Effects of Intrabony Length and Cortical Bone Density on the Primary Stability of Orthodontic Miniscrews
Abstract
:1. Introduction
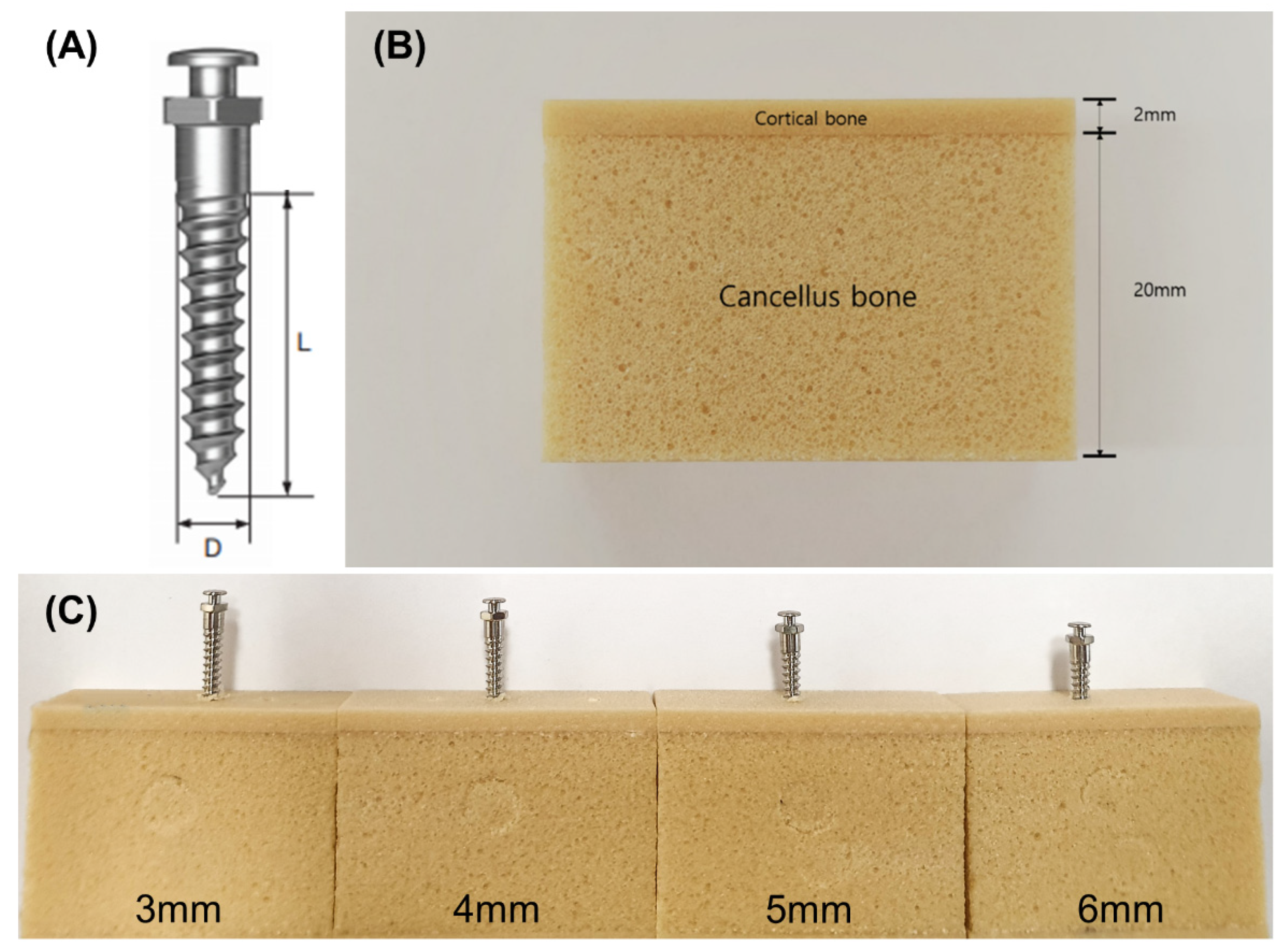
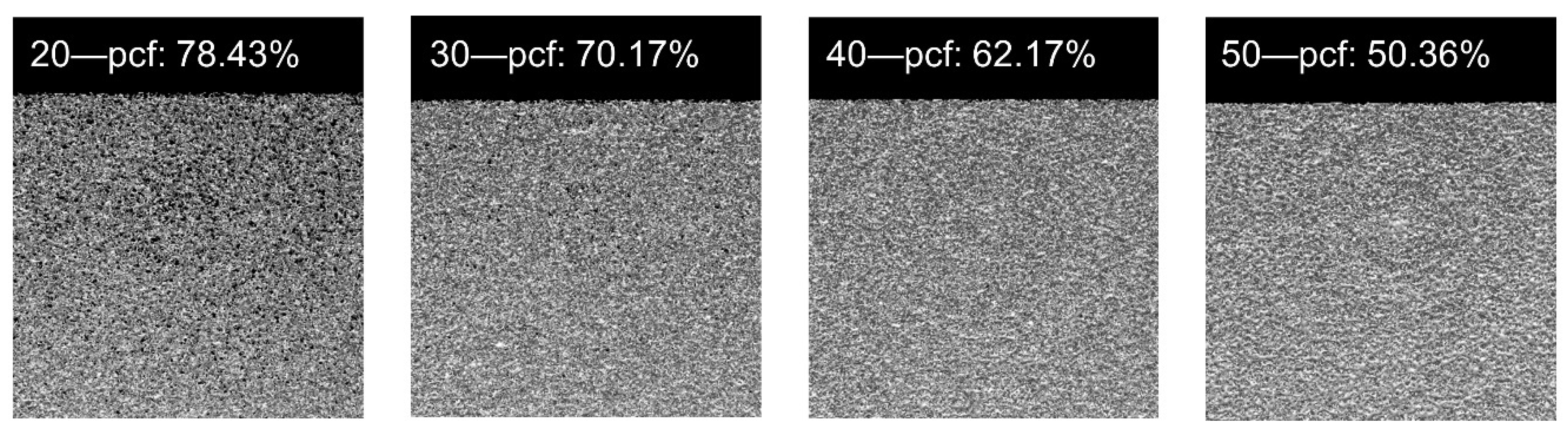
2. Materials and Methods
2.1. Materials
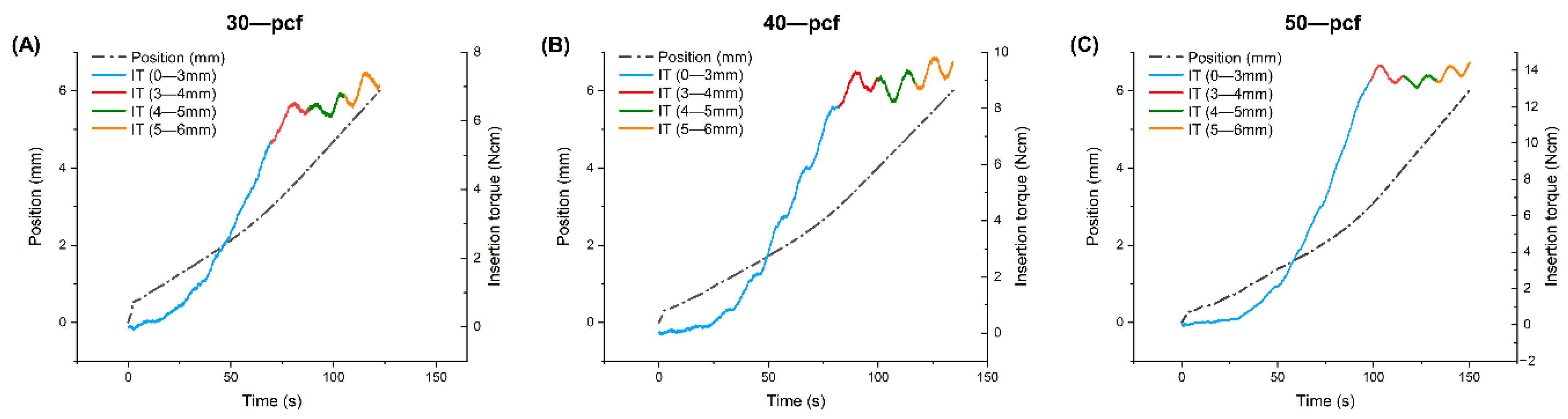
2.2. Torque
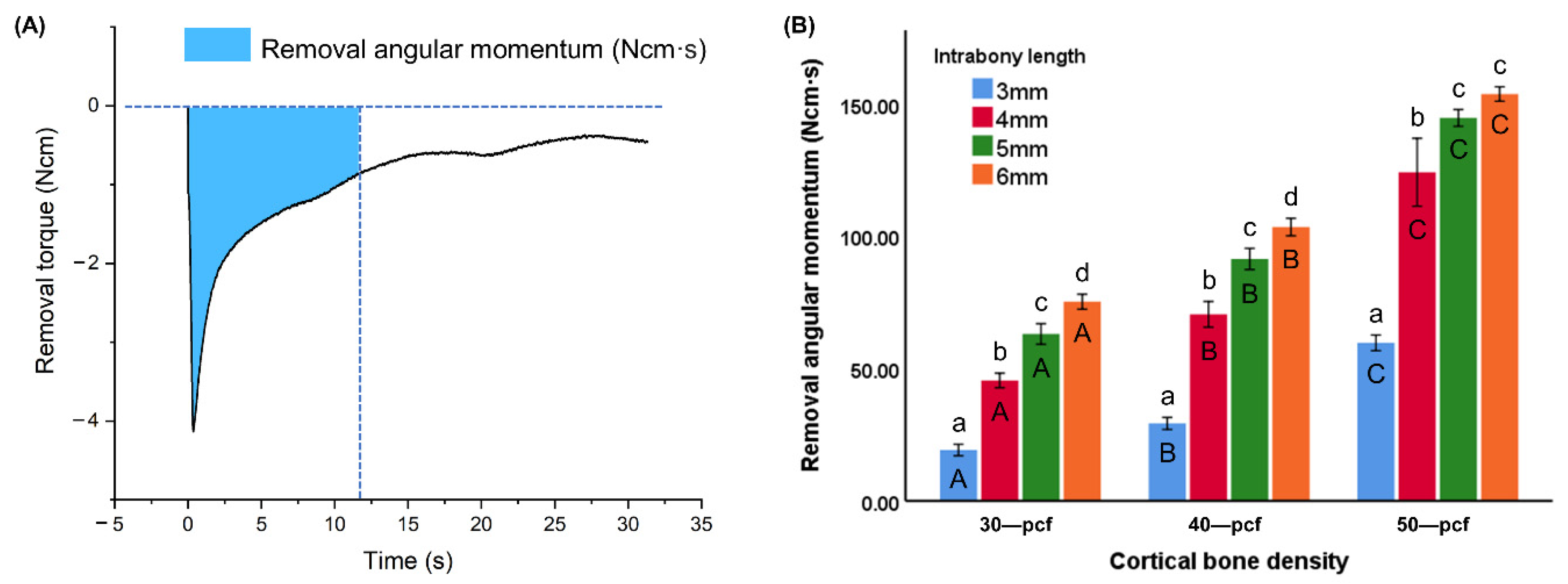
2.3. Removal Angular Momentum
2.4. Horizontal Resistance
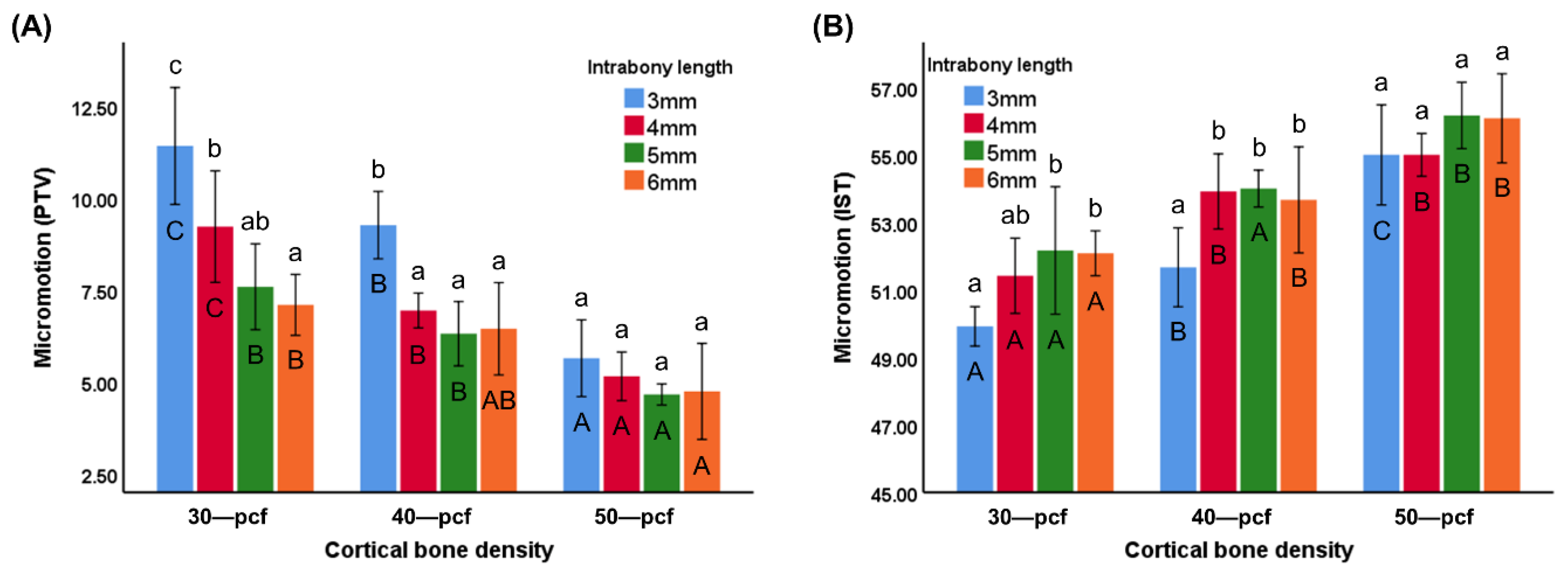
2.5. Micromotion
2.6. Statistical Analysis
3. Results
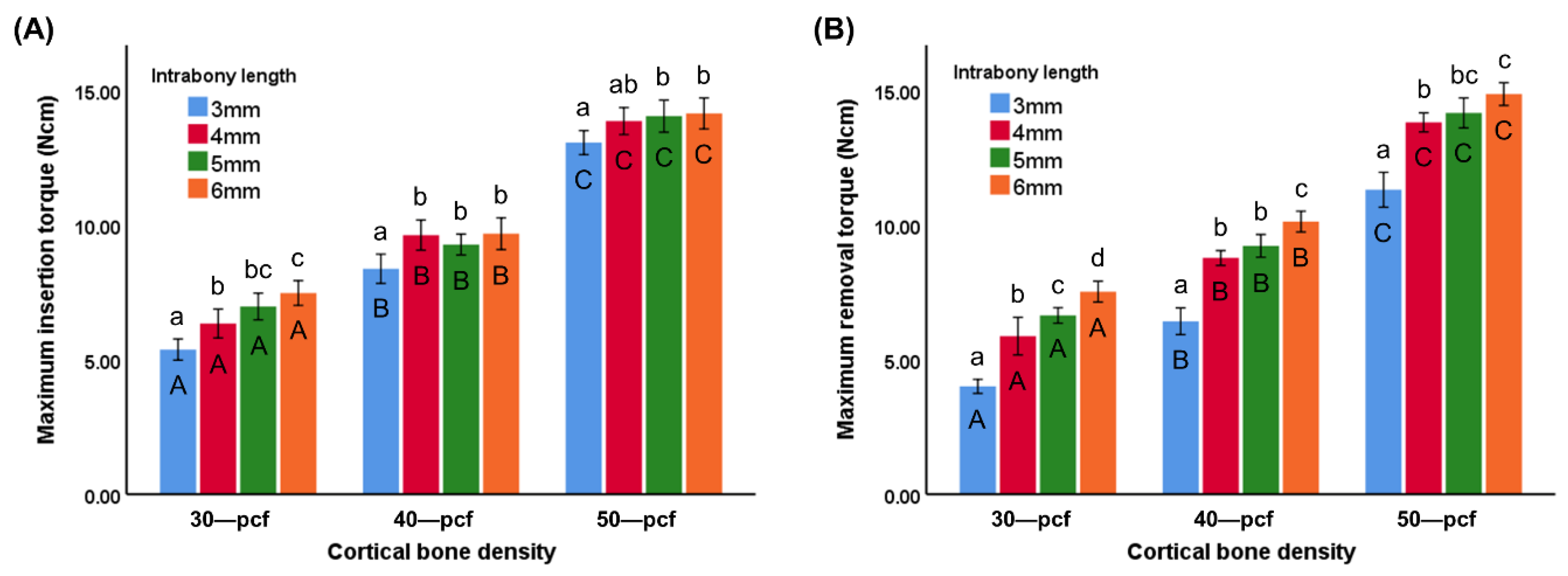
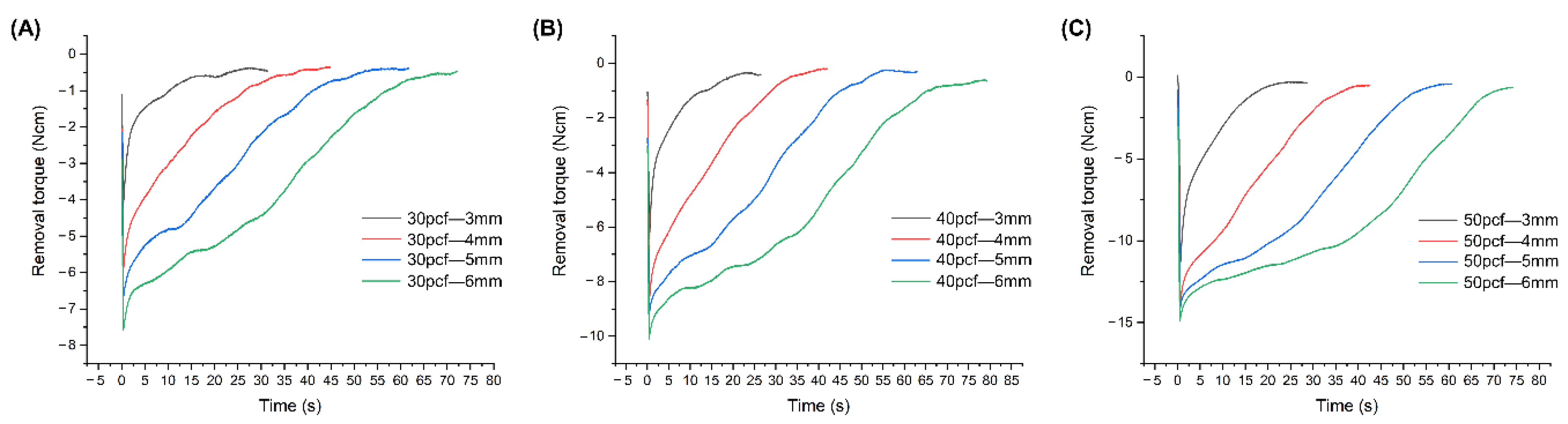
3.1. Torque
3.2. Removal Angular Momentum
3.3. Horizontal Resistance
3.4. Micromotion
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bourassa, C.; Hosein, Y.K.; Pollmann, S.I.; Galil, K.; Bohay, R.N.; Holdsworth, D.W.; Tassi, A. In vitro comparison of different palatal sites for orthodontic miniscrew insertion: Effect of bone quality and quantity on primary stability. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 809–819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motoyoshi, M.; Hirabayashi, M.; Uemura, M.; Shimizu, N. Recommended placement torque when tightening an orthodontic mini-implant. Clin. Oral Implant. Res. 2006, 17, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Jeong, S.H.; Kwon, O.W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.H.; Hwang, C.J. Factors Affecting the Failure of TADs and Efforts to Improve the Biomechanical Stability of TADs. Tempor. Anchorage Devices Clin. Orthod. 