Reliability and Correlation of Different Devices for the Evaluation of Primary Implant Stability: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- In our model, there is a high correlation between the IT and ISQ from a purely mechanical perspective.
- Bone type does not affect the high positive correlation between the initial and final Osstell and Penguin device measurements.
- Implant length does not affect the correlation between the primary stability measurements attained by the different RFA devices.
- Implant design affects the correlation between the IT and ISQ, which is maintained in the CC design. However, in the IH design it was maintained only between the RFA devices.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| ISQ | implant stability quotient |
| RFA | resonance frequency analysis |
| IT | insertion torque |
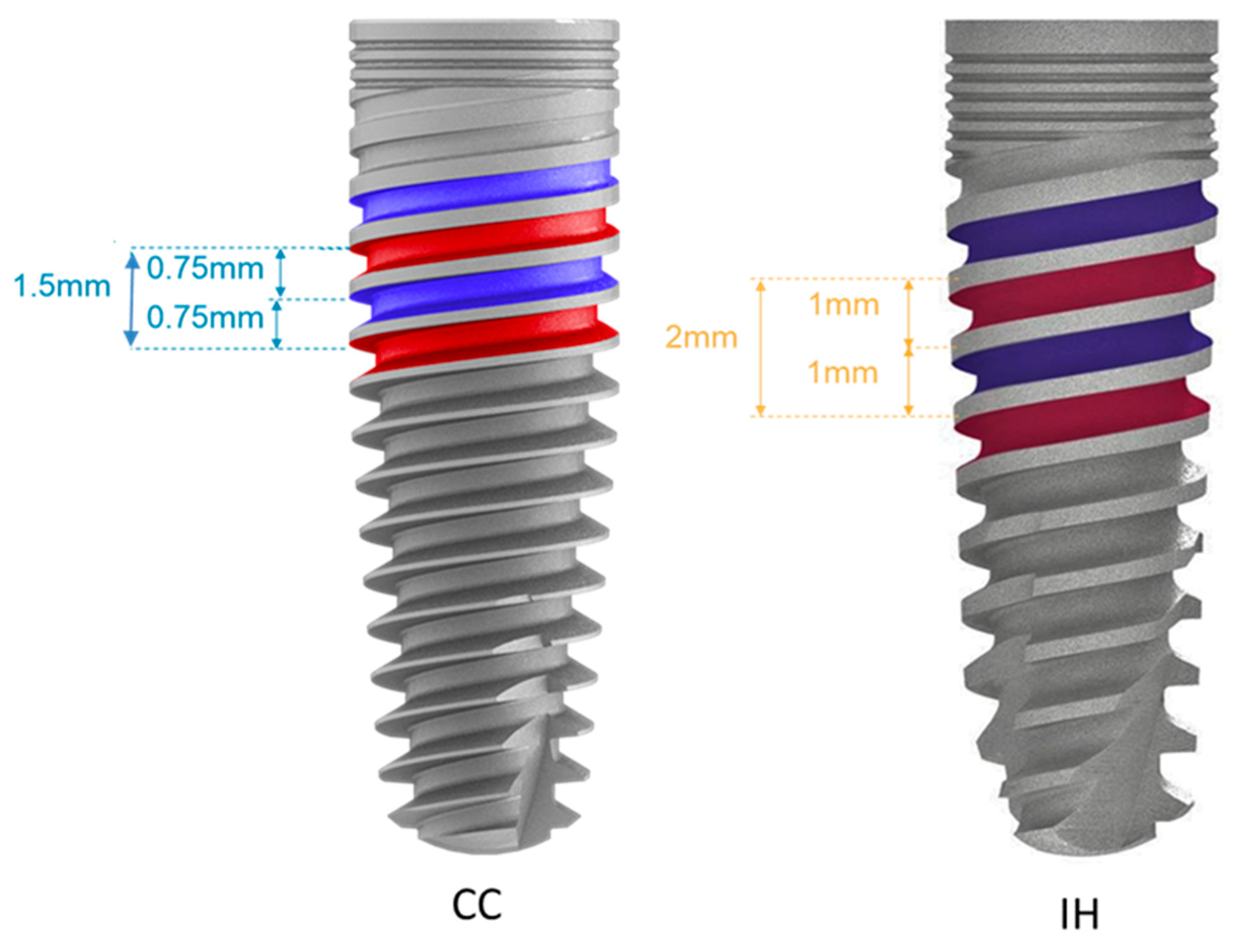
| CC | conical connection |
| IH | internal hexagon |
References
- Romanos, G.E. Present status of immediate loading of oral implants. J. Oral Implantol. 2004, 30, 189–197. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The insertion torque-depth curve integral as a measure of implant primary stability: An in vitro study on polyurethane foam blocks. J. Prosthet. Dent. 2018, 120, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Sennerby, L.; Meredith, N. Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implications. Periodontol. 2000 2008, 47, 51–66. [Google Scholar] [CrossRef]
- Fanuscu, M.I.; Chang, T.-L.; Akça, K. Effect of Surgical Techniques on Primary Implant Stability and Peri-Implant Bone. J. Oral Maxillofac. Surg. 2007, 65, 2487–2491. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I.; Tozum, T. Enhancing primary implant stability by undersizing implant site preparation: A human cadaver study. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; D’Arcangelo, C.; Piattelli, A.; Iezzi, G. An In Vitro alysis on Polyurethane Foam Blocks of the Insertion Torque (IT) Values Removal Torque Values (RTVs), and Resonance Frequency Analysis (RFA) Values in Tapered and Cylin-drical Implants. Int. J. Environ. Res. Public Health 2021, 18, 9238. [Google Scholar] [CrossRef]
- Attanasio, F.; Antonelli, A.; Brancaccio, Y.; Averta, F.; Figliuzzi, M.M.; Fortunato, L.; Giudice, M. Primary Stability of Three Different Osteotomy Techniques in Medullary Bone: An in Vitro Study. Dent. J. 2020, 8, 21. [Google Scholar] [CrossRef] [Green Version]
