Evaluation of Physical–Chemical Properties of Contemporary CAD/CAM Materials with Chromatic Transition “Multicolor”
Abstract
1. Introduction
2. Materials and Methods
2.1. Ultimate Tensile Strength (UTS), Flexural Strength (FS), and Modulus of Elasticity
2.2. Water Sorption
2.3. Cross-Link Density (CLD) and Surface Roughness
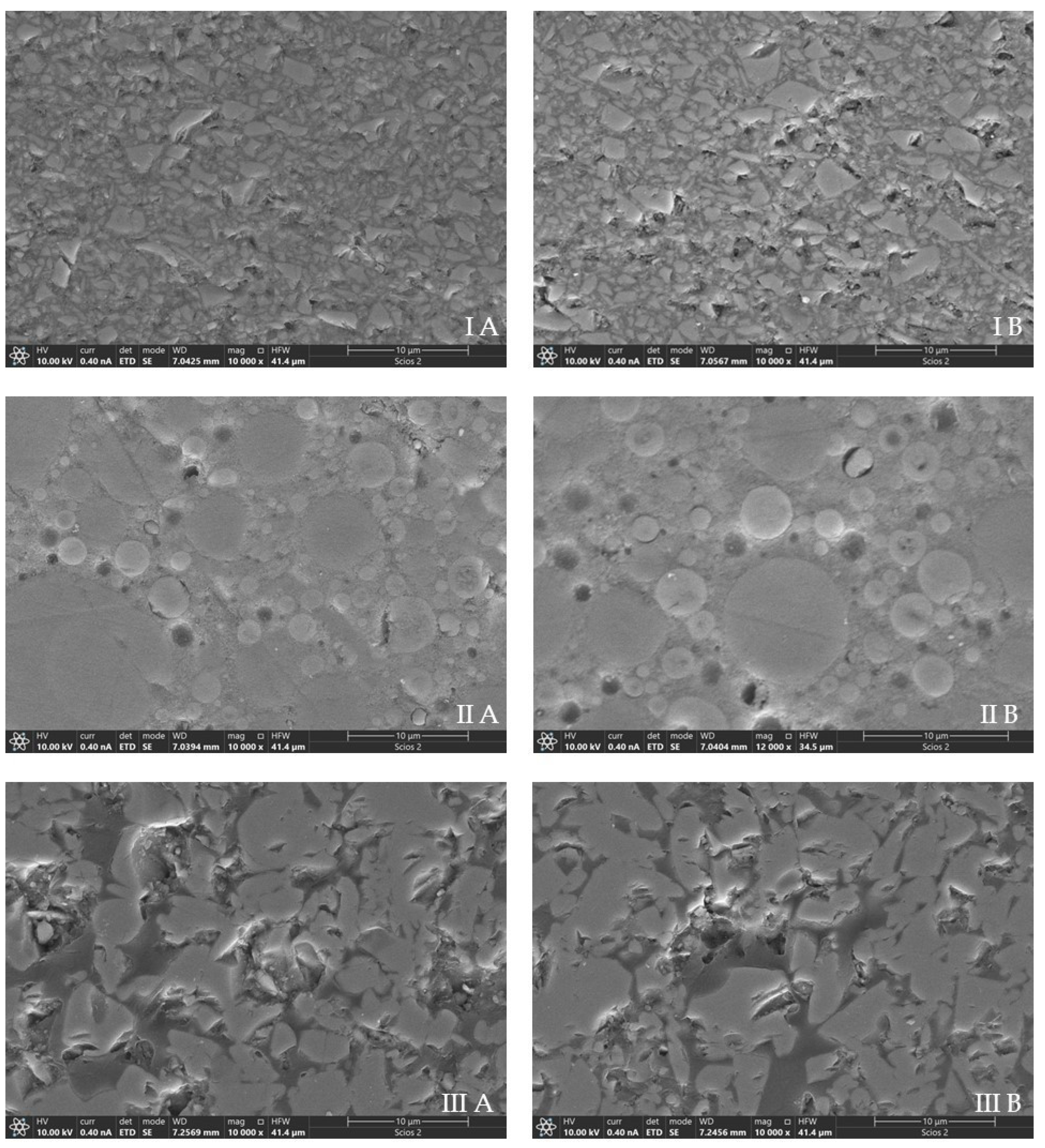
2.4. Scanning Electron Microscopy
2.5. Statistical Analysis
3. Results
3.1. Ultimate Tensile Strength Test (UTS), Flexural Strength (FS), and Modulus of Elasticity
3.2. Water Sorption
3.3. Cross-Link Density (CLD) and Surface Roughness
3.4. Scanning Electron Microscopy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rekow, E.D. Digital Dentistry: The New State of the Art—Is It Disruptive or Destructive? Dent. Mater. 2020, 36, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Alamoush, R.A.; Sung, R.; Satterthwaite, J.D.; Silikas, N. The Effect of Different Storage Media on the Monomer Elution and Hardness of CAD/CAM Composite Blocks. Dent. Mater. 2021, 37, 1202–1213. [Google Scholar] [CrossRef]
- Giordano, R. Materials for Chairside CAD/CAM-Produced Restorations. J. Am. Dent. Assoc. 2006, 137 (Suppl. 1), 14S–21S. [Google Scholar] [CrossRef]
- Ruse, N.D.; Sadoun, M.J. Resin-Composite Blocks for Dental CAD/CAM Applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef]
- Nicholson, J.W.; Sidhu, S.K.; Czarnecka, B. Enhancing the Mechanical Properties of Glass-Ionomer Dental Cements: A Review. Materials 2020, 13, 2510. [Google Scholar] [CrossRef]
- Rosentritt, M.; Hahnel, S.; Schneider-Feyrer, S.; Strasser, T.; Schmid, A. Martens Hardness of CAD/CAM Resin-Based Composites. Appl. Sci. 2022, 12, 7698. [Google Scholar] [CrossRef]
- Hensel, F.; Koenig, A.; Doerfler, H.-M.; Fuchs, F.; Rosentritt, M.; Hahnel, S. CAD/CAM Resin-Based Composites for Use in Long-Term Temporary Fixed Dental Prostheses. Polymers 2021, 13, 3469. [Google Scholar] [CrossRef] [PubMed]
- Grzebieluch, W.; Mikulewicz, M.; Kaczmarek, U. Resin Composite Materials for Chairside CAD/CAM Restorations: A Comparison of Selected Mechanical Properties. J. Healthc. Eng. 2021, 2021, 8828954. [Google Scholar] [CrossRef] [PubMed]
- Bahadır, H.S.; Bayraktar, Y. Evaluation of the Repair Capacities and Color Stabilities of a Resin Nanoceramic and Hybrid CAD/CAM Blocks. J. Adv. Prosthodont. 2020, 12, 140–149. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.-F. Evaluation of Mechanical and Optical Behavior of Current Esthetic Dental Restorative CAD/CAM Composites. J. Mech. Behav. Biomed. Mater. 