Polysaccharide-Based Membrane Biocompatibility Study of Anacardium occidentale L. and Polyvinyl Alcohol after Subcutaneous Implant in Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Facilities
2.2. CGP/PVA Membrane Production
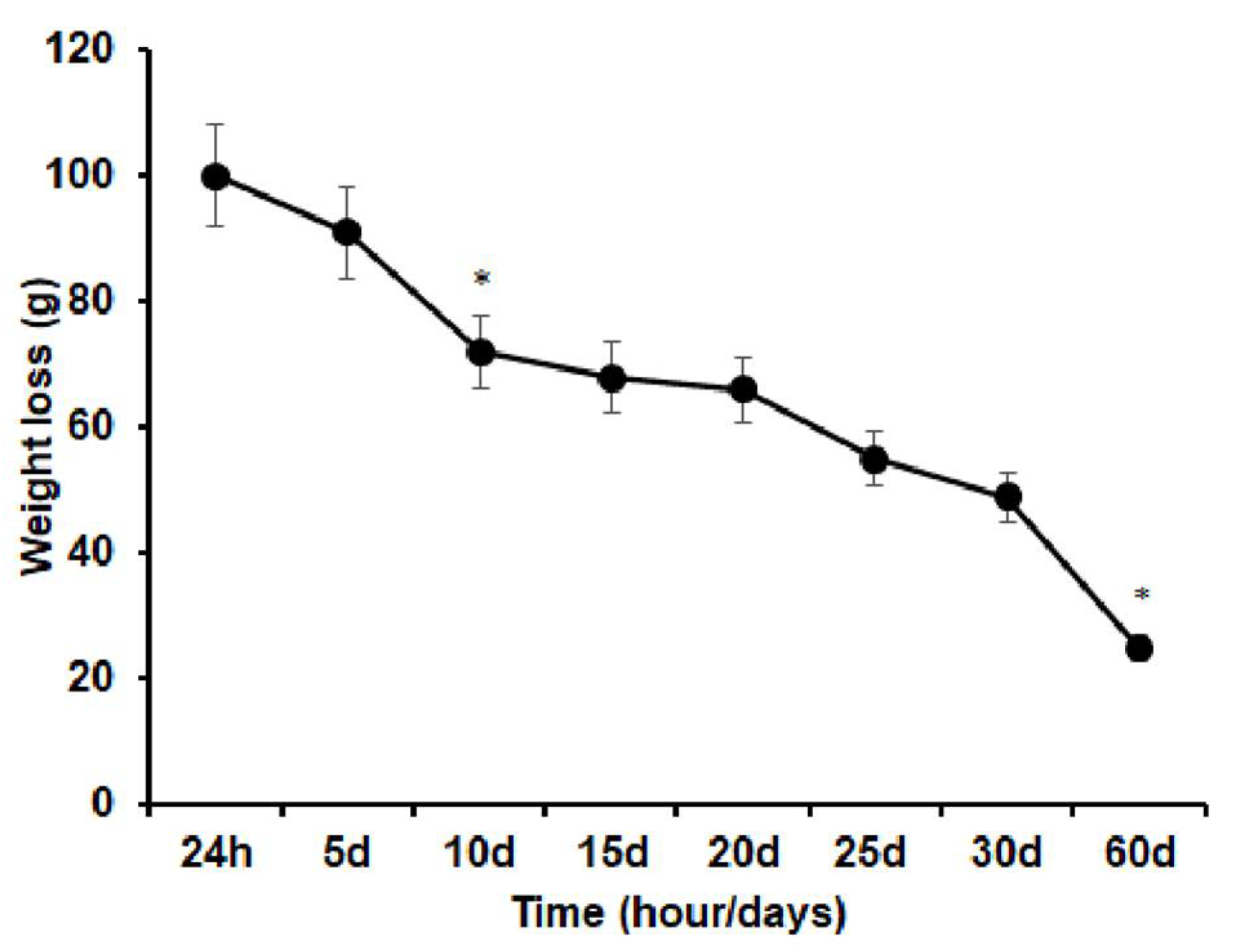
2.3. In Vitro Degradation Test
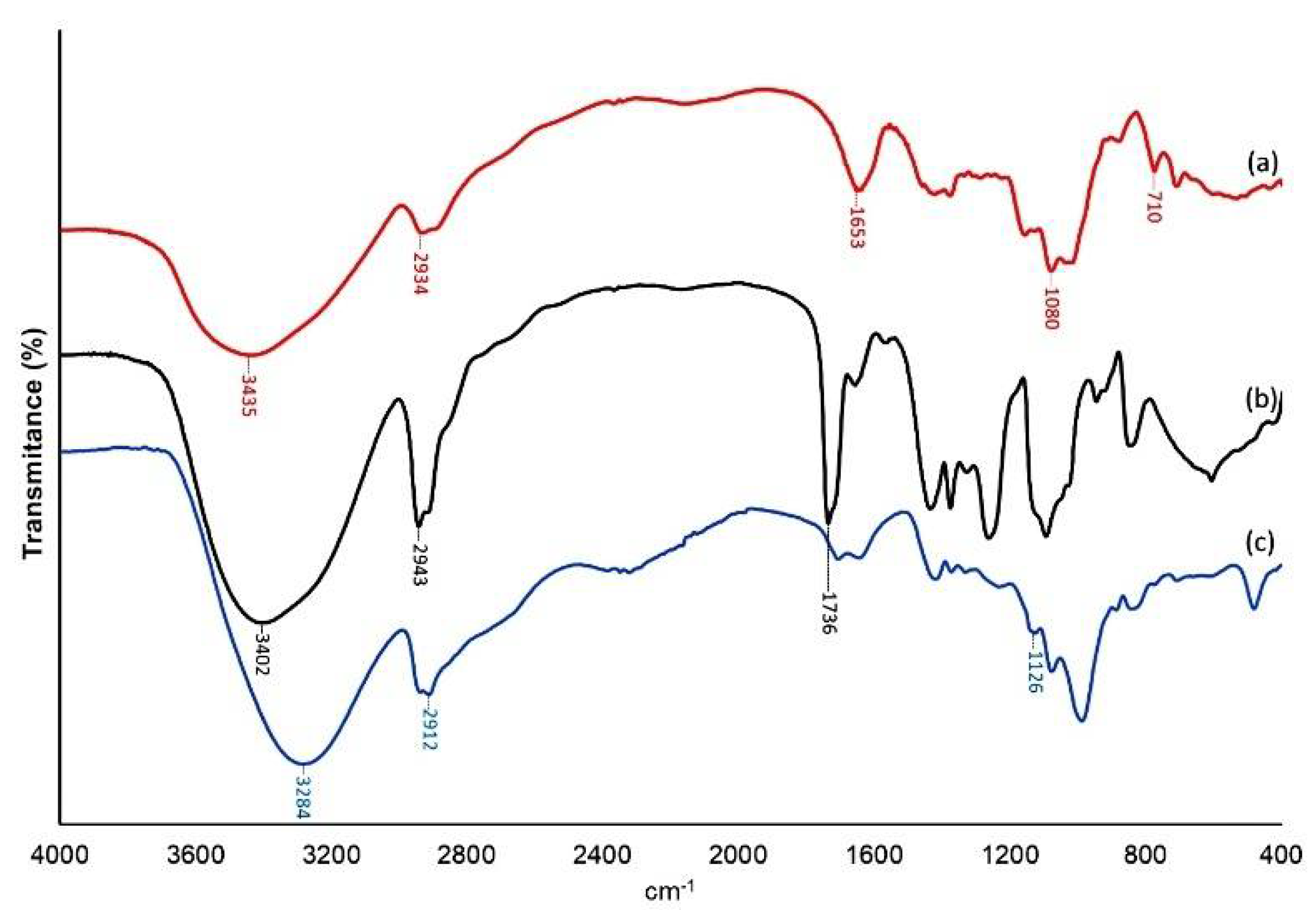
2.4. Fourier Transform Infrared (FTIR) Spectroscopy
2.5. Ethical Principles and Guideline Requirements
2.6. Experimental Design