- Ahn, S.J.; Leesungbok, R.; Lee, S.W.; Heo, Y.K.; Kang, K.L. Differences in implant stability associated with various methods of prep-aration of the implant bed: An in vitro study. J. Prosthet. Dent. 2012, 107, 366–372. [Google Scholar] [CrossRef]
- Degidi, M.; Daprile, G.; Piattelli, A.; Iezzi, G. Development of a New Implant Primary Stability Parameter: Insertion Torque Revisited. Clin. Implant. Dent. Relat. Res. 2011, 15, 637–644. [Google Scholar] [CrossRef]
- Sim, C.P.; Lang, N.P. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integra-tion: I. Instrument positioning, bone structure, implant length. Clin. Oral Implants Res. 2010, 21, 598–604. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Santos-Garcia, R.; Jaramillo-Santos, R.; Romero-Ruiz, M.; Fernández-Palacín, A.; Lazaro-Calvo, P.; Bullon, P.; Ríos-Santos, J. Assessment of osstell isq’s reliability for implant stability measurement: A cross-sectional clinical study. Med. Oral. Patol. Oral Cir. Bucal. 2013, 18, e877–e882. [Google Scholar] [CrossRef]
- Valderrama, P.; Oates, T.W.; Jones, A.A.; Simpson, J.; Schoolfield, J.D.; Cochran, D.L. Evaluation of Two Different Resonance Frequency Devices to Detect Implant Stability: A Clinical Trial. J. Periodontol. 2007, 78, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Rittel, D.; Dorogoy, A.; Haïat, G.; Shemtov-Yona, K. Resonant frequency analysis of dental implants. Med. Eng. Phys. 2019, 66, 65–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farronato, D.; Manfredini, M.; Stocchero, M.; Caccia, M.; Azzi, L.; Farronato, M. Influence of Bone Quality, Drilling Protocol, Implant Diameter/Length on Primary Stability: An In Vitro Comparative Study on Insertion Torque and Resonance Frequency Analysis. J. Oral Implantol. 2020, 46, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Iezzi, G.; Piattelli, A.; Tumedei, M. An In Vitro Evaluation, on Polyurethane Foam Sheets, of the Insertion Torque (IT) Values, Pull-Out Torque Values, and Resonance Frequency Analysis (RFA) of NanoShort Dental Implants. Polymers 2019, 11, 1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajendra, K.; Manual, L.; Kochhar, A.S.; A Haseeb, S.; Dubey, D.; Dang, G.S. Comparative Evaluation of Implant Stability, Insertion Torque, and Implant Macrogeometry in Different Bone Densities Using Resonance Frequency Analysis. J. Contemp. Dent. Pract. 2021, 22, 665–668. [Google Scholar] [CrossRef]
- Degidi, M.; Daprile, G.; Piattelli, A. Primary Stability Determination by Means of Insertion Torque and RFA in a Sample of 4135 Implants. Clin. Implant. Dent. Relat. Res. 2010, 14, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Msc, F.S.L.; Douglas-De-Oliveira, D.W.; Costa, F. Relationship between implant stability measurements obtained by insertion torque and resonance frequency analysis: A systematic review. Clin. Implant. Dent. Relat. Res. 2017, 20, 26–33. [Google Scholar]
