Printing Accuracy and Flexural Properties of Different 3D-Printed Denture Base Resins
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
- DentaBASE (ASIGA, Erfurt, Germany);
- Denture Base Resin LP (Formlabs Inc, Somerville, MA, USA);
- Denture 3D+ (NextDent B.V., Soesterberg, The Netherlands).
2.2. Printing Accuracy
2.3. Flexural Strength and Elastic Modulus
2.4. Statistical Analysis
3. Results
3.1. Printing Accuracy
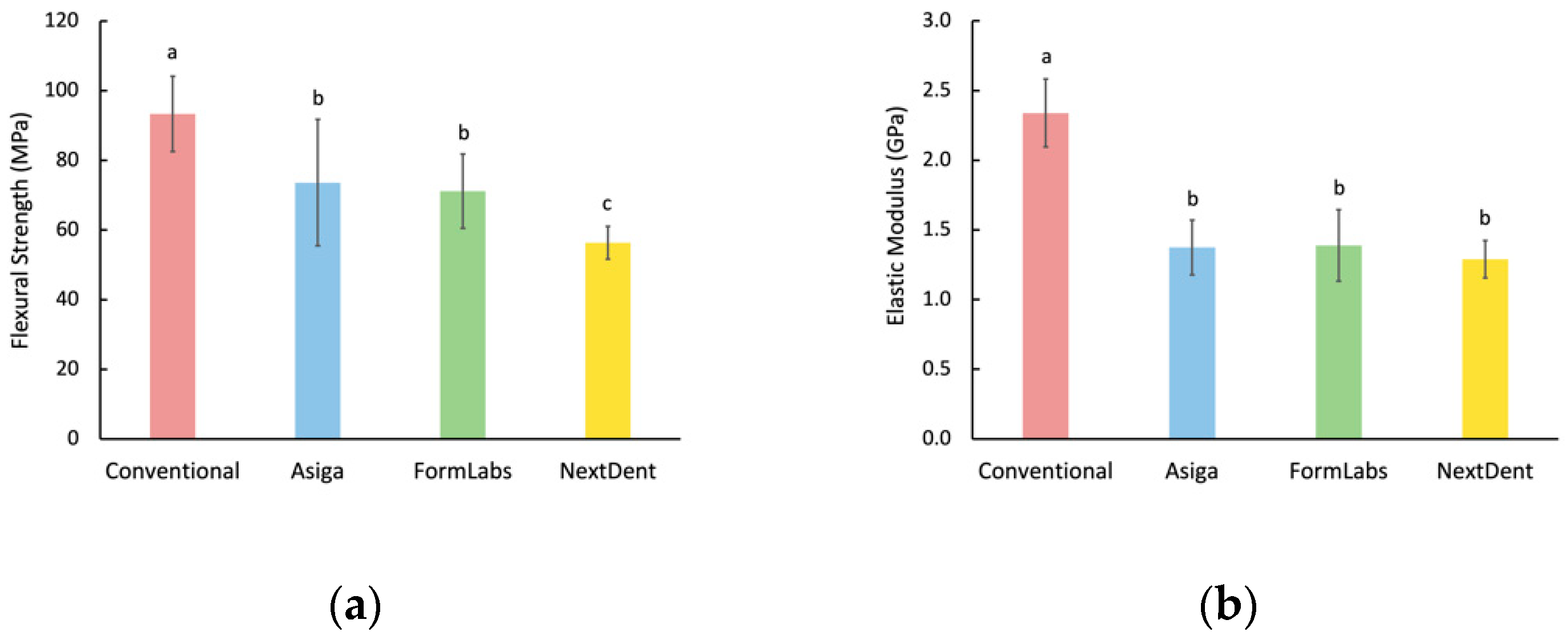
3.2. Flexural Strength and Elastic Modulus
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Wahl, E.; Zander, A.T.; Huettig, F.; Spintzyk, S. Intraoral scanning to fabricate complete dentures with functional borders: A proof-of-concept case report. BMC Oral Health 2019, 19, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herpel, C.; Tasaka, A.; Higuchi, S.; Finke, D.; Kühle, R.; Odaka, K.; Rues, S.; Lux, C.J.; Yamashita, S.; Rammelsberg, P.; et al. Accuracy of 3D printing compared with milling—A multi-center analysis of try-in dentures. J. Dent. 2021, 110, 103681. [Google Scholar] [CrossRef] [PubMed]
- Kraemer Fernandez, P.; Unkovskiy, A.; Benkendorff, V.; Klink, A.; Spintzyk, S. Surface Characteristics of Milled and 3D Printed Denture Base Materials Following Polishing and Coating: An In-Vitro Study. Materials 2020, 13, 3305. [Google Scholar] [CrossRef] [PubMed]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applica-tions in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Shim, J.S.; Kim, J.-E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental ma-terials. Dent Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Tymrak, B.M.; Kreiger, M.; Pearce, J.M. Mechanical properties of components fabricated with open-source 3-D printers under realistic environmental conditions. Mater. Des. 2014, 58, 242–246. [Google Scholar] [CrossRef] [Green Version]
- McCord, J.F. Contemporary Techniques for Denture Fabrication. J. Prosthodont. 2009, 18, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.-J.; Lee, S.J.; Park, E.-J.; Yoon, H.-I. Assessment of the trueness and tissue surface adaptation of CAD-CAM maxillary denture bases manufactured using digital light processing. J. Prosthet. Dent. 2019, 121, 110–117. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.-F.; Xie, P.-J.; Wu, J.-H. Accuracy of digital complete dentures: A systematic review of in vitro studies. J. Prosthet. Dent. 2021, 125, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Keßler, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Cheng, D.-H.; Huang, S.-C.; Lin, Y.-M. Comparison of flexural properties and cytotoxicity of interim materials printed from mono-LCD and DLP 3D printers. J. Prosthet. Dent. 2021, 126, 703–708. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Standardization. Specification 1567: Denture Base Polymers, 2nd ed.; ISO: Geneva, Switzerland, 1998. [Google Scholar]
