Impact of Ceramic Material and Preparation Design on Marginal Fit of Endocrown Restorations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Natural Teeth Collection
2.2. Sample Grouping
- The two tested groups are:
- -
- CD; Celtra Duo.
- -
- VE; Vita Enamic.
- The two tested sub-groups are:
- -
- CD-W; Celtra Duo with 3 mm intraradicular extension.
- -
- CD-WO; Celtra Duo without intraradicular extension.
- -
- VE-W; Vita Enamic with 3 mm intraradicular extension.
- -
- VE-WO; Vita Enamic without intraradicular extension.
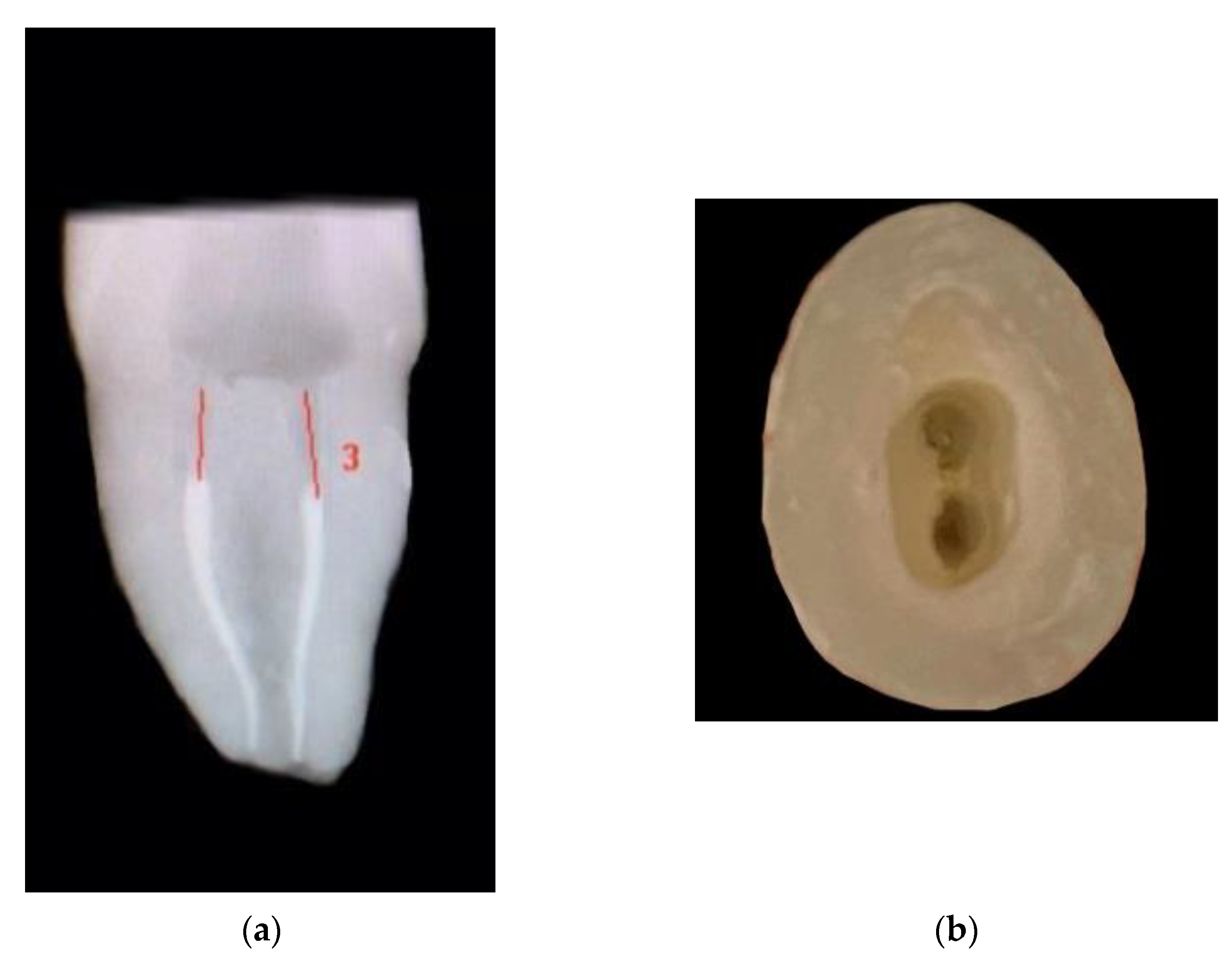
2.3. Coronal Preparation
2.4. Endodontic Treatment of All Teeth
2.5. Intraradicular Preparation
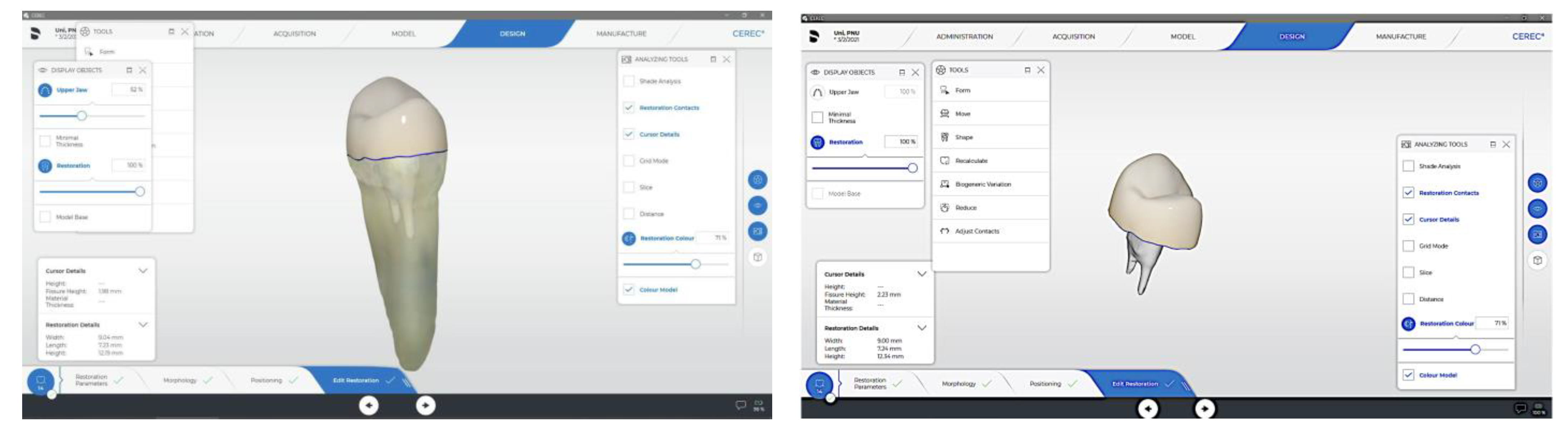
2.6. CAD/CAM Fabrication of Endocrown Restoration
2.7. Marginal Gap Testing
2.8. Statistical Analysis
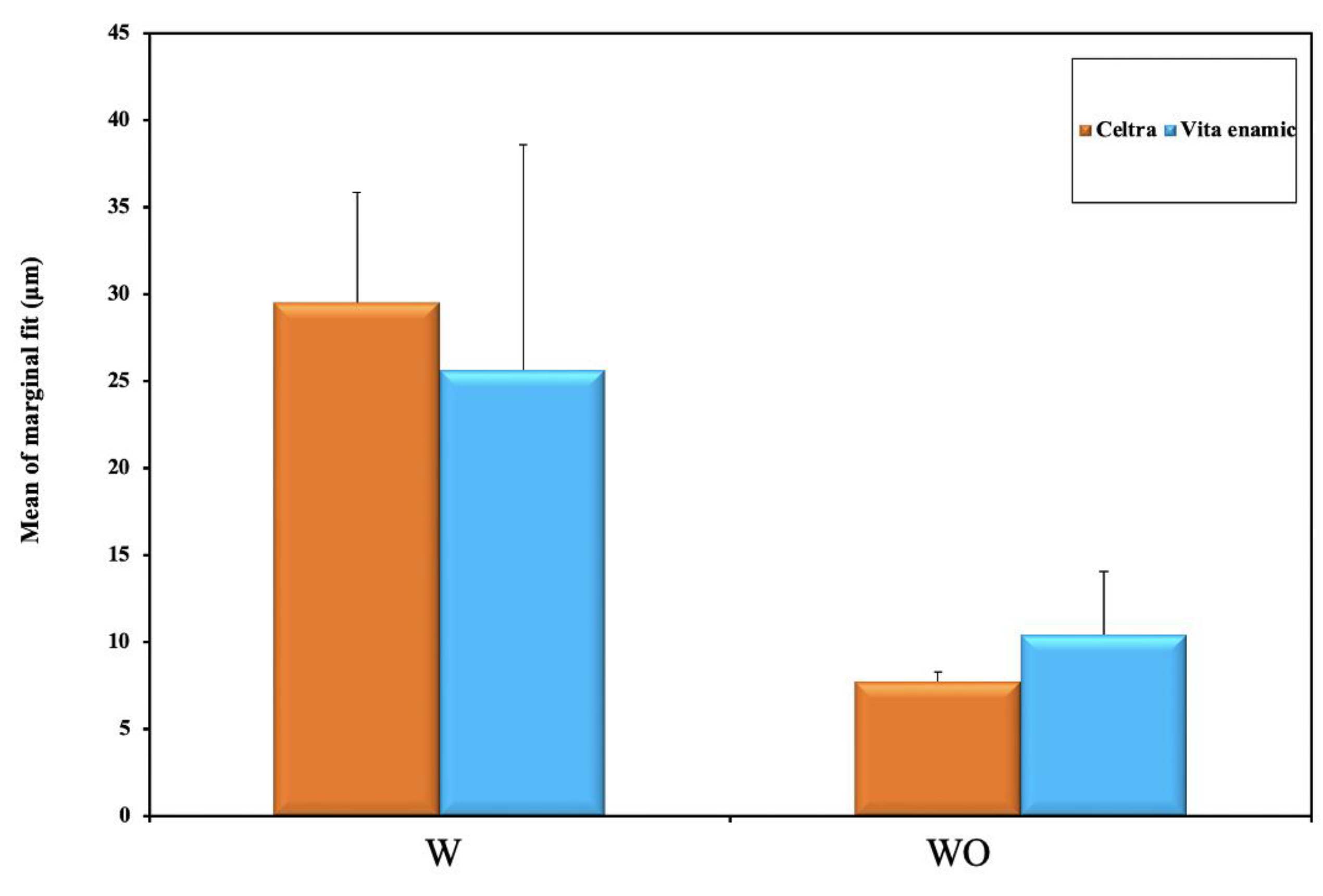
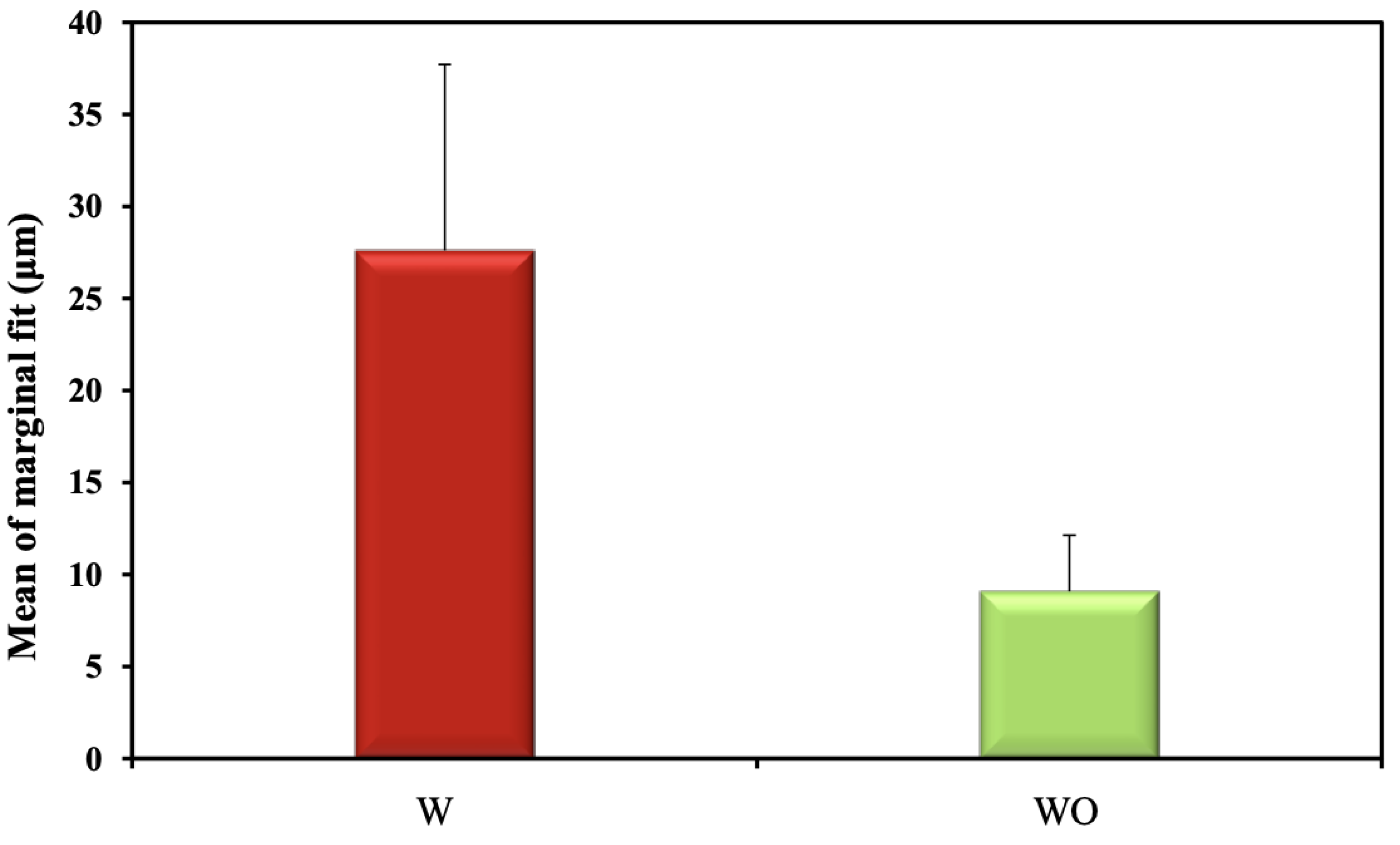
3. Results
4. Discussion
5. Conclusions
- Both tested materials and preparation designs recorded marginal gap values that are within clinically accepted values.
- CAD/CAM material selection may influence the fitting accuracy of CAD/CAM-fabricated restorations, as resin-based hybrid ceramic material recorded least marginal gab when compared to zirconia-reinforced lithium silicate.
- Intraradicular extension for endocrown restorations adversely affects marginal fit, however, the marginal gap is still within a clinically accepted range.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kanat-Ertürk, B.; Saridağ, S.; Köseler, E.; Helvacioğlu-Yiğit, D.; Avcu, E.; Yildiran-Avcu, Y. Fracture strengths of endocrown restorations fabricated with different preparation depths and CAD/CAM materials. Dent. Mater. J. 2018, 37, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Ghajghouj, O.; Taşar-Faruk, S. Evaluation of Fracture Resistance and Microleakage of Endocrowns with Different Intracoronal Depths and Restorative Materials Luted with Various Resin Cements. Materials 2019, 12, 2528. [Google Scholar] [CrossRef] [PubMed]