2016, 55, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lambert, H.; Durand, J.-C.; Jacquot, B.; Fages, M. Dental Biomaterials for Chairside CAD/CAM: State of the Art. J. Adv. Prosthodont. 2017, 9, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Wendler, M.; Stenger, A.; Ripper, J.; Priewich, E.; Belli, R.; Lohbauer, U. Mechanical Degradation of Contemporary CAD/CAM Resin Composite Materials after Water Ageing. Dent. Mater. 2021, 37, 1156–1167. [Google Scholar] [CrossRef] [PubMed]
- Ling, L.; Ma, Y.; Malyala, R. A Novel CAD/CAM Resin Composite Block with High Mechanical Properties. Dent. Mater. 2021, 37, 1150–1155. [Google Scholar] [CrossRef]
- Marchesi, G.; Piloni, A.C.; Nicolin, V.; Turco, G.; Di Lenarda, R. Chairside Cad/Cam Materials: Current Trends of Clinical Uses. Biology 2021, 10, 1170. [Google Scholar] [CrossRef]
- Ionescu, A.C.; Hahnel, S.; König, A.; Brambilla, E. Resin Composite Blocks for Dental CAD/CAM Applications Reduce Biofilm Formation in Vitro. Dent. Mater. 2020, 36, 603–616. [Google Scholar] [CrossRef]
- Alamoush, R.A.; Silikas, N.; Salim, N.A.; Al-Nasrawi, S.; Satterthwaite, J.D. Effect of the Composition of CAD/CAM Composite Blocks on Mechanical Properties. BioMed Res. Int. 2018, 2018, 4893143. [Google Scholar] [CrossRef]
- Knezevic, A.; Zeljezic, D.; Kopjar, N.; Duarte, S.J.; Par, M.; Tarle, Z. Toxicology of Pre-Heated Composites Polymerized Directly and Through CAD/CAM Overlay. Acta Stomatol. Croat. 2018, 52, 203–217. [Google Scholar] [CrossRef]
- Sideridou, I.; Tserki, V.; Papanastasiou, G. Study of Water Sorption, Solubility and Modulus of Elasticity of Light-Cured Dimethacrylate-Based Dental Resins. Biomaterials 2003, 24, 655–665. [Google Scholar] [CrossRef]
- Ferracane, J.L. Hygroscopic and Hydrolytic Effects in Dental Polymer Networks. Dent. Mater. 2006, 22, 211–222. [Google Scholar] [CrossRef]
- Mourouzis, P.; Diamantopoulou, E.-I.; Plastiras, O.; Samanidou, V.; Tolidis, K. Elution of Monomers From CAD-CAM Materials and Conventional Resin Composite in Distilled Water and Artificial Saliva. Oper. Dent. 2022, 47, E241–E252. [Google Scholar] [CrossRef]
- Szczesio-Wlodarczyk, A.; Sokolowski, J.; Kleczewska, J.; Bociong, K. Ageing of Dental Composites Based on Methacrylate Resins—A Critical Review of the Causes and Method of Assessment. Polymers 2020, 12, 882. [Google Scholar] [CrossRef]
- Heintze, S.D.; Ilie, N.; Hickel, R.; Reis, A.; Loguercio, A.; Rousson, V. Laboratory Mechanical Parameters of Composite Resins and Their Relation to Fractures and Wear in Clinical Trials—A Systematic Review. Dent. Mater. 2017, 33, e101–e114. [Google Scholar] [CrossRef] [PubMed]
