Clinical Split-Mouth Trial. J. Clin. Med. 2019, 9, 112. [Google Scholar] [CrossRef] [PubMed]
- Nammour, S.; El Mobadder, M.; Maalouf, E.; Namour, M.; Namour, A.; Rey, G.; Matamba, P.; Matys, J.; Zeinoun, T.; Grzech-Leśniak, K. Clinical Evaluation of Diode (980 nm) Laser-Assisted Nonsurgical Periodontal Pocket Therapy: A Randomized Comparative Clinical Trial and Bacteriological Study. Photobiomodul. Photomed. Laser Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Grzech-Leśniak, K.; Flieger, R.; Dominiak, M. Assessment of an impact of a diode laser mode with wavelength of 980 nm on a temperature rise measured by means of k-02 thermocouple: Preliminary results. Dent. Med. Probl. 2016, 53, 341–351. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K. Making Use of Lasers in Periodontal Treatment: A New Gold Standard? Photomed. Laser Surg. 2017, 35, 513–514. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Jurczyszyn, K.; Ziółkowski, P.; Dominiak, M.; Brugnera, A., Jr.; Romeo, U. Histological and Thermometric Examination of Soft Tissue De-Epithelialization Using Digitally Controlled Er:YAG Laser Handpiece: An Ex Vivo Study. Photomed Laser Surg. 2018, 36, 313–319. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Gaspirc, B.; Sculean, A. Clinical and microbiological effects of multiple applications of antibacterial photodynamic therapy in periodontal maintenance patients. A randomized controlled clinical study. Photodiagnosis Photodyn. Ther. 2019, 27, 44–50. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Dominiak, M. Comparison of the clinical and microbiological effects of antibiotic therapy in periodontal pockets following laser treatment: An in vivo study. Adv. Clin. Exp. Med. 2018, 27, 1263–1270. [Google Scholar] [CrossRef]
- Deeb, J.G.; Grzech-Leśniak, K.; Weaver, C.; Matys, J.; Bencharit, S. Retrieval of Glass Fiber Post Using Er:YAG Laser and Conventional Endodontic Ultrasonic Method: An In Vitro Study. J Prosthodont. 2019, 28, 1024–1028. [Google Scholar] [CrossRef]
- Matys, J.; Flieger, R.; Dominiak, M. Assessment of Temperature Rise and Time of Alveolar Ridge Splitting by Means of Er:YAG Laser, Piezosurgery, and Surgical Saw: An Ex Vivo Study. Biomed. Res. Int. 2016, 2016, 1–8. [Google Scholar] [CrossRef]
- Zakrzewski, W.; Dobrzynski, M.; Kuropka, P.; Matys, J.; Malecka, M.; Kiryk, J.; Rybak, Z.; Dominiak, M.; Grzech-Leśniak, K.; Wiglusz, K.; et al. Removal of Composite Restoration from the Root Surface in the Cervical Region Using Er: YAG Laser and Drill-In Vitro Study. Materials 2020, 7, 3027. [Google Scholar] [CrossRef]
- Matys, J.; Romeo, U.; Mroczka, K.; Grzech-Leśniak, K.; Dominiak, M. Temperature Changes and SEM Effects of Three Different Implants-Abutment Connection during Debridement with Er:YAG Laser: An Ex Vivo Study. Materials 2019, 14, 3748. [Google Scholar] [CrossRef]