- Adel, S.; Abo-madina, M.M.; Farag, S.A.A. Fracture Strength of Hybrid Ceramic Endocrown Restoration with Different Preparation Depths and Designs. IOSR J. Dent. Med. Sci. 2019, 18, 17–23. [Google Scholar]
- Sevimli, G.; Cengiz, S.; Oruç, M.S. Endocrowns: Review. J. Istanb. Univ. Fac. Dent. 2015, 49, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Gaintantzopoulou, M.D.; El-Damanhoury, H.M. Effect of Preparation Depth on the Marginal and Internal Adaptation of Computer-aided Design/Computer-assisted Manufacture Endocrowns. Oper. Dent. 2016, 41, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Elalem, I.A.; Ibraheem, R.M.; Hamdy, A.M. Scient Open Access Clinical Evaluation of The Marginal Integrity, and Internal Fit of E-Max Endocrown Restorations with Different Marginal Preparation Designs. J. Dent. Oral Health 2019, 5, 1–7. [Google Scholar]
- Elrashid, A.H.; AlKahtani, A.H.; Alqahtani, S.J.; Alajmi, N.B.; Alsultan, F.H. Stereomicroscopic evaluation of marginal fit of E. Max press and E. Max computer-aided design and computer-assisted manufacturing lithium disilicate ceramic crowns: An in vitro study. J. Int. Soc. Prev. Community Dent. 2019, 9, 178. [Google Scholar] [PubMed]
- Alshalan, A.; Almutair, A.; Awad, D.; Alshmlani, M.; Abbas SBin Asif, Z. International Journal of Dentistry and Oral Health Marginal and Internal Fit of CAD CAM System. Explor. Sci. Community 2019, 5, 39–47. [Google Scholar]
- Vág, J.; Nagy, Z.; Bocklet, C.; Kiss, T.; Nagy, Á.; Simon, B.; Mikolicz, Á.; Renne, W. Marginal and internal fit of full ceramic crowns milled using CADCAM systems on cadaver full arch scans. BMC Oral Health 2020, 20, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.L.; Chang, Y.H.; Hsieh, S.K.; Chang, W.J. Estimation of the failure risk of a maxillary premolar with different crack depths with endodontic treatment by computer-aided design/computer-aided manufacturing ceramic restorations. J. Endod. 2013, 39, 375–379. [Google Scholar] [CrossRef]
