Evaluation of Biodentine in Pulpotomies of Primary Teeth with Different Stages of Root Resorption Using a Novel Composite Outcome Score
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
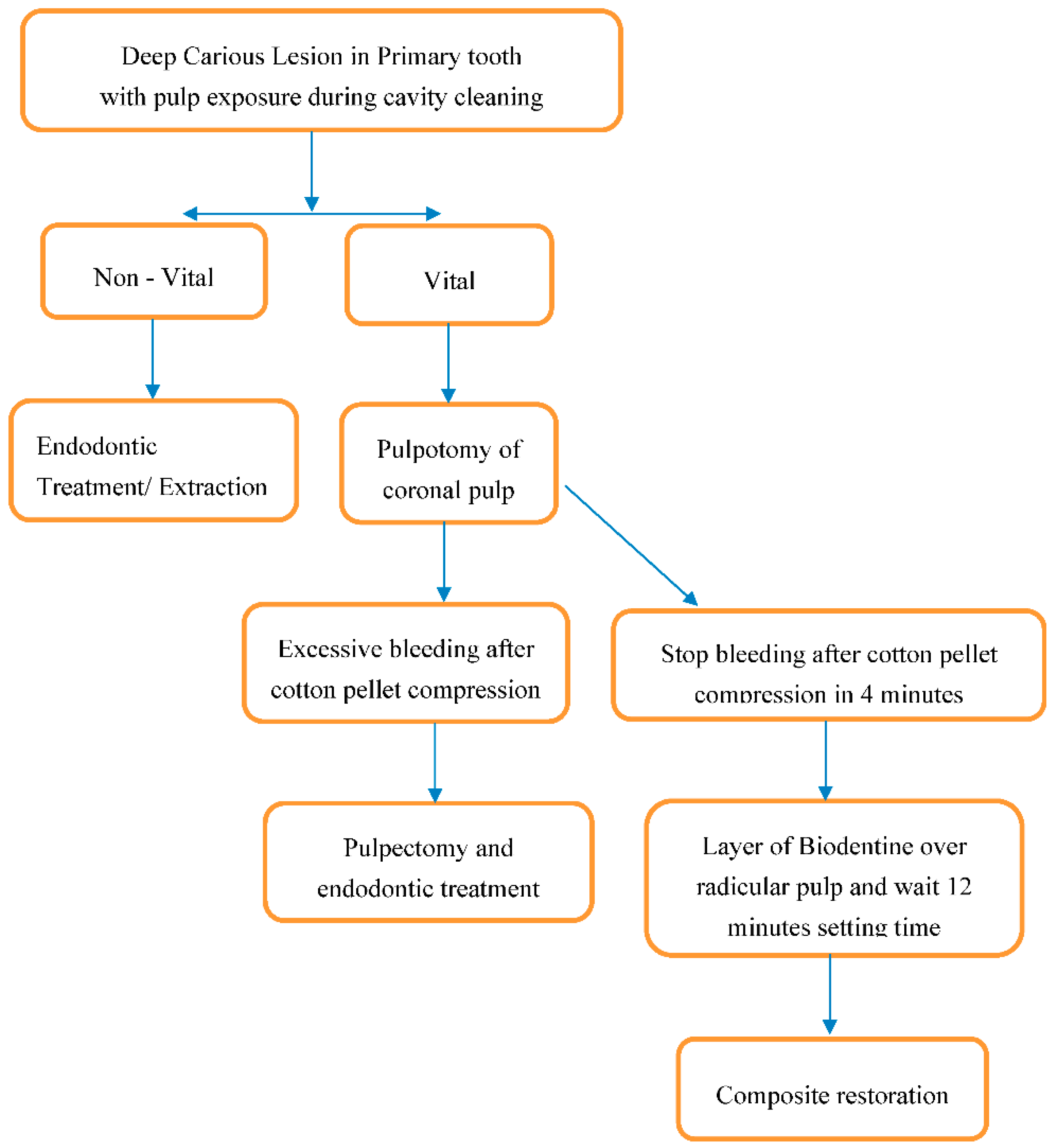
2.2. Clinical Procedures
2.3. Clinical and Radiographic Outcomes
2.4. Statistical Analysis
3. Results
3.1. Clinical and Radiographic Outcomes
3.2. Patient-Related Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kazeminia, M.; Abdi, A.; Shohaimi, S.; Jalali, R.; Vaisi-Raygani, A.; Salari, N.; Mohammadi, M. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: A systematic review and meta-analysis. Head Face Med. 2020, 16, 22. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, P.; Petersen, P.E. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004, 7, 201–226. [Google Scholar] [CrossRef]
- Brosnan, M.G.; Natarajan, A.K.; Campbell, J.M.; Drummond, B.K. Management of the pulp in primary teeth–an update. N. Z. Dent. J. 2014, 110, 119–123. [Google Scholar] [PubMed]
- Dhar, V.; Marghalani, A.A.; Crystal, Y.O.; Kumar, A.; Ritwik, P.; Tulunoglu, O.; Graham, L. Use of vital pulp therapies in primary teeth with deep caries lesions. Paediatr. Dent. 2017, 39, 146–159. [Google Scholar]
- Bossù, M.; Iaculli, F.; Di Giorgio, G.; Salucci, A.; Polimeni, A.; Di Carlo, S. Different pulp dressing materials for the pulpotomy of primary teeth: A systematic review of the literature. J. Clin. Med. 2020, 9, 838. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, B.O. Pulpotomy in primary molars: Long-term clinical and histological evaluation. Int. Endod. J. 1980, 13, 143–155. [Google Scholar] [CrossRef]
- Ounsi, H.F.; Debaybo, D.; Salameh, Z.; Chebaro, A.; Bassam, H. Endodontic considerations in pediatric dentistry: A clinical perspective. Int. Dent. SA 2009, 11, 40–50. [Google Scholar]
- Law, A.; Messer, H. An evidence-based analysis of the antibacterial effectiveness of intracanal medicaments. J. Endod. 2004, 30, 689–694. [Google Scholar] [CrossRef]
- Stanley, H.R. Pulp capping: Conserving the dental pulp—Can it be done? Is it worth it? Oral Surg. Oral Med. Oral Pathol. 1989, 68, 628–639. [Google Scholar] [CrossRef]
- Torabinejad, M.; Watson, T.F.; Ford Pitt, T.R. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J. Endod. 1993, 19, 591–595. [Google Scholar] [CrossRef]
- Magnusson, B. Attempts to predict prognosis of pulpotomy in primary molars. Bacteriologic and histologic examination. Scand. J. Dent. Res. 1970, 78, 232–240. [Google Scholar] [CrossRef]
- Via, W.F., Jr. Evaluation of deciduous molars treated by pulpotomy and calcium hydroxide. J. Am. Dent. Assoc. 1955, 50, 34–41. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatric Dentistry. Pulp therapy for primary and immature permanent teeth. Pediatr. Dent. 2017, 39, 325–333. [Google Scholar]