- Kim, D.-S.; Lee, W.-J.; Choi, S.-C.; Lee, S.-S.; Heo, M.-S.; Huh, K.-H.; Kim, T.-I.; Yi, W.-J. Comparison of dental implant stabilities by impact response and resonance frequencies using artificial bone. Med. Eng. Phys. 2013, 36, 715–720. [Google Scholar] [CrossRef]
- Devlin, H.; Horner, K.; Ledgerton, D. A comparison of maxillary and mandibular bone mineral densities. J. Prosthet. Dent. 1998, 79, 323–327. [Google Scholar] [CrossRef]
- Miyamoto, I.; Tsuboi, Y.; Wada, E.; Suwa, H.; Iizuka, T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery-clinical, prospective, biomechanical, and imaging study. Bone 2005, 37, 776–780. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I. A comparison between insertion torque and resonance frequency in the assessment of torque capacity and primary stability of Brånemark system implants. J. Oral Rehabil. 2006, 33, 754–759. [Google Scholar] [CrossRef]
- Baldi, D.; Lombardi, T.; Colombo, J.; Cervino, G.; Perinetti, G.; Di Lenarda, R.; Stacchi, C. Correlation between Insertion Torque and Implant Stability Quotient in Tapered Implants with Knife-Edge Thread Design. BioMed Res. Int. 2018, 2018, 7201093. [Google Scholar] [CrossRef] [PubMed]
- Becker, W.; Hujoel, P.; Becker, B.E. Resonance frequency analysis: Comparing two clinical instruments. Clin. Implant. Dent. Relat. Res. 2018, 20, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Bayarchimeg, D.; Namgoong, H.; Kim, B.K.; Kim, M.D.; Kim, S.; Kim, T.-I.; Seol, Y.J.; Lee, Y.M.; Ku, Y.; Rhyu, I.-C.; et al. Evaluation of the correlation between insertion torque and primary stability of dental implants using a block bone test. J. Periodontal Implant. Sci. 2013, 43, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Açil, Y.; Sievers, J.; Ayna, M.; Wiltfang, J.; Terheyden, H.; Gülses, A. Correlation between resonance frequency, insertion torque and bone-implant contact in self-cutting threaded implants. Odontology 2016, 105, 347–353. [Google Scholar] [CrossRef]
- Nakashima, D.; Mikami, K.; Kikuchi, S.; Nishikino, M.; Kitamura, T.; Hasegawa, N.; Matsumoto, M.; Nakamura, M.; Nagura, T. Laser resonance frequency analysis of pedicle screw stability: A cadaveric model bone study. J. Orthop. Res. 2021. [Google Scholar] [CrossRef] [PubMed]
