Investigation of the Friction Properties of a New Artificial Imitation Cartilage Material: PHEMA/Glycerol Gel
(This article belongs to the Section Biomaterials)
Abstract
:1. Introduction
2. Materials and Method
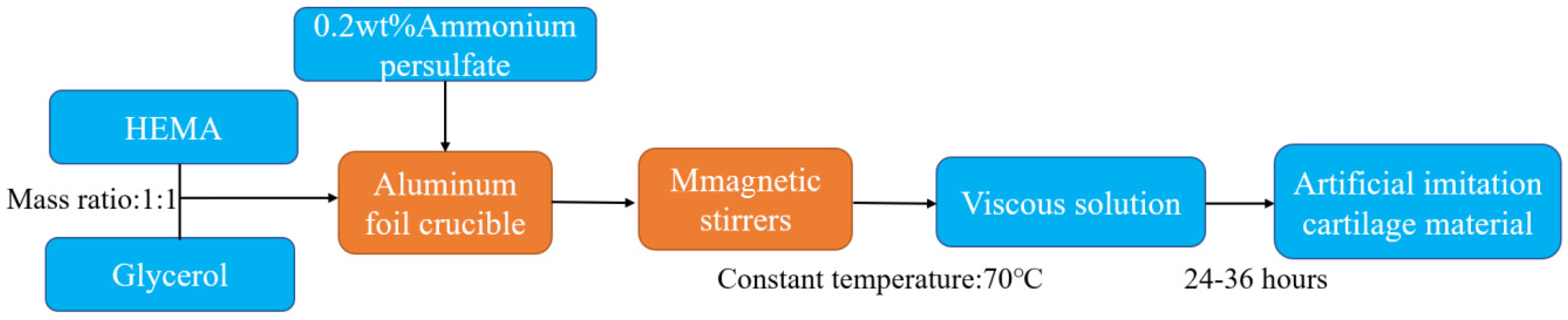
2.1. Preparation of Gel
2.2. Compressive Elasticity Test
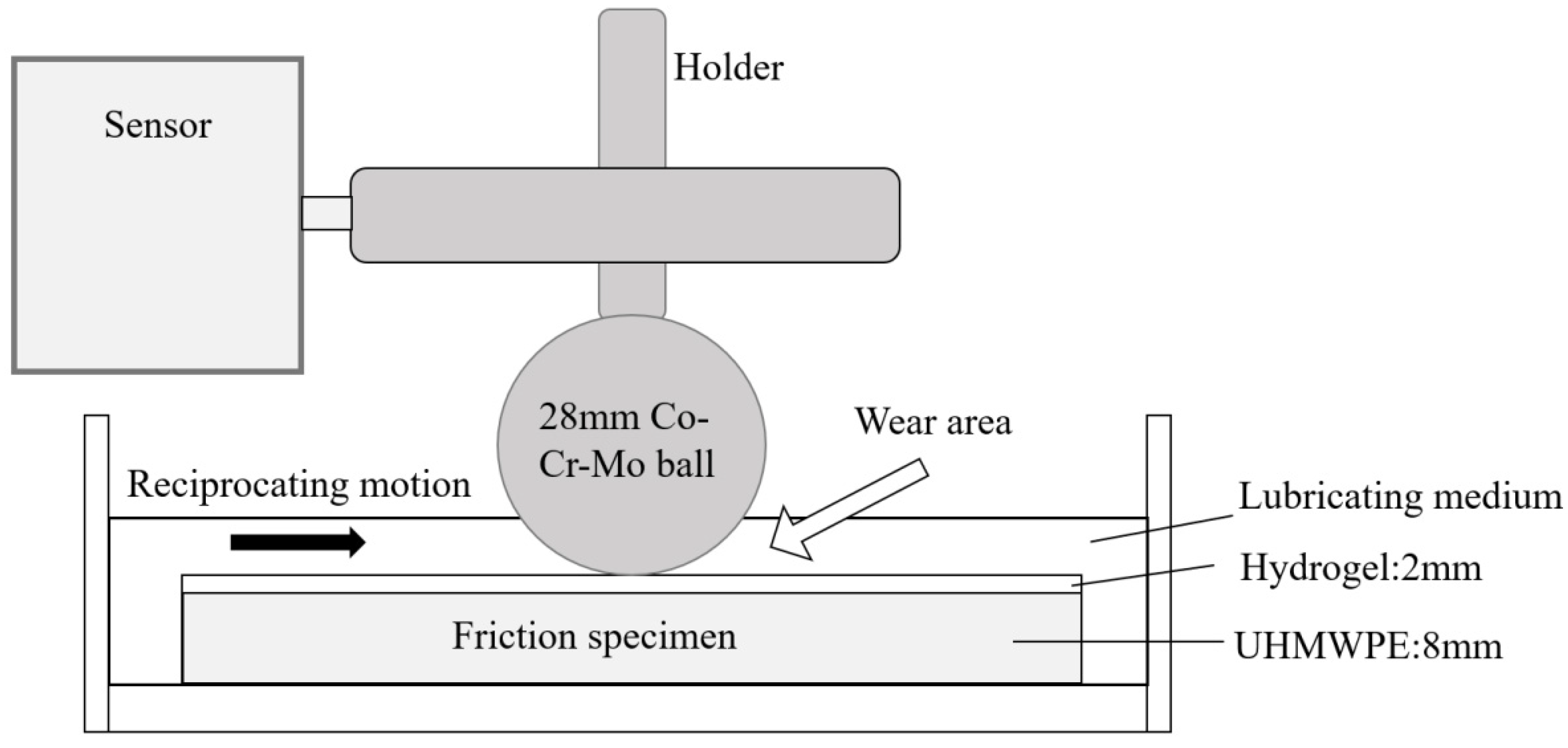
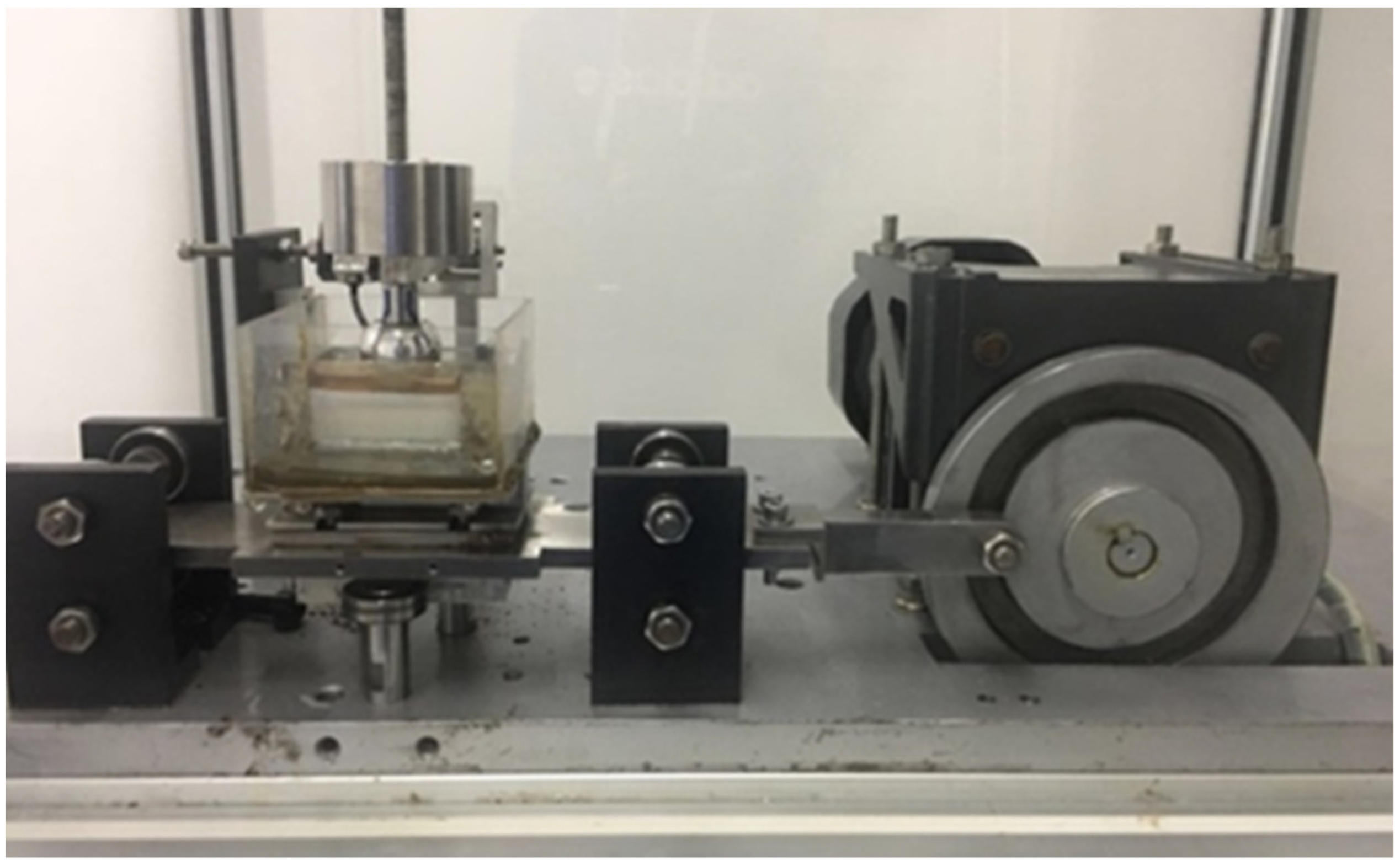
2.3. Tribological Performance Test
3. Results
3.1. Analysis of Compressive Elasticity Test
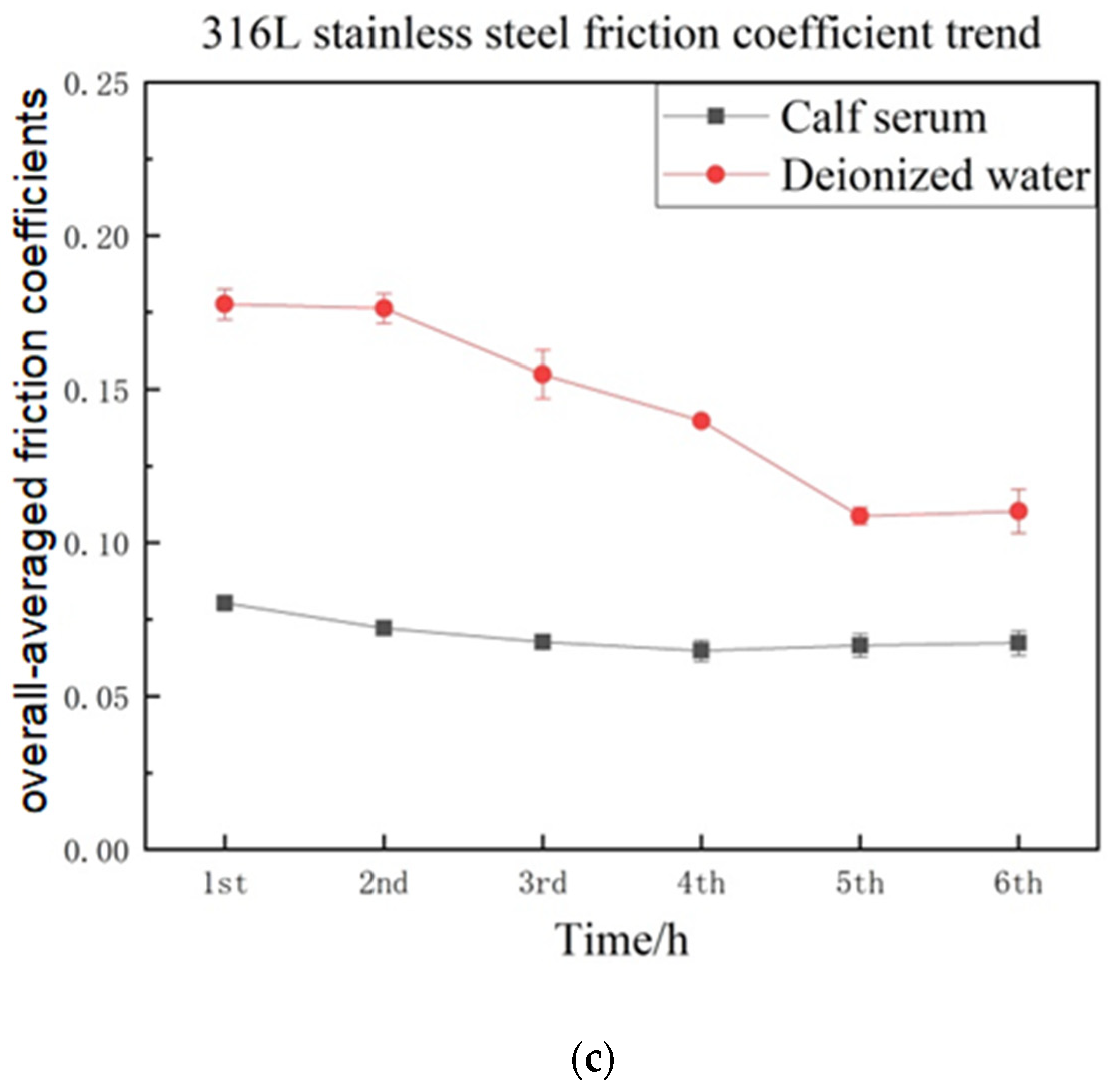
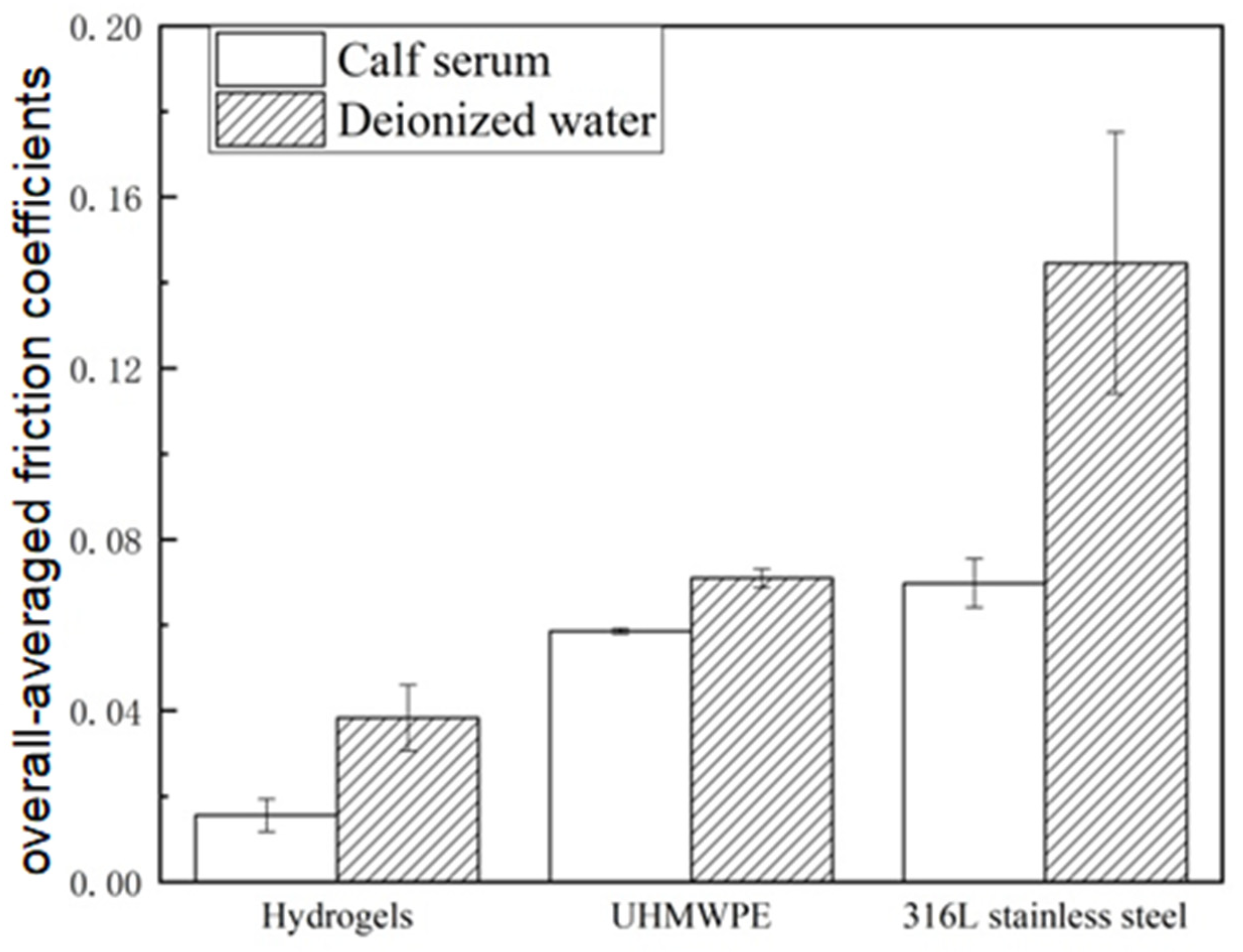
3.2. Comparative Analysis of the Friction Coefficients
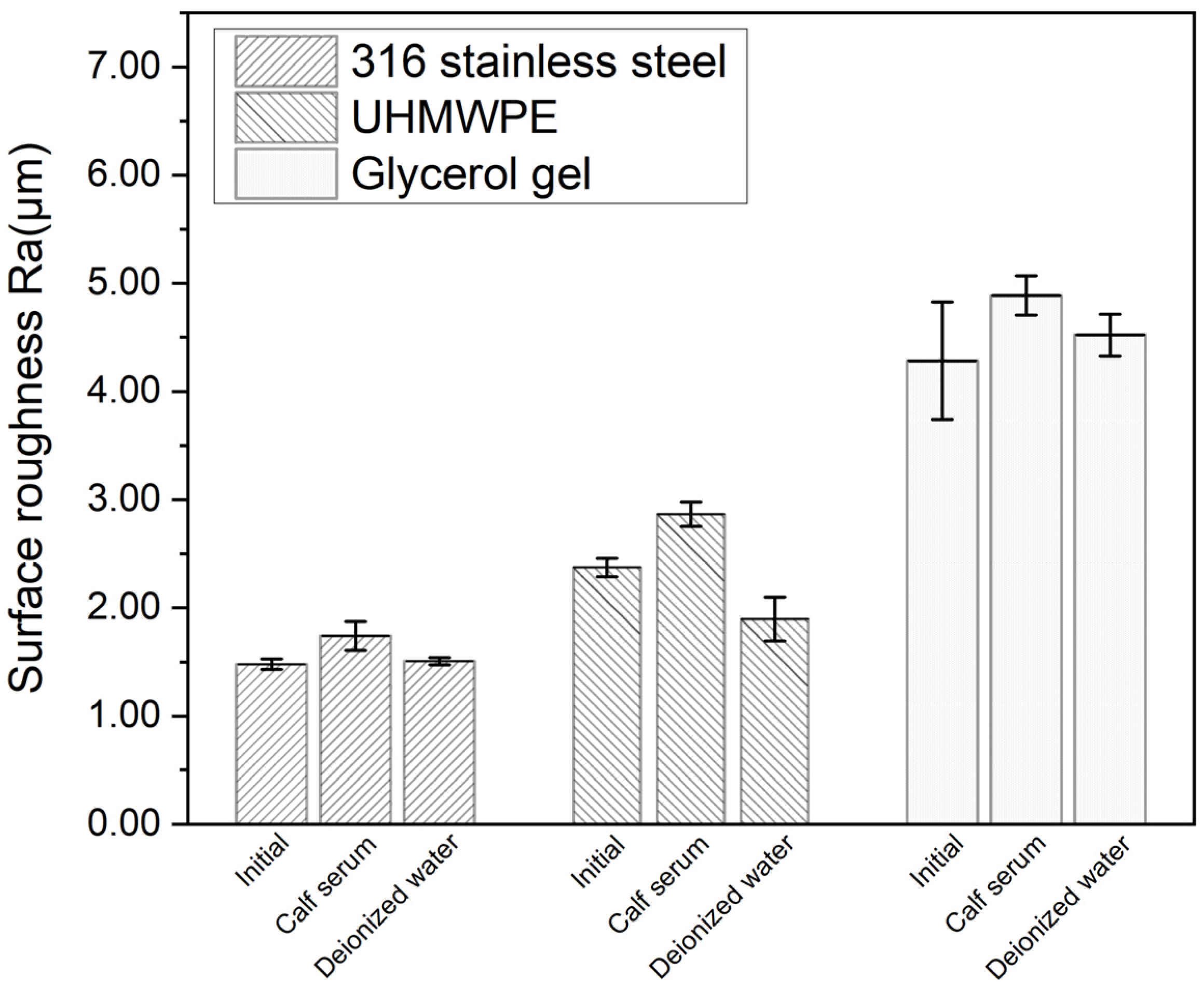
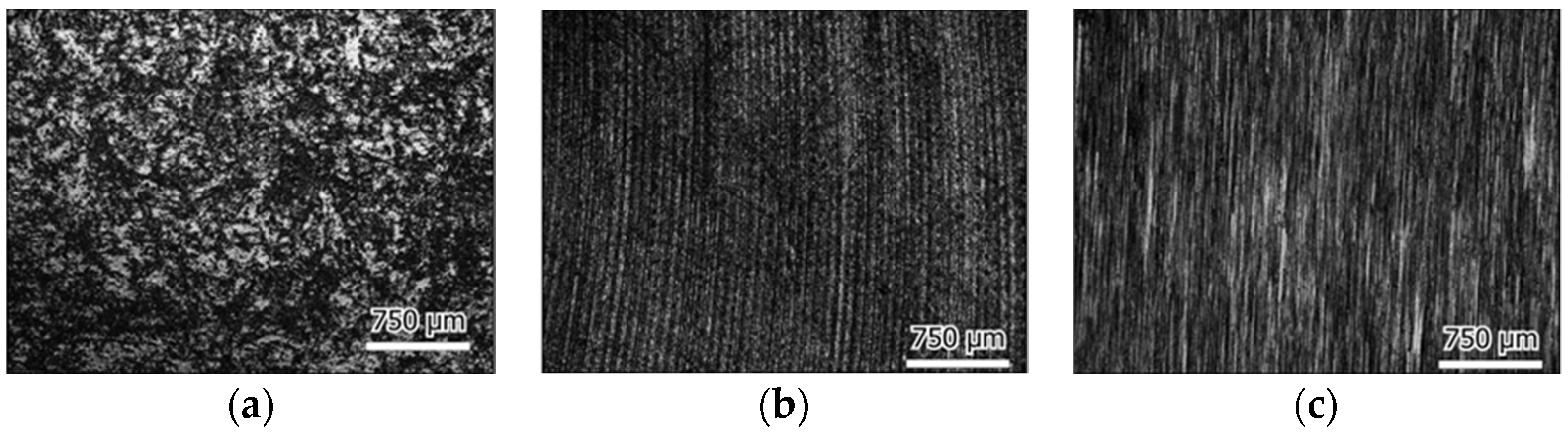
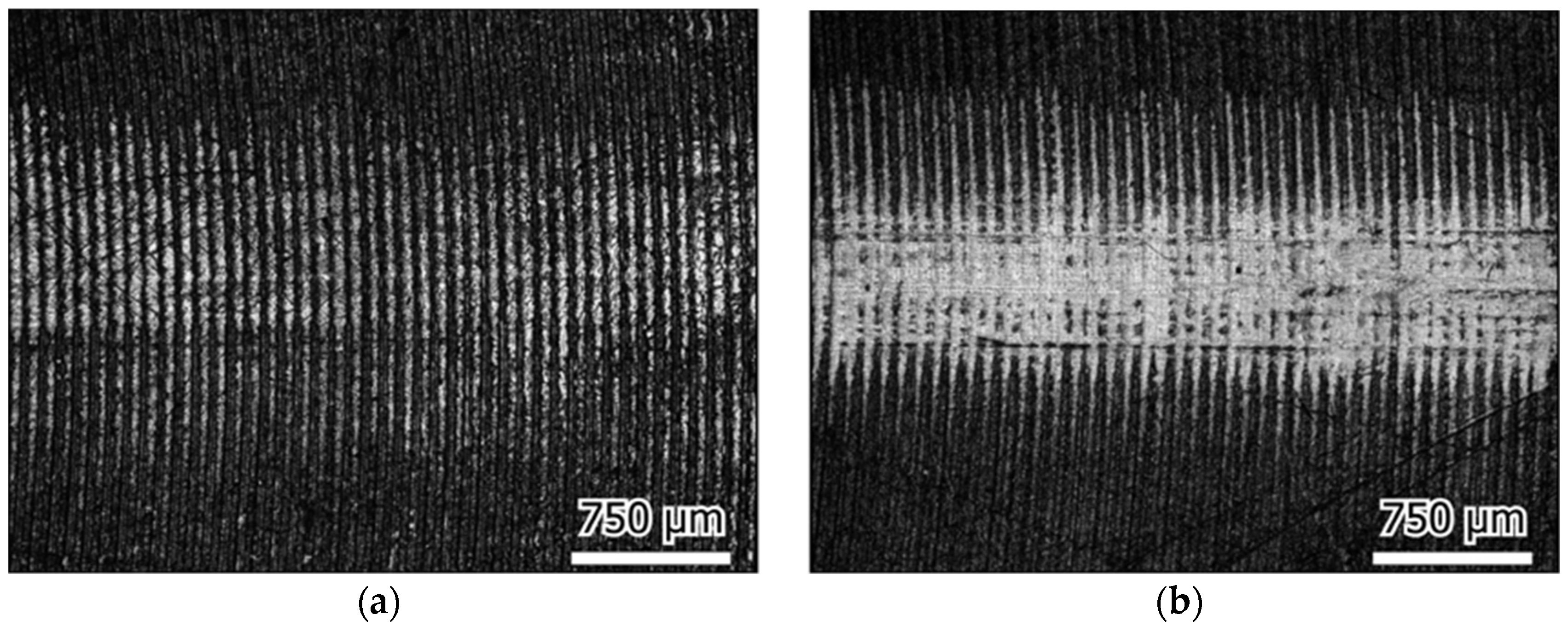
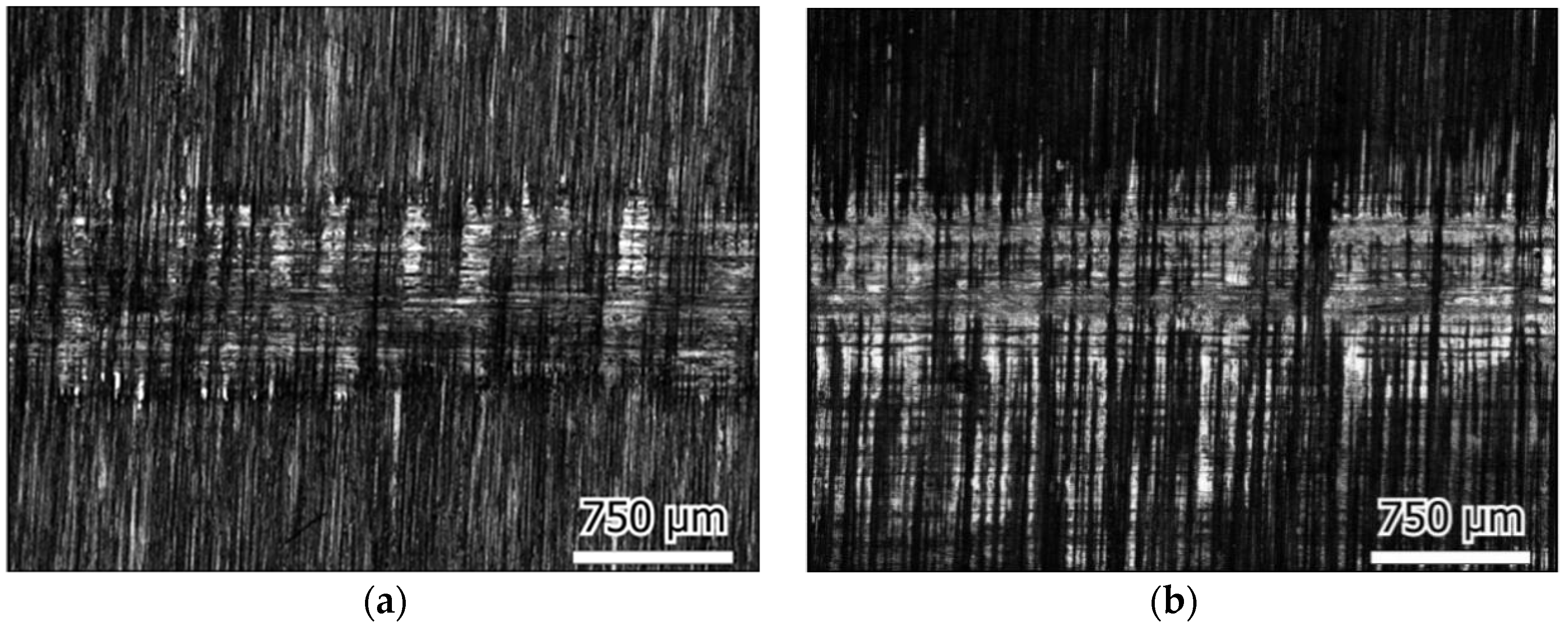
3.3. Morphological Analysis of Wear
3.4. Wear Element Released in Lubricating Media
4. Discussion
4.1. Compressive Properties
4.2. Coefficient of Friction
4.3. Surface Morphology
5. Conclusions
- The synthetic gel with HEMA and glycerin at a mass ratio of 1:1 exhibited excellent compressive properties in terms of elastic recovery and compression resistance.