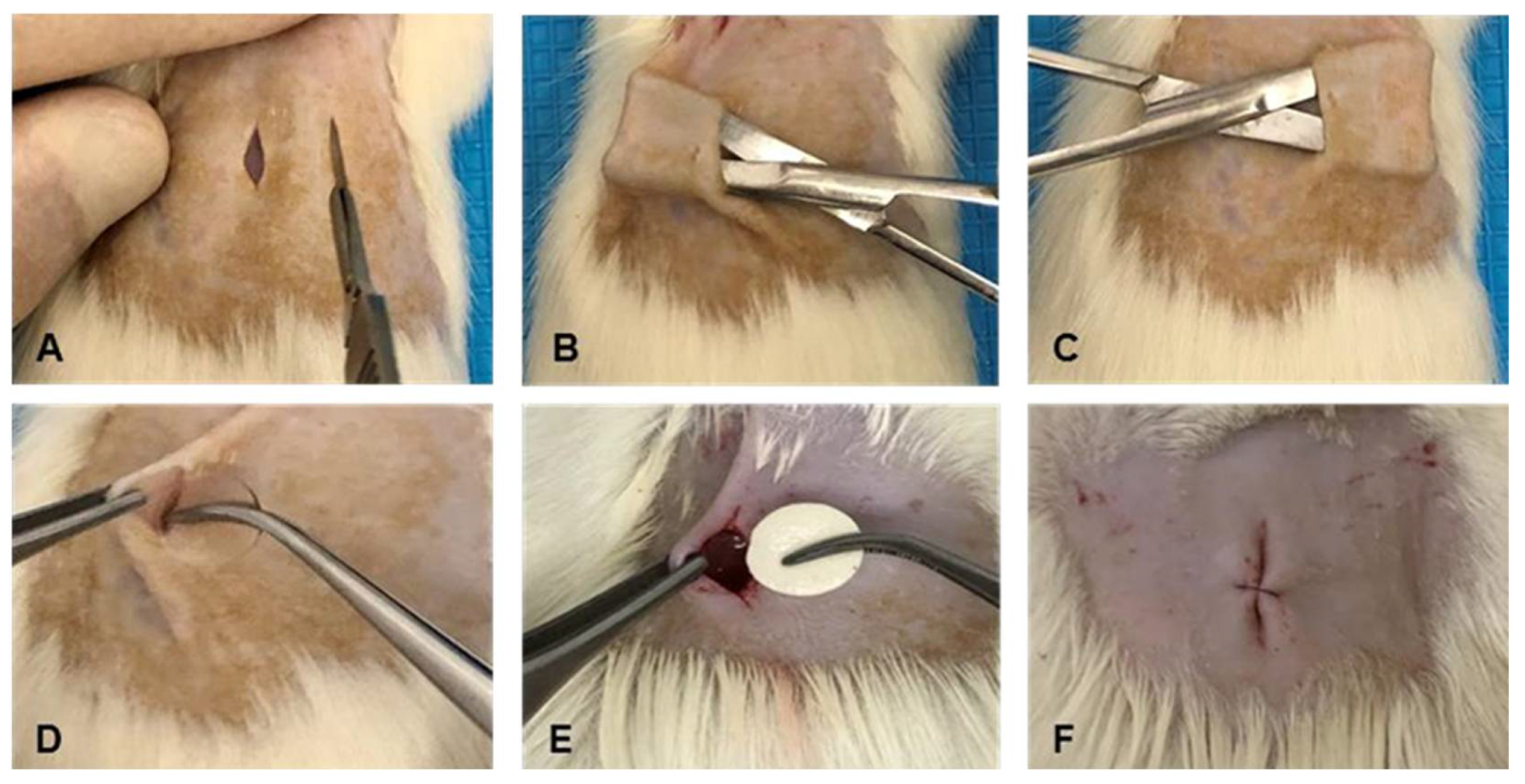
2.7. Surgical Procedure and Post-Operative Care
2.8. Sample Processing
2.9. Microscopic Descriptive Analysis
2.10. Evaluation of the Local Biological Effects of the Implantation
2.10.1. Semi-Quantitative Histological Analysis: ISO 10993-6:2016/Part6/Annex E
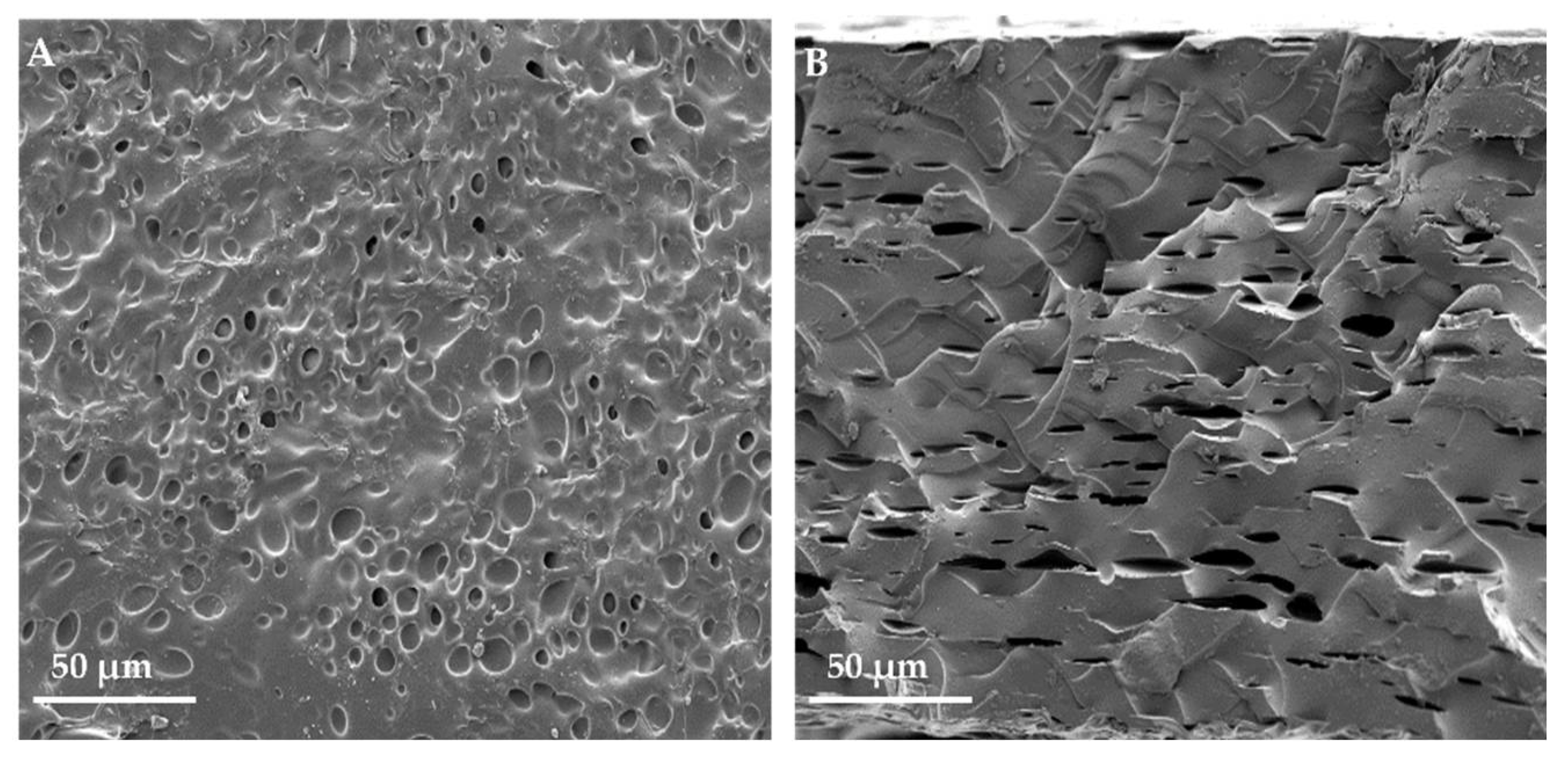
2.10.2. Scanning Electron Microscopy (SEM)
2.11. Statistical Analysis
3. Results
3.1. In Vitro Degradation Test
3.2. Fourier Transform Infrared (FTIR) Spectroscopy