- Bergamo, E.T.P.; Zahoui, A.; Barrera, R.B.; Huwais, S.; Coelho, P.G.; Karateew, E.D.; Bonfante, E.A. Osseodensification effect on implants primary and secondary stability: Multicenter controlled clinical trial. Clin. Implant. Dent. Relat. Res. 2021, 23, 317–328. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Inchingolo, A.M.; Bordea, I.R.; Xhajanka, E.; Romeo, D.M.; Romeo, M.; Zappone, C.M.F.; Malcangi, G.; Scarano, A.; Lorusso, F.; et al. The Effectiveness of Osseodensification Drilling Protocol for Implant Site Osteotomy: A Systematic Review of theLiterature and Meta-Analysis. Materials 2021, 14, 114. [Google Scholar] [CrossRef]
| Implant Type, Diameter/Length | Soft Bone (4 Blocks) | Dense Bone (4 Blocks) | Total Implants |
|---|---|---|---|
| Design IH Ø 3.75/13 mm | 12 | 12 | 24 |
| Design CC Ø 3.75/8 mm | 12 | 12 | 24 |
| Design IH Ø 3.75/13 mm | 12 | 12 | 24 |
| Design CC Ø 3.75/8 mm | 12 | 12 | 24 |
| Total | 48 | 48 | 96 |
| Device | N | Mean | SD |
|---|---|---|---|
| IT (N/cm) | 93 | 41.70 | 5.44 |
| Osstell initial | 93 | 56.87 | 5.42 |
| Penguin initial | 93 | 55.07 | 5.63 |
| Osstell final | 93 | 65.08 | 7.18 |
| Penguin final | 93 | 63.95 | 8.47 |
| Bone Type | Implant Length (mm) | Implant Type | Peak IT (N/cm) | Inserted Length % | Osstell Initial | Penguin Initial | Osstell Final | Penguin Final |
|---|---|---|---|---|---|---|---|---|
| Soft | 13 | CC | 43 ± 3.13 | 88.81 | 62.21 ± 4.06 | 60.60 ± 4.61 | 67.33 ± 3.13 | 66.48 ± 2.09 |
| Soft | 13 | HI | 36.66 ± 4.14 | 86.19 | 51.18 ± 4.08 | 49.24 ± 3.69 | 57.54 ± 3.52 | 56.12 ± 4.14 |
| Soft | 8 | CC | 42.25 ± 2.14 | 85.68 | 56.83 ± 3.37 | 55.61 ± 4.74 | 62.66 ± 1.96 | 60.91 ± 2.65 |
| Soft | 8 | HI | 39.41 ± 4.12 | 87.14 | 48.97 ± 4.01 | 47.08 ± 2.99 | 53.61 ± 3.78 | 51.58 ± 3.38 |
| Dense | 13 | CC | 46.66 ± 3.20 | 61.54 | 59.55 ± 2.33 | 57.83 ± 2.64 | 73.38 ± 2.11 | 74.47 ± 2.35 |
| Dense | 13 | HI | 36.91 ± 3.65 | 72.73 | 61.90 ± 3.49 | 60.59 ± 4.56 | 68.96 ± 4.20 | 67.33 ± 6.62 |
| Dense | 8 | CC | 47.41 ± 4.78 | 62.5 | 59.33 ± 1.81 | 57.61 ± 2.03 | 72.13 ± 2.51 | 72.86 ± 3.34 |
| Dense | 8 | HI | 40.83 ± 5.78 | 66.67 | 56.11 ± 3.54 | 53.52 ± 3.92 | 64.88 ± 4.09 | 61.72 ± 6.13 |
| Correlation Coefficient | Significance (2-Tailed) | ||
|---|---|---|---|
| Peak IT | Osstell initial | 0.498 ** | 3.26 × 10−7 |
| Peak IT | Osstell final | 0.494 ** | 4.7 × 10−7 |
| Peak IT | Penguin initial | 0.486 ** | 6.77 × 10−7 |
| Peak IT | Penguin final | 0.529 ** | 5.06 × 10−8 |
| Osstell initial | Penguin initial | 0.953 ** | 1.78 × 10−49 |
| Osstell final | Penguin final | 0.964 ** | 2.42 × 10−54 |
| Dense Bone | Soft Bone | ||||
|---|---|---|---|---|---|