- The PHEMA/glycerol gel showed a low friction coefficient which was close to the natural cartilage, and no metal ion was released in the lubricant.
- The friction coefficient increased during testing, probably due to the gel’s poro- and visco-elastic properties, and reached a stable structure in about 4 h.
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tie, X.J.; Zheng, R.G.; Zhao, M.; Han, Y.J.; Guo, H.L.; Wang, Z.Z.; Ma, G.J. Prevalence of knee osteoarthritis in the middle-aged and elderly in China: A Meta-analysis. Chin. J. Tissue Eng. Res. 2018, 22, 650–656. [Google Scholar]
- Salih, S.; Hamer, A. Hip and knee replacement. Surgery 2013, 31, 482–487. [Google Scholar] [CrossRef]
- Iavicoli, I.; Falcone, G.; Alessandrelli, M.; Cresti, R.; De Santis, V.; Salvatori, S.; Alimonti, A.; Carelli, G. The release of metals from metal-on-metal surface arthroplasty of the hip. J. Trace Elements Med. Biol. 2006, 20, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.; Reinisch, G.; Trettenhahn, G.; Zweymüller, K.; Lintner, F. Presence of corrosion products and hypersensitivity-associated reactions in periprosthetic tissue after aseptic loosening of total hip replacements with metal bearing surfaces. Acta Biomater. 