Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies
Abstract
1. Introduction
2. Materials and Methods
- Population: patients rehabilitated with fixed implant-supported full-arch prostheses in one or both jaws.
- Intervention: fixed full-arch prothesis realized with any type of framework material (or monolithic prosthesis).
- Comparison: fixed full-arch prothesis realized with a different framework material.
- Outcomes: implant and prosthesis survival (iCSR and pCSR), bone resorption, biological and technical complications.
2.1. Search Strategy
- Minimum of 10 patients included;
- At least 1-year follow-up since prosthesis delivery;
- The framework material should be clearly indicated;
- Studies including the comparison of at least two different framework materials.
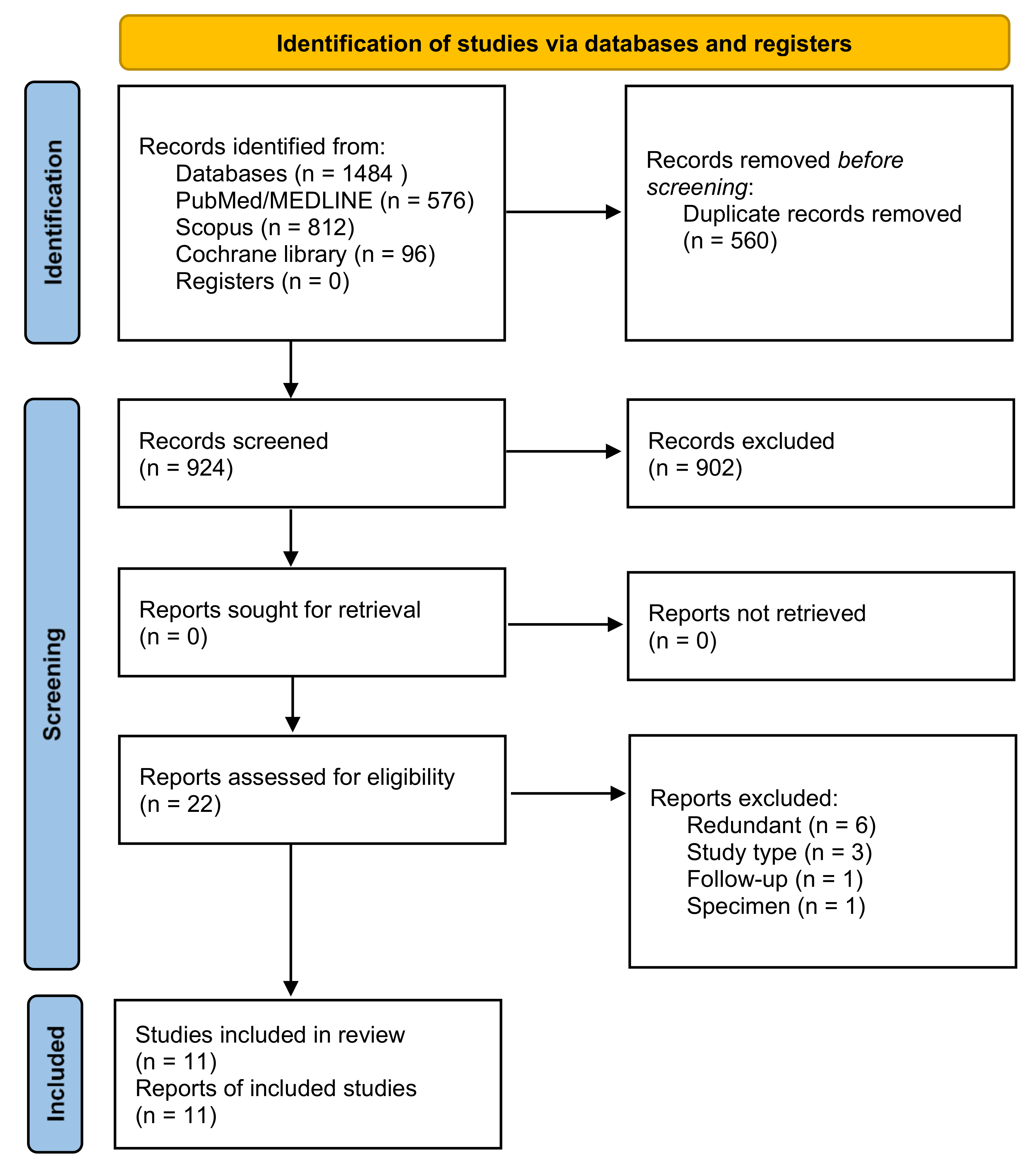
2.2. Screening and Selection
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Bibliographic Search and Study Selection
3.2. Description of the Included Studies
3.3. Excluded Studies
3.4. Quality Assessment
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Study | Reason for Exclusion |
|---|---|
| Jemt et al. 1998 | (redundant) |
| Bergendal and Palmquist 1995 | (redundant) |
| Ortorp et al. 2000 | (redundant) |
| Ortorp et al. 2002 | (redundant) |
| Ortorp et al. 2004 | (redundant) |
| Cannizzaro et al. 2014 | (redundant) |
| Pozzi et al. 2015 | (non-comparative) |
| Merli et al. 2017 | (insufficient follow-up) |
| Wolff et al. 2018 | (non-comparative) |
| Castorina et al. 2019 | (case report) |
| Hulterström et al. 1991 | (only one framework material tested) |
References
- Pera, P.; Menini, M.; Pesce, P.; Bevilacqua, M.; Pera, F.; Tealdo, T. Immediate Versus Delayed Loading of Dental Implants Supporting Fixed Full-Arch Maxillary Prostheses: A 10-year Follow-up Report. Int. J. Prosthodont. 2019, 32, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Sailer, I.; Zwahlen, M.; Hämmerle, C.H. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: Single crowns. Clin. Oral. Implant. Res. 2007, 18, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Pera, P. On immediately loaded fixed maxillary prostheses. Int. J. Prosthodont. 2014, 27, 513–516. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Menini, M.; Pesce, P.; Bevilacqua, M.; Pera, F.; Tealdo, T.; Barberis, F.; Pera, P. Effect of Framework in an Implant-Supported Full-Arch Fixed Prosthesis: 3D Finite Element Analysis. Int. J. Prosthodont. 2015, 28, 627–630. [Google Scholar] [CrossRef][Green Version]