| Correlation Coefficient | Significance (2-Tailed) | Correlation Coefficient | Significance (2-Tailed) | ||
| Peak IT | Osstell initial | 0.274 | 0.060 | 0.711 ** | 4.502 × 10−8 |
| Peak IT | Osstell final | 0.465 ** | 0.001 | 0.637 ** | 2.521 × 10−6 |
| Peak IT | Penguin initial | 0.273 | 0.061 | 0.684 ** | 2.252 × 10−7 |
| Peak IT | Penguin final | 0.494 ** | 0.000 | 0.599 ** | 1.408 × 10−5 |
| Osstell initial | Penguin initial | 0.977 ** | 1.09 × 10−32 | 0.955 ** | 2.702 × 10−24 |
| Osstell final | Penguin final | 0.955 ** | 1.93 × 10−25 | 0.983 ** | 2.693 × 10−33 |
| 8 mm Implant Length | Significance (2-Tailed) | 13 mm Implant Length | Significance (2-Tailed) | ||
|---|---|---|---|---|---|
| Peak IT | Osstell initial | 0.737 ** | 2.255 × 10−9 | 0.390 ** | 0.0073 |
| Peak IT | Osstell final | 0.500 ** | 2.974 × 10−4 | 0.556 ** | 7.293 × 10−5 |
| Peak IT | Penguin initial | 0.715 ** | 1.148 × 10−8 | 0.413 ** | 0.0043 |
| Peak IT | Penguin final | 0.550 ** | 5.208 × 10−5 | 0.563 ** | 5.630 × 10−5 |
| Osstell initial | Penguin initial | 0.924 ** | 7.963 × 10−21 | 0.974 ** | 4.094 × 10−30 |
| Osstell final | Penguin final | 0.963 ** | 1.024 × 10−27 | 0.964 ** | 2.267 × 10−26 |
| CC | Significance (2-Tailed) | IH | Significance (2-Tailed) | ||
|---|---|---|---|---|---|
| Peak IT | Osstell initial | 0.468 ** | 0.001 | 0.112 | 0.453 |
| Peak IT | Osstell final | 0.602 ** | 7.592 × 10−6 | −0.074 | 0.626 |
| Peak IT | Penguin initial | 0.385 ** | 0.0075 | 0.100 | 0.502 |
| Peak IT | Penguin final | 0.571 ** | 2.758 × 10−5 | −0.064 | 0.668 |
| Osstell initial | Penguin initial | 0.876 ** | 7.310 × 10−16 | 0.967 ** | 0.000 |
| Osstell final | Penguin final | 0.986 ** | 1.447 × 10−36 | 0.937 ** | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raz, P.; Meir, H.; Levartovsky, S.; Peleg, M.; Sebaoun, A.; Beitlitum, I. Reliability and Correlation of Different Devices for the Evaluation of Primary Implant Stability: An In Vitro Study. Materials 2021, 14, 5537. https://doi.org/10.3390/ma14195537
Raz P, Meir H, Levartovsky S, Peleg M, Sebaoun A, Beitlitum I. Reliability and Correlation of Different Devices for the Evaluation of Primary Implant Stability: An In Vitro Study. Materials. 2021; 14(19):5537. https://doi.org/10.3390/ma14195537
Chicago/Turabian StyleRaz, Perry, Haya Meir, Shifra Levartovsky, Maia Peleg, Alon Sebaoun, and Ilan Beitlitum. 2021. "Reliability and Correlation of Different Devices for the Evaluation of Primary Implant Stability: An In Vitro Study" Materials 14, no. 19: 5537. https://doi.org/10.3390/ma14195537