2009, 5, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Wooley, P.H.; Schwarz, E.M. Aseptic loosening. Gene Ther. 2004, 11, 402–407. [Google Scholar] [CrossRef]
- Abu-Amer, Y.; Darwech, I.; Clohisy, J.C. Aseptic loosening of total joint replacements: Mechanisms underlying osteolysis and potential therapies. Arthritis Res. Ther. 2007, 9 (Suppl. 1), S6. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Linneberg, A.; Menné, T.; Johansen, J.D. The epidemiology of contact allergy in the general population—Prevalence and main findings. Contact Dermat. 2007, 57, 287–299. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Menne, T. Metal Allergy-A Review on Exposures, Penetration, Genetics, Prevalence, and Clinical Implications. Chem. Res. Toxicol. 2010, 23, 309–318. [Google Scholar] [CrossRef]
- Zhang, H.-Y.; Zhu, Y.-J.; Hu, X.-Y.; Sun, Y.-F.; Sun, Y.-L.; Han, J.-M.; Yan, Y.; Zhou, M. An investigation on the biotribocorrosion behaviour of CoCrMo alloy grafted with polyelectrolyte brush. Bio-Medical Mater. Eng. 2014, 24, 2151–2159. [Google Scholar] [CrossRef]
- Keurentjes, J.C.; Kuipers, R.M.; Wever, D.J.; Schreurs, B.W. High Incidence of Squeaking in THAs with Alumina Ceramic-on-ceramic Bearings. Clin. Orthop. Relat. Res. 2008, 466, 1438–1443. [Google Scholar] [CrossRef]
- Wu, G.-L.; Zhu, W.; Zhao, Y.; Ma, Q.; Weng, X.-S. Hip Squeaking after Ceramic-on-ceramic Total Hip Arthroplasty. Chin. Med. J. 2016, 129, 1861–1866. [Google Scholar] [CrossRef] [PubMed]
- Hua, Z.; Yan, X.; Liu, D.; Jin, Z.; Wang, X.; Liu, L. Analysis of the Friction-Induced Squeaking of Ceramic-on-Ceramic Hip Prostheses Using a Pelvic Bone Finite Element Model. Tribol. Lett. 2016, 61, 1–7. [Google Scholar] [CrossRef]
- Hosseini, S.A.; Mohammadi, R.; Noruzi, S.; Ganji, R.; Oroojalian, F.; Sahebkar, A. Evolution of hydrogels for cartilage tissue engineering of the knee: A systematic review and meta-analysis of clinical studies. Jt. Bone Spine 2020, 88, 105096. [Google Scholar] [CrossRef]