- Wang, T.M.; Lee, M.S.; Wang, J.S.; Lin, L.D. The effect of implant design and bone quality on insertion torque, resonance frequency analysis, and insertion energy during implant placement in low or low- to medium-density bone. Int. J. Prosthodont. 2015, 28, 40–47. [Google Scholar] [CrossRef]
- Ogawa, S.; Dhaliwal, I.; Naert, A.; Mine, M.; Kronstrom, K.; Sasaki, J.; Duyck, J. Impact of implant number, distribution and prosthesis material on loading on implants supporting fixed prostheses. J. Oral. Rehabil. 2010, 37, 525–531. [Google Scholar] [CrossRef]
- Menini, M.; Pesce, P.; Pera, F.; Barberis, F.; Lagazzo, A.; Bertola, L.; Pera, P. Biological and mechanical characterization of carbon fiber frameworks for dental implant applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 70, 646–655. [Google Scholar] [CrossRef]
- Malo, P.; Nobre, M.d.A.; Borges, J.; Almeida, R. Retrievable metalceramic implant-supported fixed prostheses with milled titanium frameworks and all-ceramic crowns: Retrospective clinical study with up to 10 years of follow-up. J. Prosthodont. 2012, 21, 256–264. [Google Scholar] [CrossRef]
- Tiossi, R.; Gomes, É.A.; Faria, A.C.L.; Rodrigues, R.C.S.; Ribeiro, R.F. Biomechanical behavior of titanium and zirconia frameworks for implant-supported full-arch fixed dental prosthesis. Clin. Implant Dent. Relat. Res. 2017, 19, 860–866. [Google Scholar] [CrossRef]
- Kolgeci, L.; Mericske, E.; Worni, A.; Walker, P.; Katsoulis, J.; Mericske-Stern, R. Technical complications and failures of zirconia-based prostheses supported by implants followed up to 7 years: A case series. Int. J. Prosthodont. 2014, 27, 544–552. [Google Scholar] [CrossRef]
- Katsoulis, J.; Takeichi, T.; Sol Gaviria, A.; Peter, L.; Katsoulis, K. Misfit of implant prostheses and its impact on clinical outcomes. Definition, assessment and a systematic review of the literature. Eur. J. Oral. Implantol. 2017, 10, 121–138. [Google Scholar]
- Vallittu, P.K. An overview of development and status of fiber-reinforced composites as dental and medical biomaterials. Acta Biomater. Odontol. Scand. 2018, 4, 44–55. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated 11]. In The Cochrane Collaboration; Higgins, J.P.T., Green, S., Eds.; 20 March 2011; Available online: www.handbook.cochrane.org (accessed on 25 April 2021).
