The Application of Angulated Screw-Channels in Metal-Free, Implant-Supported Restorations: A Retrospective Survival Analysis
Abstract
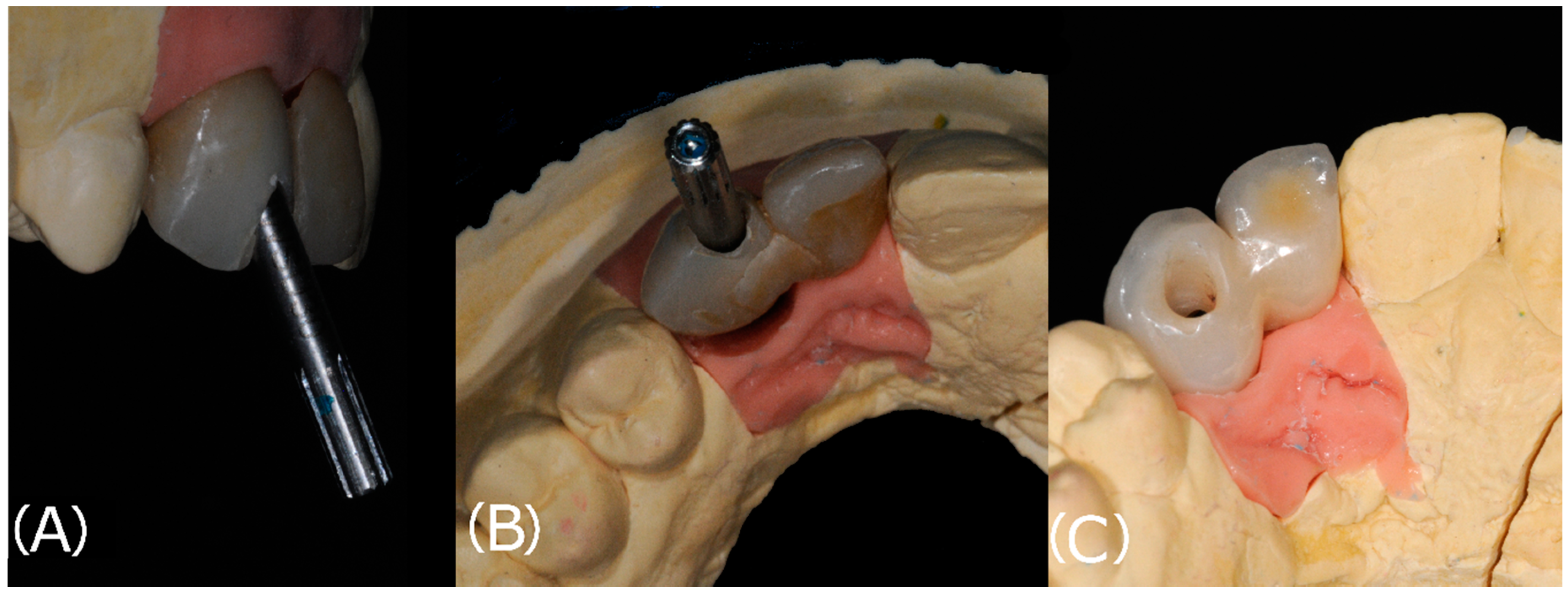
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
Success Rate
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Howe, M.-S.; Keys, W.; Richards, D. Long-Term (10-Year) Dental Implant Survival: A Systematic Review and Sensitivity Meta-Analysis. J. Dent. 2019, 84, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Tan, K.; Lang, N.P.; Brägger, U.; Egger, M.; Zwahlen, M. A Systematic Review of the Survival and Complication Rates of Fixed Partial Dentures (FPDs) after an Observation Period of at Least 5 Years. Clin. Oral Implants Res. 2004, 15, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Brägger, U.; Lang, N.P.; Zwahlen, M. Comparison of Survival and Complication Rates of Tooth-Supported Fixed Dental Prostheses (FDPs) and Implant-Supported FDPs and Single Crowns (SCs). Clin. Oral Implants Res. 2007, 18 (Suppl. 3), 97–113. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Mühlemann, S.; Zwahlen, M.; Hämmerle, C.H.F.; Schneider, D. Cemented and Screw-Retained Implant Reconstructions: A Systematic Review of the Survival and Complication Rates. Clin. Oral Implants Res. 2012, 23 (Suppl. 6), 163–201. [Google Scholar] [CrossRef]
- Serino, G.; Ström, C. Peri-Implantitis in Partially Edentulous Patients: Association with Inadequate Plaque Control. Clin. Oral Implants Res. 2009, 20, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Monje, A.; Pons, R.; Insua, A.; Nart, J.; Wang, H.-L.; Schwarz, F. Morphology and Severity of Peri-Implantitis Bone Defects. Clin. Implant Dent. Relat. Res. 2019, 21, 635–643. [Google Scholar] [CrossRef]
- Ma, S.; Fenton, A. Screw- versus Cement-Retained Implant Prostheses: A Systematic Review of Prosthodontic Maintenance and Complications. Int. J. Prosthodont. 2015, 28, 127–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thilander, B.; Odman, J.; Gröndahl, K.; Friberg, B. Osseointegrated Implants in Adolescents. An Alternative in Replacing Missing Teeth? Eur. J. Orthod. 1994, 16, 84–95. [Google Scholar] [CrossRef]
- Korsch, M.; Obst, U.; Walther, W. Cement-Associated Peri-Implantitis: A Retrospective Clinical Observational Study of Fixed Implant-Supported Restorations Using a Methacrylate Cement. Clin. Oral Implants Res. 2014, 25, 797–802. [Google Scholar] [CrossRef]
- Salinas, T.J.; Eckert, S.E. In Patients Requiring Single-Tooth Replacement, What Are the Outcomes of Implant- as Compared to Tooth-Supported Restorations? Int. J. Oral Maxillofac. Implants 2007, 22, 71–95. [Google Scholar]
- Kraus, R.D.; Epprecht, A.; Hämmerle, C.H.F.; Sailer, I.; Thoma, D.S. Cemented vs Screw-Retained Zirconia-Based Single Implant Reconstructions: A 3-Year Prospective Randomized Controlled Clinical Trial. Clin. Implant Dent. Relat. Res. 2019, 21, 578–585. [Google Scholar] [CrossRef]