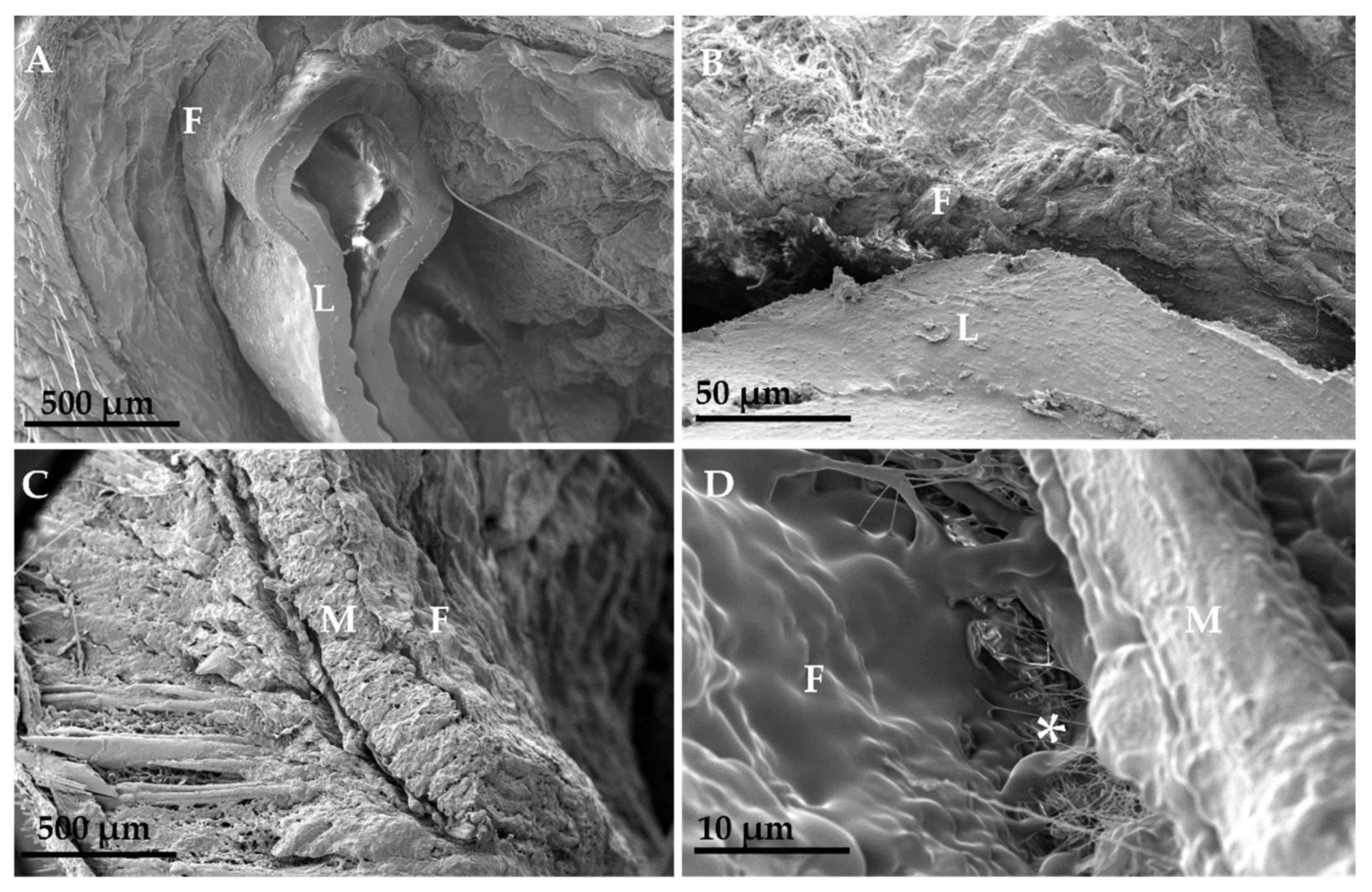
3.3. Scanning Electron Microscopy (SEM)
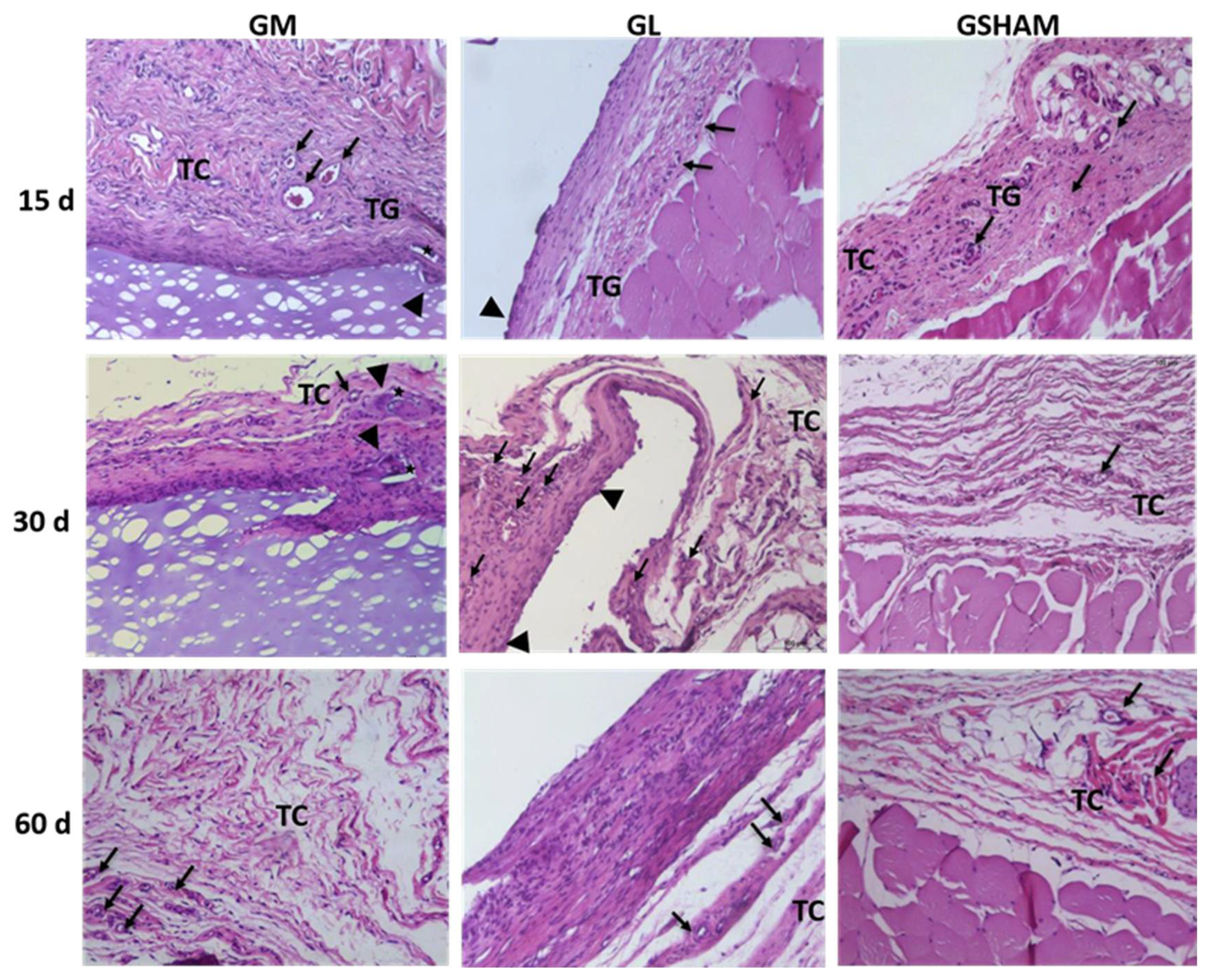
3.4. Descriptive Analysis of the In Vivo Test
3.5. Fibrous Capsule Evaluation
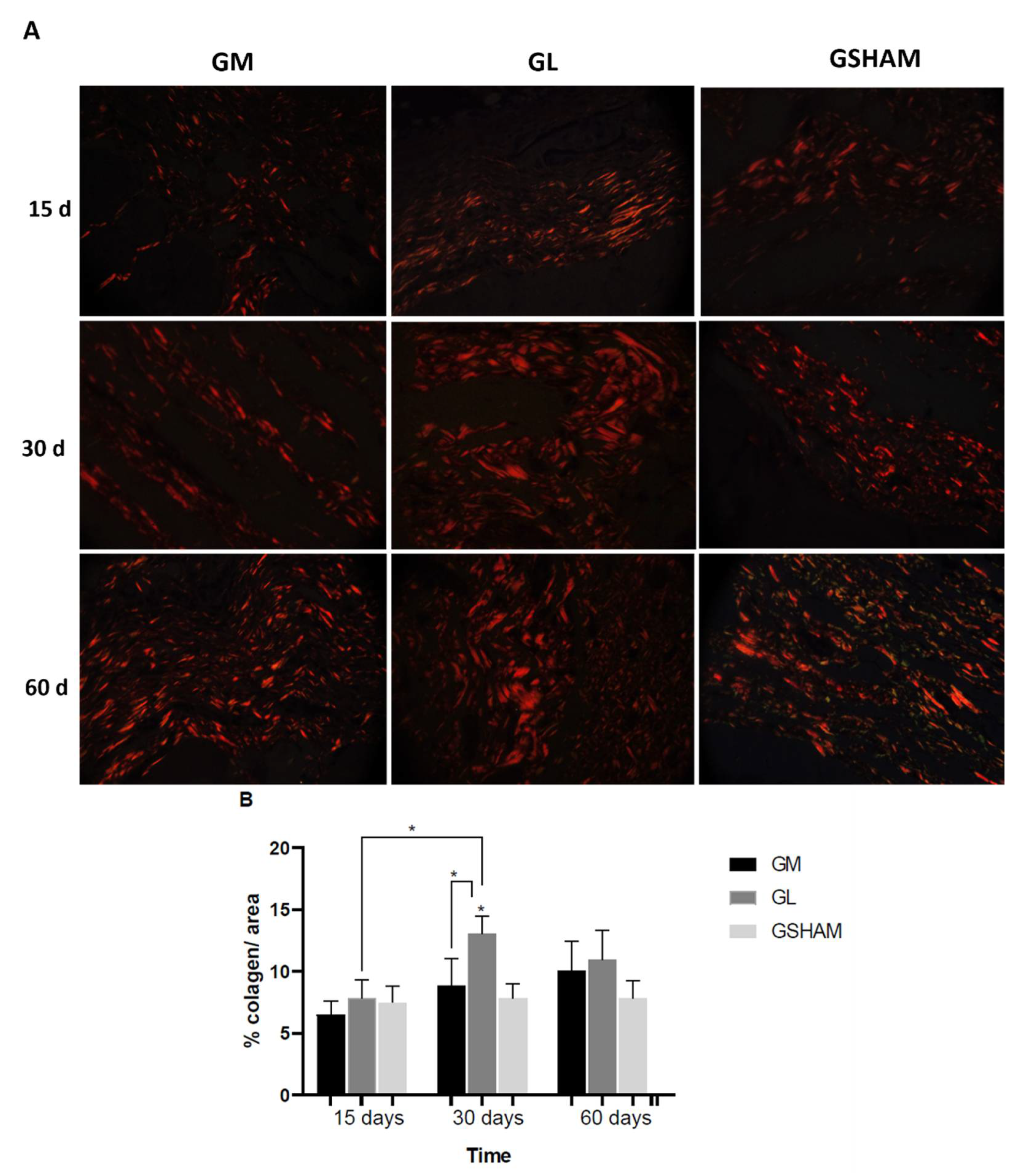
3.6. Collagen Assessment
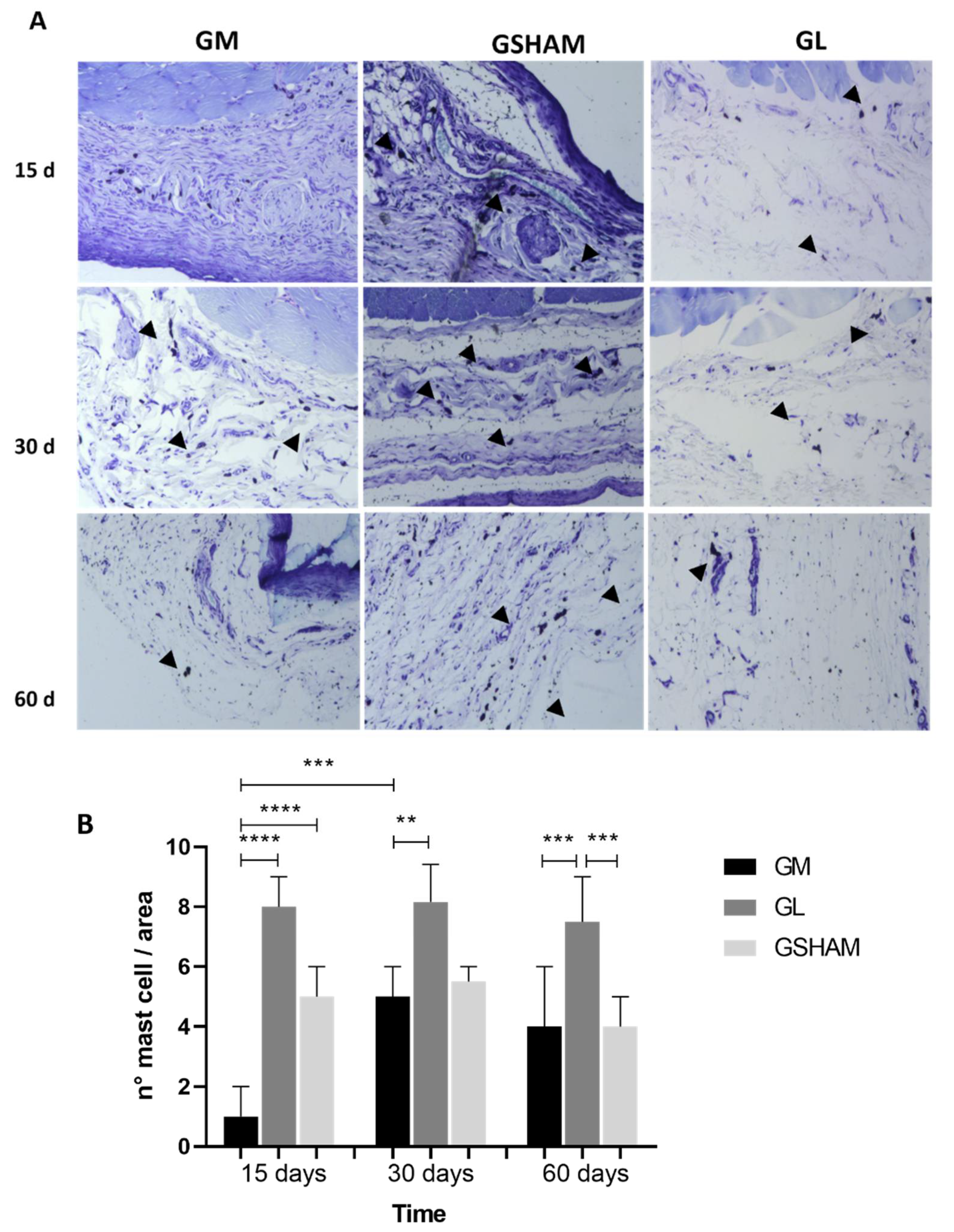
3.7. Quantification of Mast Cells
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bal, T.; Yadav, S.K.; Rai, N.; Swain, S.; Garg, S.; Sen, G. Invitro Evaluations of Free