- Barbosa, D.B.; De Souza, R.F.; Pero, A.; Marra, J.; Compagnoni, M.A. Flexural strength of acrylic resins polymerized by different cycles. J. Appl. Oral Sci. 2007, 15, 424–428. [Google Scholar] [CrossRef]
- Albasarah, S.; Al Abdulghani, H.; Alaseef, N.; Al-Qarni, F.D.; Akhtar, S.; Khan, S.Q.; Ateeq, I.S.; Gad, M.M. Impact of ZrO2 nanoparticles addition on flexural properties of denture base resin with different thickness. J. Adv. Prosthodont. 2021, 13, 226–236. [Google Scholar] [CrossRef]
- Kwon, J.S.; Kim, J.Y.; Mangal, U.; Seo, J.Y.; Lee, M.J.; Jin, J.; Yu, J.H.; Choi, S.H. Durable Oral Biofilm Resistance of 3D-Printed Dental Base Polymers Containing Zwitterionic Materials. Int. J. Mol. Sci. 2021, 22, 417. [Google Scholar] [CrossRef]
- Iwaki, M.; Kanazawa, M.; Arakida, T.; Minakuchi, S. Mechanical properties of a polymethyl methacrylate block for CAD/CAM dentures. J. Oral Sci. 2020, 62, 420–422. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; ArRejaie, A.S.; Al-Thobity, A.M. Comparative Effect of Different Polymerization Techniques on the Flex-ural and Surface Properties of Acrylic Denture Bases. J. Prosthodont. 2019, 28, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Kalberer, N.; Mehl, A.; Schimmel, M.; Müller, F.; Srinivasan, M. CAD-CAM milled versus rapidly prototyped (3D-printed) com-plete dentures: An in vitro evaluation of trueness. J. Prosthet. Dent. 2019, 121, 637–643. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. J. Prosthodont. 2021, in press. [Google Scholar] [CrossRef]
- Awad, A.N.; Cho, S.-H.; Kesterke, M.J.; Chen, J.-H. Comparison of tensile bond strength of denture reline materials on denture bases fabricated with CAD-CAM technology. J. Prosthet. Dent. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Wemken, G.; Spies, B.C.; Pieralli, S.; Adali, U.; Beuer, F.; Wesemann, C. Do hydrothermal aging and microwave sterilization affect the trueness of milled, additive manufactured and injection molded denture bases? J. Mech. Behav. Biomed. Mater. 2020, 111, 103975. [Google Scholar] [CrossRef] [PubMed]
- Neshandar Asli, H.; Rahimabadi, S.; Babaee Hemmati, Y.; Falahchai, M. Effect of different surface treatments on surface rough-ness and flexural strength of repaired 3D-printed denture base: An in vitro study. J. Prosthet. Dent. 2021, 126, 595.e1–595.e8. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.-Y.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y.; Kim, J.-G. Dimensional Accuracy of Dental Models for Three-Unit Prostheses Fabricated by Various 3D Printing Technologies. Materials 2021, 14, 1550. [Google Scholar] [CrossRef] [PubMed]
- Takamata, T.; Setcos, J.C. Resin denture bases: Review of accuracy and methods of polymerization. Int. J. Prosthodont. 1989, 2, 555–562. [Google Scholar]