- Grandio Disc Multicolor: Aesthetically Pleasing Restorations at the Push of a Button. Available online: https://www.voco.dental/en/service/press/press-area/grandio-disc-multicolor-aesthetically-pleasing-restorations-at-the-push-of-a-button.aspx (accessed on 19 March 2023).
- El-Askary, F.S.; Botros, S.A.; Nassif, M.S.A.; Özcan, M. Flexural Strength of Nano-Hybrid Resin Composite as a Function of Light Attenuation Distance and Specimen Dimension. J. Adhes. Sci. Technol. 2017, 31, 520–529. [Google Scholar] [CrossRef]
- Sfalcin, R.A.; Correr, A.B.; Morbidelli, L.R.; Araújo, T.G.F.; Feitosa, V.P.; Correr-Sobrinho, L.; Watson, T.F.; Sauro, S. Influence of Bioactive Particles on the Chemical-Mechanical Properties of Experimental Enamel Resin Infiltrants. Clin. Oral Investig. 2017, 21, 2143–2151. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.F.J.; Moraes, R.R.; Cavalcante, L.M.; Sinhoreti, M.A.C.; Correr-Sobrinho, L.; Consani, S. Cross-Link Density Evaluation through Softening Tests: Effect of Ethanol Concentration. Dent. Mater. 2008, 24, 199–203. [Google Scholar] [CrossRef]
- Babaier, R.; Haider, J.; Silikas, N.; Watts, D.C. Effect of CAD/CAM Aesthetic Material Thickness and Translucency on the Polymerisation of Light- and Dual-Cured Resin Cements. Dent. Mater. 2022, 38, 2073–2083. [Google Scholar] [CrossRef]
- Scribante, A.; Bollardi, M.; Chiesa, M.; Poggio, C.; Colombo, M. Flexural Properties and Elastic Modulus of Different Esthetic Restorative Materials: Evaluation after Exposure to Acidic Drink. BioMed Res. Int. 2019, 2019, 5109481. [Google Scholar] [CrossRef]
- Abhay, S.S.; Ganapathy, D.; Veeraiyan, D.N.; Ariga, P.; Heboyan, A.; Amornvit, P.; Rokaya, D.; Srimaneepong, V. Wear Resistance, Color Stability and Displacement Resistance of Milled PEEK Crowns Compared to Zirconia Crowns under Stimulated Chewing and High-Performance Aging. Polymers 2021, 13, 3761. [Google Scholar] [CrossRef]
- Thompson, G.A.; Luo, Q. Contribution of Postpolymerization Conditioning and Storage Environments to the Mechanical Properties of Three Interim Restorative Materials. J. Prosthet. Dent. 2014, 112, 638–648. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of Flexural Strength of Different CAD/CAM PMMA-Based Polymers. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 28, e491–e495. [Google Scholar] [CrossRef]
- Heboyan, A.; Zafar, M.S.; Rokaya, D.; Khurshid, Z. Insights and Advancements in Biomaterials for Prosthodontics and Implant Dentistry. Molecules 2022, 27, 5116. [Google Scholar] [CrossRef]
