Stability of Cantilever Fixed Dental Prostheses on Zirconia Implants
Abstract
:1. Introduction
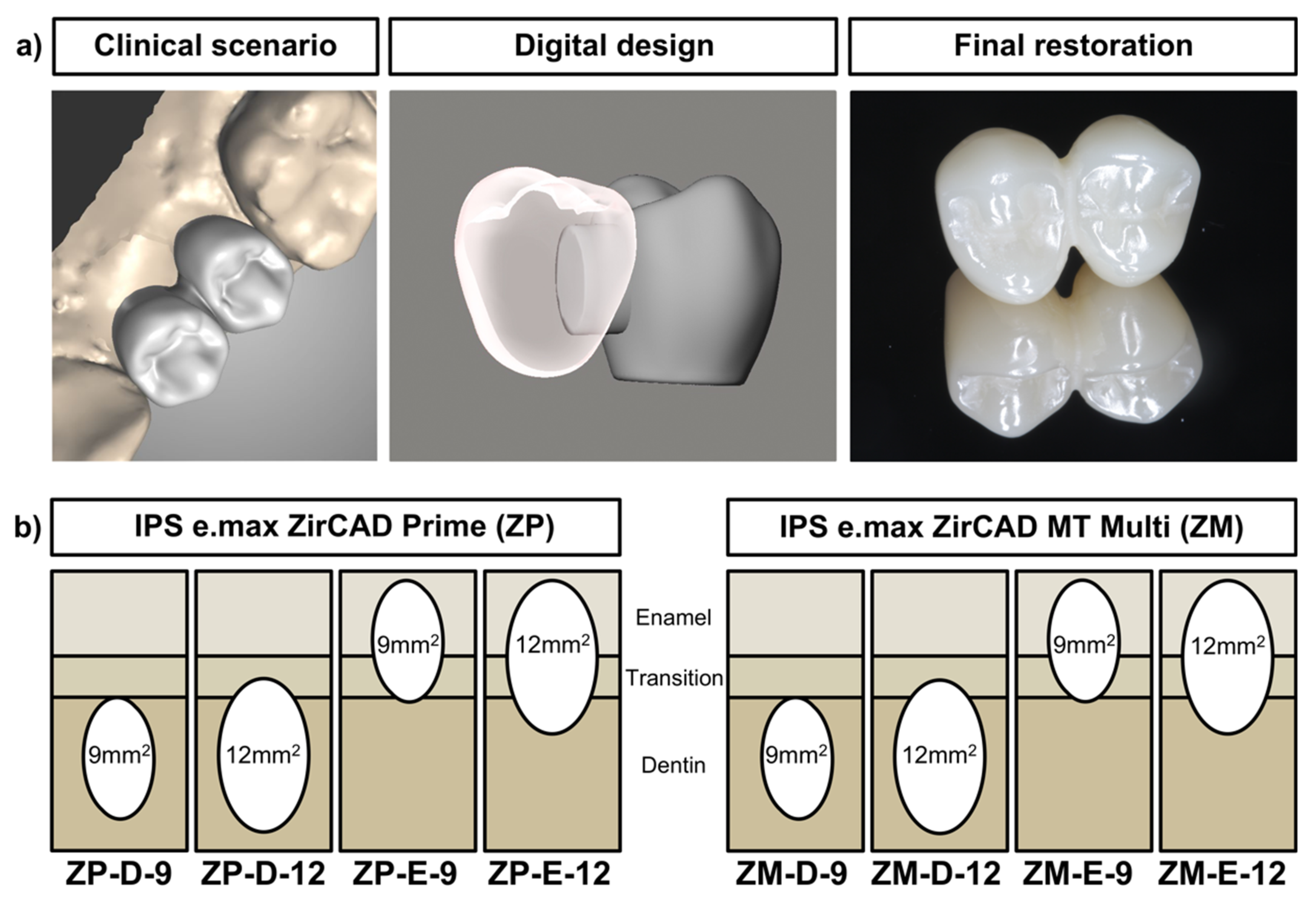
2. Materials and Methods
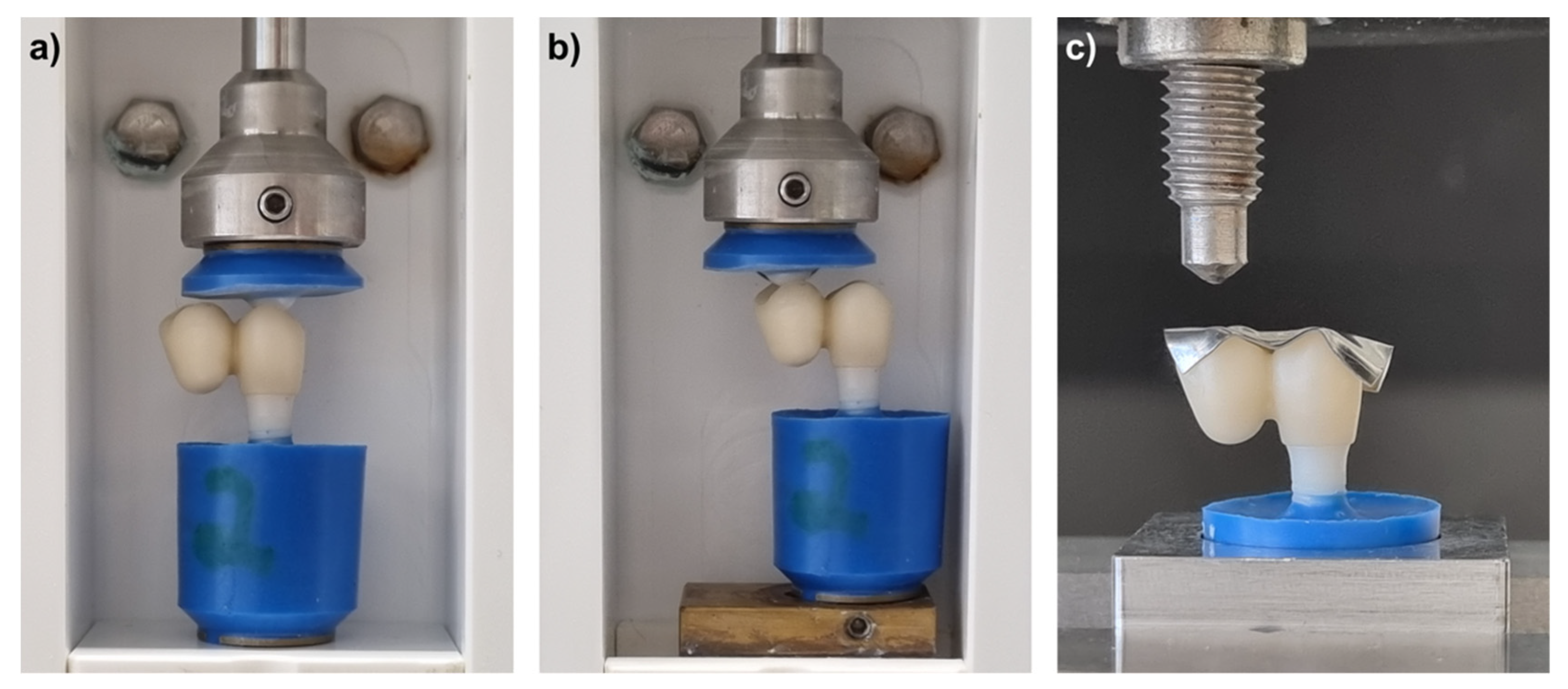
2.1. Chewing Simulation
2.2. Fracture Load