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-Year Study of Osseointegrated Implants in the Treatment of the Edentulous Jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Michalakis, K.X.; Hirayama, H.; Garefis, P.D. Cement-Retained versus Screw-Retained Implant Restorations: A Critical Review. Int. J. Oral Maxillofac. Implants 2003, 18, 719–728. [Google Scholar]
- Manicone, P.F.; De Angelis, P.; Rella, E.; Papetti, L.; D’Addona, A. Proximal Contact Loss in Implant-Supported Restorations: A Systematic Review and Meta-Analysis of Prevalence. J. Prosthodont. 2021. [Google Scholar] [CrossRef] [PubMed]
- Torrado, E.; Ercoli, C.; Al Mardini, M.; Graser, G.N.; Tallents, R.H.; Cordaro, L. A Comparison of the Porcelain Fracture Resistance of Screw-Retained and Cement-Retained Implant-Supported Metal-Ceramic Crowns. J. Prosthet. Dent. 2004, 91, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Edmondson, E.K.; Trejo, P.M.; Soldatos, N.; Weltman, R.L. The Ability to Screw-Retain Single Implant-Supported Restorations in the Anterior Maxilla: A CBCT Analysis. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- Hu, E.; Petrich, A.; Imamura, G.; Hamlin, C. Effect of Screw Channel Angulation on Reverse Torque Values of Dental Implant Abutment Screws. J. Prosthodont. 2019, 28, 969–972. [Google Scholar] [CrossRef] [PubMed]
- Solá-Ruiz, M.F.; Baixauli-López, M.; Roig-Vanaclocha, A.; Amengual-Lorenzo, J.; Agustín-Panadero, R. Prospective Study of Monolithic Zirconia Crowns: Clinical Behavior and Survival Rate at a 5-Year Follow-Up. J. Prosthodont. Res. 2021, 65, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three Generations of Zirconia: From Veneered to Monolithic. Part I. Quintessence Int. Berl. Ger. 1985 2017, 48, 369–380. [Google Scholar] [CrossRef]
- Garcia-Hammaker, S.; Saglik, B.; Sierraalta, M.; Razzoog, M. Influence of Screw Channel Angulation on the Fracture Resistance of Zirconia Abutments: An In Vitro Study. J. Prosthodont. 2021, 30, 329–334. [Google Scholar] [CrossRef]
- Pol, C.W.P.; Raghoebar, G.M.; Maragkou, Z.; Cune, M.S.; Meijer, H.J.A. Full-Zirconia Single-Tooth Molar Implant-Supported Restorations with Angulated Screw Channel Abutments: A 1-Year Prospective Case Series Study. Clin. Implant Dent. Relat. Res. 2020, 22, 138–144. [Google Scholar] [CrossRef] [Green Version]
- Drew, A.; Randi, A.; DiPede, L.; Luke, A. Fracture Strength of Implant Screw-Retained All-Ceramic Crowns with the Use of the Angulated Screw Channel: A Pilot Study. Int. J. Periodontics Restorat. Dent. 2020, 40, 245–252. [Google Scholar] [CrossRef]