- Fouda, S.M.; Gad, M.M.; Ellakany, P.A.; Al Ghamdi, M.; Khan, S.Q.; Akhtar, S.; Ali, M.S.; Al-Harbi, F.A. Flexural Properties, Impact Strength, and Hardness of Nanodiamond-Modified PMMA Denture Base Resin. Int. J. Biomater. 2022, 2022, 6583084. [Google Scholar] [CrossRef]
- Calabrese, L.; Fabiano, F.; Bonaccorsi, L.M.; Fabiano, V.; Borsellino, C. Evaluation of the Clinical Impact of ISO 4049 in Comparison with Miniflexural Test on Mechanical Performances of Resin Based Composite. Int. J. Biomater. 2015, 2015, 149798. [Google Scholar] [CrossRef]
- Chirumamilla, G.; Goldstein, C.E.; Lawson, N.C. A 2-Year Retrospective Clinical Study of Enamic Crowns Performed in a Private Practice Setting. J. Esthet. Restor. Dent. 2016, 28, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Wendler, M.; Belli, R.; Petschelt, A.; Mevec, D.; Harrer, W.; Lube, T.; Danzer, R.; Lohbauer, U. Chairside CAD/CAM Materials. Part 2: Flexural Strength Testing. Dent. Mater. 2017, 33, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Ludovichetti, F.S.; Trindade, F.Z.; Werner, A.; Kleverlaan, C.J.; Fonseca, R.G. Wear Resistance and Abrasiveness of CAD-CAM Monolithic Materials. J. Prosthet. Dent. 2018, 120, e1–e318. [Google Scholar] [CrossRef] [PubMed]
- Hynkova, K.; Ozcan, M.; Voborná, I. Composition and Mechanical Properties of Contemporary CAD/CAM Glass Ceramics. Ital. J. Dent. Med. 2020, 5, 63–69. [Google Scholar]
- Porto, T.S.; Roperto, R.C.; Akkus, A.; Akkus, O.; Teich, S.; Faddoul, F.; Porto-Neto, S.T.; Campos, E.A. Effect of Storage and Aging Conditions on the Flexural Strength and Flexural Modulus of CAD/CAM Materials. Dent. Mater. J. 2019, 38, 264–270. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Kowalewski, P.; Sopel, M.; Mikulewicz, M. Influence of Artificial Aging on Mechanical Properties of Six Resin Composite Blocks for CAD/CAM Application. Coatings 2022, 12, 837. [Google Scholar] [CrossRef]
- Abualsaud, R.; Gad, M.M. Flexural Strength of CAD/CAM Denture Base Materials: Systematic Review and Meta-Analysis of: In-Vitro: Studies. J. Int. Soc. Prev. Community Dent. 2022, 12, 160. [Google Scholar] [CrossRef]
- Alt, V.; Hannig, M.; Wöstmann, B.; Balkenhol, M. Fracture Strength of Temporary Fixed Partial Dentures: CAD/CAM versus Directly Fabricated Restorations. Dent. Mater. 2011, 27, 339–347. [Google Scholar] [CrossRef]
- Bähr, N.; Keul, C.; Edelhoff, D.; Eichberger, M.; Roos, M.; Gernet, W.; Stawarczyk, B. Effect of Different Adhesives Combined with Two Resin Composite Cements on Shear Bond Strength to Polymeric CAD/CAM Materials. Dent. Mater. J. 2013, 32, 492–501. [Google Scholar] [CrossRef]