2.3. Biaxial Flexural Strength
2.4. Statistics
3. Results
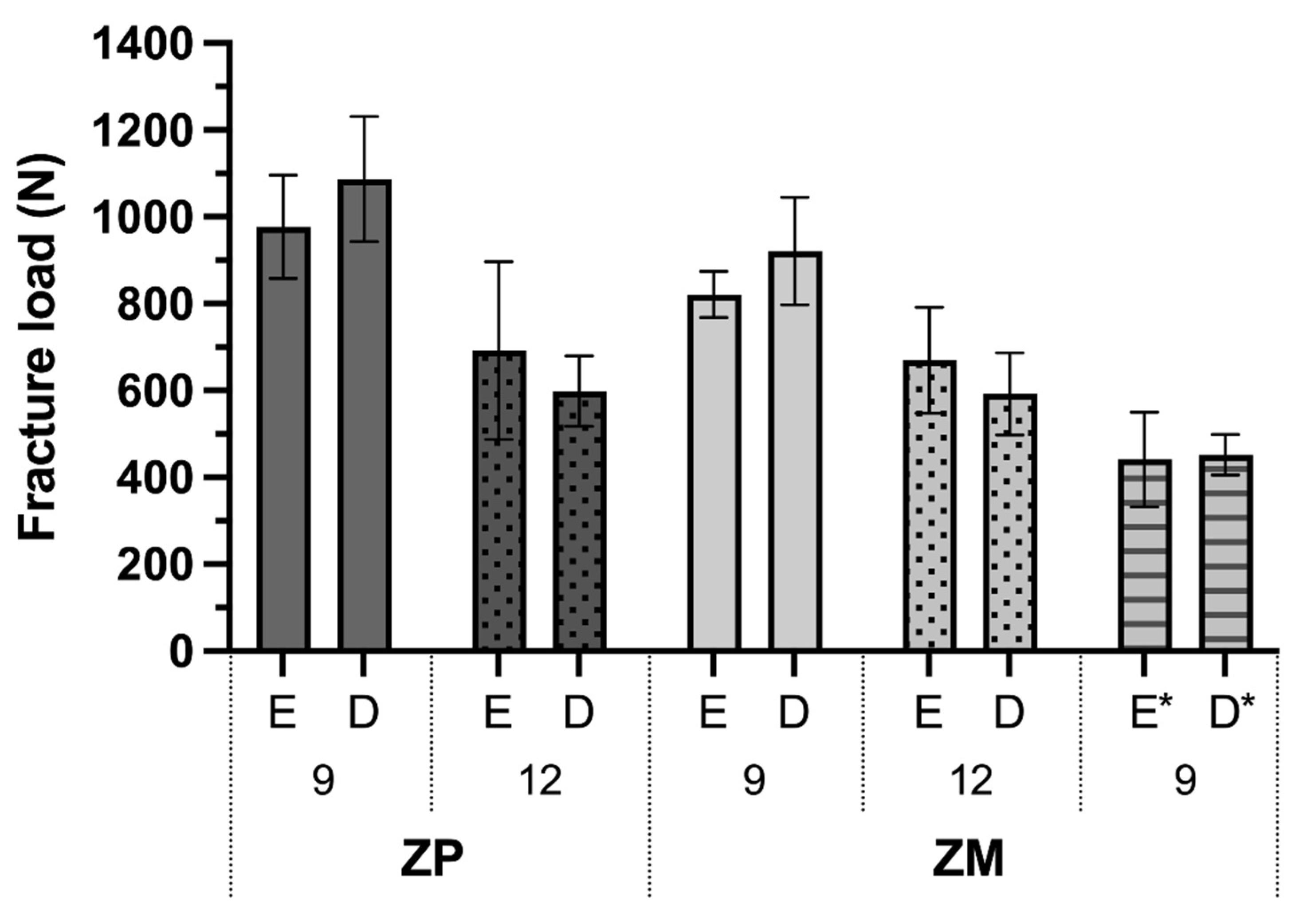
3.1. Fracture Load and Fracture Analysis
3.2. Biaxial Flexural Strength
4. Discussion
5. Conclusions
- Higher fracture load values are obtained for cantilever restorations with a 9 mm2 than for a 12 mm2 connector.
- Fracture load values are significantly higher for ICFDPs made of 3Y-TZP/5Y-PSZ than for 4Y-PSZ disks, while implant fractures are also increased with high-strength zirconia restorations.