- Palma, P.J.; Marques, J.A.; Santos, J.; Falacho, R.I.; Sequeira, D.; Diogo, P.; Caramelo, F.; Ramos, J.C.; Santos, J.M. Tooth discoloration after regenerative endodontic procedures with calcium silicate-based cements—An ex vivo study. Appl. Sci. 2020, 10, 5793. [Google Scholar] [CrossRef]
- Neamatollahi, H.; Tajik, A. Comparison of clinical and radiographic success rates of pulpotomy in primary molars using formocresol, ferric sulfate and mineral trioxide aggregate (MTA). J. Dent. 2006, 3, 6–14. [Google Scholar]
- Balaprasanna Kumar, C. Pulpotomy in primary teeth—A review. JIADS 2011, 2, 29–31. [Google Scholar]
- Swift, E.J.; Trope, M.; Ritter, A.V. Vital pulp therapy for the mature tooth—Can it work? Endod. Top. 2003, 5, 49–56. [Google Scholar] [CrossRef]
- Camilleri, J.; Sorrentino, F.; Damidot, D. Investigation of the hydration and bioactivity of radiopacified tricalcium silicate cement, Biodentine and MTA Angelus. Dent. Mater. 2013, 29, 580–593. [Google Scholar] [CrossRef]
- Kim, J.R.; Nosrat, A.; Fouad, A.F. Interfacial characteristics of Biodentine and MTA with dentine in simulated body fluid. J. Dent. 2015, 43, 241–247. [Google Scholar] [CrossRef]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part III: Clinical applications, drawbacks, and mechanism of action. J. Endod. 2010, 36, 400–441. [Google Scholar] [CrossRef]
- Camilleri, J. Color stability of white mineral trioxide aggregate in contact with hypochlorite solution. J. Endod. 2014, 40, 436–440. [Google Scholar] [CrossRef]
- Smaïl-Faugeron, V.; Glenny, A.M.; Courson, F.; Durieux, P.; Muller-Bolla, M.; Fron Chabouis, H. Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst. Rev. 2018, 5, CD003220. [Google Scholar] [CrossRef]
- Kaur, M.; Singh, H.; Dhillon, J.S.; Batra, M.; Saini, M. MTA versus Biodentine: Review of literature with a comparative analysis. J. Clin. Diagn. Res. 2017, 11, ZG01–ZG05. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, A.N.; Nikonov, S.Y.; Pancio, A.K.; Niu, L.N.; Agee, K.A.; Loushine, R.J.; Weller, R.N.; Pashley, D.H.; Tay, F.R. Effects of calcium silicate-based materials on the flexural properties of dentin. J. Endod. 2012, 38, 680–683. [Google Scholar] [CrossRef] [PubMed]
- Dammaschke, T. A new bioactive cement for direct pulp capping. Int. Dent. SA 2008, 2, 64–69. [Google Scholar]
- Aminabadi, N.A.; Farahani, R.M.; Gajan, E.B. A clinical study of formocresol pulpotomy versus root canal therapy of vital primary incisors. J. Clin. Pediatr. Dent. 2008, 32, 211–214. [Google Scholar] [CrossRef]
- Fuks, A.B. Vital pulp therapy with new materials for primary teeth: New directions and treatment perspectives. Pediatr. Dent. 2008, 30, 211–219. [Google Scholar] [CrossRef]
