Improving the Hydrophobicity of Plasticized Polyvinyl Chloride for Use in an Endotracheal Tube
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
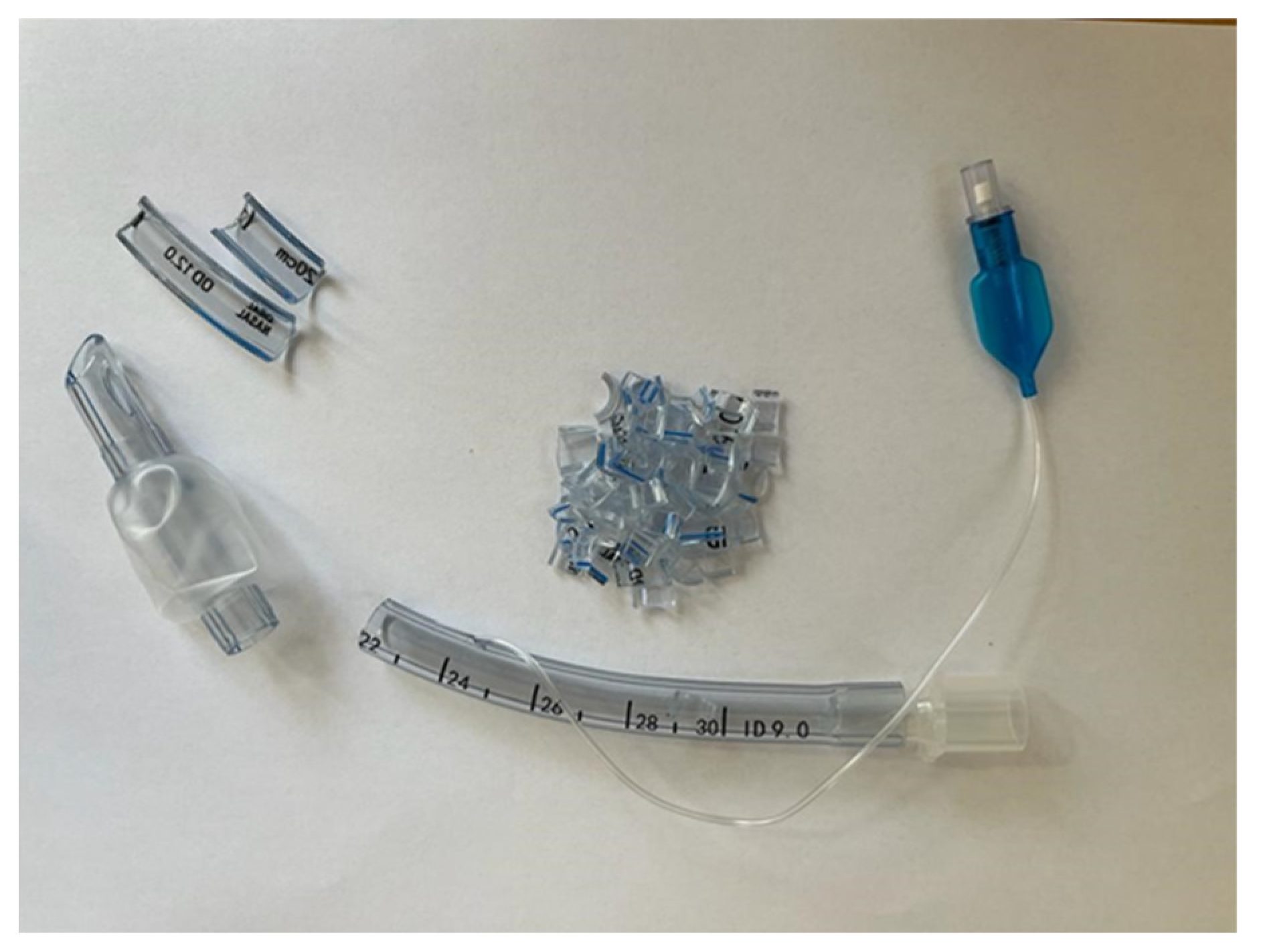
2.1.1. General Presentation of the Materials Used
2.1.2. PVC Sample Surface Treatment
Surface Fluorination by Plasma Treatment in SF6 Discharge
Magnetron Sputtering Physical Evaporation from the PTFE Target
2.2. Characterization Methods
2.2.1. The Chemical Structures of Samples ED0, ED1, and ED2
X-ray Photoelectron Spectroscopy (XPS)
Attenuated Total Reflection Fourier-Infrared (ATR-FTIR) Spectroscopy
2.2.2. Surface Analysis
Scanning Electron Microscopy (SEM) and Energy Dispersive X-ray Analysis (EDAX)
Contact Angle Measurements
Profilometry Analysis
2.2.3. Thermal Analysis
2.2.4. Material Density Measurement and Hardness Shore A Analyses
2.2.5. Antimicrobial and Cytotoxicity Analyses
Antimicrobial Tests
Cytotoxicity Analysis
3. Results and Discussion
3.1. Chemical Structure Analyses
3.1.1. X-ray Photoelectron Spectroscopy (XPS)
3.1.2. Attenuated Total Reflection Fourier-Infrared (ATR-FTIR) Spectroscopy
3.2. Surface Analysis
3.2.1. Scanning Electron Microscopy (SEM)
3.2.2. Contact Angle
3.2.3. Profilometry Analysis
3.3. Thermogravimetric Analysis (TGA) and Differential Scanning Calorimetry (DSC)
3.4. Mass Density and Hardness Shore A Measurements
3.5. Antimicrobial and Cytotoxicity Analyses
3.5.1. Antimicrobial Tests
3.5.2. Cytotoxicity Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Strömberg, E. Microbiological growth testing on silicone rubber materials. In Fibre and Polymer Technology; Royal Institute of Technology: Stockholm, Sweden, 2004. [Google Scholar]
- Lynch, J.F.; Lappin-Scott, H.M.; Costerton, J.W. Microbial Biofilms; Cambridge University Press: Cambridge, UK, 2003. [Google Scholar]
- Flemming, H.-C. Relevance of biofilms for the biodeterioration of surfaces of polymeric materials. Polym. Degrad. Stab. 1998, 59, 309–315. [Google Scholar] [CrossRef]
- Seal, K.J.; Morton, L.G.H. Chemical Materials; Schönborn, W., Ed.; VCH: Dusseldorf, Germany, 1986; pp. 583–606. [Google Scholar]
- Fleming, H.C.; Wingender, J. The biofilm matrix. Nat. Rev. Microbiol. 2010, 8, 623–633. [Google Scholar] [CrossRef]
- Lethongkam, S.; Daengngam, C.; Tansakul, C.; Siri, R.; Chumpraman, A.; Phengmak, M.; Voravuthikunchai, S.P. Prolonged inhibitory effects against planktonic growth, adherence, and biofilm formation of pathogens causing ventilator-associated pneumonia using a novel polyamide/silver nanoparticle composite-coated endotracheal tube. Biofouling 2020, 36, 292–307. [Google Scholar] [CrossRef] [PubMed]