- The position of the ICFDP within the enamel or dentin layer of the zirconia disk does not affect fracture load values significantly.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3Y-TZP | 3 mol% yttria-stabilized tetragonal zirconia |
| 4Y/5Y-PSZ | 4/5 mol% yttria partially stabilized zirconia |
| Al | aluminum |
| BSE | backscattered electron |
| D | dentin layer |
| E | enamel layer |
| EDX | energy-dispersive X-ray spectroscopy |
| FDP | fixed dental prosthesis |
| HF | hafnium |
| ICFDP | implant-supported cantilever fixed dental prostheses |
| M | middle layer |
| MDP | 10-methacryloyloxydecyl dihydrogen phosphate |
| O | oxygen |
| SE | secondary electron |
| SEM | scanning electron microscopy |
| Y | yttrium |
| ZM | IPS e.max ZirCAD MT Multi group |
| ZP | IPS e.max ZirCAD Prime group |
| Zr | zirconium |
References
- Zurdo, J.; Romão, C.; Wennström, J.L. Survival and Complication Rates of Implant-Supported Fixed Partial Dentures with Cantilevers: A Systematic Review. Clin. Oral Implant. Res. 2009, 20 (Suppl. 4), 59–66. [Google Scholar] [CrossRef]
- Van Nimwegen, W.G.; Raghoebar, G.M.; Tymstra, N.; Vissink, A.; Meijer, H.J.A. How to Treat Two Adjacent Missing Teeth with Dental Implants. A Systematic Review on Single Implant-Supported Two-Unit Cantilever FDP’s and Results of a 5-Year Prospective Comparative Study in the Aesthetic Zone. J. Oral Rehabil. 2017, 44, 461–471. [Google Scholar] [CrossRef]
- Roccuzzo, A.; Jensen, S.S.; Worsaae, N.; Gotfredsen, K. Implant-Supported 2-Unit Cantilevers Compared with Single Crowns on Adjacent Implants: A Comparative Retrospective Case Series. J. Prosthet. Dent. 2019, 123, 717–723. [Google Scholar] [CrossRef]
- de Souza Batista, V.E.; Verri, F.R.; Almeida, D.A.F.; Santiago, J.F., Jr.; Lemos, C.A.A.; Pellizzer, E.P. Finite Element Analysis of Implant-Supported Prosthesis with Pontic and Cantilever in the Posterior Maxilla. Comput. Methods Biomech. Biomed. Eng. 2017, 20, 663–670. [Google Scholar] [CrossRef] [Green Version]
- Sailer, I.; Strasding, M.; Valente, N.A.; Zwahlen, M.; Liu, S.; Pjetursson, B.E. A Systematic Review of the Survival and Complication Rates of Zirconia-Ceramic and Metal-Ceramic Multiple-Unit Fixed Dental Prostheses. Clin. Oral Implant. Res. 2018, 29 (Suppl. 16), 184–198. [Google Scholar] [CrossRef] [Green Version]
- Chevalier, J.; Gremillard, L.; Virkar, A.V.; Clarke, D.R. The Tetragonal-Monoclinic Transformation in Zirconia: Lessons Learned and Future Trends. J. Am. Ceram. Soc. 2009, 92, 1901–1920. [Google Scholar] [CrossRef]
- Zhang, Y.; Lawn, B.R. Novel Zirconia Materials in Dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef]
- Kolakarnprasert, N.; Kaizer, M.R.; Kim, D.K.; Zhang, Y. New Multi-Layered Zirconias: Composition, Microstructure and Translucency. Dent. Mater. 2019, 35, 797–806. [Google Scholar] [CrossRef]
- Kaizer, M.R.; Kolakarnprasert, N.; Rodrigues, C.; Chai, H.; Zhang, Y. Probing the Interfacial Strength of Novel Multi-Layer Zirconias. Dent. Mater. 2020, 36, 60–67. [Google Scholar] [CrossRef]