- Shin, Y.; Park, S.; Park, J.W.; Kim, K.M.; Park, Y.B.; Roh, B.D. Evaluation of the marginal and internal discrepancies of CAD-CAM endocrowns with different cavity depths: An in vitro study. J. Prosthet. Dent. 2017, 117, 109–115. [Google Scholar] [CrossRef]
- Zimmermann, M.; Valcanaia, A.; Neiva, G.; Mehl, A.; Fasbinder, D. Three-Dimensional Digital Evaluation of the Fit of Endocrowns Fabricated from Different CAD/CAM Materials. J. Prosthodont. 2019, 18, e504–e509. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Hauschild, U.; Veronesi, G.; Imburgia, M.; Mangano, C.; Admakin, O. Trueness and precision of 5 intraoral scanners in the impressions of single and multiple implants: A comparative in vitro study. BMC Oral Health 2019, 19, 101. [Google Scholar] [CrossRef] [PubMed]
- Ender, A.; Zimmermann, M.; Mehl, A. Accuracy of complete- and partial-arch impressions of actual intraoral scanning systems in vitro. Int. J. Comput. Dent. 2019, 22, 11–19. [Google Scholar] [PubMed]
- Chen, Y.; Zhai, Z.; Li, H.; Yamada, S.; Matsuoka, T.; Ono, S.; Nakano, T. Influence of liquid on the tooth surface on the accuracy of intraoral scanners: An in vitro study. J. Prosthodont. 2021, 31, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Erozan, Ç.; Ozan, O. Evaluation of the precision of different intraoral scanner-Computer Aided Design (CAD) software combinations in digital dentistry. Med. Sci. Monit. 2020, 26, e918529. [Google Scholar] [CrossRef] [PubMed]
- Oh, K.C.; Park, J.; Moon, H.S. Effects of scanning strategy and scanner type on the accuracy of intraoral scans: A new approach for assessing the accuracy of scanned data. J. Prosthodont. 2020, 29, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Lee, K.B. Effect of finish line locations of tooth preparation on the accuracy of intraoral scanners. Int. J. Comput. Dent. 2021, 24, 29–40. [Google Scholar] [PubMed]
