Base Materials’ Influence on Fracture Resistance of Molars with MOD Cavities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of Teeth
2.2. Preparation of Test Specimens
2.3. Fracture Resistance Test
2.4. Statistical Analysis
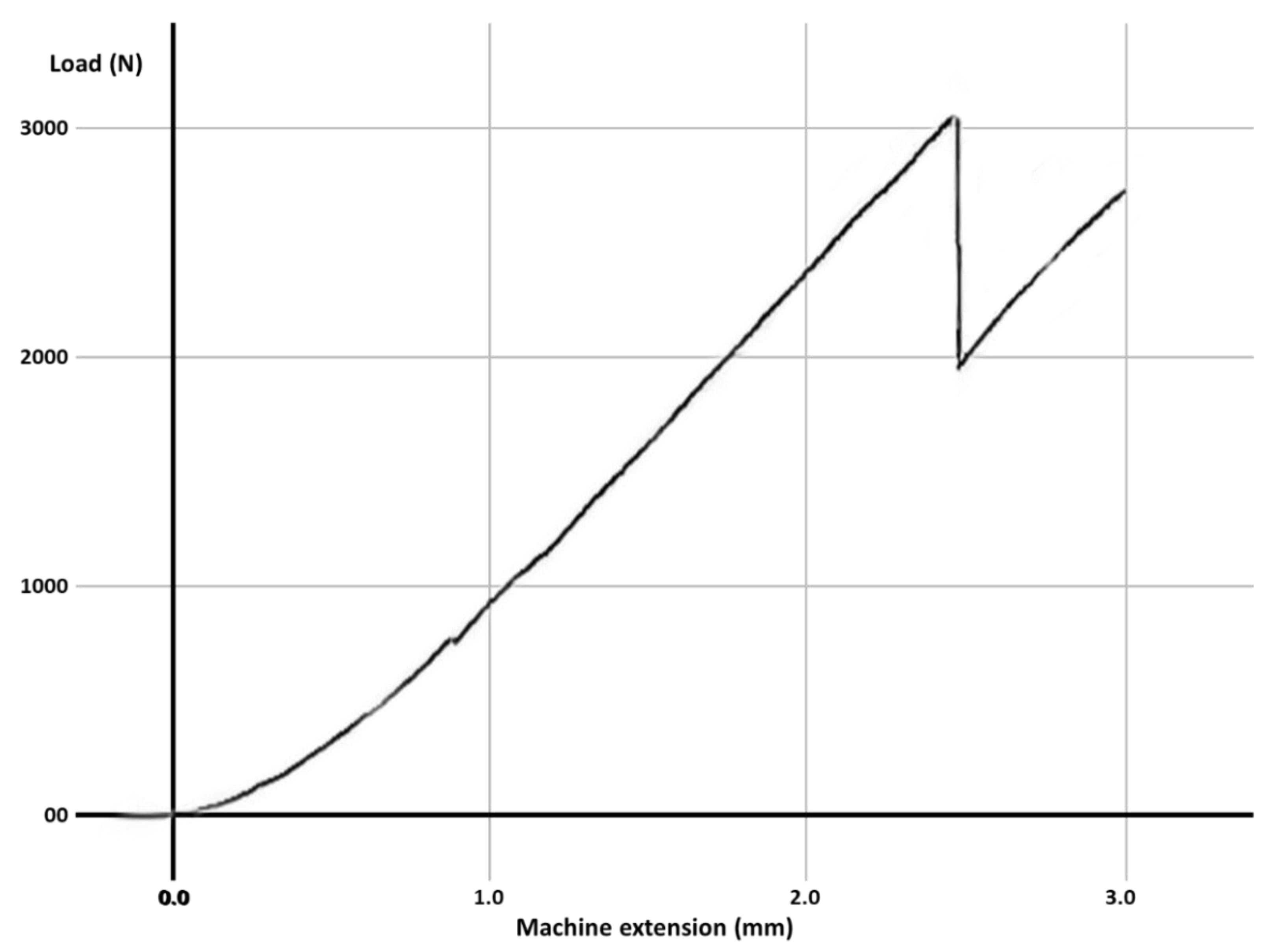
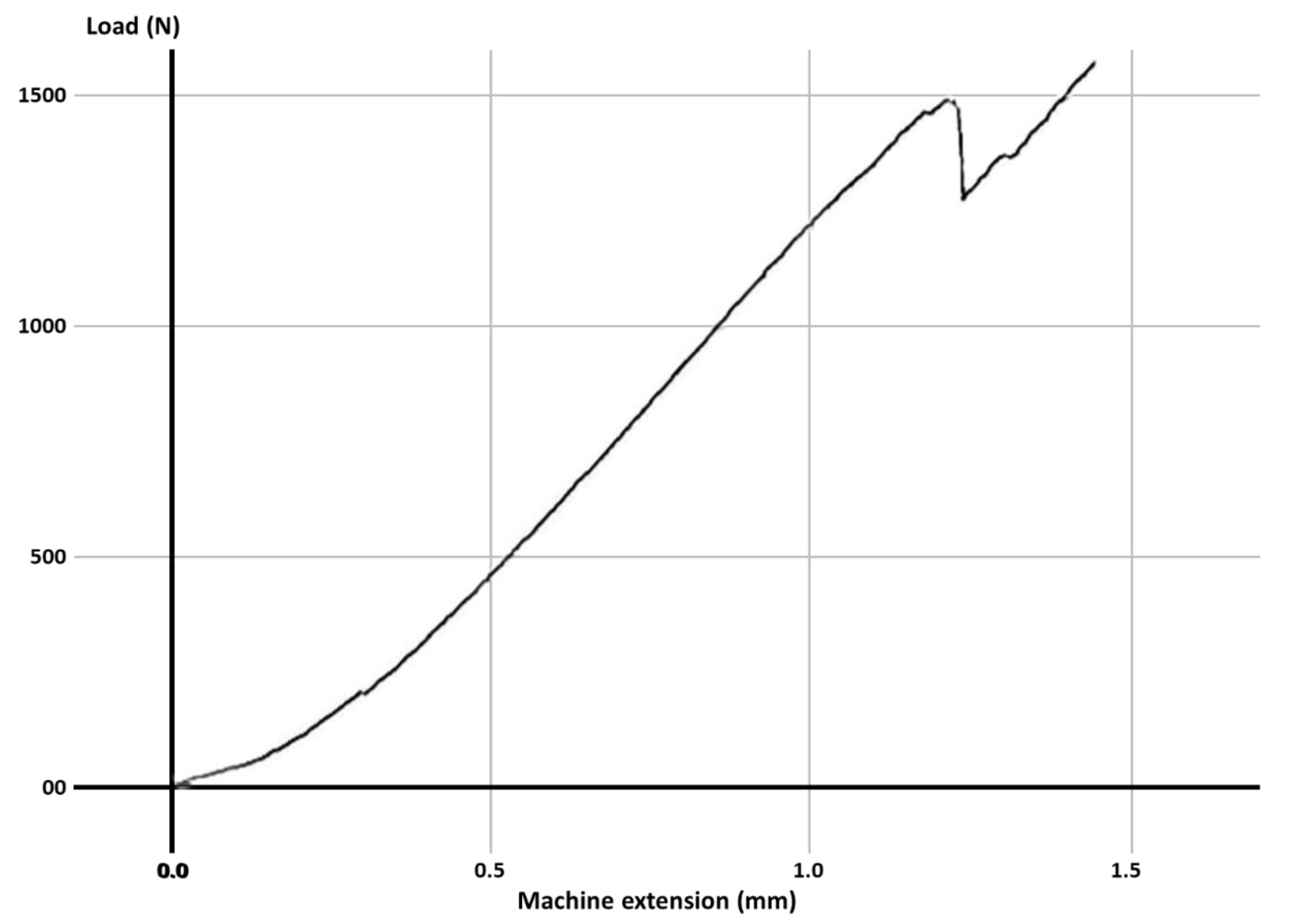
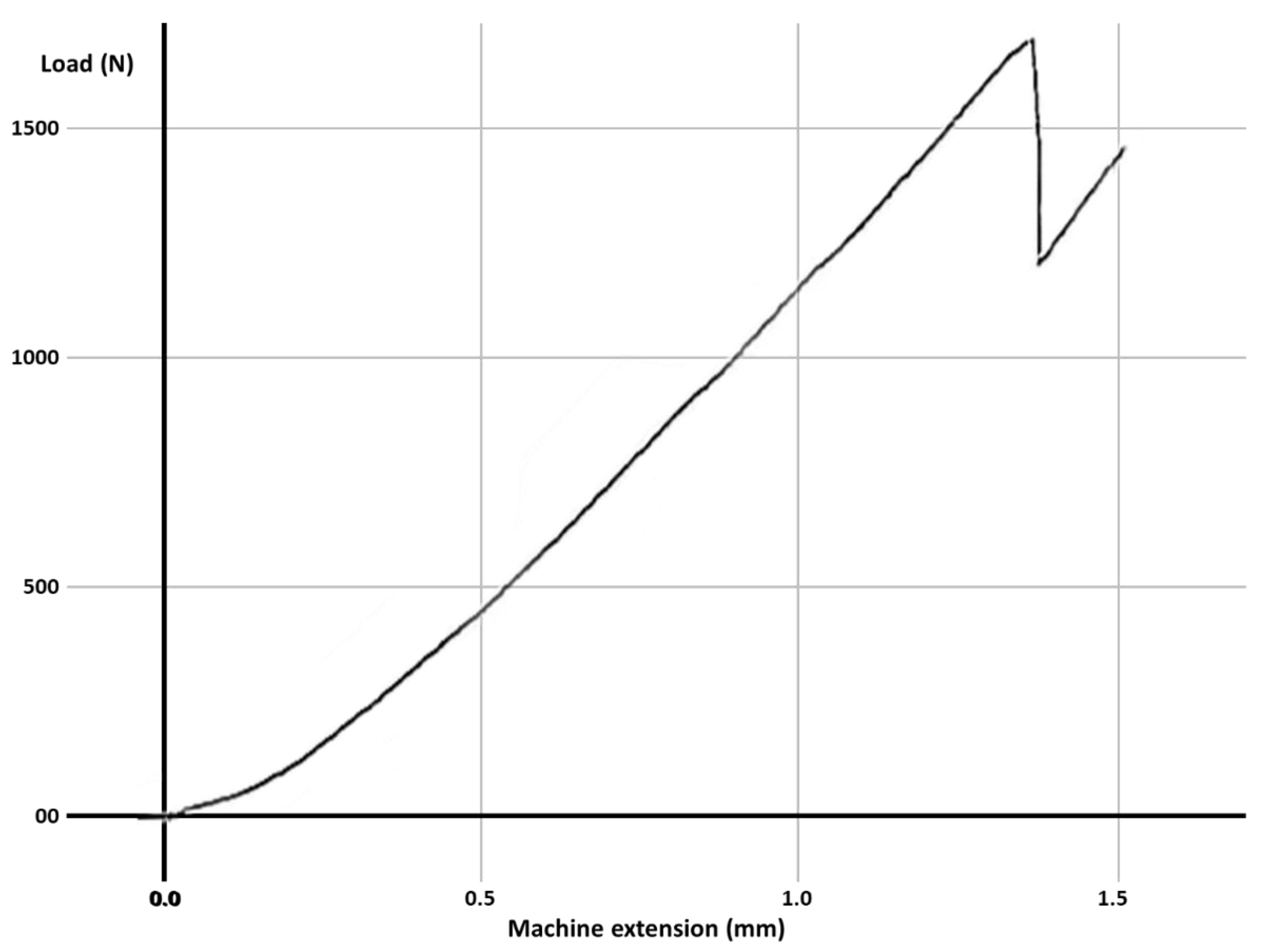
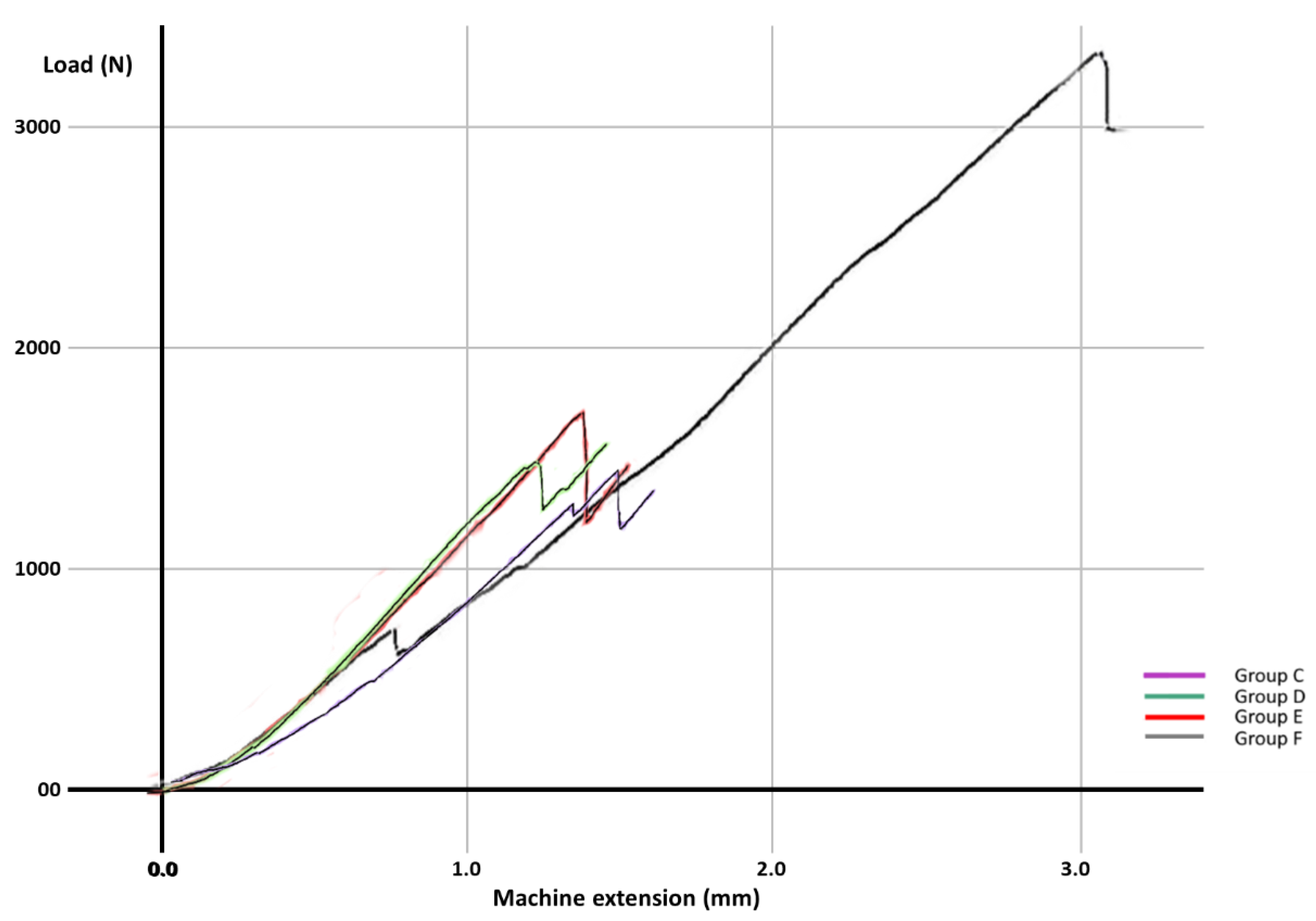
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Nam, S.H.; Chang, H.S.; Min, K.S.; Lee, Y.; Cho, H.W.; Bae, J.M. Effect of the number of residual walls on fracture resistances, failure patterns, and photoelasticity of simulated premolars restored with or without fiber-reinforced composite posts. J. Endod. 2010, 36, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.F.; Chen, Y.M.; Guang, H.B.; Yip, K.H.; Smales, R.J. Effect of a ferrule and increased clinical crown length on the in vitro fracture resistance of premolars restored using two dowel-and-core systems. Oper. Dent. 2007, 32, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.V.; Santos-Filho, P.C.; Martins, L.R.; Soares, C.J. Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part I: Fracture resistance and fracture mode. J. Prosthet. Dent. 2008, 99, 30–37. [Google Scholar] [CrossRef]
- Sorrentino, R.; Aversa, R.; Ferro, V.; Auriemma, T.; Zarone, F.; Ferrari, M.; Apicella, A. Three-dimensional finite element analysis of strain and stress distributions in endodontically treated maxillary central incisors restored with different post, core and crown materials. Dent. Mater. 2007, 23, 983–993. [Google Scholar] [CrossRef]