- Flieger, R.; Matys, J.; Dominiak, M. The best time for orthodontic treatment for Polish children based on skeletal age analysis in accordance to refund policy of the Polish National Health Fund (NFZ). Adv. Clin. Exp. Med. 2018, 27, 1377–1382. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Bencharit, S.; Dalal, N.; Mroczka, K.; Deeb, J.G. In Vitro Examination of the Use of Er:YAG Laser to Retrieve Lithium Disilicate Crowns from Titanium Implant Abutments. J. Prosthodont. 2019, 28, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Deeb, J.G.; Bencharit, S.; Dalal, N.; Abdulmajeed, A.; Grzech-Leśniak, K. Using Er:YAG laser to remove lithium disilicate crowns from zirconia implant abutments: An in vitro study. PLoS ONE 2019, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Matys, J.; Zmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Brugnera, A.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Sculean, A.; Gašpirc, B. Laser reduction of specific microorganisms in the periodontal pocket using Er:YAG and Nd:YAG lasers: a randomized controlled clinical study. Lasers Med. Sci. 2018, 33, 1461–1470. [Google Scholar] [CrossRef] [PubMed]
- Tsen, S.; Chapa, T.; Beatty, W.; Xu, B.; Tsen, K.; Achilefu, S. Ultrashort pulsed laser treatment inactivates viruses by inhibiting viral replication and transcription in the host nucleus. Antiviral Res. 2014, 110, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Fekrazad, R. Photobiomodulation and Antiviral Photodynamic Therapy as a Possible Novel Approach in COVID-19 Management. Photobiomod. Photomed. Laser Surg. 2020, 38, 1–3. [Google Scholar] [CrossRef]
- Schikora, D.; Hepburn, J.; Plavin, S. Reduction of the Viral Load by Non-Invasive Photodynamic Therapy in Early Stages of COVID-19 infection. Am J Viro Dis. 2020, 2, 1–5. [Google Scholar]
- Atkinson, J.; Chartier, Y.; Lúcia Pessoa-Silva, C.; Jensen, P.; Li, Y.; Seto, W.-H. Natural Ventilation for Infection Control in Health-Care Settings WHO Library Cataloguing-in-Publication Data: Natural Ventilation for Infection Control in Health-Care Settings; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Carter, W.J.; Seal, J.R. Upper Respiratory Infections in Dental Personnel and Their Patients; Research Project Report NMOO50511403. Naval Medical Research Unit No.4; Administrative Command, US Naval Training Center: Great Lakes, IL, USA, 1953. [Google Scholar]
- WHO. Infection Prevention and Control of Epidemic-and Pandemic Prone Acute Respiratory Infections in Health Care; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Matys, J.; Grzech-Leśniak, K.; Dominiak, M. Disinfectants and devices for surface and air disinfection in dental offices. J. Stomatol. 2020, 73, 200–205. [Google Scholar] [CrossRef]
- Seto, W.H. Airborne transmission and precautions: Facts and myths. J. Hosp. Infect. 2015, 89, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Jacks, M.E. A laboratory comparison of evacuation devices on aerosol reduction. J Dent Hyg. 2002, 76, 202–206. [Google Scholar] [PubMed]
- Szymańska, J. Dental bioaerosol as an occupational hazard in a dentist’s workplace. Ann. Agric. Environ. Med. 2007, 14, 203–207. [Google Scholar]
- Liu, M.H.; Chen, C.T.; Chuang, L.C.; Lin, W.M.; Wan, G.H. Removal efficiency of central vacuum system and protective masks to suspended particles from dental treatment. PLoS ONE 2019, 14, e0225644. [Google Scholar] [CrossRef]
- Sotiriou, M.; Ferguson, S.F.; Davey, M.; Wolfson, J.M.; Demokritou, P.; Lawrence, J.; Sax, S.N.; Koutrakis, P. Measurement of particle concentrations in a dental office. Environ. Monit. Assess. 2008, 137, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Graetz, C.; Plaumann, A.; Tillner, A.; Salzer, S.; Bielfeldt, J.; Dorfer, C. Efficacy versus health risks: An in vitro evaluation of power-driven scalers. J. Indian Soc. Periodontol. 2015, 19, 18. [Google Scholar] [CrossRef] [PubMed]
