Influence of Thickness of Opaque Porcelain and Alloy Color on the Final Color of Porcelain-Fused-to-Metal Restorations
Abstract
:1. Introduction
- (i)
- The thickness of the opaque layer applied on metal frameworks has no influence on the final color of PFM restorations.
- (ii)
- The difference in color of metal frameworks has no influence on the final color of PFM restorations.
2. Materials and Methods
3. Results
4. Discussion
4.1. Opaque
4.2. Alloy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walton, T.R. The Up-to-14-Year Survival and Complication Burden of 256 TiUnite Implants Supporting One-Piece Cast Abutment/Metal-Ceramic Implant-Supported Single Crowns. J. Oral. Maxillofac. Implant. 2016, 31, 1349–1358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walton, T.R. An Up-to-15-Year Comparison of the Survival and Complication Burden of Three-Unit Tooth-Supported Fixed Dental Prostheses and Implant-Supported Single Crowns. J. Oral. Maxillofac. Implant. 2015, 30, 851–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayne, S.C.; Ferracane, J.L.; Marshall, G.W.; Marshall, S.J.; van Noort, R. The Evolution of Dental Materials over the Past Century: Silver and Gold to Tooth Color and Beyond. J. Dent. Res. 2019, 98, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Fani, G.; Vichi, A.; Davidson, C.L. Spectrophotometric and visual shade measurements of human teeth using three shade guides. Am. J. Dent. 2007, 20, 142–146. [Google Scholar] [PubMed]
- Kelly, J.R.; Nishimura, I.; Campbell, S.D. Ceramics in dentistry: Historical roots and current perspectives. J. Prosthet. Dent. 1996, 75, 18–32. [Google Scholar] [CrossRef]
- Vichi, A.; Fraioli, A.; Davidson, C.L.; Ferrari, M. Influence of thickness on color in multi-layering technique. Dent. Mater. 2007, 23, 1584–1589. [Google Scholar] [CrossRef]
- Douglas, R.D.; Brewer, J.D. Variability of porcelain color reproduction by commercial laboratories. J. Prosthet. Dent. 2003, 90, 339–346. [Google Scholar] [CrossRef]
- Ozturk, O.; Uludag, B.; Usumez, A.; Sahin, V.; Celik, G. The effect of ceramic thickness and number of firings on the color of two all-ceramic systems. J. Prosthet. Dent. 2008, 100, 99–106. [Google Scholar] [CrossRef]
- Corciolani, G.; Vichi, A.; Goracci, C.; Ferrari, M. Colour correspondence of a single ceramic system in two different shade guides. J. Dent. 2009, 37, 98–101. [Google Scholar] [CrossRef]
- Fazi, G.; Vichi, A.; Corciolani, G.; Ferrari, M. Spectrophotometric evaluation of color match to VITA Classical shade guide of four different porcelain systems for metal-ceramic restorations. Am. J. Dent. 2009, 22, 19–22. [Google Scholar]
- Corciolani, G.; Vichi, A.; Louca, C.; Ferrari, M. Color match of two different ceramic systems to selected shades of one shade guide. J. Prosthet. Dent. 2011, 105, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Kürklü, D.; Azer, S.S.; Yilmaz, B.; Johnston, W.M. Porcelain thickness and cement shade effects on the colour and translucency of porcelain veneering materials. J. Dent. 2013, 41, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Xu, B. Effects of dentin and enamel porcelain layer thickness on the color of various ceramic restorations. J. Esthet. Restor. Dent. 2021, 33, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Barghi, N.; Lorenzana, R.E. Optimum thickness of opaque and body porcelain. J. Prosthet. Dent. 1982, 48, 429–431. [Google Scholar] [CrossRef] [PubMed]