- Mărgărit, R.; Suciu, I.; Bodnar, D.C.; Grigore, M.; Scărlătescu, S.A.; Andrei, O.C.; Măgureanu, C.M.; Chirilă, M.; Bencze, A.; Ionescu, E. Fracture resistance of molars with MOD cavities restored with different materials. Rom. Biotechnol. Lett. 2021, 26, 2323–2330. [Google Scholar] [CrossRef]
- Mărgărit, R.; Tănăsescu, L.A.; Bodnar, D.; Ion, C.G.; Burlibaşa, M.; Bisoc, A.; Farcaşiu, C.; Dina, M.N.; Andrei, O.C. Comparison of fracture resistance of teeth presenting non-carious cervical lesions, restored with different composite materials. Mater. Plast. 2020, 57, 299–305. [Google Scholar] [CrossRef]
- Soares, P.V.; Santos-Filho, P.C.; Gomide, H.A.; Araujo, C.A.; Martins, L.R.; Soares, C.J. Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part II: Strain measurement and stress distribution. J. Prosthet. Dent. 2008, 99, 114–122. [Google Scholar] [CrossRef]
- Krämer, N.; Reinelt, C.; Frankenberger, R. Ten-year clinical performance of posterior resin composite restorations. J. Adhes. Dent. 2015, 17, 433–441. [Google Scholar]
- Pallesen, U.; Van Dijken, J.W. A randomized controlled 30 years follow up of three conventional resin composites in class II restorations. Dent. Mater. 2015, 31, 1232–1244. [Google Scholar] [CrossRef]
- Eskitaşcioǧlu, G.; Belli, S.; Kalkan, M. Evaluation of two post core systems using two different methods (fracture strength test and a finite elemental stress analysis). J. Endod. 2002, 28, 629–633. [Google Scholar] [CrossRef]
- Mondelli, R.F.; Ishikiriama, S.K.; De Oliveira Filho, O.; Mondelli, J. Fracture resistance of weakened teeth restored with condensable resin with and without cusp coverage. J. Appl. Oral Sci. 2009, 17, 161–165. [Google Scholar] [CrossRef]
- Plotino, G.; Buono, L.; Grande, N.M.; Lamorgese, V.; Somma, F. Fracture resistance of endodontically treated molars restored with extensive composite resin restorations. J. Prosthet. Dent. 2008, 99, 225–232. [Google Scholar] [CrossRef]