2020, 61–67. [Google Scholar] [CrossRef]
- Migliorati, M.; Benedicenti, S.; Signori, A.; Drago, S.; Barberis, F.; Tournier, H.; Silvestrini-Biavati, A. Miniscrew design and bone characteristics: An experimental study of primary stability. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 228–234. [Google Scholar] [CrossRef]
- Huja, S.S.; Katona, T.R.; Burr, D.B.; Garetto, L.P.; Roberts, W.E. Microdamage adjacent to endosseous implants. Bone 1999, 25, 217–222. [Google Scholar] [CrossRef]
- Martin, R.B. Fatigue microdamage as an essential element of bone mechanics and biology. Calcif. Tissue Int. 2003, 73, 101–107. [Google Scholar] [CrossRef]
- Suzuki, M.; Deguchi, T.; Watanabe, H.; Seiryu, M.; Iikubo, M.; Sasano, T.; Fujiyama, K.; Takano-Yamamoto, T. Evaluation of optimal length and insertion torque for miniscrews. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 251–259. [Google Scholar] [CrossRef]
- Lee, K.J.; Joo, E.; Kim, K.D.; Lee, J.S.; Park, Y.C.; Yu, H.S. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 486–494. [Google Scholar] [CrossRef]
- Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.M.; Takano-Yamamoto, T. Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 9–15. [Google Scholar] [CrossRef]
- Lim, H.J.; Choi, Y.J.; Evans, C.A.; Hwang, H.S. Predictors of initial stability of orthodontic miniscrew implants. Eur. J. Orthod. 2011, 33, 528–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calvert, K.L.; Trumble, K.P.; Webster, T.J.; Kirkpatrick, L.A. Characterization of commercial rigid polyurethane foams used as bone analogs for implant testing. J. Mater. Sci. Mater. Med. 2010, 21, 1453–1461. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.J.; Jung, K.Y.; Choi, Y.J.; Kim, K.H. Biomechanical characteristics and reinsertion guidelines for retrieved orthodontic miniscrews. Angle Orthod. 2014, 84, 878–884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hergel, C.A.; Acar, Y.B.; Ates, M.; Kucukkeles, N. In vitro evaluation of the effects of insertion and sterilization procedures on the mechanical and surface characteristics of mini screws. Eur. Oral Res. 2019, 53, 25–31. [Google Scholar] [CrossRef]
- Devlin, H.; Horner, K.; Ledgerton, D. A comparison of maxillary and mandibular bone mineral densities. J. Prosthet. Dent. 1998, 79, 323–327. [Google Scholar] [CrossRef]
- Kido, H.; Schulz, E.E.; Kumar, A.; Lozada, J.; Saha, S. Implant diameter and bone density: Effect on initial stability and pull-out resistance. J. Oral Implantol. 1997, 23, 163–169. [Google Scholar]