- Corciolani, G.; Vichi, A.; Louca, C.; Ferrari, M. Influence of layering thickness on the color parameters of a ceramic system. Dent. Mater. 2010, 26, 737–742. [Google Scholar] [CrossRef]
- Roberts, H.W.; Berzins, D.W.; Moore, K.; Charlton, D.G. Metal–ceramic alloys in dentistry: A review. J. Prosthodont. 2009, 18, 188–194. [Google Scholar] [CrossRef]
- O’Neal, S.J.; Leinfelder, K.F.; Lemons, J.E.; Jamison, H.C. Effect of metal surfacing on the color characteristics of porcelain veneer. Dent. Mater. 1987, 3, 97–101. [Google Scholar] [CrossRef]
- Seghi, R.R.; Johnston, W.M.; O’Brien, W.J. Spectrophotometric analysis of color differences between porcelain systems. J. Prosthet. Dent. 1986, 56, 35–40. [Google Scholar] [CrossRef]
- Terada, Y.; Sakai, T.; Hirayasu, R. The masking ability of an opaque porcelain: A spectrophotometric study. Int. J. Prosthodont. 1989, 2, 259–264. [Google Scholar]
- Woolsey, G.D.; Johnson, W.M.; O’Brien, W.J. Masking power of dental opaque porcelains. J. Dent. Res. 1984, 63, 936–939. [Google Scholar] [CrossRef] [Green Version]
- Crispin, B.J.; Seghi, R.R.; Globe, H. Effect of different metal ceramic alloys on the color of opaque and dentin porcelain. J. Prosthet. Dent. 1991, 65, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Stavridakis, M.M.; Papazoglou, E.; Seghi, R.R.; Johnston, W.M.; Brantley, W.A. Effect of different high-palladium metal-ceramic alloys on the color of opaque porcelain. J. Prosthodont. 2000, 9, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Stavridakis, M.M.; Papazoglou, E.; Seghi, R.R.; Johnston, W.M.; Brantley, W.A. Effect of different high-palladium metal–ceramic alloys on the color of opaque and dentin porcelain. J. Prosthet. Dent. 2004, 92, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Ozcelik, T.B.; Yilmaz, B.; Ozcan, I.; Kircelli, C. Colorimetric analysis of opaque porcelain fired to different base metal alloys used in metal ceramic restorations. J. Prosthet. Dent. 2008, 9, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Louca, C.; Corciolani, G.; Ferrari, M. Color related to ceramic and zirconia restorations: A review. Dent. Mater. 2011, 27, 97–108. [Google Scholar] [CrossRef]
- Arif, R.; Yilmaz, B.; Mortazavi, A.; Ozcelik, T.B.; Johnston, W.M. Effect of metal opaquer on the final color of 3 ceramic crown types on 3 abutment configurations. J. Prosthet. Dent. 2018, 120, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Jörn, D.; Waddell, N.; Swain, M.W. The influence of opaque application methods on the bond strength and final shade of PFM restorations. J. Dent. 2010, 38, e143–e149. [Google Scholar] [CrossRef]
- Terada, Y.; Maeyama, S.; Hirasu, R. The influence of different thicknesses of dentin porcelain on the color reflected from thin opaque porcelain fused to metal. Int. J. Prosthodont. 1989, 2, 353–356. [Google Scholar]
- Shillingburg, H.T.; Hobo, S.; Whitsett, L.D.; Jacobi, R.; Brackett, S.E. Fundamentals of Fixed Prosthodontics, 3rd ed.; Quintessence: Chicago, IL, USA, 1997; pp. 433–481. [Google Scholar]
- Wataha, J.C. Alloys for prosthodontic restorations. J. Prosthet. Dent. 2002, 87, 351–363. [Google Scholar] [CrossRef]