- Park, J.M. Comparative analysis on reproducibility among 5 intraoral scanners: Sectional analysis according to restoration type and preparation outline form. J. Adv. Prosthodont. 2016, 8, 354–362. [Google Scholar] [CrossRef]
- Roberto, R.; Assr, H.; Soars-Porto, T.; Lang, L.; Teach, S. Are different generations of CAD/CAM milling machines capable to produce restorations with similar quality? J. Clin. Exp. Dent. 2016, 8, e423–e428. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, C.; Ender, A.; Attin, T.; Mehl, A. Truness of four different milling procedures used in dental CAD/CAM systems. Clin. Oral Investig. 2017, 21, 551–558. [Google Scholar] [CrossRef]
- Bosch, G.; Ender, A.; Mehl, A. A 3-dimensional accuracy analysis of chairside CAD/CAM milling processes. J. Prosthet. Dent. 2014, 112, 1425–1431. [Google Scholar] [CrossRef]
- §Haralur, S.B.; Alamrey, A.A.; Alshehri, S.A.; Alzahrani, D.S.; Alfarsi, M. Effect of different preparation designs and all ceramic materials on fracture strength of molar endocrowns. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020947329. [Google Scholar] [CrossRef]
- Irmaleny, Z.; Ardjanggi, S.; Mardiyah, A.A.; Wahjuningrum, D.A. Endocrown restoration on postendodontics treatment on lower first molar. J. Int. Soc. Prev. Community Dent. 2019, 9, 303. [Google Scholar]
- Taha, D.; Spintzyk, S.; Sabet, A.; Wahsh, M.; Salah, T. Assessment of marginal adaptation and fracture resistance of endocrown restorations utilizing different machinable blocks subjected to thermomechanical aging. J. Esthet. Restor. Dent. 2018, 30, 319–328. [Google Scholar] [CrossRef]
- Facenda, J.C.; Borba, M.; Corazza, P.H. A literature review on the new polymer-infiltrated ceramic-network material (PICN). J. Esthet. Restor. Dent. 2018, 30, 281–286. [Google Scholar] [CrossRef]
- Rinke, S.; Pabel, A.K.; Rödiger, M.; Ziebolz, D. Chairside fabrication of an all-ceramic partial crown using a zirconia-reinforced lithium silicate ceramic. Case Rep. Dent. 2016, 2016, 1354186. [Google Scholar] [CrossRef]