- Demars, C.; Fortier, J.P. Propos sur l’endodontie des dents temporaires. Actual Odontostomatol. 1981, 35, 213–224. [Google Scholar]
- Fortier, J.P.; Demars-Fremault, C. Abrégé de Pédodontie; Masson: Paris, France, 1987. [Google Scholar]
- Smail-Faugeron, V.; Fron Chabouis, H.; Durieux, P.; Attal, J.-P.; Muller-Bolla, M.; Courson, F. Development of a core set of outcomes for randomized controlled trials with multiple outcomes—Example of pulp treatments of primary teeth for extensive decay in children. PLoS ONE 2013, 8, e51908. [Google Scholar]
- Garra, G.; Singer, A.J.; Taira, B.R.; Chohan, J.; Cardoz, H.; Chisena, E.; Thode, H.C., Jr. Validation of the Wong-Baker Faces pain rating scale in pediatric emergency department patients. Acad. Emerg. Med. 2010, 17, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Riba, H.; Al-Zahrani, S.; Al-Buqmi, N.; Al-Jundi, A. A review of behavior evaluation scales in pediatric dentistry and suggested modification to the Frankl scale. EC Dent. Sci. 2017, 16, 269–275. [Google Scholar]
- Niranjani, K.; Prasad, M.G.; Vasa, A.A.; Divya, G.; Thakur, M.S.; Saujanya, K. Clinical evaluation of success of primary teeth pulpotomy using mineral trioxide aggregate, laser and Biodentine™—An in vivo study. J. Clin. Diagn. Res. 2015, 9, ZC35–ZC37. [Google Scholar] [CrossRef] [PubMed]
- Xuan, X.V.; Salehi, H.; Truong, M.T.; Sandra, M.; Sadoine, J.; Jacquot, B.; Cuisinier, F.; Chaussain, C.; Boukpessi, T. Reparative mineralized tissue characterization after direct pulp capping with calcium-silicate-based cements. Materials 2019, 12, 2102. [Google Scholar]
- Rajasekharan, S.; Martens, L.C.; Vandenbulcke, J.; Jacquet, W.; Bottenberg, P.; Cauwels, R.G. Efficacy of three different pulpotomy agents in primary molars: A randomized control trial. Int. Endod. J. 2017, 50, 215–228. [Google Scholar] [CrossRef]
- Cuadros-Fernández, C.; Lorente Rodríguez, A.I.; Sáez-Martínez, S.; García-Binimelis, J.; About, I.; Mercadé, M. Short-term treatment outcome of pulpotomies in primary molars using mineral trioxide aggregate and Biodentine™: A randomized clinical trial. Clin. Oral Investig. 2016, 20, 1639–1645. [Google Scholar] [CrossRef]
- Nasseh, H.N.; El Noueiri, B.; Pilipili, C.; Ayoub, F. Evaluation of Biodentine pulpotomies in deciduous molars with physiological root resorption (Stage 3). Int. J. Clin. Pediatr. Dent. 2018, 11, 393–398. [Google Scholar]
- Nasrallah, H.; El Noueiri, B.; Pilipili, C.; Ayoub, F. Clinical and radiographic evaluations of Biodentine™ pulpotomies in mature primary molars (Stage 2). Int. J. Clin. Pediatr. Dent. 2018, 11, 496–504. [Google Scholar]