- van Velzen, F.J.J.; Ofec, R.; Schulten, E.A.J.M.; Ten Bruggenkate, C.M. 10-Year Survival Rate and the Incidence of Peri-Implant Disease of 374 Titanium Dental Implants with a SLA Surface: A Prospective Cohort Study in 177 Fully and Partially Edentulous Patients. Clin. Oral Implants Res. 2015, 26, 1121–1128. [Google Scholar] [CrossRef]
- Howe, M.-S.; Keys, W.; Richards, D. Long-Term (10-Year) Dental Implant Survival: A Systematic Review and Sensitivity Meta-Analysis. J. Dent. 2019, 84, 9–21. [Google Scholar] [CrossRef]
- Thoma, D.S.; Maggetti, I.; Waller, T.; Hämmerle, C.H.F.; Jung, R.E. Clinical and Patient-Reported Outcomes of Implants Placed in Autogenous Bone Grafts and Implants Placed in Native Bone: A Case-Control Study with a Follow-up of 5–16 Years. Clin. Oral Implant. Res. 2019, 30, 242–251. [Google Scholar] [CrossRef] [Green Version]
- Buser, D.; Janner, S.F.M.; Wittneben, J.-G.; Brägger, U.; Ramseier, C.A.; Salvi, G.E. 10-Year Survival and Success Rates of 511 Titanium Implants with a Sandblasted and Acid-Etched Surface: A Retrospective Study in 303 Partially Edentulous Patients. Clin. Implant Dent. Relat. Res. 2012, 14, 839–851. [Google Scholar] [CrossRef]
- Kohal, R.-J.; Spies, B.C.; Vach, K.; Balmer, M.; Pieralli, S. A Prospective Clinical Cohort Investigation on Zirconia Implants: 5-Year Results. J. Clin. Med. 2020, 9, 2585. [Google Scholar] [CrossRef]
- Balmer, M.; Spies, B.C.; Kohal, R.; Hämmerle, C.H.; Vach, K.; Jung, R.E. Zirconia Implants Restored with Single Crowns or Fixed Dental Prostheses: 5-year Results of a Prospective Cohort Investigation. Clin. Oral Implants Res. 2020, 31, 452–462. [Google Scholar] [CrossRef]
- Spies, B.C.; Witkowski, S.; Vach, K.; Kohal, R.-J. Clinical and Patient-Reported Outcomes of Zirconia-Based Implant Fixed Dental Prostheses: Results of a Prospective Case Series 5 Years after Implant Placement. Clin. Oral Implant. Res. 2018, 29, 91–99. [Google Scholar] [CrossRef]
- Kohal, R.-J.; Kilian, J.; Stampf, S.; Spies, B. All-Ceramic Single Crown Restauration of Zirconia Oral Implants and Its Influence on Fracture Resistance: An Investigation in the Artificial Mouth. Materials 2015, 8, 1577–1589. [Google Scholar] [CrossRef] [Green Version]
- Kohal, R.-J.; Finke, H.C.; Klaus, G. Stability of Prototype Two-Piece Zirconia and Titanium Implants after Artificial Aging: An In Vitro Pilot Study. Clin. Implant Dent. Relat. Res. 2009, 11, 323–329. [Google Scholar] [CrossRef]
- AlHomidhi, M.; Alqahtani, F. Evaluation of Fracture Load of Cement-, Screw-, and Multiscrew-Retained Abutments for Implant-Supported Fixed Partial Dentures. Int. J. Oral Maxillofac. Implant. 2021, 36, 55–58. [Google Scholar] [CrossRef]
- Øilo, M.; Arola, D. Fractographic Analyses of Failed One-Piece Zirconia Implant Restorations. Dent. Mater. 2018, 34, 922–931. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Factors Influencing the Fracture of Dental Implants. Clin. Implant Dent. Relat. Res. 2018, 20, 58–67. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Mekki, M.; Crottaz, C.; Gahlert, M.; Romelli, E.; Marger, L.; Durual, S.; Vittecoq, E. Translational Research on Clinically Failed Zirconia Implants. Dent. Mater. 2019, 35, 368–388. [Google Scholar] [CrossRef]