- Denry, J.; Kelly, J. Emerging ceramic-based materials for dentistry. J. Dent. Res. 2014, 93, 1235–1242. [Google Scholar] [CrossRef]
- Kruger, S.; Deubener, J.; Ritzberger, C.; Holand, W. Nucleation kinetics of lithium metasilicate in ZrO2-bearing lithium disilicate glasses for dental application. Int. J. Appl. Sci. 2013, 4, 9–19. [Google Scholar] [CrossRef]
- Preis, V.; Behr, M.; Hahnel, S.; Rosentritt, M. Influence of cementation on in vitro performance, marginal adaptation and fracture resistance of CAD/ CAM-fabricated ZLS molar crowns. Dent. Mater. 2015, 31, 1363–1369. [Google Scholar] [CrossRef]
- Mainjot, A. Recent advances in composite CAD/CAM blocks. Int. J. Esthet. Dent. 2016, 11, 275–280. [Google Scholar]
- Nguyen, J.F.; Migonney, V.; Ruse, N.D.; Sadoun, M. Resin composite blocks via high-pressure high-temperature polymerization. Dent. Mater. 2012, 28, 529–534. [Google Scholar] [CrossRef]
- El Zhawi, H.; Kaizer, M.R.; Chughtai, A.; Moraes, R.R.; Zhang, Y. Polymer infiltrated ceramic network structures for resistance to fatigue fracture and wear. Dent. Mater. 2016, 32, 1352–1361. [Google Scholar] [CrossRef]
- Fassbinder, D.J. Material Matters: A Review of Chairside CAD/CAM Restorative Maretials. J. Cosmet. Dent. 2018, 34, 64–74. [Google Scholar]
- Spitznagel, F.A.; Scholz, K.J.; Strub, J.R.; Vach, K.; Gierthmuehlen, P.C. Polymer-infiltrated ceramic CAD/CAM inlays and partial coverage restorations: 3-year results of a prospective clinical study over 5 years. Clin. Oral Investig. 2018, 22, 1973–1983. [Google Scholar] [CrossRef]
- He, L.H.; Swain, M. A novel polymer infiltrated ceramic dental material. Dent. Mater. 2011, 27, 527–534. [Google Scholar] [CrossRef]
- AL-Zomur, S.; Abo-Madina, M.; Hassouna, M. Influence of Different Marginal Preparation Designs and Materials on the Marginal Integrity and Internal Adaptation of Endocrown Restorations. Egypt. Dent. J. 2021, 67, 3491–3500. [Google Scholar] [CrossRef]
- Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, e275–e283. [Google Scholar] [CrossRef]
- Ng, J.; Ruse, D.; Wyatt, C. A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J. Prosthet. Dent. 2014, 112, 555–560. [Google Scholar] [CrossRef]
- Chang, C.-Y.; Kuo, J.-S.; Lin, Y.-S.; Chang, Y.-H. Fracture resistance and failure modes of CEREC endo-crowns and conventional post and core-supported CEREC crowns. J. Dent. Sci. 2009, 4, 110–117. [Google Scholar] [CrossRef]
- Ajay, M.V.; Verma, S. Comparison of Marginal Fit of Zirconia Copyings Milled with 4-Axis and 5-Axis Milling Machines. IJSRD —Int. J. Sci. Res. Dev. 2017, 4, 89–92. [Google Scholar]
- Hasanzade, M.; Sahebi, M.; Zarrati, S.; Payaminia, L.; Alikhasi, M. Comparative evaluation of the internal and marginal adaptations of CAD/CAM endocrowns and crowns fabricated from three different materials. Int. J. Prosthodont. 2020, 34, 341–347. [Google Scholar] [CrossRef]
- Habib, S.R. Digital microscopic evaluation of vertical marginal discrepancies of CAD/CAM fabricated zirconia cores. Biomed. Eng. /Biomed. Technik. 2019, 64, 207–214. [Google Scholar] [CrossRef]
- Wolfart, S.; Wegner, S.M.; Al-Halabi, A.; Kern, M. Clinical evaluation of marginal fit of a new experimental all-ceramic system before and after cementation. Int. J. Prosthodont. 2003, 16, 587–592. [Google Scholar]
- Cho, L.; Choi, J.; Yi, Y.J.; Park, C.J. Effect of finish line variants on marginal accuracy and fracture strength of ceramic optimized polymer/fiber-reinforced composite crowns. J. Prosthet. Dent. 2004, 91, 554–560. [Google Scholar] [CrossRef]
- El Ghoul, W.A.; Özcan, M.; Ounsi, H.; Tohme, H.; Salameh, Z. Effect of different CAD-CAM materials on the marginal and internal adaptation of endocrown restorations: An in vitro study. J. Prosthet. Dent. 2020, 123, 128–134. [Google Scholar] [CrossRef]