Radical Assisted Microwave Irradiated Polyacrylamide Grafted Cashew Gum (Cg) Biocompatible Graft Copolymer (CG-g-PAM) as Effective Polymeric Scaffold. J. Drug Deliv. Sci. Technol. 2020, 56, 101572. [Google Scholar] [CrossRef]
- Caversan, M.d.S.S. Desenvolvimento E Análise De Bandagem De Bioestimulaçãodentino/Pulpar (Bbio). Ph.D. Thesis, Universidade de São Paulo, Bauru, São Paulo, Brazil, 2018. [Google Scholar]
- Oliveira, N.N.; Mothé, C.G.; Mothé, M.G. Sustainable Uses of Cashew Tree Rejects: Cashew Apple Bagasse and Cashew Gum. Biomass Conv. Bioref. 2020. [Google Scholar] [CrossRef]
- De Paula, R.C.M.; Heatley, F.; Budd, P.M. Characterization of Anacardium Occidentale Exudate Polysaccharide. Polym. Int. 1998, 45, 27–35. [Google Scholar] [CrossRef]
- Animesh, K.; Afrasim, M.; Shruthi, R.; Ayaz, A.; Hosakote, G.S. Cashew Gum a Versatile Hydrophyllic Polymer: A Review. Available online: https://www.eurekaselect.com/96943/article (accessed on 18 June 2021).