- Bazak, K.; Jakob, M.V.; Crawford, R.J.; Ivanova, E.P. Efficient surface modification of biomaterial to prevent biofilm formation and the attachment of microorganisms. Appl. Microbiol. Biotechnol. 2012, 95, 299–311. [Google Scholar] [CrossRef]
- Duplantier, A.J.; van Hoek, M.L. The human cathelicidin antimicrobial peptide LL-37as a potential treatment for polymicrobial infected wounds. Front Immunol. 2013, 4, 1–14. [Google Scholar] [CrossRef]
- Vandencasteele, N.; Nisol, B.; Viville, P.; Lazzaroni, R.; Castner, D.G.; Reniers, F. Plasma-Modified PTFE for Biological Applications: Correlation between Protein-Resistant Properties and Surface Characteristics. Plasma Processes Polym. 2008, 5, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Jafari, R.; Asadollahi, S.; Farzaneh, M. Applications of plasma technology in development of superhydrophobic surfaces. Plasma Chem. Plasma Process. 2013, 33, 177–200. [Google Scholar] [CrossRef]
- Mohammadi Hashemi, M. Antibacterial and Antifungal Activity of Ceragenins, Mimics of Endogenous Antimicrobial Peptides. Ph.D. Thesis, Brigham Young University, Provo, UT, USA, 2019; p. 7411. [Google Scholar]
- Guan, Q.; Li, C.; Schmidt, E.J.; Boswell, J.S.; Walsh, J.P.; Allman, G.W.; Savage, P.B. Preparation and Characterization of Cholic Acid-Derived Antimicrobial Agents with Controlled Stabilities. Org. Lett. 2000, 2, 2837–2840. [Google Scholar] [CrossRef]
- Savage, P.B.; Li, C. Cholic acid derivatives: Novel antimicrobials. Expert Opin. Investig. Drugs 2000, 9, 263–272. [Google Scholar] [CrossRef]
- Li, C.; Lewis, M.R.; Gilbert, A.B.; Noel, M.D.; Scoville, D.H.; Allman, G.W.; Savage, P.B. Antimicrobial Activities of Amine- and Guanidine-Functionalized Cholic Acid Derivatives. Antimicrob. Agents Chemother. 1999, 43, 1347–1349. [Google Scholar] [CrossRef]
- Surel, U.; Niemirowicz, K.; Marzec, M.; Savage, P.B.; Bucki, R. Ceragenins–a new weapon to fight multidrug resistant bacterial infections. Stud. Med. 2014, 30, 207–213. [Google Scholar] [CrossRef]
- Schmidt, E.J.; Boswell, J.S.; Walsh, J.P.; Schellenberg, M.M.; Winter, T.W.; Li, C.; Allman, G.W.; Savage, P.B. Activities of cholic acid-derived antimicrobial agents against multidrug-resistant bacteria. J. Antimicrob. Chemother. 2001, 47, 671–674. [Google Scholar] [CrossRef] [PubMed]