- Eliades, T.; Zinelis, S.; Papadopoulos, M.A.; Eliades, G. Characterization of retrieved orthodontic miniscrew implants. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 10–17.e11. [Google Scholar] [CrossRef]
- Kim, G.T.; Jin, J.; Mangal, U.; Lee, K.J.; Kim, K.M.; Choi, S.H.; Kwon, J.S. Primary Stability of Orthodontic Titanium Miniscrews due to Cortical Bone Density and Re-Insertion. Materials 2020, 13, 4433. [Google Scholar] [CrossRef]
- Nienkemper, M.; Santel, N.; Honscheid, R.; Drescher, D. Orthodontic mini-implant stability at different insertion depths: Sensitivity of three stability measurement methods. J. Orofac. Orthop. 2016, 77, 296–303. [Google Scholar] [CrossRef]
- Kang, S.-Y.; Yu, J.-M.; Kim, H.-S.; Lee, J.-S.; Yeon, C.-M.; Park, K.-S.; Choi, S.-H.; Lee, S.-Y. Influence of Orthodontic Anchor Screw Anchorage Method on the Stability of Artificial Bone: An In vitro Study. Materials 2020, 13, 3205. [Google Scholar] [CrossRef]
- Yu, J.-H. Mechanical effects of micro-thread orthodontic mini-screw design on artificial cortical bone. J. Med. Biol. Eng. 2014, 34, 49–55. [Google Scholar] [CrossRef]