- Zahnfabrik, V.I.T.A. VITA ENAMIC® Technical and Scientific Documentation; VITA Zahnfabrik: Bad Sackingen, Germany, 2019. [Google Scholar]
- Mormann, W.H.; Stawarczyk, B.; Ender, A.; Sener, B.; Attin, T.; Mehl, A. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: Two-body wear, gloss retention, roughness and Martens hardness. J. Mech. Behav. Biomed. Mater. 2013, 20, 113–125. [Google Scholar] [CrossRef]
- Sağlam, G.; Cengiz, S.; Karacaer, Ö. Marginal adaptation and fracture resistance of feldspathic and polymer-infiltrated ceramic network CAD/CAM endocrowns for maxillary premolars. Niger J. Clin. 2020, 23, 1–6. [Google Scholar]
- Ewadh, A.M.; Jasim, H.H. The influence of different CAD/CAM materials on the marginal fit of endocrown with different cavity depths (A comparative in-vitro study). Mater. Today Proc. 2021, 61, 695–699. [Google Scholar] [CrossRef]
- Gurpinar, B.; Tak, O. Effect of pulp chamber depth on the accuracy of endocrown scans made with different intraoral scanners versus an industrial scanner: An in vitro study. J. Prosthet. Dent. 2020, 127, 430–437. [Google Scholar] [CrossRef]
- Lee, J.H.; Son, K.; Lee, K.B. Marginal and internal fit of ceramic restorations fabricated using digital scanning and conventional impressions: A clinical study. J. Clin. Med. 2020, 9, 4035. [Google Scholar] [CrossRef] [PubMed]





| Material | Manufacturer | Ceramic Type | Chemical Composition |
|---|---|---|---|
| Celtra Duo | Dentsply, United States | zirconia-reinforced lithium silicate ceramic | SiO2, P2O5, Al2O3, Li2O, ZnO, 10% ZrO2 |
| Vita ENAMIC | VITA-Zahnfabrik, Germany | polymer infiltrated ceramic | Polymer-infiltrated-feldspatic ceramic-network material (UDMA, TEGDMA) with 86 wt% ceramic (SiO2, Al2O3, Na2O, K2O, B2O3, CaO, TiO2, coloring oxides) |
| Materials | Total Designs | ||
|---|---|---|---|
| Designs | Group C; Celtra Duo | Group E, Enamic | |
| W, with 3 mm extension | (n = 10) | (n = 10) | (n = 20) |
| Min.–Max. | 18.97–36.16 | 7.42–43.93 | 7.42–43.93 |