- Wnorowska, U.; Niemirowicz, K.; Myint, M.; Diamond, S.L.; Wróblewska, M.; Savage, P.B.; Janmey, P.A.; Bucki, R. Bactericidal Activities of Cathelicidin LL-37 and Select Cationic Lipids against the Hypervirulent Pseudomonas aeruginosa Strain LESB58. Antimicrob. Agents Chemother. 2015, 59, 3808–3815. [Google Scholar] [CrossRef]
- Chin, J.N.; Jones, R.N.; Sader, H.S.; Savage, P.B.; Rybak, M.J. Potential synergy activity of the novel ceragenin, CSA-13, against clinical isolates of Pseudomonas aeruginosa, including multidrug-resistant P. aeruginosa. J. Antimicrob. Chemother. 2008, 61, 365–370. [Google Scholar] [CrossRef]
- Hashemi, M.M.; Holden, B.S.; DurnaAA, B.; Buck, R.; Savage, P.B. Ceragenins as Mimics of Endogenous Antimicrobial Peptides. J. Antimicrob. Agents 2017, 3, 2. [Google Scholar] [CrossRef]
- Mitchell, G.; Silvis, M.R.; Talkington, K.C.; Budzik, J.M.; Dodd, C.E.; Paluba, J.M.; Oki, E.A.; Trotta, K.L.; Licht, D.J.; Jimenez-Morales, D.; et al. Ceragenins and Antimicrobial Peptides Kill Bacteria through Distinct Mechanisms. Mbio 2022, 13, e0272621. [Google Scholar] [CrossRef]
- Bahar, A.A.; Ren, D. Antimicrobial Peptides. Pharmaceuticals 2013, 6, 1543–1575. [Google Scholar] [CrossRef]
- Durnaś, B.; Wnorowska, U.; Pogoda, K.; Deptuła, P.; Wątek, M.; Piktel, E.; Głuszek, S.; Gu, X.; Savage, P.B.; Niemirowicz, K.; et al. Candidacidal Activity of Selected Ceragenins and Human Cathelicidin LL-37 in Experimental Settings Mimicking Infection Sites. PLoS ONE 2016, 11, e0157242. [Google Scholar] [CrossRef]
- Hashemi, M.M.; Rovig, J.; Bateman, J.; Holden, B.S.; Modelzelewski, T.; Gueorguieva, I.; von Dyck, M.; Bracken, R.; Genberg, C.; Deng, S.; et al. Preclinical testing of a broad-spectrum antimicrobial endotracheal tube coated with an innate immune synthetic mimic. J. Antimicrob. Chemother. 2018, 73, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Satulu, V.; Ionita, M.D.; Vizireanu, S.; Mitu, B.; Dinescu, G. Plasma Processing with Fluorine Chemistry for Modification of Surfaces Wettability. Molecules 2016, 21, 1711. [Google Scholar] [CrossRef]
- Nagant, C.; Pitts, B.; Stewart, P.S.; Feng, Y.; Savage, P.B.; Dehaye, J.-P. Study of the effect of antimicrobial peptide mimic, CSA-13, on an established biofilm formed by Pseudomonas aeruginosa. Microbiologyopen 2013, 2, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Oyardi, O.; Eltimur, T.; Demir, E.S.; Alkan, B.; Savage, P.B.; Akcali, A.; Bozkurt-Guzel, C. Antibacterial and Antibiofilm Activities of Ceragenins Alone and in Combination with Levofloxacin Against Multidrug Resistant Myroides spp. Clinical Isolates from Patients with Urinary Tract Infections. Curr. Microbiol. 2023, 80, 210. [Google Scholar] [CrossRef]