- Bostan, L.; Trunfio-Sfarghiu, A.-M.; Verestiuc, L.; Popa, M.; Munteanu, F.; Rieu, J.-P.; Berthier, Y. Mechanical and tribological properties of poly(hydroxyethyl methacrylate) hydrogels as articular cartilage substitutes. Tribol. Int. 2012, 46, 215–224. [Google Scholar] [CrossRef]
- Mahmood, H.; Eckold, D.; Stead, I.; Shepherd, D.E.; Espino, D.M.; Dearn, K.D. A method for the assessment of the coefficient of friction of articular cartilage and a replacement biomaterial. J. Mech. Behav. Biomed. Mater. 2020, 103, 103580. [Google Scholar] [CrossRef]
- Arjmandi, M.; Ramezani, M. Mechanical and tribological assessment of silica nanoparticle-alginate-polyacrylamide nanocomposite hydrogels as a cartilage replacement. J. Mech. Behav. Biomed. Mater. 2019, 95, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Stoimenov, B.; Fridrici, V.; Kapsa, P.; Kosukegawa, H.; Ohta, M. Bioengineering Materials and Conditions for Obtaining Low Friction with PVA Hydrogels. Tribol. Online 2013, 8, 140–152. [Google Scholar] [CrossRef]
- Hafezi, M.; Qin, L.; Mahmoodi, P.; Yang, H.; Dong, G. Releasable agarose-hyaluronan hydrogel with anti-friction performance and enhanced stability for artificial joint applications. Tribol. Int. 2020, 153, 106622. [Google Scholar] [CrossRef]