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2000; Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 25 April 2021).
- Jemt, T.; Bergendal, B.; Arvidsson, K.; Bergendal, T.; Karlsson, U.; Linden, B.; Palmqvist, S.; Rundcrantz, T.; Bergström, C. Laser-welded titanium frameworks supported by implants in the edentulous maxilla: A 2-year prospective multicenter study. Int. J. Prosthodont. 1998, 11, 551–557. [Google Scholar]
- Bergendal, B.; Palmqvist, S. Laser-welded titanium frameworks for fixed prostheses supported by osseointegrated implants: A 2-year multicenter study report. Int. J. Oral. Maxillofac. Implant. 1995, 10, 199–206. [Google Scholar]
- Ortorp, A.; Jemt, T. Clinical experiences of CNC-milled titanium frameworks supported by implants in the edentulous jaw: 1-year prospective study. Clin. Implant Dent. Relat. Res. 2000, 2, 2–9. [Google Scholar] [CrossRef]
- Ortorp, A.; Jemt, T. Clinical experience of CNC-milled titanium frameworks supported by implants in the edentulous jaw: A 3-year interim report. Clin. Implant Dent. Relat. Res. 2002, 4, 104–109. [Google Scholar] [CrossRef]
- Ortorp, A.; Jemt, T. Clinical experiences of computer numeric control-milled titanium frameworks supported by implants in the edentulous jaw: A 5-year prospective study. Clin. Implant Dent. Relat. Res. 2004, 6, 199–209. [Google Scholar] [CrossRef]
- Cannizzaro, G.; Felice, P.; Boveri, M.; Lazzarini, M.; Ferri, V.; Leone, M.; Esposito, M. Immediate loading of two flapless placed mandibular implants supporting cross-arch fixed prostheses: A 3-year follow-up prospective single cohort study. Eur J. Oral. Implantol. 2014, 7, 89–98. [Google Scholar]
- Pozzi, A.; Holst, S.; Fabbri, G.; Tallarico, M. Clinical reliability of CAD/CAM cross-arch zirconia bridges on immediately loaded implants placed with computer-assisted/template-guided surgery: A retrospective study with a follow-up between 3 and 5 years. Clin. Implant Dent. Relat. Res. 2015, 17, e86–e96. [Google Scholar] [CrossRef]
- Merli, M.; Bianchini, E.; Mariotti, G.; Moscatelli, M.; Piemontese, M.; Rappelli, G.; Nieri, M. Ceramic vs composite veneering of full arch implant-supported zirconium frameworks: Assessing patient preference and satisfaction. A crossover double-blind randomised controlled trial. Eur. J. Oral. Implantol. 2017, 10, 311–322. [Google Scholar]
- Wolff, D.; Wohlrab, T.; Saure, D.; Krisam, J.; Frese, C. Fiber-reinforced composite fixed dental prostheses: A 4-year prospective clinical trial evaluating survival, quality, and effects on surrounding periodontal tissues. J. Prosthet. Dent. 2018, 119, 47–52. [Google Scholar] [CrossRef]
- Castorina, G. Carbon-Fiber Framework for Full-Arch Implant-Supported Fixed Dental Prostheses Supporting Resin-Based Composite and Lithium Disilicate Ceramic Crowns: Case Report and Description of Features. Int. J. Periodontics Restor. Dent. 2019, 39, 175–184. [Google Scholar] [CrossRef]
- Hulterström, M.; Nilsson, U. Cobalt-chromium as a framework material in implant-supported fixed prostheses: A preliminary report. Int. J. Oral. Maxillofac. Implant. 1991, 6, 475–480. [Google Scholar]
- Bergendal, B.; Palmqvist, S. Laser-welded titanium frameworks for implant-supported fixed prostheses: A 5-year report. Int. J. Oral. Maxillofac. Implant. 1999, 14, 69–71. [Google Scholar]