- Lee, J.; Pyo, S.W.; Cho, H.J.; An, J.S.; Lee, J.H.; Koo, K.T.; Lee, Y.M. Comparison of implant stability measurements between a resonance frequency analysis device and a modified damping capacity analysis device: An in vitro study. J. Periodontal. Implant. Sci. 2020, 50, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.H.; Cha, J.Y.; Joo, U.H.; Hwang, C.J. Surface changes of anodic oxidized orthodontic titanium miniscrew. Angle Orthod. 2012, 82, 522–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, S.A.; Cha, J.Y.; Hwang, C.J. Insertion torque of orthodontic miniscrews according to changes in shape, diameter and length. Angle Orthod. 2008, 78, 234–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miyamoto, I.; Tsuboi, Y.; Wada, E.; Suwa, H.; Iizuka, T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery—Clinical, prospective, biomechanical, and imaging study. Bone 2005, 37, 776–780. [Google Scholar] [CrossRef]
- Miyawaki, S.; Koyama, I.; Inoue, M.; Mishima, K.; Sugahara, T.; Takano-Yamamoto, T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 373–378. [Google Scholar] [CrossRef]
- Wilmes, B.; Ottenstreuer, S.; Su, Y.Y.; Drescher, D. Impact of implant design on primary stability of orthodontic mini-implants. J. Orofac. Orthop. 2008, 69, 42–50. [Google Scholar] [CrossRef]
- Wilmes, B.; Rademacher, C.; Olthoff, G.; Drescher, D. Parameters affecting primary stability of orthodontic mini-implants. J. Orofac. Orthop. 2006, 67, 162–174. [Google Scholar] [CrossRef]