- Torquato, D.S.; Ferreira, M.L.; Sá, G.C.; Brito, E.S.; Pinto, G.A.S.; Azevedo, E.H.F. Evaluation of Antimicrobial Activity of Cashew Tree Gum. World J. Microbiol. Biotechnol. 2004, 20, 505–507. [Google Scholar] [CrossRef]
- Da Silva, J.G.; Souza, I.A.; Higino, J.S.; Siqueira-Junior, J.P.; Pereira, J.V.; Pereira, M.d.S.V. Atividade Antimicrobiana Do Extrato de Anacardium Occidentale Linn. Em Amostras Multiresistentes de Staphylococcus Aureus. Rev. Bras. Farmacogn. 2007, 17, 572–577. [Google Scholar] [CrossRef]
- Campos, D.A.; Ribeiro, A.C.; Costa, E.M.; Fernandes, J.C.; Tavaria, F.K.; Araruna, F.B.; Eiras, C.; Eaton, P.; Leite, J.R.S.A.; Manuela Pintado, M. Study of Antimicrobial Activity and Atomic Force Microscopy Imaging of the Action Mechanism of Cashew Tree Gum. Carbohydr. Polym. 2012, 90, 270–274. [Google Scholar] [CrossRef]
- Schirato, G.V.; Monteiro, F.M.F.; Silva, F.d.; Lima Filho, J.L.d.; Leão, A.M.d.A.C.; Porto, A.L.F. O Polissacarídeo Do Anacardium Occidentale L. Na Fase Inflamatória Do Processo Cicatricial de Lesões Cutâneas. Cienc. Rural 2006, 36, 149–154. [Google Scholar] [CrossRef]
- Nicolau, L.A.D.; Batista-Lima, F.J.; Santana, A.P.M.; Sales, T.M.A.L.; Carmo-Neto, J.P.; Freitas, G.B.; Oliveira, T.M.; Medeiros, J.V.R.; Silva, D.A.; Lee, C.; et al. Cashew Gum, a Biopolymer, Topically Protects Oesophageal Mucosa in Non Erosive Reflux Disease: A Promising Translational Study. Carbohydr. Polym. 2019, 226, 115205. [Google Scholar] [CrossRef]
- Yamassaki, F.T.; Lenzi, R.M.; Campestrini, L.H.; Bovo, F.; Seyfried, M.; Soldera-Silva, A.; Stevan-Hancke, F.R.; Zawadzki-Baggio, S.F.; Pettolino, F.A.; Bacic, A.; et al. Effect of the Native Polysaccharide of Cashew-Nut Tree Gum Exudate on Murine Peritoneal Macrophage Modulatory Activities. Carbohydr. Polym. 2015, 125, 241–248. [Google Scholar] [CrossRef]
- Araújo, T.S.L.; Costa, D.S.; Sousa, N.A.; Souza, L.K.M.; de Araújo, S.; Oliveira, A.P.; Sousa, F.B.M.; Silva, D.A.; Barbosa, A.L.R.; Leite, J.R.S.A.; et al. Antidiarrheal Activity of Cashew GUM, a Complex Heteropolysaccharide Extracted from Exudate of Anacardium Occidentale L. in Rodents. J. Ethnopharmacol. 2015, 174, 299–307. [Google Scholar] [CrossRef]
- Carvalho, N.S.; Silva, M.M.; Silva, R.O.; Nicolau, L.A.D.; Sousa, F.B.M.; Damasceno, S.R.B.; Silva, D.A.; Barbosa, A.L.R.; Leite, J.R.S.A.; Medeiros, J.V.R. Gastroprotective Properties of Cashew Gum, a Complex Heteropolysaccharide of Anacardium Occidentale, in Naproxen-Induced Gastrointestinal Damage in Rats: Gastroprotective Effects of Cashew Gum. Drug Dev. Res. 2015, 76, 143–151. [Google Scholar] [CrossRef]
- Baracuhy, J.G.d.; Furtado, D.A.; Francisco, P.R.M.; Lima, J.L.S.d.; Pereira, J.P.G. Plantas Medicinais de uso Comum no Nordeste do Brasil; UFCG: Campina Grande, Brazil, 2016. [Google Scholar]
- Paula, H.C.B.; Rodrigues, M.L.L.; Ribeiro, W.L.C.; Stadler, A.S.; Paula, R.C.M.; Abreu, F.O.M.S. Protective Effect of Cashew Gum Nanoparticles on Natural Larvicide from Moringa Oleifera Seeds. J. Appl. Polym. Sci. 2012, 124, 1778–1784. [Google Scholar] [CrossRef]
- de Oliveira Silva Ribeiro, F.; de França Dourado, F.; Silva, M.F.S.; Brito, L.M.; Pessoa, C.; de Lima, L.R.M.; de Paula, R.C.M.; de Souza de Almeida Leite, J.R.; de Araújo, A.R.; da Silva, D.A. Anti-Proliferative Profile of Anacardium Occidentale Polysaccharide and Characterization by AFM. Int. J. Biol. Macromol. 2020, 156, 981–987. [Google Scholar] [CrossRef]
- da Silva, D.A.; de Paula, R.C.M.; Feitosa, J.P.A. GraftCopolymerisation of Acrylamide onto Cashew Gum. Eur. Polym. J. 2007, 43, 2620–2629. [Google Scholar] [CrossRef]
- Eskandarinia, A.; Kefayat, A.; Agheb, M.; Rafienia, M.; Amini Baghbadorani, M.; Navid, S.; Ebrahimpour, K.; Khodabakhshi, D.; Ghahremani, F. A Novel Bilayer Wound Dressing Composed of a Dense Polyurethane/Propolis Membrane and a Biodegradable Polycaprolactone/Gelatin Nanofibrous Scaffold. Sci. Rep. 2020, 10, 3063. [Google Scholar] [CrossRef]
- Kalirajan, C.; Hameed, P.; Subbiah, N.; Palanisamy, T. A Facile Approach to Fabricate Dual Purpose Hybrid Materials for Tissue Engineering and Water Remediation. Sci. Rep. 2019, 9, 1040. [Google Scholar] [CrossRef]
- Cruz, M.V.; Pereira-Júnior, M.A.; Batista, K.A.; Fernandes, K.F. Use of Statistical Design Strategies to Produce Biodegradable and Eco-Friendly Films from Cashew Gum Polysaccharide and Polyvinyl Alcohol. Materials 2019, 12, 1149. [Google Scholar] [CrossRef]
- Cruz, M.V.; Jacobowski, A.C.; Macedo, M.L.R.; Batista, K.A.; Fernandes, K.F. Immobilization of Antimicrobial Trypsin Inhibitors onto Cashew Gum Polysaccharide/PVA Films. Int. J. Biol. Macromol. 2019, 127, 433–439. [Google Scholar] [CrossRef]
- Pourbaix, M. Electrochemical Corrosion of Metallic Biomaterials. Biomaterials 1984, 5, 122–134. [Google Scholar] [CrossRef]
- Ding, S.-J. Biodegradation Behavior of Chitosan/Calcium Phosphate Composites. J. Non-Cryst. Solids 2007, 353, 2367–2373. [Google Scholar] [CrossRef]
- Kilkenny, C.; Browne, W.J.; Cuthill, I.C.; Emerson, M.; Altman, D.G. Improving Bioscience Research Reporting: The ARRIVE Guidelines for Reporting Animal Research. Osteoarthr. Cartil. 2012, 20, 256–260. [Google Scholar] [CrossRef]
- Smith, A.J.; Clutton, R.E.; Lilley, E.; Hansen, K.E.A.; Brattelid, T. Prepare: Guidelines for Planning Animal Research and Testing. Lab. Anim. 2018, 52, 135–141. [Google Scholar] [CrossRef]
- Subramanian, A.; Krishnan, U.M.; Sethuraman, S. In Vivo Biocompatibility of PLGA-Polyhexylthiophene Nanofiber Scaffolds in a Rat Model. BioMed Res. Int. 2013, 2013, 1–8. [Google Scholar] [CrossRef]
- ISO 10993-12; Biological evaluation of medical devices — Part 12: Sample preparation and reference materials. ISO: Geneva, Switzerland, 2021. Available online: https://www.iso.org/obp/ui/#iso:std:iso:10993:-12:ed-5:v1:en (accessed on 20 June 2021).