- Chen, J.; Lacefield, W.; Castleberry, D. Effect of denture thickness and curing cycle on the dimensional stability of acrylic resin denture bases. Dent. Mater. 1988, 4, 20–24. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture base adaptation between CAD-CAM and con-ventional fabrication techniques. J. Prosthet. Dent. 2016, 116, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Alifui-Segbaya, F.; Bowman, J.; White, A.R.; George, R.; Fidan, I. Characterization of the Double Bond Conversion of Acrylic Res-ins for 3D Printing of Dental Prostheses. Compend. Contin. Educ. Dent. 2019, 40, e7–e11. [Google Scholar]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Väyrynen, V.O.; Tanner, J.; Vallittu, P.K. The anisotropicity of the flexural properties of an occlusal device material processed by stereolithography. J. Prosthet. Dent. 2016, 116, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Alifui-Segbaya, F.; Bowman, J.; White, A.R.; George, R.; Fidan, I.; Love, R.M. Chemical characterization of additively manufactured methacrylates for dental devices. Addit. Manuf. 2020, 31, 100944. [Google Scholar] [CrossRef]

| Material | Printer | Manufacturer | Printing Technology |
|---|---|---|---|
| ASIGA DentaBASE | ASIGA MAX™ | ASIGA, Erfurt, Germany | LED-based digital light processing (DLP) |
| Formlabs Denture Base Resin LP | Form 2 | Formlabs Inc., Somerville, MA, USA | Stereolithography (SLA) |
| NextDent Denture 3D+ | NextDent 5100 | NextDent B.V., Soesterberg, The Netherlands | Figure 4 DLP |
| Group | Layer Thickness | Printing Orientation | Wavelength/Light Intensity | Post-Curing Rinse Solution | Post-Curing Machine | Post-Curing Time/Temperature |
|---|---|---|---|---|---|---|
| ASIGA | 50 µm | 90° | 405 nm/ 13.14 mW/cm2 | Isopropyl Alcohol 99.9% | LC-D Print Box (3D systems) | 10 m/60 °C |
| Formlabs | 50 µm | 90° | 395 nm/ 1.176 mW/cm2 | Isopropyl Alcohol 99.9% | LC-D Print Box (3D systems) | 10 m/60 °C |
| NextDent | 50 µm | 90° | 405 nm/ 1.4 mW/cm3 | Isopropyl Alcohol 99.9% | LC-D Print Box (3D systems) | 10 m/60 °C |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
al-Qarni, F.D.; Gad, M.M. Printing Accuracy and Flexural Properties of Different 3D-Printed Denture Base Resins. Materials 2022, 15, 2410. https://doi.org/10.3390/ma15072410
al-Qarni FD, Gad MM. Printing Accuracy and Flexural Properties of Different 3D-Printed Denture Base Resins. Materials. 2022; 15(7):2410. https://doi.org/10.3390/ma15072410
Chicago/Turabian Styleal-Qarni, Faisal D., and Mohammed M. Gad. 2022. "Printing Accuracy and Flexural Properties of Different 3D-Printed Denture Base Resins" Materials 15, no. 7: 2410. https://doi.org/10.3390/ma15072410
APA Styleal-Qarni, F. D., & Gad, M. M. (2022). Printing Accuracy and Flexural Properties of Different 3D-Printed Denture Base Resins. Materials, 15(7), 2410. https://doi.org/10.3390/ma15072410