- Alomari, Q.D.; Reinhardt, J.W.; Boyer, D.B. Effect of liners on cusp deflection and gap formation in composite restorations. Oper. Dent. 2001, 26, 406–411. [Google Scholar]
- Cho, E.; Chikawa, H.; Kishikawa, R.; Inai, N.; Otsuki, M.; Foxton, R.M.; Tagami, J. Influence of elasticity on gap formation in a lining technique with flowable composite. Dent. Mater. J. 2006, 25, 538–544. [Google Scholar] [CrossRef] [Green Version]
- Yoshida, Y.; Van Meerbeek, B.; Nakayama, Y.; Snauwaert, J.; Hellemans, L.; Lambrechts, P.; Vanherle, G.; Wakasa, K. Evidence of chemical bonding at biomaterial-hard tissue interfaces. J. Dent. Res. 2000, 79, 709–714. [Google Scholar] [CrossRef]
- Feilzer, A.J.; De Gee, A.J.; Davidson, C.L. Curing contraction of composites and glass-ionomer cements. J. Prosthet. Dent. 1988, 59, 297–300. [Google Scholar] [CrossRef]
- Kovarik, R.E.; Breeding, L.C.; Caughman, W.F. Fatigue life of three core materials under simulated chewing conditions. J. Prosthet. Dent. 1992, 68, 584–590. [Google Scholar] [CrossRef]
- Jemt, T.; Stalblad, P.A.; Øilo, G. Adhesion of polycarboxylate- based dental cements to enamel: An in vivo study. J. Dent. Res. 1986, 65, 885–887. [Google Scholar] [CrossRef]
- Cara, R.R.; Fleming, G.J.; Palin, W.M.; Walmsley, A.D.; Burke, F.J. Cuspal deflection and microleakage in premolar teeth restored with resin-based composites with and without an intermediary flowable layer. J. Dent. 2007, 35, 482–489. [Google Scholar] [CrossRef]
- Roggendorf, M.J.; Kramer, N.; Appelt, A.; Naumann, M.; Frankenberger, R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J. Dent. 2011, 39, 643–647. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-fill resin-based composites: An in vitro assessment of their mechanical performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef]