| Mean ± SD. | 29.54 ± 6.32 | 25.63 ± 12.96 | 27.59 ± 10.12 |
| WO; without extension | (n = 10) | (n = 10) | (n = 20) |
| Min.–Max. | 5.69–9.84 | 7.66–17.20 | 5.69–17.20 |
| Mean ± SD. | 7.74 ± 1.55 | 10.42 ± 3.63 | 9.08 ± 3.04 |
| Total Materials | (n = 20) | (n = 20) | (n = 40) |
| Min.–Max. | 5.69–36.16 | 7.42–43.93 | 5.69–43.93 |
| Mean ± SD. | 18.64 ± 12.05 | 18.03 ± 12.11 | 18.33 ± 11.93 |
| Source | Type III Sum of Squares | DF | Mean Square | F | p |
|---|---|---|---|---|---|
| Corrected Model | 3537.1 | 3 | 1179.0 | 21.100 | <0.001 * |
| Materials | 3.8 | 1 | 3.8 | 0.068 | 0.796 |
| Designs | 3424.8 | 1 | 3424.8 | 61.291 | <0.001 * |
| Materials * Designs | 108.5 | 1 | 108.5 | 1.942 | 0.172 |
| Error | 2011.6 | 36 | 55.9 | ||
| Corrected Total | 5548.7 | 39 |
| Materials | p | ||
|---|---|---|---|
| Celtra (n = 20) | Vita Enamic (n = 20) | ||
| Marginal fit | |||
| Mean ± SD. | 18.64 ± 12.05 | 18.03 ± 12.11 | 0.873 |
| Designs | p | ||
|---|---|---|---|
| W (n = 20) | WO (n = 20) | ||
| Marginal fit | |||
| Mean ± SD. | 27.59 ± 10.12 | 9.08 ± 3.04 | < 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soliman, M.; Alzahrani, G.; Alabdualataif, F.; Eldwakhly, E.; Alsamady, S.; Aldegheishem, A.; Abdelhafeez, M.M. Impact of Ceramic Material and Preparation Design on Marginal Fit of Endocrown Restorations. Materials 2022, 15, 5592. https://doi.org/10.3390/ma15165592
Soliman M, Alzahrani G, Alabdualataif F, Eldwakhly E, Alsamady S, Aldegheishem A, Abdelhafeez MM. Impact of Ceramic Material and Preparation Design on Marginal Fit of Endocrown Restorations. Materials. 2022; 15(16):5592. https://doi.org/10.3390/ma15165592
Chicago/Turabian StyleSoliman, Mai, Ghadeer Alzahrani, Foton Alabdualataif, Elzahraa Eldwakhly, Sahar Alsamady, Alhanoof Aldegheishem, and Manal M. Abdelhafeez. 2022. "Impact of Ceramic Material and Preparation Design on Marginal Fit of Endocrown Restorations" Materials 15, no. 16: 5592. https://doi.org/10.3390/ma15165592