- Bai, Y.; Yuan, S.; Wu, J. Evaluation of Surface Roughness and Elastic Modulus in Ceramic and Resin Composite CAD/CAM Materials during Ageing. Ceram.-Silikaty 2021, 65, 24–29. [Google Scholar] [CrossRef]
- Ducke, V.M.; Ilie, N. Aging Behavior of High-Translucent CAD/CAM Resin-Based Composite Blocks. J. Mech. Behav. Biomed. Mater. 2021, 115, 104269. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, J. Effect of Immersion in Various Media on the Sorption, Solubility, Elution of Unreacted Monomers, and Flexural Properties of Two Model Dental Composite Compositions. J. Mater. Sci. Mater. Med. 2008, 19, 2477–2483. [Google Scholar] [CrossRef] [PubMed]
- Niem, T. Influence of Accelerated Ageing on the Physical Properties of CAD/CAM Restorative Materials. Clin. Oral Investig. 2020, 24, 2415–2425. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Yu, Y.; Gao, S.; Zhang, Z.; Zhao, H. Biodegradation of Dental Resin-Based Composite—A Potential Factor Affecting the Bonding Effect: A Narrative Review. Biomedicines 2022, 10, 2313. [Google Scholar] [CrossRef] [PubMed]
- Farahat, D.S.; El-Wassefy, N.A. Effects of Food-Simulating Solutions on the Surface Properties of Two CAD/CAM Resin Composites. J. Clin. Exp. Dent. 2022, 14, e782–e790. [Google Scholar] [CrossRef]
- Yao, J.; Li, J.; Wang, Y.; Huang, H. Comparison of the Flexural Strength and Marginal Accuracy of Traditional and CAD/CAM Interim Materials before and after Thermal Cycling. J. Prosthet. Dent. 2014, 112, 649–657. [Google Scholar] [CrossRef]
- Palacios, T.; Tarancón, S.; Pastor, J.Y. On the Mechanical Properties of Hybrid Dental Materials for CAD/CAM Restorations. Polymers 2022, 14, 3252. [Google Scholar] [CrossRef]
- Egilmez, F.; Ergun, G.; Cekic-Nagas, I.; Vallittu, P.K.; Lassila, L.V.J. Does Artificial Aging Affect Mechanical Properties of CAD/CAM Composite Materials. J. Prosthodont. Res. 2018, 62, 65–74. [Google Scholar] [CrossRef]
- Kim, S.H.; Choi, Y.S.; Kang, K.H.; Att, W. Effects of Thermal and Mechanical Cycling on the Mechanical Strength and Surface Properties of Dental CAD-CAM Restorative Materials. J. Prosthet. Dent. 2022, 128, 79–88. [Google Scholar] [CrossRef]
- Masouras, K.; Silikas, N.; Watts, D.C. Correlation of Filler Content and Elastic Properties of Resin-Composites. Dent. Mater. 2008, 24, 932–939. [Google Scholar] [CrossRef]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical Properties of Polymer-Infiltrated-Ceramic-Network Materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- ISO/FDIS:4049; Dentistry: Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2009.