- Taha, N.A.; Palamara, J.E.; Messer, H.H. Fracture strength and fracture patterns of root filled teeth restored with direct resin restorations. J. Dent. 2011, 39, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Bo, H.; Yongchun, G.; Longxing, N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: A three-dimensional finite element analysis. J. Prosthet. Dent. 2010, 103, 6–12. [Google Scholar] [CrossRef]
- Kinney, J.H.; Marshall, S.J.; Marshall, G.W. The mechanical properties of human dentin: A critical review and re-evaluation of the dental literature. Crit. Rev. Oral Biol. Med. 2003, 14, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Tam, L.E.; Pulver, E.; Mccomb, D.; Smith, D.C. Physical properties of calcium hydroxide and glass-ionomer base and lining materials. Dent. Mater. 1989, 5, 145–149. [Google Scholar] [CrossRef]
- Akinmade, A.O.; Hill, R.G. Influence of cement layer thickness on the adhesive bond strength of polyalkenoate cements. Biomater 1992, 13, 931–936. [Google Scholar] [CrossRef]
- Natale, L.; Rodrigues, M.; Xavier, T.; Simoes, A.; De Souza, D.; Braga, R. Ion release and mechanical properties of calcium silicate and calcium hydroxide materials used for pulp capping. Int. Endod. J. 2015, 48, 89–94. [Google Scholar] [CrossRef]
- Chan, T.; Kucukkaya Eren, S.; Wong, R.; Parashos, P. In vitro fracture strength and patterns in root-filled teeth restored with different base materials. Aust. Dent. J. 2018, 63, 99–108. [Google Scholar] [CrossRef]