- Jemt, T.; Bergendal, B.; Arvidson, K.; Bergendal, T.; Karlsson, L.D.; Linden, B.; Rundcrantz, T.; Wendelhag, I. Implant-supported welded titanium frameworks in the edentulous maxilla: A 5-year prospective multicenter study. Int. J. Prosthodont. 2002, 15, 544–548. [Google Scholar]
- Murphy, W.M.; Absi, E.G.; Gregory, M.C.; Williams, K.R. A prospective 5-year study of two cast framework alloys for fixed implant-supported mandibular prostheses. Int. J. Prosthodont. 2002, 15, 133–138. [Google Scholar]
- Ortorp, A.; Jemt, T. Early laser-welded titanium frameworks supported by implants in the edentulous mandible: A 15-year comparative follow-up study. Clin. Implant Dent. Relat. Res. 2009, 11, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Vinci, R.; Capparé, P.; Romanos, G.E.; Gherlone, E. A clinical study of edentulous patients rehabilitated according to the "all on four" immediate function protocol. Int. J. Oral. Maxillofac. Implant. 2012, 27, 428–434. [Google Scholar]
- Örtorp, A.; Jemt, T. CNC-milled titanium frameworks supported by Implant. in the edentulous jaw: A 10-year comparative clinical study. Clin. Implant Dent. Relat. Res. 2012, 14, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Tartaglia, G.M.; Maiorana, C.; Gallo, M.; Codari, M.; Sforza, C. Implant-Supported Immediately Loaded Full-Arch Rehabilitations: Comparison of Resin and Zirconia Clinical Outcomes in a 5-Year Retrospective Follow-Up Study. Implant Dent. 2016, 25, 74–82. [Google Scholar] [CrossRef]
- Cannizzaro, G.; Felice, P.; Lazzarini, M.; Ferri, V.; Leone, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate loading of two flapless placed mandibular Implant. supporting cross-arch fixed prostheses: A 5-year follow-up prospective single cohort study. Eur. J. Oral. Implantol. 2016, 9, 165–177. [Google Scholar]
- Pera, F.; Pesce, P.; Solimano, F.; Tealdo, T.; Pera, P.; Menini, M. Carbon fibre versus metal framework in full-arch immediate loading rehabilitations of the maxilla—A cohort clinical study. J. Oral. Rehabil. 2017, 44, 392–397. [Google Scholar] [CrossRef]
- Caramês, J.; Marques, D.; Malta Barbosa, J.; Moreira, A.; Crispim, P.; Chen, A. Full-arch implant-supported rehabilitations: A prospective study comparing porcelain-veneered zirconia frameworks to monolithic zirconia. Clin. Oral. Implant. Res. 2019, 30, 68–78. [Google Scholar] [CrossRef]
- Barootchi, S.; Askar, H.; Ravidà, A.; Gargallo-Albiol, J.; Travan, S.; Wang, H.L. Long-term Clinical Outcomes and Cost-Effectiveness of Full-Arch Implant-Supported Zirconia-Based and Metal-Acrylic Fixed Dental Prostheses: A Retrospective Analysis. Int. J. Oral. Maxillofac. Implant. 2020, 35, 395–405. [Google Scholar] [CrossRef]
- Skalak, R. Biomechanical considerations in osseointegrated prostheses. J. Prosthet. Dent. 1983, 49, 843–848. [Google Scholar] [CrossRef]
- Menini, M.; Conserva, E.; Tealdo, T.; Bevilacqua, M.; Pera, F.; Signori, A.; Pera, P. Shock absorption capacity of restorative materials for dental implant prostheses: An in vitro study. Int. J. Prosthodont. 2013, 26, 549–556. [Google Scholar] [CrossRef][Green Version]
- Abdulmajeed, A.A.; Lim, K.G.; Närhi, T.O.; Cooper, L.F. Complete-arch implant-supported monolithic zirconia fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2016, 115, 672–677. [Google Scholar] [CrossRef]