- Alamoush, R.A.; Salim, N.A.; Silikas, N.; Satterthwaite, J.D. Long-Term Hydrolytic Stability of CAD/CAM Composite Blocks. Eur. J. Oral Sci. 2022, 130, e12834. [Google Scholar] [CrossRef]
- Ilie, N. Accelerated versus Slow In Vitro Aging Methods and Their Impact on Universal Chromatic, Urethane-Based Composites. Materials 2023, 16, 2143. [Google Scholar] [CrossRef]
- Marovic, D.; Par, M.; Macan, M.; Klarić, N.; Plazonić, I.; Tarle, Z. Aging-Dependent Changes in Mechanical Properties of the New Generation of Bulk-Fill Composites. Materials 2022, 15, 902. [Google Scholar] [CrossRef] [PubMed]
- Liebermann, A.; Wimmer, T.; Schmidlin, P.R.; Scherer, H.; Löffler, P.; Roos, M.; Stawarczyk, B. Physicomechanical Characterization of Polyetheretherketone and Current Esthetic Dental CAD/CAM Polymers after Aging in Different Storage Media. J. Prosthet. Dent. 2016, 115, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Elution of Leachable Components from Composites. J. Oral Rehabil. 1994, 21, 441–452. [Google Scholar] [CrossRef]
- Colombo, M.; Poggio, C.; Lasagna, A.; Chiesa, M.; Scribante, A. Vickers Micro-Hardness of New Restorative CAD/CAM Dental Materials: Evaluation and Comparison after Exposure to Acidic Drink. Materials 2019, 12, 1246. [Google Scholar] [CrossRef] [PubMed]
- Tango, R.N.; Todorović, A.; Stamenković, D.; Karasan, D.N.; Sailer, I.; Paravina, R.D. Effect of Staining and Aging on Translucency Parameter of CAD-CAM Materials. Acta Stomatol. Croat. 2021, 55, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Hampe, T.; Wiessner, A.; Frauendorf, H.; Alhussein, M.; Karlovsky, P.; Bürgers, R.; Krohn, S. Monomer Release from Dental Resins: The Current Status on Study Setup, Detection and Quantification for In Vitro Testing. Polymers 2022, 14, 1790. [Google Scholar] [CrossRef]
- Alshali, R.Z.; Salim, N.A.; Satterthwaite, J.D.; Silikas, N. Long-Term Sorption and Solubility of Bulk-Fill and Conventional Resin-Composites in Water and Artificial Saliva. J. Dent. 2015, 43, 1511–1518. [Google Scholar] [CrossRef] [PubMed]
- Alshali, R.Z.; Salim, N.A.; Sung, R.; Satterthwaite, J.D.; Silikas, N. Analysis of Long-Term Monomer Elution from Bulk-Fill and Conventional Resin-Composites Using High Performance Liquid Chromatography. Dent. Mater. 2015, 31, 1587–1598. [Google Scholar] [CrossRef]
- Sunbul, H.A.; Silikas, N.; Watts, D.C. Surface and Bulk Properties of Dental Resin- Composites after Solvent Storage. Dent. Mater. 2016, 32, 987–997. [Google Scholar] [CrossRef]
- Ilie, N. Altering of Optical and Mechanical Properties in High-Translucent CAD-CAM Resin Composites during Aging. J. Dent. 2019, 85, 64–72. [Google Scholar] [CrossRef]
- Saba, D.A.; Salama, R.A.; Haridy, R. Effect of Different Beverages on the Color Stability and Microhardness of CAD/CAM Hybrid versus Feldspathic Ceramic Blocks: An In-Vitro Study. Futur. Dent. J. 2017, 3, 61–66. [Google Scholar] [CrossRef]
- Atay, A.; Sağirkaya, E. Effects of Different Storage Conditions on Mechanical Properties of CAD/CAM Restorative Materials. Odovtos-Int. J. Dent. Sci. 2020, 22, 83–96. [Google Scholar] [CrossRef]