- Hernandez, R.; Bader, S.; Boston, D.; Trope, M. Resistance to fracture of endodontically treated premolars restored with new generation dentine bonding systems. Int. Endod. J. 1994, 27, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Wendt, S.L., Jr.; Harris, B.M.; Hunt, T.E. Resistance to cusp fracture in endodontically treated teeth. Dent. Mater. 1987, 3, 232–235. [Google Scholar] [CrossRef]
- Davidson, C.L. Glass-ionomer bases under posterior composites. J. Esthet. Dent. 1994, 6, 223–224. [Google Scholar] [CrossRef]
- Taha, N.A.; Palamara, J.E.; Messer, H.H. Assessment of laminate technique using glass ionomer and resin composite for restoration of root filled teeth. J. Dent. 2012, 40, 617–623. [Google Scholar] [CrossRef]
- Trope, M.; Tronstad, L. Resistance to fracture of endodontically treated premolars restored with glass ionomer cement or acid etch composite resin. J. Endod. 1991, 17, 257–259. [Google Scholar] [CrossRef]
- Banomyong, D.; Harnirattisai, C.; Burrow, M.F. Posterior resin composite restorations with or without resin-modified, glass-ionomer cement lining: A 1-year randomized, clinical trial. J. Investig. Clin. Dent. 2011, 2, 63–69. [Google Scholar] [CrossRef]
- Eakle, W.S. Increased fracture resistance of teeth: Comparison of five bonded composite resin systems. Quintessence Int. 1986, 17, 17–20. [Google Scholar]
- Oz, F.D.; Ergin, E.; Gurgan, S. Comparison of different base materials on fracture strength of mesio-occlusal-distal composite restorations. Eur. J. Gen. Dent. 2018, 7, 25–30. [Google Scholar] [CrossRef]