- Bidra, A.S.; Rungruanganunt, P.; Gauthier, M. Clinical outcomes of full arch fixed implant-supported zirconia prostheses: A systematic review. Eur. J. Oral. Implantol. 2017, 10, 35–45. [Google Scholar]
- Guess, P.C.; Schultheis, S.; Bonfante, E.A.; Coelho, P.G.; Ferencz, J.L.; Silva, N.R. All-ceramic systems: Laboratory and clinical performance. Dent. Clin. N. Am. 2011, 55, 333–352. [Google Scholar] [CrossRef]
- Marchack, B.W.; Sato, S.; Marchack, C.B.; White, S.N. Complete and partial contour zirconia designs for crowns and fixed dental prostheses: A clinical report. J. Prosthet. Dent. 2011, 106, 145–152. [Google Scholar] [CrossRef]
- Ayman, A.D. The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins. Electron. Physician 2017, 9, 4766–4772. [Google Scholar] [CrossRef] [PubMed]
- AlHelal, A.; AlRumaih, H.S.; Kattadiyil, M.T.; Baba, N.Z.; Goodacre, C.J. Comparison of retention between maxillary milled and conventional denture bases: A clinical study. J. Prosthet. Dent. 2017, 117, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Nobre, M.d.A.; Guedes, C.M.; Almeida, R.; Silva, A.; Sereno, N.; Legatheaux, J. Short-term report of an ongoing prospective cohort study evaluating the outcome of full-arch implant-supported fixed hybrid polyetheretherketone-acrylic resin prostheses and the All-on-Four concept. Clin. Implant Dent. Relat. Res. 2018, 20, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Jackson, B.J. The Use of Laser-welded Titanium Framework Technology: A Case Report for the Totally Edentulous Patient. J. Oral. Implantol. 2005, 31, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Vaicelyte, A.; Janssen, C.; Le Borgne, M.; Grosgogeat, B. Cobalt–Chromium Dental Alloys: Metal Exposures, Toxicological Risks, CMR Classification, and EU Regulatory Framework. Crystals 2020, 10, 1151. [Google Scholar] [CrossRef]
- Sierraalta, M.; Vivas, J.L.; Razzoog, M.E.; Wang, R.F. Precision of fit of titanium and cast implant frameworks using a new matching formula. Int. J. Dent. 2012, 2012, 374315. [Google Scholar] [CrossRef]
- Gonzalez-Gonzalez, I.; de Llanos-Lanchares, H.; Brizuela-Velasco, A.; Alvarez-Riesgo, J.A.; Llorente-Pendas, S.; Herre-ro-Climent, M.; Alvarez-Arenal, A. Complications of Fixed Full-Arch Implant-Supported Metal-Ceramic Prostheses. Int. J. Environ. Res. Public Health 2020, 17, 4250. [Google Scholar] [CrossRef]
- Menini, M.; Pera, F.; Migliorati, M.; Pesce, P.; Pera, P. Adhesive strength of the luting technique for passively fitting screw-retained implant-supported prostheses: An in vitro evaluation. Int. J. Prosthodont. 2015, 28, 37–39. [Google Scholar] [CrossRef][Green Version]
- Menini, M.; Dellepiane, E.; Pera, P.; Bevilacqua, M.; Pesce, P.; Pera, F.; Tealdo, T. A Luting Technique for Passive Fit of Implant-Supported Fixed Dentures. J. Prosthodont. 2016, 25, 77–82. [Google Scholar] [CrossRef]
- Pesce, P.; Lagazzo, A.; Barberis, F.; Repetto, L.; Pera, F.; Baldi, D.; Menini, M. Mechanical characterisation of multi vs. uni-directional carbon fiber frameworks for dental implant applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 102, 186–191. [Google Scholar] [CrossRef]
| Authors (Year) | Study Type | Type of Loading | N° of Implants | N° of Patients | Test | Control | Jaw | Follow-Up | Results | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|