- Sonmez, N.; Gultekin, P.; Turp, V.; Akgungor, G.; Sen, D.; Mijiritsky, E. Evaluation of Five CAD/CAM Materials by Microstructural Characterization and Mechanical Tests: A Comparative in Vitro Study. BMC Oral Health 2018, 18, 5. [Google Scholar] [CrossRef]
- Mota, E.G.; Smidt, L.N.; Fracasso, L.M.; Burnett, L.H.; Spohr, A.M. The Effect of Milling and Postmilling Procedures on the Surface Roughness of CAD/CAM Materials. J. Esthet. Restor. Dent. 2017, 29, 450–458. [Google Scholar] [CrossRef]
- Alghamdi, W.S.; Labban, N.; Maawadh, A.; Alsayed, H.D.; Alshehri, H.; Alrahlah, A.; Alnafaiy, S.M. Influence of Acidic Environment on the Hardness, Surface Roughness and Wear Ability of CAD/CAM Resin-Matrix Ceramics. Materials 2022, 15, 6146. [Google Scholar] [CrossRef] [PubMed]
- Kara, D.; Tekçe, N.; Fidan, S.; Demirci, M.; Tuncer, S.; Balcı, S. The Effects of Various Polishing Procedures on Surface Topography of CAD/CAM Resin Restoratives. J. Prosthodont. 2021, 30, 481–489. [Google Scholar] [CrossRef]
- Bai, Y.; Zhao, J.; Si, W.; Wang, X. Two-Body Wear Performance of Dental Colored Zirconia after Different Surface Treatments. J. Prosthet. Dent. 2016, 116, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Alhassan, M.; Maawadh, A.; Labban, N.; Alnafaiy, S.M.; Alotaibi, H.N.; BinMahfooz, A.M. Effect of Different Surface Treatments on the Surface Roughness and Gloss of Resin-Modified CAD/CAM Ceramics. Appl. Sci. 2022, 12, 11972. [Google Scholar] [CrossRef]
- Alharbi, N.; Teerakanok, S.; Satterthwaite, J.D.; Giordano, R.; Silikas, N. Quantitative Nano-Mechanical Mapping AFM-Based Method for Elastic Modulus and Surface Roughness Measurements of Model Polymer Infiltrated Ceramics. Dent. Mater. 2022, 38, 935–945. [Google Scholar] [CrossRef]
- Rashid, H. Evaluation of the Surface Roughness of a Standard Abraded Dental Porcelain Following Different Polishing Techniques. J. Dent. Sci. 2012, 7, 184–189. [Google Scholar] [CrossRef]
- Mei, L.; Busscher, H.J.; van der Mei, H.C.; Ren, Y. Influence of Surface Roughness on Streptococcal Adhesion Forces to Composite Resins. Dent. Mater. 2011, 27, 770–778. [Google Scholar] [CrossRef]
- Grangeiro, M.T.; Rodrigues, C.D.; Rossi, N.R.; da Silva, J.M.; Ramos, N.D.; Tribst, J.P.; Anami, L.C.; Bottino, M.A. Effect of Surface-Etching Treatment, Glaze, and the Antagonist on Roughness of a Hybrid Ceramic after Two-Body Wear. Materials 2022, 15, 6870. [Google Scholar] [CrossRef]
- Ereifej, N.S.; Oweis, Y.G.; Eliades, G. The Effect of Polishing Technique on 3-D Surface Roughness and Gloss of Dental Restorative Resin Composites. Oper. Dent. 2013, 38, E1–E12. [Google Scholar] [CrossRef]
| Material | Type | Composition | Filler Weight (w%) | |
|---|---|---|---|---|
| Inorganic Fillers/Structure | Main Resin Monomers | |||
| Grandio disc multicolor [Grandio] {VOCO GmbH, Cuxhaven, Germany} | Composite resin | Barium aluminium borosilicate glass, silicon dioxide | Not disclosed by the company | 86 |
| Shofu Block HC (two-layered block) [Shofu] {Shofu Inc., Kyoto, Japan} | Composite resin | Silica, fumed silica and zirconium silicate | UDMA, TEGDMA | 75 |
| Vita Enamic multiColor (Blocks) [Vita] {Vita Zahnfabrik, Bad Sackingen, Germany} | Resin-ceramic material (PICN) | Feldspar ceramic enriched with aluminium oxide (86 wt%): SiO2 (58–63%), Al2O3 (20–23%), Na2O (9–11%), K2O (4–6%), B2O3 (0.5–2%), ZrO2 (<1%), KaO (<1%) | UDMA + TEGDMA (14 wt%) | 86 |