- Taha, N.A.; Maghaireh, G.A.; Ghannam, A.S.; Palamara, J.E. Effect of bulk-fill base material on fracture strength of root-filled teeth restored with laminate resin composite restorations. J. Dent. 2017, 63, 60–64. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R.; Valceanu, A.S.; Huth, K.C. Fracture toughness of dental restorative materials. Clin. Oral Investig. 2012, 16, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Rosatto, C.M.; Bicalho, A.A.; Verissimo, C.; Braganca, G.F.; Rodrigues, M.P.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. J. Dent. 2015, 43, 1519–1528. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent. Mater. 2011, 27, 348–355. [Google Scholar] [CrossRef]
- Kim, R.J.; Kim, Y.J.; Choi, N.S.; Lee, I.B. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J. Dent. 2015, 43, 430–439. [Google Scholar] [CrossRef]
- Belli, S.; Erdemir, A.; Ozcopur, M.; Eskitascioglu, G. The effect of fibre insertion on fracture resistance of root filled molar teeth with MOD preparations restored with composite. Int. Endod. J. 2005, 38, 73–80. [Google Scholar] [CrossRef]
- Hormati, A.A.; Fuller, J.L. The fracture strength of amalgam overlying base materials. J. Prosthet. Dent. 1980, 43, 52–57. [Google Scholar] [CrossRef]
- Versluis, A.; Tantbirojn, D.; Pintado, M.R.; Delong, R.; Douglas, W.H. Residual shrinkage stress distributions in molars after composite restoration. Dent. Mater. 2004, 20, 554–564. [Google Scholar] [CrossRef]
- Kahler, B.; Swain, M.V.; Kotousov, A. Comparison of an analytical expression of resin composite curing stresses with in vitro observations of marginal cracking. Am. J. Dent. 2010, 23, 357–364. [Google Scholar]




| Material | Adhesion | Modulus of Elasticity | Compression Strength |
|---|---|---|---|
| Adhesor carbofine (Spofa Dental) | Natural adhesion to the hard dental tissues | 4.4 GPa | 47 MPa |
| Fuji IX (GC) | Intrinsic adhesion to dentine and enamel, without the need for etching and bonding | 8.3 GPa | 220 MPa |