- Piktel, E.; Pogoda, K.; Roman, M.; Niemirowicz, K.; Tokajuk, G.; Wróblewska, M.; Szynaka, B.; Kwiatek, W.M.; Savage, P.B.; Bucki, R. Sporicidal activity of ceragenin CSA-13 against Bacillus subtilis. Sci. Rep. 2017, 7, srep44452. [Google Scholar] [CrossRef]
- Yasin, B.; Wang, W.; Pang, M.; Cheshenko, N.; Hong, T.; Waring, A.J.; Herold, B.C.; Wagar, E.A.; Lehrer, R.I. θ Defensins Protect Cells from Infection by Herpes Simplex Virus by Inhibiting Viral Adhesion and Entry. J. Virol. 2004, 78, 5147–5156. [Google Scholar] [CrossRef]
- Howell, M.D.; Streib, J.E.; Kim, B.E.; Lesley, L.J.; Dunlap, A.P.; Geng, D.; Feng, Y.; Savage, P.B.; Leung, D.Y. Ceragenins: A Class of Antiviral Compounds to Treat Orthopox Infections. J. Investig. Dermatol. 2009, 129, 2668–2675. [Google Scholar] [CrossRef] [PubMed]
- Zasloff, M. Magainins, a class of antimicrobial peptides from Xenopus skin: Isolation, characterization of two active forms, and partial cDNA sequence of a precursor. Proc. Natl. Acad. Sci. USA 1987, 84, 5449–5453. [Google Scholar] [CrossRef]
- Park, Y.; Jang, S.H.; Lee, D.G.; Hahm, K.S. Antinematodal effect of antimicrobial peptide, PMAP-23, isolated from porcine myeloid against Caenorhabditis elegans. J. Pept. Sci. 2004, 10, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Lara, D.; Feng, Y.; Bader, J.; Savage, P.B.; Maldonado, R.A. Anti-Trypanosomatid Activity of Ceragenins. J. Parasitol. 2010, 96, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Niemirowicz, K.; Durnaś, B.; Tokajuk, G.; Piktel, E.; Michalak, G.; Gu, X.; Kułakowska, A.; Savage, P.B.; Bucki, R. Formulation and candidacidal activity of magnetic nanoparticles coated with cathelicidin LL-37 and ceragenin CSA-13. Sci. Rep. 2017, 7, 1–12. [Google Scholar] [CrossRef]
- Durnaś, B.; Piktel, E.; Wątek, M.; Wollny, T.; Góźdź, S.; Smok-Kalwat, J.; Niemirowicz, K.; Savage, P.B.; Bucki, R. Anaerobic bacteria growth in the presence of cathelicidin LL-37 and selected ceragenins delivered as magnetic nanoparticles cargo. BMC Microbiol. 2017, 17, 167. [Google Scholar] [CrossRef]
- Zanini, S.; Grimoldi, E.; Riccardi, C. Development of controlled releasing surfaces by plasma deposited multilayers. Mater. Chem. Phys. 2013, 138, 850–855. [Google Scholar] [CrossRef]