- Vulcani, V.A.S.; Franzo, V.S.; Rabelo, R.E.; Rabbers, A.S.; Assis, B.M.; D’Ávila, M.A.; Antoni, S.M.B. In Vivo Biocompatibility of Nanostructured Chitosan/Peo Membranes. Arq. Bras. Med. Vet. Zootec. 2015, 67, 1039–1044. [Google Scholar] [CrossRef][Green Version]
- Bock, N.; Pham, T.L.-B.; Nguyen, T.B.; Nguyen, T.B.; Tran, H.A.; Tran, P.A. Polydopamine Coating of Uncrosslinked Chitosan as an Acellular Scaffold for Full Thickness Skin Grafts. Carbohydr. Polym. 2020, 245, 116524. [Google Scholar] [CrossRef]
- Ibrahim, M.; Bond, J.; Medina, M.A.; Chen, L.; Quiles, C.; Kokosis, G.; Bashirov, L.; Klitzman, B.; Levinson, H. Characterization of the Foreign Body Response to Common Surgical Biomaterials in a Murine Model. Eur J. Plast Surg. 2017, 40, 383–392. [Google Scholar] [CrossRef]
- Kaur, M.; Singh, K. Review on Titanium and Titanium Based Alloys as Biomaterials for Orthopaedic Applications. Mater. Sci. Eng. C 2019, 102, 844–862. [Google Scholar] [CrossRef]
- Ratner, B.D. Biomaterials: Been There, Done That, and Evolving into the Future. Annu. Rev. Biomed. Eng. 2019, 21, 171–191. [Google Scholar] [CrossRef]
- ISO 10993-6:2016; Biological evaluation of medical devices — Part 6: Tests for local effects after implantation. ISO: Geneva, Switzerland, 2016. Available online: https://www.iso.org/cms/render/live/en/sites/isoorg/contents/data/standard/06/10/61089.html (accessed on 20 June 2021).
- Silva, B.D.S.; Ulhoa, C.J.; Batista, K.A.; di Medeiros, M.C.; Filho, R.R.d.; Yamashita, F.; Fernandes, K.F. Biodegradable and Bioactive CGP/PVA Film for Fungal Growth Inhibition. Carbohydr. Polym. 2012, 89, 964–970. [Google Scholar] [CrossRef]
- Vicentini, D.S.; Smania, A.; Laranjeira, M.C.M. Chitosan/Poly (Vinyl Alcohol) Films Containing ZnO Nanoparticles and Plasticizers. Mater. Sci. Eng. C 2010, 30, 503–508. [Google Scholar] [CrossRef]
- Zhang, Z.; Cui, H. Biodegradability and Biocompatibility Study of Poly(Chitosan-g-Lactic Acid) Scaffolds. Molecules 2012, 17, 3243–3258. [Google Scholar] [CrossRef] [PubMed]
- Al-Maawi, S.; Orlowska, A.; Sader, R.; James Kirkpatrick, C.; Ghanaati, S. In Vivo Cellular Reactions to Different Biomaterials—Physiological and Pathological Aspects and Their Consequences. Semin. Immunol. 2017, 29, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Korzinskas, T.; Jung, O.; Smeets, R.; Stojanovic, S.; Najman, S.; Glenske, K.; Hahn, M.; Wenisch, S.; Schnettler, R.; Barbeck, M. In Vivo Analysis of the Biocompatibility and Macrophage Response of a Non-Resorbable PTFE Membrane for Guided Bone Regeneration. IJMS 2018, 19, 2952. [Google Scholar] [CrossRef] [PubMed]
- Corradetti, B.; Taraballi, F.; Corbo, C.; Cabrera, F.; Pandolfi, L.; Minardi, S.; Wang, X.; van Eps, J.; Bauza, G.; Weiner, B.; et al. Immune Tuning Scaffold for the Local Induction of a Pro-Regenerative Environment. Sci. Rep. 2017, 7, 17030. [Google Scholar] [CrossRef]
- Jardelino, C.; Takamori, E.R.; Hermida, L.F.; Lenharo, A.; Castro-Silva, I.I.; Granjeiro, J.M. Porcine Peritoneum as Source of Biocompatible Collagen in Mice. Acta Cir. Bras. 2010, 25, 332–336. [Google Scholar] [CrossRef]
- Wang, J.; Hao, S.; Luo, T.; Cheng, Z.; Li, W.; Gao, F.; Guo, T.; Gong, Y.; Wang, B. Feather Keratin Hydrogel for Wound Repair: Preparation, Healing Effect and Biocompatibility Evaluation. Colloids Surf. B Biointerfaces 2017, 149, 341–350. [Google Scholar] [CrossRef]
- Childs, D.R.; Murthy, A.S. Overview of Wound Healing and Management. Surg. Clin. N. Am. 2017, 97, 189–207. [Google Scholar] [CrossRef]
- Paiva, Introdução à Espectroscopia. Available online: https://www.cengage.com.br/livro/introducao-a-espectroscopia/ (accessed on 13 January 2022).
- Pitombeira, N.A.O.; Veras Neto, J.G.; Silva, D.A.; Feitosa, J.P.A.; Paula, H.C.B.; de Paula, R.C.M. Self-Assembled Nanoparticles of Acetylated Cashew Gum: Characterization and Evaluation as Potential Drug Carrier. Carbohydr. Polym. 2015, 117, 610–615. [Google Scholar] [CrossRef]
- Lima, M.R.; Paula, H.C.B.; Abreu, F.O.M.S.; da Silva, R.B.C.; Sombra, F.M.; de Paula, R.C.M. Hydrophobization of Cashew Gum by Acetylation Mechanism and Amphotericin B Encapsulation. Int. J. Biol. Macromol. 2018, 108, 523–530. [Google Scholar] [CrossRef]
- Hassan, C.M.; Peppas, N.A. Structure and Applications of Poly(Vinyl Alcohol) Hydrogels Produced by Conventional Cross-linking or by Freezing/Thawing Methods. Biopolym. PVA Hydrogels Anionic Polym. Nanocomposites 2000, 153, 37–65. [Google Scholar]
- Peppas, N.A. Tear Propagation Resistance of Semicrystalline Polymeric Networks. Polymer 1977, 18, 403–407. [Google Scholar] [CrossRef]
- Reis, E.F.d.; Campos, F.S.; Lage, A.P.; Leite, R.C.; Heneine, L.G.; Vasconcelos, W.L.; Lobato, Z.I.P.; Mansur, H.S. Synthesis and Characterization of Poly (Vinyl Alcohol) Hydrogels and Hybrids for RMPB70 Protein Adsorption. Mat. Res. 2006, 9, 185–191. [Google Scholar] [CrossRef]
- Malathi, J.; Kumaravadivel, M.; Brahmanandhan, G.M.; Hema, M.; Baskaran, R.; Selvasekarapandian, S. Structural, Thermal and Electrical Properties of PVA–LiCF3SO3 Polymer Electrolyte. J. Non-Cryst. Solids 2010, 356, 2277–2281. [Google Scholar] [CrossRef]
- Coates, J. Interpretation of infrared spectra, a practical approach. In Encyclopedia of Analytical Chemistry; Meyers, R.A., Ed.; John Wiley & Sons Ltd.: Chichester, UK, 2000; pp. 10815–10837. [Google Scholar]
- Mansur, H.; Oréfice, R.; Pereira, M.; Lobato, Z.; Vasconcelos, W.; Machado, L. FTIR and UV-vis Study of Chemically Engineered Biomaterial Surfaces for Protein Immobilization. Spectroscopy 2002, 16, 351–360. [Google Scholar] [CrossRef]