- Zhang, X.; Lou, Z.; Yang, X.; Chen, Q.; Chen, K.; Feng, C.; Qi, J.; Luo, T.; Zhang, D. Fabrication and Characterization of a Multilayer Hydrogel as a Candidate for Artificial Cartilage. ACS Appl. Polym. Mater. 2021, 3, 3039–5050. [Google Scholar] [CrossRef]
- Wichterle, O.; Lím, D. Hydrophilic Gels for Biological Use. Nature 1960, 185, 117–118. [Google Scholar] [CrossRef]
- Passos, M.F.; Dias, D.R.C.; Bastos, G.N.T.; Jardini, A.L.; Benatti, A.C.B.; Dias, C.G.B.T.; Maciel Filho, R. pHEMA hydrogels: Synthesis, kinetics and in vitro tests. J. Therm. Anal. Calorim. 2016, 125, 361–368. [Google Scholar] [CrossRef]
- Bavaresco, V.; Zavaglia, C.; Reis, M.; Gomes, J. Study on the tribological properties of pHEMA hydrogels for use in artificial articular cartilage. Wear 2008, 265, 269–277. [Google Scholar] [CrossRef]
- Wang, D.; Tao, D.H.; Huang, X.L.; Hua, Z.K. Preparation and properties of poly (hydroxyethyl methacrylate) glycerol gel as biomimetic cartilage replacement material. J. Mater. Eng. 2019, 47, 71–75. [Google Scholar]