- Collado-González, M.; García-Bernal, D.; Oñate-Sánchez, R.E.; Ortolani-Seltenerich, P.S.; Álvarez-Muro, T.; Lozano, A.; Fornel, L.; Llena, C.; Moraleda, J.M.; Rodriguez-Lozano, F.J. Cytotoxicity and bioactivity of various pulpotomy materials on stem cells from human exfoliated primary teeth. Int. Endod. J. 2017, 50 (Suppl. 2), e19–e30. [Google Scholar] [CrossRef]
- Coll, J.A.; Seale, N.S.; Vargas, K.; Marghalani, A.A.; Al Shamali, S.; Graham, L. Primary tooth vital pulp therapy: A systematic review and meta-analysis. Pediatr. Dent. 2017, 39, 16–123. [Google Scholar]
- Caruso, S.; Dinoi, T.; Marzo, G.; Campanella, V.; Giuca, M.R.; Gatto, R.; Pasini, M. Clinical and radiographic evaluation of Biodentine versus calcium hydroxide in primary teeth pulpotomies: A retrospective studies. BMC Oral. Health 2018, 18, 54. [Google Scholar] [CrossRef]
- Guelmann, M.; Shapira, J.; Silva, D.R.; Fuks, A.B. Esthetic restorative options for pulpotomized primary molars: A review of literature. J. Clin. Pediatr. Dent. 2011, 36, 123–126. [Google Scholar] [CrossRef]
- Koubi, G.; Colon, P.; Franquin, J.C.; Hartmann, A.; Richard, G.; Faure, M.O.; Lambert, G. Clinical evaluation of the performance and safety of a new dentine substitute, biodentine, in the restoration of posterior teeth—A prospective study. Clin. Oral Investig. 2013, 17, 243–249. [Google Scholar] [CrossRef]
- Palma, P.J.; Marques, J.A.; Falacho, R.I.; Vinagre, A.; Santos, J.M.; Ramos, J.C. Does delayed restoration improve shear bond strength of different restorative protocols to calcium silicate-based cements? Materials 2018, 11, 2216. [Google Scholar] [CrossRef] [PubMed]
- Shafie, L.; Barghi, H.; Parirokh, M.; Ebrahimneiad, H.; Nakhae, N.; Esmalif, S. Postoperative pain following pulpotomy of primary molars with two biomaterials: A randomized split mouth clinical trial. Iran. Endod. J. 2017, 12, 10–14. [Google Scholar] [PubMed]
- von Baeyer, C.L. Children’s self-reports of pain intensity: Scale selection, limitations and interpretation. Pain Res. Manag. 2006, 11, 157–162. [Google Scholar] [CrossRef]
- Brill, W.A. Behavior of pediatric dental patients throughout the course of restorative dental treatment in a private pediatric dental practice. J. Clin. Pediatr. Dent. 2001, 26, 55–60. [Google Scholar] [CrossRef]
- Sivakumar, P.; Gurunathan, D. Behavior of children toward various dental procedures. Int. J. Clin. Pediatr. Dent. 2019, 12, 379–384. [Google Scholar] [CrossRef]
- Andreasen, J.O. Pulp and periodontal tissue repair—regeneration or tissue metaplasia after dental trauma. A review. Dent. Traumatol. 2012, 28, 19–24. [Google Scholar] [CrossRef]



| OUTCOMES | 3 MONTHS | 6 MONTHS | 12 MONTHS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Clinical | + | − | NA | + | − | NA | + | − | NA |