| Fuji II LC (GC) | Strong adhesion, excellent bond strength to teeth even in presence of saliva | 5.33 GPa | 245 MPa |
| Charisma flow (Heraeus Kulzer) | Adhesive for any bonding technique | 14.3 GPa | 325 MPa |
| Charisma (Heraeus Kulzer) | Adhesive for any bonding technique | 8 GPa | 325 MPa |
| Material | Purpose | Type | Chemical Composition |
|---|---|---|---|
| Adhesor carbofine (Spofa Dental) | Base | ZPC—zinc polycarboxylate cement | Zinc oxide, magnesium oxide, aluminum oxide, boric acid, acrylic acid, maleic anhydride, distilled water |
| Fuji IX (GC) | Base | GIC—glass ionomer cement | Alumino-silicate glass 95%, polyacrylic acid powder 5% |
| Fuji II LC (GC) | Base | RMGIC- Light-cured Resin Reinforced Glass Ionomer cement | Fluoro-alumino-silicate glass, polyacrylic acid 30–35%, distilled water 20–30%, 2HEMA 25–30%, initiator, urethan dymethylacrylate, camphorquinone |
| Charisma flow (Heraeus Kulzer) | Base | FC-Flowable resin-micro-hybrid flowable composite, Light-cured | multifunctional methacrylate monomers (EBADMA/TEGDMA); contains approximately 62% by weight or 38% by volume inorganic fillers such as Ba-AI-F silicate glass and SiO2. The filler particle size is between 0.005 μm and 5 μm. |
| Charisma (Heraeus Kulzer) | Final restoration | Universal hybrid composite with microparticles, Light-cured | BIS-GMA matrix; contains 64% filler by volume: barium aluminum fluoride glass (0.02–2 microns); colloidal silica −0.01–0.07 μm. |
| Group | Mean (N) | Standard Deviation | Median | Fracture Force (N) for Each Specimen | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||||
| A | 2902 | 114 | 2889 | 2780 | 2795 | 2835 | 2943 | 3010 | 3050 |