| Bergendal and Palmquist 1999 [27]. | Multicenter prospective cohort study, with a historical control group | Not reported | 818: 415 (test) 403 (control) | 184 (reported until the 2-years follow-up) | Laser-welded titanium framework; 67 at the 5-years examination | Gold-alloy framework; 66 at the 5-years examination | Maxilla and mandible | 2 and 5 years |
| Titanium framework clinical behavior is encouraging |
| Jemt et al. 2002 [28]. | Multicenter randomized clinical trial | Not reported | 349 | 58: 28 (test) vs. 30(control) | Laser- welded titanium | Cast-gold alloy | Maxillary | 5 years |
| No clinical or radiographic differences were observed between the two groups (similar favorable clinical performance). |
| Murphy et al. 2002 [29]. | Prospective | Delayed (3 months) | Not directly reported. 66–67 implants (test) vs. 65–66 (control) can be deducted from the text | 26 | Gold alloy | Silver-palladium alloy | Mandibular | 5 years |
| Despite differences in mechanical properties, clinical performance of both materials and radiographic changes in peri-implant bone was similar over 5 years (similar accuracy of fit and resistance to functional stress). Therefore, silver-palladium alloy may be considered a suitable low-cost substitute for gold alloy for implant- supported frameworks. |
| Ortorp et al., 2009 [30] | Post-trial follow-up | Delayed | 821 | 155 (test) vs. 53 (control); 53 (test) vs. 13 (control) reached the 15-years follow-up | Laser-welded titanium | Gold alloy castings | Mandibular | 15 years |
| The gold alloy frameworks had a tendency to work better when compared with welded titanium frameworks over 15 years. However, more bone loss was observed for implants supporting gold alloy frameworks. |
| Crespi et al. 2012 [31]. | Randomized clinical trial | Immediate | 176 | 36 | Full-acrylic | Metal-acrylic | Maxillary and mandibular | 3 years |
| The same clinical outcomes were found, regardless of whether the acrylic-resin restorations were reinforced with metal |
| Ortorp et al. 2012 [32]. | Randomized clinical trial | Delayed | 728 | 126: 65 (test) vs. 61 (control) 36 (test) 38 (control) reached the 10-years follow-up | Computer Numerical Controlled (CNC) titanium | Cast gold-alloy | Maxillary and mandibular | 10 years |
| CNC-milled titanium frameworks are a viable alternative to gold-alloy castings for restoring patients with implant-supported protheses in the edentulous jaw. |
| Tartaglia et al. 2015 [33]. | Retrospective cohort study | Immediate | 1058 | 113 | CAD-CAM zirconia prostheses veneered with feldspathic porcelain* | CAD-CAM PMMA prostheses veneered using composite resin teeth* | Maxilla and mandible | 2–60 months |
| Prosthesis material did not influence complication risk. |
| Cannizzaro et al. 2016 [34]. | Prospective cohort study | Immediate | 160 | 80 | Laser- welded titanium | Cast silver- palladium | Mandibular | 5 years |
| Laser-welded framework constructionshould be considered as a long-term temporary prosthesis and not definitive. Immediately loaded mandibular cross-arch prostheses can be supported by only two implants up to 5 years, if made with a robust cast framework. |
| Pera et al. 2017 [35]. | Prospective cohort study, with a historical control group | Immediate | 333: 170 test) vs. 163 (control) | 76: 42 (test) vs. 34 (control) | Carbon fiber frameworks | Cast metal framework (34 patients163 implants) | Maxilla | 22 months (range: 18–24) |