- Chen, W.-M.; Jin, J.; Park, T.; Ryu, K.-S.; Lee, S.-J. Strain behavior of malaligned cervical spine implanted with metal-on-polyethylene, metal-on-metal, and elastomeric artificial disc prostheses—A finite element analysis. Clin. Biomech. 2018, 59, 19–26. [Google Scholar] [CrossRef]
- ISO (14242-2); Implants for Surgery—Wear of Total Hip-Joint Prostheses—Part 2: Methods of Measurement. ISO: Geneva, Switzerland, 2016.
- Fox, S.; Alice, J.; Bendy, A.; Rodeo, S.A. The basic science of articular cartilage: Structure, composition, and function. Sport. Health 2009, 1, 461–468. [Google Scholar]
- ISO (7206-2); Implants for Surgery—Partial and Total Hip Joint Prostheses—Part 2: Articulating Surfaces Made of Metallic, Ceramic and Plastics Materials. ISO: Geneva, Switzerland, 2011.
- Brand, R.A. Joint contact stress: A reasonable surrogate for biological processes? Iowa Orthop. J. 2005, 25, 82–94. [Google Scholar]
- Unsworth, A. Recent developments in the tribology of artificial joints. Tribol. Int. 1995, 28, 485–495. [Google Scholar] [CrossRef]
- ASTM(F732-17); Standard Test Method for Wear Testing of Polymeric Materials Used in Total Joint Prostheses. ASTM: West Conshohocken, PA, USA, 2017.