- Harrel, S.K.; Barnes, J.B.; Rivera-Hidalgo, F. Aerosol and Splatter Contamination from the Operative Site during Ultrasonic Scaling. J. Am. Dent. Assoc. 1998, 129, 1241–1249. [Google Scholar] [CrossRef]
- Guderian, D.B.; Loth, A.G.; Weiß, R.; Diensthuber, M.; Stöver, T.; Leinung, M. In vitro comparison of surgical techniques in times of the SARS-CoV-2 pandemic: electrocautery generates more droplets and aerosol than laser surgery or drilling. Eur. Arch. Oto-Rhino-Laryngol. 2020, 1, 3. [Google Scholar]
- Siddique, I.; Mahmood, H.; Mohammed-Ali, R. Paracetamol overdose secondary to dental pain: a case series. Br. Dent. J. 2015, 219, e6. [Google Scholar] [CrossRef]




| Procedure | Tools | Exhaustion | Place of Measurement | ANOVA p | ||
|---|---|---|---|---|---|---|
| Manikin (A) | Operator (B) | Assistant (C) | ||||
| Caries | High-speed handpiece | Saliva ejector | 260.2 ± 20.6 | 121.2 ± 20.8 | 121.5 ± 9.5 | A vs. BC p < 0.001 |
| Saliva ejector + extraoral vacuum | 120.3 ± 18.3 | 43.9 ± 2.6 | 35.1 ± 1.6 | A vs. BC p < 0.001 | ||
| High volume evacuator | 60.5 ± 3.0 | 40.7 ± 3.3 | 31.5 ± 2.4 | A vs. BC p < 0.001 B vs. C p < 0.001 | ||
| High volume evacuator + extraoral vacuum | 40.7 ± 0.9 | 43.9 ± 1.9 | 44.5 ± 1.8 | A vs. BC p < 0.01 | ||
| Zirc evacuator | 32.1 ± 2.0 | 31.0 ± 1.4 | 31.0 ± 1.0 | 0.353 | ||
| New high volume evacuator—black | 31.6 ± 1.1 | 31.5 ± 1.1 | 31.5 ± 0.8 | 0.979 | ||
| New high volume evacuator—white | 31.5 ± 0.9 | 34.0 ± 1.2 | 31.2 ± 1.0 | B vs. AC p < 0.001 | ||
| Place of Measurement | Tooth Polishing Procedure with the Low-Speed Handpiece | |||||
|---|---|---|---|---|---|---|
| 1000 rpm | 10000 rpm | |||||
| Saliva Ejector | High Volume Evacuator | p-Value | Saliva Ejector | High Volume Evacuator | p-Value | |
| Manikin | 345.7 ± 65.8 | 201.0 ± 13.9 | <0.001 | 330.1 ± 40.3 | 79.7 ± 3.1 | <0.001 |
| Operator | 37.9 ± 2.3 | 34.6 ± 3.1 | 0.063 | 35.3 ± 6.9 | 34.5 ± 1.9 | 0.814 |
| Assistant | 31.6 ± 1.0 | 31.8 ± 1.5 | 0.803 | 32.7 ± 2.8 | 30.9 ± 1.3 | 0.192 |
| <0.001 | <0.001 | <0.001 | <0.001 | |||
| Place of Measurement | Exhaustion | Test Result | |
|---|---|---|---|
| Saliva Ejector | High Volume Evacuator | ||
| Manikin | 34.2 ± 2.8 | 29.7 ± 1.4 | 0.005 |
| Operator | 32.5 ± 2.3 | 28.4 ± 1.2 | 0.003 |
| Assistant | 31.0 ± 1.6 | 29.6 ± 0.6 | 0.079 |
| ANOVA p | 0.072 | 0.139 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matys, J.; Grzech-Leśniak, K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials 2020, 13, 5109. https://doi.org/10.3390/ma13225109
Matys J, Grzech-Leśniak K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials. 2020; 13(22):5109. https://doi.org/10.3390/ma13225109
Chicago/Turabian StyleMatys, Jacek, and Kinga Grzech-Leśniak. 2020. "Dental Aerosol as a Hazard Risk for Dental Workers" Materials 13, no. 22: 5109. https://doi.org/10.3390/ma13225109
APA StyleMatys, J., & Grzech-Leśniak, K. (2020). Dental Aerosol as a Hazard Risk for Dental Workers. Materials, 13(22), 5109. https://doi.org/10.3390/ma13225109