- Baumgaertel, S.; Hans, M.G. Assessment of infrazygomatic bone depth for mini-screw insertion. Clin. Oral Implant. Res. 2009, 20, 638–642. [Google Scholar] [CrossRef]
- Al Maaitah, E.F.; Safi, A.A.; Abdelhafez, R.S. Alveolar bone density changes around miniscrews: A prospective clinical study. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 758–767. [Google Scholar] [CrossRef]
- Tepedino, M.; Masedu, F.; Chimenti, C. Comparative evaluation of insertion torque and mechanical stability for self-tapping and self-drilling orthodontic miniscrews—An in vitro study. Head Face Med. 2017, 13, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldmann, A.; Schweizer, M.; Stucki, S.; Nolte, L. Experimental evaluation of cortical bone substitute materials for tool development, surgical training and drill bit wear investigations. Med. Eng. Phys. 2019, 66, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.T.; Fuh, L.J.; Tu, M.G.; Li, Y.F.; Chen, K.T.; Huang, H.L. The effects of cortical bone thickness and trabecular bone strength on noninvasive measures of the implant primary stability using synthetic bone models. Clin. Implant. Dent. Relat. Res. 2013, 15, 251–261. [Google Scholar] [CrossRef]
- Lettry, S.; Seedhom, B.B.; Berry, E.; Cuppone, M. Quality assessment of the cortical bone of the human mandible. Bone 2003, 32, 35–44. [Google Scholar] [CrossRef]