- Vlachos, N.; Skopelitis, Y.; Psaroudaki, M.; Konstantinidou, V.; Chatzilazarou, A.; Tegou, E. Applications of Fourier Transform-Infrared Spectroscopy to Edible Oils. Anal. Chim. Acta 2006, 573, 459–465. [Google Scholar] [CrossRef]
- Zhou, G.; Groth, T. Host Responses to Biomaterials and Anti-Inflammatory Design-a Brief Review. Macromol. Biosci. 2018, 18, 1800112. [Google Scholar] [CrossRef]
- Gheno, E.; Mourão, C.F.d.B.; Mello-Machado, R.C.d.; Stellet Lourenço, E.; Miron, R.J.; Catarino, K.F.F.; Alves, A.T.; Alves, G.G.; Calasans-Maia, M.D. In Vivo Evaluation of the Biocompatibility and Biodegradation of a New Denatured Plasma Membrane Combined with Liquid PRF (Alb-PRF). Platelets 2020, 32, 542–554. [Google Scholar] [CrossRef]
- Klopfleisch, R.; Jung, F. The Pathology of the Foreign Body Reaction against Biomaterials: Foreign Body Reaction to Biomaterials. J. Biomed. Mater. Res. 2017, 105, 927–940. [Google Scholar] [CrossRef]
- Onuki, Y.; Bhardwaj, U.; Papadimitrakopoulos, F.; Burgess, D.J. A Review of the Biocompatibility of Implantable Devices: Current Challenges to Overcome Foreign Body Response. J. Diabetes Sci. Technol. 2008, 2, 1003–1015. [Google Scholar] [CrossRef]
- Luttikhuizen, D.T.; Dankers, P.Y.W.; Harmsen, M.C.; van Luyn, M.J.A. Material Dependent Differences in Inflammatory Gene Expression by Giant Cells during the Foreign Body Reaction. J. Biomed. Mater. Res. 2007, 83A, 879–886. [Google Scholar] [CrossRef]
- Kastellorizios, M.; Papadimitrakopoulos, F.; Burgess, D.J. Prevention of Foreign Body Reaction in a Pre-Clinical Large Animal Model. J. Control. Release 2015, 202, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.M.; McNally, A.K. Biocompatibility of Implants: Lymphocyte/Macrophage Interactions. Semin. Immunopathol. 2011, 33, 221–233. [Google Scholar] [CrossRef]
- Rizik, D.G.; Hermiller, J.B.; Kereiakes, D.J. The ABSORB Bioresorbable Vascular Scaffold: A Novel, Fully Resorbable Drug-Eluting Stent: Current Concepts and Overview of Clinical Evidence: ABSORB Bioresorbable Vascular Scaffold. Cathet. Cardiovasc. Intervent. 2015, 86, 664–677. [Google Scholar] [CrossRef] [PubMed]
- Bancroft, J.D. Theory and Practice of Histological Techniques; Elsevier Health Sciences: Amsterdam, The Netherlands, 2008; ISBN 9780443102790. [Google Scholar]
- Montes, G.S.; Junqueira, L.C.U. The Use of the Picrosirius-Polarization Method for the Study of the Biopathology of Collagen. Mem. Inst. Oswaldo Cruz 1991, 86, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Van Putte, L.; de Schrijver, S.; Moortgat, P. The Effects of Advanced Glycation End Products (AGEs) on Dermal Wound Healing and Scar Formation: A Systematic Review. Scars Burn. Heal. 2016, 2, 205951311667682. [Google Scholar] [CrossRef] [PubMed]
- da Fonseca, T.S.; Silva, G.F.; Guerreiro-Tanomaru, J.M.; Sasso-Cerri, E.; Tanomaru-Filho, M.; Cerri, P.S. Mast Cells and Immunoexpression of FGF-1 and Ki-67 in Rat Subcutaneous Tissue Following the Implantation of Biodentine and MTA Angelus. Int. Endod. J. 2019, 52, 54–67. [Google Scholar] [CrossRef]
- Thevenot, P.T.; Baker, D.W.; Weng, H.; Sun, M.-W.; Tang, L. The Pivotal Role of Fibrocytes and Mast Cells in Mediating Fibrotic Reactions to Biomaterials. Biomaterials 2011, 32, 8394–8403. [Google Scholar] [CrossRef]

| Criteria | Scores | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Day 15 | Day 30 | Day 60 | |||||||
| GM | GL | GSHAM | GM | GL | GSHAM | GM | GL | GSHAM | |
| PMN | 3.8 | 4.8 | 2.2 | 4.8 | 4 | 3.6 | 2.8 | 7 | 1.2 |
| MN | 13.2 | 15.8 | 4.8 | 12.6 | 13.6 | 9.4 | 11.8 | 15.2 | 6.6 |
| MGC | 2 | 2.8 | 0.4 | 1.8 | 3.4 | 0.4 | 1.4 | 3.8 | 0 |
| Subtotal (×2) | 6.3 | 7.8 | 2.46 | 6.4 | 7 | 4.46 | 5.33 | 8.66 | 2.6 |
| Neovascularization | 3.6 | 5 | 2 | 4 | 5.2 | 2.2 | 3 | 4.6 | 3 |
| Connective tissue | 1.6 | 5.8 | 10 | 6 | 6 | 4 | 6 | 6 | 8 |
| Subtotal | 0.86 | 1.8 | 2 | 1.6 | 1.86 | 1.03 | 1.5 | 1.76 | 1.83 |
| Total | 7.16 | 9.6 | 4.46 | 8 | 8.86 | 5.49 | 6.8 | 10.42 | 4.43 |
| Irritation pattern (test-control) (Teste-control) | 2.7 | 5.14 | - | 2.5 | 3.37 | - | 2.4 | 5.99 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chagas, A.d.L.d.; Oliveira, L.P.d.; Cruz, M.V.; Melo, R.M.d.; Miguel, M.P.; Fernandes, K.F.; Menezes, L.B.d. Polysaccharide-Based Membrane Biocompatibility Study of Anacardium occidentale L. and Polyvinyl Alcohol after Subcutaneous Implant in Rats. Materials 2022, 15, 1296. https://doi.org/10.3390/ma15041296
Chagas AdLd, Oliveira LPd, Cruz MV, Melo RMd, Miguel MP, Fernandes KF, Menezes LBd. Polysaccharide-Based Membrane Biocompatibility Study of Anacardium occidentale L. and Polyvinyl Alcohol after Subcutaneous Implant in Rats. Materials. 2022; 15(4):1296. https://doi.org/10.3390/ma15041296
Chicago/Turabian StyleChagas, Angelica de Lima das, Leiny Paula de Oliveira, Mauricio Vicente Cruz, Renato Miranda de Melo, Marina Pacheco Miguel, Katia Flavia Fernandes, and Liliana Borges de Menezes. 2022. "Polysaccharide-Based Membrane Biocompatibility Study of Anacardium occidentale L. and Polyvinyl Alcohol after Subcutaneous Implant in Rats" Materials 15, no. 4: 1296. https://doi.org/10.3390/ma15041296
APA StyleChagas, A. d. L. d., Oliveira, L. P. d., Cruz, M. V., Melo, R. M. d., Miguel, M. P., Fernandes, K. F., & Menezes, L. B. d. (2022). Polysaccharide-Based Membrane Biocompatibility Study of Anacardium occidentale L. and Polyvinyl Alcohol after Subcutaneous Implant in Rats. Materials, 15(4), 1296. https://doi.org/10.3390/ma15041296