- Opler, R.; Wadhwani, C.; Chung, K.-H. The Effect of Screwdriver Angle Variation on the Off-Axis Implant Abutment System and Hexalobular Screw. J. Prosthet. Dent. 2020, 123, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Mulla, S.H.; Seghi, R.R.; Johnston, W.M.; Yilmaz, B. Effect of Cyclic Loading on Reverse Torque Values of Angled Screw Channel Systems. J. Prosthet. Dent. 2021, 21, S0022-3913. [Google Scholar] [CrossRef] [PubMed]
- Vigolo, P.; Gracis, S.; Carboncini, F.; Mutinelli, S.; AIOP (Italian Academy of Prosthetic Dentistry) Clinical Research Group. Internal-vs External-Connection Single Implants: A Retrospective Study in an Italian Population Treated by Certified Prosthodontists. Int. J. Oral Maxillofac. Implants 2016, 31, 1385–1396. [Google Scholar] [CrossRef] [Green Version]
- De Angelis, P.; Gasparini, G.; Rella, E.; De Angelis, S.; Grippaudo, C.; D’Addona, A.; Manicone, P.F. Patient Satisfaction with Implant-Supported Monolithic and Partially Veneered Zirconia Restorations. BioMed Res. Int. 2021, 2021, 669293. [Google Scholar] [CrossRef]
- De Angelis, P.; Gasparini, G.; Camodeca, F.; De Angelis, S.; Liguori, M.G.; Rella, E.; Cannata, F.; D’Addona, A.; Manicone, P.F. Technical and Biological Complications of Screw-Retained (CAD/CAM) Monolithic and Partial Veneer Zirconia for Fixed Dental Prostheses on Posterior Implants Using a Digital Workflow: A 3-Year Cross-Sectional Retrospective Study. BioMed Res. Int. 2021, 2021, 5581435. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.G.; Gavric, J.; Belser, U.C.; Bornstein, M.M.; Joda, T.; Chappuis, V.; Sailer, I.; Brägger, U. Esthetic and Clinical Performance of Implant-Supported All-Ceramic Crowns Made with Prefabricated or CAD/CAM Zirconia Abutments: A Randomized, Multicenter Clinical Trial. J. Dent. Res. 2017, 96, 163–170. [Google Scholar] [CrossRef]
- Lv, X.-L.; Qian, S.-J.; Qiao, S.-C.; Gu, Y.-X.; Lai, H.-C.; Shi, J.-Y. Clinical, Radiographic, and Immunological Evaluation of Angulated Screw-Retained and Cemented Single-Implant Crowns in the Esthetic Region: A 1-Year Randomized Controlled Clinical Trial. Clin. Implant Dent. Relat. Res. 2021, 23, 692–702. [Google Scholar] [CrossRef]
- Amorfini, L.; Storelli, S.; Mosca, D.; Scanferla, M.; Romeo, E. Comparison of Cemented vs Screw-Retained, Customized Computer-Aided Design/Computer-Assisted Manufacture Zirconia Abutments for Esthetically Located Single-Tooth Implants: A 10-Year Randomized Prospective Study. Int. J. Prosthodont. 2018, 31, 359–366. [Google Scholar] [CrossRef]
- Manicone, P.F.; Rossi Iommetti, P.; Raffaelli, L. An Overview of Zirconia Ceramics: Basic Properties and Clinical Applications. J. Dent. 2007, 35, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Habibi, Y.; Dawid, M.-T.; Waldecker, M.; Rammelsberg, P.; Bömicke, W. Three-Year Clinical Performance of Monolithic and Partially Veneered Zirconia Ceramic Fixed Partial Dentures. J. Esthet. Restor. Dent. 2020, 32, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Bömicke, W.; Rammelsberg, P.; Stober, T.; Schmitter, M. Short-Term Prospective Clinical Evaluation of Monolithic and Partially Veneered Zirconia Single Crowns. J. Esthet. Restor. Dent. 2017, 29, 22–30. [Google Scholar] [CrossRef] [PubMed]