- Marquezan, M.; Lima, I.; Lopes, R.T.; Sant’Anna, E.F.; de Souza, M.M. Is trabecular bone related to primary stability of miniscrews? Angle Orthod. 2014, 84, 500–507. [Google Scholar] [CrossRef] [Green Version]
- Trisi, P.; Perfetti, G.; Baldoni, E.; Berardi, D.; Colagiovanni, M.; Scogna, G. Implant micromotion is related to peak insertion torque and bone density. Clin. Oral Implant. Res. 2009, 20, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Mogra, S.; Shetty, V.S.; Shetty, S.; Philip, P. Three-dimensional finite element analysis of strength, stability, and stress distribution in orthodontic anchorage: A conical, self-drilling miniscrew implant system. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 327–336. [Google Scholar] [CrossRef]
- McManus, M.M.; Qian, F.; Grosland, N.M.; Marshall, S.D.; Southard, T.E. Effect of miniscrew placement torque on resistance to miniscrew movement under load. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e93–e98. [Google Scholar] [CrossRef]
- Dalstra, M.; Cattaneo, P.; Melsen, B.J.O. Load transfer of miniscrews for orthodontic anchorage. Orthodontics 2004, 1, 53–62. [Google Scholar]
- Gallas, M.M.; Abeleira, M.T.; Fernández, J.R.; Burguera, M. Three-dimensional numerical simulation of dental implants as orthodontic anchorage. Eur. J. Orthod. 2005, 27, 12–16. [Google Scholar] [CrossRef]