- Annamalai, M.; Gopinadhan, K.; Han, S.A.; Saha, S.; Park, H.J.; Cho, E.B.; Kumar, B.; Patra, A.; Kim, S.-W.; Venkatesan, T. Surface energy and wettability of van der Waals structures. Nanoscale 2016, 8, 5764–5770. [Google Scholar] [CrossRef]
- Pugmire, D.L.; Wetteland, C.J.; Duncan, W.S.; Lakis, R.E.; Schwartz, D.S. Cross-linking of polytetrafluoroethylene during room-temperature irradiation. Polym. Degrad. Stab. 2009, 94, 1533–1541. [Google Scholar] [CrossRef]
- Kravets, L.I.; Yablokov MY Gilman, A.B.; Shchegolikhin AN Mitu, B.; Dinescu, G. Micro-and Nanofluidic Diodes Based on Track-Etched Poly(EthyleneTerephthalate) Membrane. High Energ. Chem. 2015, 49, 367–374. [Google Scholar] [CrossRef]
- Vizireanu, S.; Ionita, M.D.; Dinescu, G.; Enculescu, I.; Baibarac, M.; Baltog, I. Post-synthesis Carbon Nanowalls Transformation under Hydrogen, Oxygen, Nitrogen, Tetrafluoroethane and Sulfur Hexafluoride Plasma Treatments. Plasma Process. Polym. 2012, 9, 363–370. [Google Scholar] [CrossRef]
- Resnik, M.; Zaplotnik, R.; Mozetic, M.; Vesel, A. Comparison of SF6 and CF4 Plasma Treatment for Surface Hydrophobization of PET Polymer. Materials 2018, 11, 311. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Wang, X.; Jia, H.; Zhou, Y.; Ma, J.; Liu, X.; Jiang, L.; Chen, S. Superhydrophobic Polytetrafluoroethylene/Heat-Shrinkable Polyvinyl Chloride Composite Film with Super Anti-Icing Property. Polymers 2019, 11, 805. [Google Scholar] [CrossRef]
- Eswaramoorthy, N.; McKenzie, D.R. Plasma treatments of dressings for wound healing: A review. Biophys. Rev. 2017, 9, 895–917. [Google Scholar] [CrossRef] [PubMed]
- Dowling, D.P. Surface processing using cold atmospheric pressure plasmas. In Comprehensive Materials Processing; Cameron, D., Ed.; Elsevier: Oxford, UK, 2014; Volume 4, pp. 171–185. [Google Scholar] [CrossRef]
- Chaivan, P.; Pasaja, N.; Boonyawan, D.; Suanpoot, P.; Vilaithong, T. Low-temperature plasma treatment for hydrophobicity improvement of silk. Surf. Coat Technol. 2005, 193, 356–360. [Google Scholar] [CrossRef]
- Nanchang Kaimed Medical Apparatus Co., Ltd. Available online: http://www.kaimed.com/ (accessed on 1 July 2023).
- COUNCIL DIRECTIVE 93/42/EEC of 14 June 1993 Concerning Medical Devices (OJ L 169, 12.7.1993, p. 1). Available online: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CONSLEG:1993L0042:20071011:en:PDF (accessed on 4 October 2023).