| Variable | Absolute Frequency (Relative Frequency) |
|---|---|
| Sex | |
| Male | 52 (49.52%) |
| Female | 53 (50.48%) |
| Design of Restoration | |
| Monolithic Zirconia | 52 (49.52%) |
| Partially veneered Zirconia | 53 (50.48%) |
| Type of restoration | |
| FPD | 51 (48.57%) |
| SC | 54 (51.43%) |
| Condition of Antagonist Tooth | |
| Natural Tooth | 58 (55.24%) |
| Tooth supported FPD | 26 (24.76%) |
| Implant supported FPD | 12 (11.43%) |
| Missing antagonist | 4 (3.81%) |
| RPD | 5 (4.76%) |
| Time (Months) | At Risk | Fail | Lost | Survivor Function | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| 5 | 105 | 1 | 0 | 0.99 | 0.93 | 0.99 |
| 7 | 104 | 0 | 1 | 0.99 | 0.93 | 0.99 |
| 9 | 103 | 2 | 1 | 0.98 | 0.92 | 0.99 |
| 12 | 100 | 2 | 3 | 0.97 | 0.91 | 0.99 |
| 18 | 100 | 1 | 6 | 0.95 | 0.88 | 0.97 |
| 24 | 88 | 0 | 16 | 0.94 | 0.87 | 0.97 |
| 30 | 72 | 1 | 19 | 0.94 | 0.87 | 0.97 |
| 36 | 52 | 0 | 35 | 0.92 | 0.85 | 0.96 |
| 42 | 17 | 0 | 10 | 0.92 | 0.85 | 0.96 |
| Time | Survivor Function | |
|---|---|---|
| Monolithic Zirconia | Partially Veneered Zirconia | |
| 12 Months | 1.0 | 0.94 |
| 18 Months | 0.98 | 0.92 |
| 36 Months | 0.95 | 0.90 |
| 47 Months | 0.95 | 0.90 |
| 53 Months | – | 0.90 |
| Variables | Hazard Ratio | p-Value | 95% Confidence Interval |
|---|---|---|---|
| Design of restoration | – | – | – |
| Stratified Zirconia | 6.044 | 0.039 | 1.102–37.626 |
| Type of restoration | – | – | – |
| Single Crown | 0.420 | 0.279 | 0.087–2.021 |
| Position of restoration | – | – | – |
| Posterior Restoration | 6.592 | 0.099 | 0.700–62.043 |
| Condition of antagonist tooth | – | – | – |
| Tooth Supported FPD | 1.148 | 0.876 | 0.201–6.535 |
| Implant Supported FPD | 0.845 | 0.895 | 0.070–10.127 |
| RPD | <0.001 | 1 | – |
| Missing antagonist | <0.001 | 1 | – |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rella, E.; De Angelis, P.; Damis, G.; D’Addona, A.; Manicone, P.F. The Application of Angulated Screw-Channels in Metal-Free, Implant-Supported Restorations: A Retrospective Survival Analysis. Materials 2021, 14, 7006. https://doi.org/10.3390/ma14227006
Rella E, De Angelis P, Damis G, D’Addona A, Manicone PF. The Application of Angulated Screw-Channels in Metal-Free, Implant-Supported Restorations: A Retrospective Survival Analysis. Materials. 2021; 14(22):7006. https://doi.org/10.3390/ma14227006
Chicago/Turabian StyleRella, Edoardo, Paolo De Angelis, Giovanni Damis, Antonio D’Addona, and Paolo Francesco Manicone. 2021. "The Application of Angulated Screw-Channels in Metal-Free, Implant-Supported Restorations: A Retrospective Survival Analysis" Materials 14, no. 22: 7006. https://doi.org/10.3390/ma14227006