- Chen, Y.J.; Chen, Y.H.; Lin, L.D.; Yao, C.C. Removal torque of miniscrews used for orthodontic anchorage—A preliminary report. Int. J. Oral Maxillofac. Implant. 2006, 21, 283–289. [Google Scholar]


| Density | Compression | Tension | |||
|---|---|---|---|---|---|
| pcf | (g/cc) | Strength (MPa) | Modulus (MPa) | Strength (MPa) | Modulus (MPa) |
| 20 | 0.32 | 8.4 | 210 | 5.6 | 284 |
| 30 | 0.48 | 18 | 445 | 12 | 592 |
| 40 | 0.64 | 31 | 759 | 19 | 1000 |
| 50 | 0.80 | 48 | 1148 | 27 | 1469 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, J.; Kim, G.-T.; Kwon, J.-S.; Choi, S.-H. Effects of Intrabony Length and Cortical Bone Density on the Primary Stability of Orthodontic Miniscrews. Materials 2020, 13, 5615. https://doi.org/10.3390/ma13245615
Jin J, Kim G-T, Kwon J-S, Choi S-H. Effects of Intrabony Length and Cortical Bone Density on the Primary Stability of Orthodontic Miniscrews. Materials. 2020; 13(24):5615. https://doi.org/10.3390/ma13245615
Chicago/Turabian StyleJin, Jie, Gi-Tae Kim, Jae-Sung Kwon, and Sung-Hwan Choi. 2020. "Effects of Intrabony Length and Cortical Bone Density on the Primary Stability of Orthodontic Miniscrews" Materials 13, no. 24: 5615. https://doi.org/10.3390/ma13245615