| Soft tissue pathology | 0 | 22 (100%) | 0 | 1 (4.5%) | 20 (90.9%) | 1 (4.5%) | 1 (4.5%) | 19 (86.3%) | 2 (9.0%) |
| Pain to percussion | 0 | 22 (100%) | 0 | 1 (4.5%) | 20 (90.9%) | 1 (4.5%) | 1 (4.5%) | 19 (86.3%) | 2 (9.0%) |
| Pathologic mobility | 0 | 22 (100%) | 0 | 1 (4.5%) | 20 (90.9%) | 1 (4.5%) | 1 (4.5%) | 19 (86.3%) | 2 (9.0%) |
| Radiological | + | − | NA | + | − | NA | + | − | NA |
| Pathologic radiolucency | - | - | - | 1 (4.5%) | 20 (90.9%) | 1 (4.5%) | 1 (4.5%) | 19 (86.3%) | 2 (9.0%) |
| Pathologic root resorption | - | - | - | 1 (4.5%) | 20 (90.9%) | 1 (4.5%) | 1 (4.5%) | 19 (86.3%) | 2 (9.0%) |
| Composite score | 1 (4.5%) | 20 (90.9%) | 1 (4.5%) | 1 (4.5%) | 19 (86.3%) | 2 (9.0%) | |||
| Age | Wong-Baker Scale | p Value | Frankl scale | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Mild/Moderate | Severe | Definitely Negative | Negative | Intermediate | Positive | Definitely Positive | |||
| 5–6 years | 0 | 4 (36.4) | 5 | 0.041 | 0 | 0 | 3 (60) | 6 (40) | 0 | 0.006 |
| 7–9 years | 3 (60) | 6 (54.5) | 1 | 0 | 0 | 2 (40) | 8 (53.3) | 0 | ||
| 10–11 years | 2 (40) | 1 (9.1) | 0 | 0 | 0 | 0 | 1 (6.7) | 2 (100) | ||
| Total | 5 | 11 | 6 | 0 | 0 | 5 | 15 | 2 | ||
| Stage | Wong-Baker scale | p Value | Frankl Scale | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Mild/Moderate | Severe | Definitely Negative | Negative | Intermediate | Positive | Definitely Positive | |||
| S | 2 (40) | 4 (36.4) | 3 (50) | 0.860 | 0 | 0 | 3 (60) | 5 (33.3) | 1 (50) | 0.555 |
| R | 3 (60) | 7 (63.6) | 3 (50) | 0 | 0 | 2 (40) | 10 (66.4) | 1 (50) | ||
| Total | 5 | 11 | 6 | 0 | 0 | 5 | 15 | 2 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guagnano, R.; Romano, F.; Defabianis, P. Evaluation of Biodentine in Pulpotomies of Primary Teeth with Different Stages of Root Resorption Using a Novel Composite Outcome Score. Materials 2021, 14, 2179. https://doi.org/10.3390/ma14092179
Guagnano R, Romano F, Defabianis P. Evaluation of Biodentine in Pulpotomies of Primary Teeth with Different Stages of Root Resorption Using a Novel Composite Outcome Score. Materials. 2021; 14(9):2179. https://doi.org/10.3390/ma14092179
Chicago/Turabian StyleGuagnano, Rosa, Federica Romano, and Patrizia Defabianis. 2021. "Evaluation of Biodentine in Pulpotomies of Primary Teeth with Different Stages of Root Resorption Using a Novel Composite Outcome Score" Materials 14, no. 9: 2179. https://doi.org/10.3390/ma14092179
APA StyleGuagnano, R., Romano, F., & Defabianis, P. (2021). Evaluation of Biodentine in Pulpotomies of Primary Teeth with Different Stages of Root Resorption Using a Novel Composite Outcome Score. Materials, 14(9), 2179. https://doi.org/10.3390/ma14092179