- Pan, Y.; Xiong, D. Study on compressive mechanical properties of nanohydroxyapatite reinforced poly(vinyl alcohol) gel composites as biomaterial. J. Mater. Sci. Mater. Med. 2009, 20, 1291–1297. [Google Scholar] [CrossRef]
- Wang, S.; Bao, Y.; Guan, Y.; Zhang, C.; Liu, H.; Yang, X.; Gao, L.; Guo, T.; Chen, Q. Strain distribution of repaired articular cartilage defects by tissue engineering under compression loading. J. Orthop. Surg. Res. 2018, 13, 19. [Google Scholar] [CrossRef] [PubMed]
- Ma, R.; Xiong, D.; Miao, F.; Zhang, J.; Peng, Y. Novel PVP/PVA hydrogels for articular cartilage replacement. Mater. Sci. Eng. C 2009, 29, 1979–1983. [Google Scholar] [CrossRef]
- Forster, H.; Fisher, J. The influence of continuous sliding and subsequent surface wear on the friction of articular cartilage. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 1999, 213, 329–345. [Google Scholar] [CrossRef] [PubMed]
- McCutchen, C. The frictional properties of animal joints. Wear 1962, 5, 1–17. [Google Scholar] [CrossRef]
- Caligaris, M.; Ateshian, G. Effects of sustained interstitial fluid pressurization under migrating contact area, and boundary lubrication by synovial fluid, on cartilage friction. Osteoarthr. Cartil. 2008, 16, 1220–1227. [Google Scholar] [CrossRef] [PubMed]
- Geurds, L.; Xu, Y.; Stokes, J.R. Friction of lubricated hydrogels: Influence of load, speed and lubricant viscosity. Biotribology 2021, 25, 100162. [Google Scholar] [CrossRef]
- Li, F.; Zhang, G.; Wang, A.; Guo, F. The Effects of Surface Mechanical Deformation and Bovine Serum Albumin on the Tribological Properties of Polyvinyl Alcohol Hydrogel as an Artificial Cartilage. Adv. Mater. Sci. Eng. 2017, 2017, 4502904. [Google Scholar] [CrossRef]
- Li, F.; Wang, A.; Wang, C. Analysis of friction between articular cartilage and polyvinyl alcohol hydrogel artificial cartilage. J. Mater. Sci. Mater. Med. 2016, 27, 87. [Google Scholar] [CrossRef]
- Oungoulian, S.R.; Durney, K.M.; Jones, B.K.; Ahmad, C.S.; Hung, C.T.; Ateshian, G.A. Wear and damage of articular cartilage with friction against orthopedic implant materials. J. Biomech. 2015, 48, 1957–1964. [Google Scholar] [CrossRef]
- Ihnatouski, M.; Pauk, J.; Karev, D.; Karev, B. AFM-Based Method for Measurement of Normal and Osteoarthritic Human Articular Cartilage Surface Roughness. Materials 2020, 13, 2302. [Google Scholar] [CrossRef]
- Chen, K.; Yang, X.; Zhang, D.; Xu, L.; Zhang, X.; Wang, Q. Biotribology behavior and fluid load support of PVA/HA composite hydrogel as artificial cartilage. Wear 2017, 376–377, 329–336. [Google Scholar] [CrossRef]
- Saikko, V.; Kostamo, J. RandomPOD—A new method and device for advanced wear simulation of orthopaedic biomaterials. J. Biomech. 2011, 44, 810–814. [Google Scholar] [CrossRef]
- Beddoes, C.M.; Whitehouse, M.R.; Briscoe, W.H.; Su, B. Hydrogels as a Replacement Material for Damaged Articular Hyaline Cartilage. Materials 2016, 9, 443. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.P.; Daniels, A.U.; Ronken, S.; García, H.A.; Friederich, N.F.; Kurokawa, T.; Gong, J.P.; Wirz, D. Acrylamide polymer double-network hydrogels: Candidate cartilage repair materials with cartilage-like dynamic stiffness and attractive surgery-related attachment mechanics. Cartilage 2011, 2, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Peak, C.W.; Wilker, J.J.; Schmidt, G. A review on tough and sticky hydrogels. Colloid Polym. Sci. 2013, 291, 2031–2047. [Google Scholar] [CrossRef]




| Material | Supplier |
|---|---|
| Hydroxyethyl methacrylate (HEMA) | AR, Chengdu Micxy Chemical Co., Ltd., Chengdu, China |
| Glycerol (medical glycerin) | Shangqiu Liangfeng Hygiene Products Co., Ltd., Shangqiu, China |
| Ammonium persulfate ((NH4)2S2O8) | AR, Chengdu Jinshan Chemical Reagent Co., Ltd., Chengdu, China |
| Calf serum | Gibco Cell Culture, Shanghai, China |
| Load (N) | Percentage of Original Thickness Under Load (%) | Percentage of Recovery after 3 Minutes of Unloading (%) |
|---|---|---|
| 600 | 67 | 100 |
| 700 | 64 | 100 |
| 800 | 63 | 99 |
| 900 | 62 | 98 |
| 1000 | 58 | 97 |
| Plate Material | Cr | Mo |
|---|---|---|
| PHEMA/glycerol Gel | 0 | 0 |
| UHMWPE | 0 | 0 |
| 316L stainless steel | 2.57 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hua, Z.; Hu, M.; Chen, Y.; Huang, X.; Gao, L. Investigation of the Friction Properties of a New Artificial Imitation Cartilage Material: PHEMA/Glycerol Gel. Materials 2023, 16, 4023. https://doi.org/10.3390/ma16114023
Hua Z, Hu M, Chen Y, Huang X, Gao L. Investigation of the Friction Properties of a New Artificial Imitation Cartilage Material: PHEMA/Glycerol Gel. Materials. 2023; 16(11):4023. https://doi.org/10.3390/ma16114023
Chicago/Turabian StyleHua, Zikai, Mindie Hu, Yiwen Chen, Xiuling Huang, and Leiming Gao. 2023. "Investigation of the Friction Properties of a New Artificial Imitation Cartilage Material: PHEMA/Glycerol Gel" Materials 16, no. 11: 4023. https://doi.org/10.3390/ma16114023
APA StyleHua, Z., Hu, M., Chen, Y., Huang, X., & Gao, L. (2023). Investigation of the Friction Properties of a New Artificial Imitation Cartilage Material: PHEMA/Glycerol Gel. Materials, 16(11), 4023. https://doi.org/10.3390/ma16114023