- O’Connor, R.P.; Mackert, J.R., Jr.; Myers, M.L.; Parry, E.E. Castability, opaque masking, and porcelain bonding of 17 porcelain-fused-to-metal alloys. J. Prosthet. Dent. 1996, 75, 367–374. [Google Scholar] [CrossRef]
- Barrett, A.A.; Grimaudo, N.J.; Anusavice, K.J.; Yang, M.C.K. Influence of tab and disk design on shade matching of dental porcelain. J. Prosthet. Dent. 2002, 88, 591–597. [Google Scholar] [CrossRef] [Green Version]
- Vita. VM13 Working Instruction, revised ed.; Vita Zahnfabrik: Bad Sackingen, Germany, 2007; p. 18. [Google Scholar]
- Seghi, R.R.; Hewlett, E.R.; Kim, J. Visual and instrumental colorimetric assessment of small color differences on translucent dental porcelain. J. Dent. Res. 1989, 68, 1760–1764. [Google Scholar] [CrossRef] [PubMed]
- Corciolani, G.; Vichi, A. Repeatability of color reading with a clinical and a laboratory spectrophotometer. Int. Dent. S. Afr. 2006, 8, 62–70. [Google Scholar]
- Lehmann, K.M.; Igiel, C.; Schmidtmann, I.; Scheller, H. Four color-measuring devices compared with a spectrophotometric reference system. J. Dent. 2010, 38, e65–e70. [Google Scholar] [CrossRef] [PubMed]
- Clarke, F.J.J. Measurement of the Color of Human Teeth. In Dental Ceramics: Proceedings of the First International Symposium on Ceramics; Quintessence Pub Co., Inc.: Chicago, IL, USA, 1983; p. 441. [Google Scholar]
- CIE (Commission Internationale de l’Eclairage). Colorimetry—Technical Report, 2nd ed.; CIE Pub. No.15; Bureau Central de la CIE: Vienna, Austria, 1986; pp. 35–36, (corrected reprint 1996). [Google Scholar]
- Brewer, J.D.; Akers, C.K.; Garlapo, D.A.; Sorensen, S.E. Spectrometric analysis of the influence of metal substrates on the color of metal–ceramic restorations. J. Dent. Res. 1985, 64, 74–77. [Google Scholar] [CrossRef]
- Jacobs, S.H.; Goodacre, C.J.; Moore, B.K.; Dykema, R.W. Effect of porcelain thickness and type of metal–ceramic alloy on color. J. Prosthet. Dent. 1987, 57, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, B.; Ibbetson, R. The effect of the substructure on the colour of samples/restorations veneered with ceramic: A literature review. J. Dent. 2010, 38, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Ferrari, M.; Davidson, C.L. Color and opacity variations in three different resin-based composite products after water aging. Dent. Mater. 2004, 20, 530–534. [Google Scholar] [CrossRef] [Green Version]
- Ghinea, R.; Pérez, M.M.; Herrera, L.J.; Rivas, M.J.; Yebra, A.; Paravina, R.D. Color difference thresholds in dental ceramics. J. Dent. 2010, 38 (Suppl. 2), e57–e64. [Google Scholar] [CrossRef]
- Paravina, R.D.; Ghinea, R.; Herrera, L.J.; Bona, A.D.; Igiel, C.; Linninger, M.; Sakai, M.; Takahashi, H.; Tashkandi, E.; Perez Mdel, M. Color difference thresholds in dentistry. J. Esthet. Restor. Dent. 2015, 27 (Suppl. 1), S1–S9. [Google Scholar] [CrossRef]
- Paravina, R.D.; Pérez, M.M.; Ghinea, R. Acceptability and perceptibility thresholds in dentistry: A comprehensive review of clinical and research applications. J. Esthet. Restor. Dent. 2019, 31, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Heydecke, G.; Zhang, F.; Razzoog, M.E. In vitro color stability of double-layers veneers after accelerated aging. J. Prosthet. Dent. 2001, 85, 551–557. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho Panzeri Pires-de-Souza, F.; Assirati Casimiro, L.; da Fonseca Roberti Garcia, L.; Rodrigues Cruvinel, D. Color stability of dental ceramics submitted to artificial accelerated aging after repeated firings. J. Prosthet. Dent. 2009, 101, 13–18. [Google Scholar] [CrossRef] [PubMed]