- Sanon, C.; Chevalier, J.; Douillard, T.; Cattani-Lorente, M.; Scherrer, S.S.; Gremillard, L. A New Testing Protocol for Zirconia Dental Implants. Dent. Mater. 2015, 31, 15–25. [Google Scholar] [CrossRef]
- Rohr, N.; Bergemann, C.; Nebe, B.J.; Fischer, J. Crystal Structure of Zirconia Affects Osteoblast Behavior. Dent. Mater. 2020, 36, 905–913. [Google Scholar] [CrossRef]
- Spies, B.C.; Zhang, F.; Wesemann, C.; Li, M.; Rosentritt, M. Reliability and Aging Behavior of Three Different Zirconia Grades Used for Monolithic Four-Unit Fixed Dental Prostheses. Dent. Mater. 2020, 36, e329–e339. [Google Scholar] [CrossRef]
- Fontijn-Tekamp, F.A.; Slagter, A.P.; Van Der Bilt, A.; Van’T Hof, M.A.; Witter, D.J.; Kalk, W.; Jansen, J.A. Biting and Chewing in Overdentures, Full Dentures, and Natural Dentitions. J. Dent. Res. 2000, 79, 1519–1524. [Google Scholar] [CrossRef]
- Laurell, L.; Lundgren, D. Influence of Occlusion on Posterior Cantilevers. J. Prosthet. Dent. 1992, 67, 645–652. [Google Scholar] [CrossRef]
- Shinogaya, T.; Bakke, M.; Thomsen, C.E.; Vilmann, A.; Matsumoto, M. Bite Force and Occlusal Load in Healthy Young Subjects—A Methodological Study. Eur. J. Prosthodont. Restor. Dent. 2000, 8, 11–15. [Google Scholar]


| Material | ZP | ZM | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Connector size (mm2) | 9 | 12 | 9 | 12 | 9 | |||||
| Disk position | E | D | E | D | E | D | E | D | E * | D * |
| 1 | 744 | 981 | 1036 | 480 | 754 | 957 | 513 | 617 | 320 | 397 |
| 2 | 1008 | 997 | 584 | 576 | 772 | 927 | 723 | 759 | 331 | 388 |
| 3 | 1087 | 1303 | 639 | 561 | 820 | 1058 | 804 | 599 | 601 | 479 |
| 4 | 1005 | 927 | 839 | 606 | 882 | 784 | 525 | 509 | 523 | 460 |
| 5 | 1020 | 1186 | 550 | 717 | 881 | 1037 | 751 | 500 | 452 | 494 |
| 6 | 1000 | 1127 | 504 | 648 | 816 | 766 | 706 | 565 | 419 | 492 |
| mean | 977 | 1087 | 692 | 598 | 821 | 921 | 670 | 592 | 441 | 452 |
| sd | 119 | 144 | 205 | 81 | 53 | 124 | 122 | 95 | 109 | 47 |
| Fracture types | Type 1 | Type 2 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rohr, N.; Nüesch, R.; Greune, R.; Mainetti, G.; Karlin, S.; Zaugg, L.K.; Zitzmann, N.U. Stability of Cantilever Fixed Dental Prostheses on Zirconia Implants. Materials 2022, 15, 3633. https://doi.org/10.3390/ma15103633
Rohr N, Nüesch R, Greune R, Mainetti G, Karlin S, Zaugg LK, Zitzmann NU. Stability of Cantilever Fixed Dental Prostheses on Zirconia Implants. Materials. 2022; 15(10):3633. https://doi.org/10.3390/ma15103633
Chicago/Turabian StyleRohr, Nadja, Reto Nüesch, Rebecca Greune, Gino Mainetti, Sabrina Karlin, Lucia K. Zaugg, and Nicola U. Zitzmann. 2022. "Stability of Cantilever Fixed Dental Prostheses on Zirconia Implants" Materials 15, no. 10: 3633. https://doi.org/10.3390/ma15103633
APA StyleRohr, N., Nüesch, R., Greune, R., Mainetti, G., Karlin, S., Zaugg, L. K., & Zitzmann, N. U. (2022). Stability of Cantilever Fixed Dental Prostheses on Zirconia Implants. Materials, 15(10), 3633. https://doi.org/10.3390/ma15103633