| Carbon fiberframeworks may be considered as a viablealternative to the metal ones and showed lessmarginal peri-implant bone loss and a greaterimplant survival rate. |
| Caramês et al. 2019 [36]. | Prospective cohort study | Delayed: after 12 weeks or after 6–9 months (in case of bone regeneration); during healing and osseointegration immediate provisional restoration consisted in metal-reinforced fixed complete dentures | 1009: 581 (test) vs. 428 (control) | 132: 62 (test) vs. 70 (control) | MZ (milled Yttrium-stabilized monolithic zirconia) with veneering porcelain limited to non-functional surfaces | PVZ (feldspathic porcelain-veneered zirconia) | Maxilla and mandible | From 1 to 2 years |
| Zirconia (in particular MZ group) has demonstrated to be a suitable material for frameworks in full-archImplant-supported rehabilitations. |
| Barootchi et al. 2020 [37]. | Retrospective cohort study | Immediate or delayed | 452: 200 (test) vs. 252 (control) | 56: 35 (test) vs. 21 (control) | Monolithic zirconia framework with luted single ceramic crowns and light cured resin to mimic gingival tissue | Cast metal-acrylic | Maxilla and mandible | ≥ 5 years (7 test; 9,5 control) |
| Zirconia fixed implant prostheses presented higher initial costs than metal-acrylic hybrids, but with satisfactory outcomes, reduction of overall complications, and superior survival rates |
| Study | Selection Bias Sequence Generation | Selection Bias Allocation Concealment | Performance Bias | Detection Bias | Attrition Bias | Selective Reporting Bias | Other Potential Risk of Bias |
|---|---|---|---|---|---|---|---|
| Jemt et al. 2002 | Low | Low | Unclear | Unclear | Low | Low | Low |
| Ortorp and Jemt. 2009 | High | High | Unclear | Unclear | Low | Low | Low |
| Crespi et al. 2012 | Unclear | Unclear | Unclear | Unclear | High | Unclear | Low |
| Ortorp and Jemt. 2012 | Unclear | Unclear | Unclear | Unclear | Low | Low | Low |
| Study | Selection | Comparability | Outcome/Exposure | NOS Score |
|---|---|---|---|---|
| Bergendal and Palmquist 1999 | --✶✶ | ✶- | ✶✶- | 5 |
| Murphy et al. 2002 | --✶✶ | ✶- | ✶✶- | 5 |
| Tartaglia et al. 2015 | ✶✶✶✶ | ✶- | ✶✶- | 7 |
| Cannizzaro et al. 2016 | ✶✶✶✶ | ✶- | ✶✶- | 7 |
| Pera et al. 2017 | ✶✶✶✶ | -- | ✶✶- | 6 |
| Caramês et al. 2019 | ✶✶✶✶ | ✶✶ | ✶✶✶ | 9 |
| Barootchi et al. 2020 | ✶✶✶✶ | -- | ✶✶✶ | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delucchi, F.; De Giovanni, E.; Pesce, P.; Bagnasco, F.; Pera, F.; Baldi, D.; Menini, M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials 2021, 14, 3251. https://doi.org/10.3390/ma14123251
Delucchi F, De Giovanni E, Pesce P, Bagnasco F, Pera F, Baldi D, Menini M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials. 2021; 14(12):3251. https://doi.org/10.3390/ma14123251
Chicago/Turabian StyleDelucchi, Francesca, Emanuele De Giovanni, Paolo Pesce, Francesco Bagnasco, Francesco Pera, Domenico Baldi, and Maria Menini. 2021. "Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies" Materials 14, no. 12: 3251. https://doi.org/10.3390/ma14123251
APA StyleDelucchi, F., De Giovanni, E., Pesce, P., Bagnasco, F., Pera, F., Baldi, D., & Menini, M. (2021). Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials, 14(12), 3251. https://doi.org/10.3390/ma14123251