| B | 972 | 65 | 988 | 865 | 930 | 972 | 1004 | 1025 | 1040 |
| C | 1339 | 84 | 1348 | 1210 | 1286 | 1315 | 1382 | 1413 | 1430 |
| D | 1415 | 67 | 1408 | 1340 | 1358 | 1372 | 1445 | 1478 | 1500 |
| E | 1712 | 62 | 1716 | 1630 | 1655 | 1698 | 1734 | 1765 | 1790 |
| F | 2334 | 662 | 2112 | 1742 | 1795 | 1855 | 2370 | 2925 | 3320 |
| ANOVA: Single Factor | ||||||
|---|---|---|---|---|---|---|
| SUMMARY | ||||||
| Groups | Count | Sum | Average | Variance | ||
| C-ZPC | 6 | 8036 | 1339.333 | 7126.267 | ||
| D-GIC | 6 | 8493 | 1415.5 | 4563.1 | ||
| E-RMGIC | 6 | 10,272 | 1712 | 3909.2 | ||
| F-FC | 6 | 14,007 | 2334.5 | 438,639.5 | ||
| ANOVA | ||||||
| Source of Variation | SS | df | MS | F | p-Value | F Crit |
| Between Groups | 3,682,527 | 3 | 1,227,509 | 10.80939 | ||
| Within Groups | 2,271,190 | 20 | 113,559.5 | |||
| Total | 5,953,717 | 23 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciavoi, G.; Mărgărit, R.; Todor, L.; Bodnar, D.; Dina, M.N.; Tărlungeanu, D.I.; Cojocaru, D.; Farcaşiu, C.; Andrei, O.C. Base Materials’ Influence on Fracture Resistance of Molars with MOD Cavities. Materials 2021, 14, 5242. https://doi.org/10.3390/ma14185242
Ciavoi G, Mărgărit R, Todor L, Bodnar D, Dina MN, Tărlungeanu DI, Cojocaru D, Farcaşiu C, Andrei OC. Base Materials’ Influence on Fracture Resistance of Molars with MOD Cavities. Materials. 2021; 14(18):5242. https://doi.org/10.3390/ma14185242
Chicago/Turabian StyleCiavoi, Gabriela, Ruxandra Mărgărit, Liana Todor, Dana Bodnar, Magdalena Natalia Dina, Daniela Ioana Tărlungeanu, Denisa Cojocaru, Cătălina Farcaşiu, and Oana Cella Andrei. 2021. "Base Materials’ Influence on Fracture Resistance of Molars with MOD Cavities" Materials 14, no. 18: 5242. https://doi.org/10.3390/ma14185242