| UTS (MPa) | FS (MPa) | Modulus of Elasticity (GPa) | ||||
|---|---|---|---|---|---|---|
| Block | Baseline | After Aging | Baseline | After Aging | Baseline | After Aging |
| Grandio disc multicolor | 164.5 ± 17.6 A,a | 159.6 ± 17.7 A,a | 324.7 ± 7.45 A,a | 342.4 ± 28.1 A,a | 16.3 ± 1.31 A,a | 16.9 ± 0.73 A,a |
| Shofu Block HC | 123.8 ± 16 A,b | 68.9 ± 17.9 B,c | 164.3 ± 9.72 A,b | 173.1 ± 4.90 A,b | 10.9 ± 0.99 A,b | 8.8 ± 0.60 B,b |
| Vita Enamic multiColor | 108.4 ± 15.6 A,b | 102.6 ±17.2 A,b | 161.1 ± 11.7 A,b | 165.1 ±10.6 A,b | 19.4 ± 1.54 A,a | 18.9 ±1.33 A,a |
| Block | Sorption (µg/mm3) |
|---|---|
| Grandio disc multicolor | 5.70 ± 0.68 a |
| Shofu Block HC | 22.8 ± 3.37 b |
| Vita Enamic multiColor | 5.44 ± 0.45 a |
| Block | Microhardness (KHN) | Softening Ratio | |
|---|---|---|---|
| Baseline | After Aging | ||
| Grandio disc multicolor | 163.1 ± 4.9 A,a | 153.8 ± 6.2 B,a | 5.6% |
| Shofu Block HC | 72.8 ± 2.2 A,b | 54.3 ± 3.3 B,b | 25.4% |
| Vita Enamic multiColor | 211.8 ± 4.5 A,c | 208.5 ± 6.4 A,c | 1.6% |
| Block | Ra (µm) | RSm (mm) | Rz Din (µm) | |||
|---|---|---|---|---|---|---|
| Baseline | After Aging | Baseline | After Aging | Baseline | After Aging | |
| Grandio disc multicolor | 0.077 ± 0.017 A,a | 0.086 ± 0.020 A,a | 0.053 ± 0.018 A,a | 0.059 ± 0.014 A,a | 0.769 ± 0.166 A,a | 0.786 ± 0.124 A,a |
| Shofu Block HC | 0.305 ± 0.059 A,b | 0.327 ± 0.060 B,b | 0.096 ± 0.033 A,b | 0.103 ± 0.032 B,b | 3.59 ± 0.464 A,b | 3.68 ± 0.636 A,b |
| Vita Enamic multiColor | 0.199 ± 0.031 A,c | 0.202 ± 0.027 A,c | 0.036 ± 0.003 A,c | 0.037 ± 0.004 A,c | 1.61 ± 0.221 A,c | 1.630 ± 0.223 A,c |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lukomska-Szymanska, M.; Radwanski, M.; Kharouf, N.; Mancino, D.; Tassery, H.; Caporossi, C.; Inchingolo, F.; de Almeida Neves, A.; Chou, Y.F.; Sauro, S. Evaluation of Physical–Chemical Properties of Contemporary CAD/CAM Materials with Chromatic Transition “Multicolor”. Materials 2023, 16, 4189. https://doi.org/10.3390/ma16114189
Lukomska-Szymanska M, Radwanski M, Kharouf N, Mancino D, Tassery H, Caporossi C, Inchingolo F, de Almeida Neves A, Chou YF, Sauro S. Evaluation of Physical–Chemical Properties of Contemporary CAD/CAM Materials with Chromatic Transition “Multicolor”. Materials. 2023; 16(11):4189. https://doi.org/10.3390/ma16114189
Chicago/Turabian StyleLukomska-Szymanska, Monika, Mateusz Radwanski, Naji Kharouf, Davide Mancino, Herve Tassery, Corrado Caporossi, Francesco Inchingolo, Aline de Almeida Neves, Yu Fu Chou, and Salvatore Sauro. 2023. "Evaluation of Physical–Chemical Properties of Contemporary CAD/CAM Materials with Chromatic Transition “Multicolor”" Materials 16, no. 11: 4189. https://doi.org/10.3390/ma16114189
APA StyleLukomska-Szymanska, M., Radwanski, M., Kharouf, N., Mancino, D., Tassery, H., Caporossi, C., Inchingolo, F., de Almeida Neves, A., Chou, Y. F., & Sauro, S. (2023). Evaluation of Physical–Chemical Properties of Contemporary CAD/CAM Materials with Chromatic Transition “Multicolor”. Materials, 16(11), 4189. https://doi.org/10.3390/ma16114189