| Alloy | Chemical Composition | Manufacturer | Color |
|---|---|---|---|
| Esteticor Avenir (AL1) | Au 84.0%, Pt 10.9%, Pd 2.4%, Ag 0.2%, Zn 2.2%, Ir 0.1%, Fe 0.2% | Cendres Métaux | Yellow |
| Esteticor Plus (AL2) | Au 45.0%, Pd 38.9%, Ag 5.0%, In 8.6%, Ga 1.4%, Sn 0.5%, Cu 0.4%, Ru 0.2% | Cendres Métaux | Light gray |
| Biomate C (AL3) | Ni 62.0%, Cr 25.0%, Mo 9.5%, Si 3.3% Others (P, S, Cu, Al, V, Nb) | Silpo | Dark gray |
| Pre-Drying Temperature (°C) | Pre-Drying Time (min) | Heating Time (min) | Temperature Raise Time (°C/min) | End Temperature (°C) | Hold Time End Temperature (min) | Vacuum Holding Time (min) | |
|---|---|---|---|---|---|---|---|
| Oxidation | According to Manufacturer instructions | ||||||
| Opaque Paste P * | 500 | 4.00 | 5.12 | 75 | 890 | 1.00 | 5.12 |
| Opaque Paste NP * | 500 | 4.00 | 5.36 | 75 | 920 | 1.00 | 5.36 |
| Base Dentine | 500 | 6.00 | 6.55 | 55 | 880 | 1.00 | 6.55 |
| Traspa Dentine | 500 | 6.00 | 6.44 | 55 | 870 | 1.00 | 6.44 |
| Enamel | 500 | 4.00 | 4.45 | 80 | 880 | 1.00 | - |
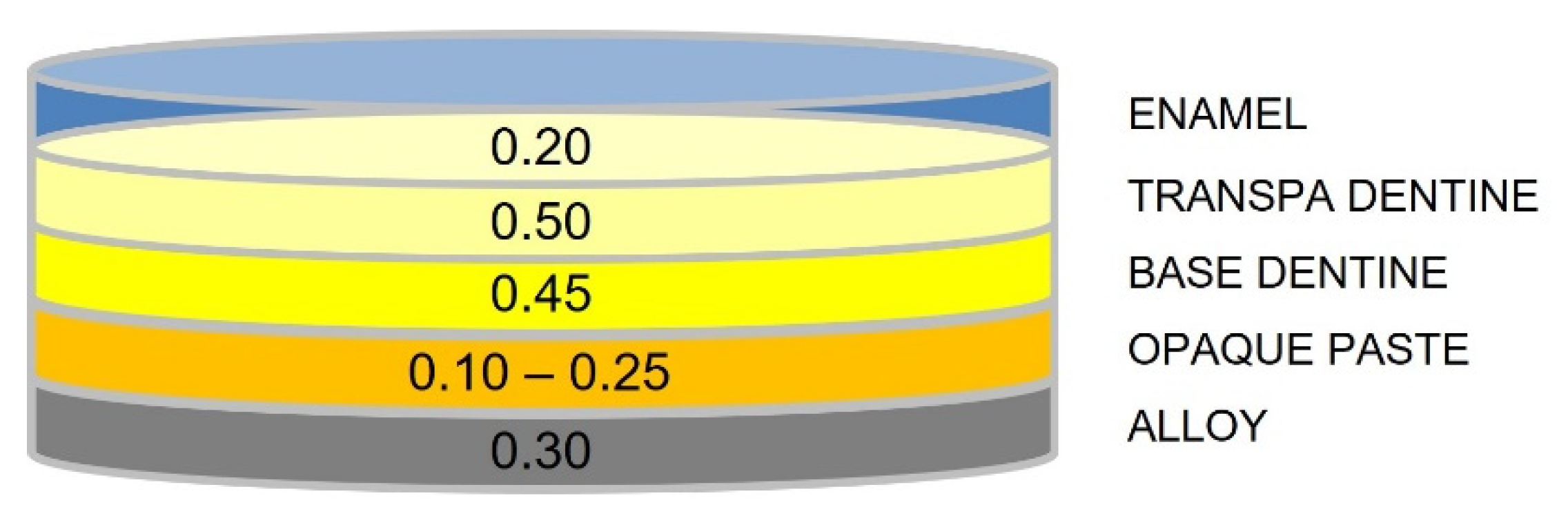
| Opaque Paste | Base Dentine | Transpa Dentine | Enamel | Total Ceramic | Total Specimen |
|---|---|---|---|---|---|
| 0.10 | 0.45 | 0.50 | 0.20 | 1.15 | 1.45 |
| 0.15 | 1.20 | 1.50 | |||
| 0.20 | 1.25 | 1.55 | |||
| 0.25 | 1.30 | 1.60 |
| 0.10 mm (TH1) | 0.15 mm (TH2) | 0.20 mm (TH3) | 0.25 mm (TH4) | Total for Alloy | Alloys Interactions | |
|---|---|---|---|---|---|---|
| Avenir (AL1) | 2.76 (0.15) | 2.36 (0.15) | 2.58 (0.26) | 2.56 (0.15) | 2.57 (0.22) | C |
| Plus (AL2) | 1.84 (0.11) | 2.04 (0.23) | 2.08 (0.25) | 2.60 (0.28) | 2.14 (0.36) | A |
| Biomate (AL3) | 2.12 (0.27) | 2.46 (0.11) | 2.36 (0.18) | 2.54 (0.21) | 2.37 (0.25) | B |
| Total for opaque thickness | 2.24 (0.44) | 2.29 (0.24) | 2.34 (0.30) | 2.57 (0.21) | ||
| Thicknesses Interactions | a | a | a | B | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vichi, A.; Corciolani, G.; Carrabba, M.; Munoz, A.; Louca, C. Influence of Thickness of Opaque Porcelain and Alloy Color on the Final Color of Porcelain-Fused-to-Metal Restorations. Materials 2023, 16, 457. https://doi.org/10.3390/ma16010457
Vichi A, Corciolani G, Carrabba M, Munoz A, Louca C. Influence of Thickness of Opaque Porcelain and Alloy Color on the Final Color of Porcelain-Fused-to-Metal Restorations. Materials. 2023; 16(1):457. https://doi.org/10.3390/ma16010457
Chicago/Turabian StyleVichi, Alessandro, Gabriele Corciolani, Michele Carrabba, Alvaro Munoz, and Chris Louca. 2023. "Influence of Thickness of Opaque Porcelain and Alloy Color on the Final Color of Porcelain-Fused-to-Metal Restorations" Materials 16, no. 1: 457. https://doi.org/10.3390/ma16010457
APA StyleVichi, A., Corciolani, G., Carrabba, M., Munoz, A., & Louca, C. (2023). Influence of Thickness of Opaque Porcelain and Alloy Color on the Final Color of Porcelain-Fused-to-Metal Restorations. Materials, 16(1), 457. https://doi.org/10.3390/ma16010457