- Bormashenko, E.; Legchenkova, I.; Navon-Venezia, S.; Frenkel, M.; Bormashenko, Y. Investigation of the Impact of Cold Plasma Treatment on the Chemical Composition and Wettability of Medical Grade Polyvinylchloride. Appl. Sci. 2020, 11, 300. [Google Scholar] [CrossRef]
- ISO 21920-2:2021; Geometrical Product Specifications (GPS), Surface Texture: Profile, Part 2: Terms, Definitions and Surface Texture Parameters. ISO: Geneva, Switzerland, 2021.
- Pocius, A.V. Adhesion and Adhesives Technology: An Introduction, 3rd ed.; Carl Hanser Verlag GmbH & Co. KG: München, Germany, 2012; ISBN 978-3-446-42748-8. [Google Scholar]
- Plastics and Ebonite—Determination of Indentation Hardness by Means of a Durometer (Shore Hardness) ISO 868:2003. Available online: https://www.iso.org/standard/34804.html (accessed on 1 July 2023).
- Humphries, R.M.; Ambler, J.; Mitchell, S.L.; Castanheira, M.; Dingle, T.; Hindler, J.A.; Koeth, L.; Sei, K. CLSI Methods Development and Standardization Working Group best practices for evaluation of antimicrobial susceptibility tests. J. Clin. Microbiol. 2018, 56, e01934-17. [Google Scholar] [CrossRef] [PubMed]
- Sathiyamoorthy, J.; Sudhakar, N. In vitro Cytotoxicity and Apoptotic Assay in HT-29 Cell Line Using Ficus hispida Linn: Leaves Extract. Pharmacogn. Mag. 2018, 13 (Suppl. 4), S756–S761. [Google Scholar] [CrossRef] [PubMed]
- Tserepi, A.D.; Vlachopoulou, M.-E.; Gogolides, E. Nanotexturing of poly(dimethylsiloxane) in plasmas for creating robust super-hydrophobic surfaces. Nanotechnology 2006, 17, 3977–3983. [Google Scholar] [CrossRef]
- Barni, R.; Zanini, S.; Beretta, D.; Riccardi, C. Experimental study of hydrophobic/hydrophilic transition in SF6plasma interaction with polymer surfaces. Eur. Phys. J. Appl. Phys. 2007, 38, 263–268. [Google Scholar] [CrossRef]
- Sant’ana, P.L.; Bortoleto, J.R.R.; da Cruz, N.C.; Rangel, E.C.; Durrant, S.F.; Schreiner, W.H. Surface functionalization of polyvinyl chloride by plasma immersion techniques. Polímeros 2020, 30. [Google Scholar] [CrossRef]
- Krimm, S. Infrared Spectra of High Polymers. Adv. Polym. Sci. 1960, 2, 51–172. [Google Scholar]
- Liang, C.Y.; Krimm, S. Infrared Spectra of High Polymers. III. Polytetrafluoroethylene and Polychlorotrifluoroethylene. J. Chem. Phys. 1956, 25, 563–571. [Google Scholar] [CrossRef]
- Lappan, U.; Gei, U.; Lunkwitz, K. Electron beam irradiation of polytetrafluoroethylene in vacuum at elevated temperature: An infrared spectroscopic study. J. Appl. Polym. Sci. 1999, 74, 1571. [Google Scholar] [CrossRef]
- Lappan, U.; Gei, U.; Häu, L.; Jehnichen, D.; Pompe, G.; Lunkwitz, K. Polymers and Electromagnetic Radiation. Nucl. Instr. Meth. Phys. Res. B 2001, 185, 178. [Google Scholar] [CrossRef]
- Piwowarczyk, J.; Jędrzejewski, R.; Moszyński, D.; Kwiatkowski, K.; Niemczyk, A.; Baranowska, J. XPS and FTIR Studies of Polytetrafluoroethylene Thin Films Obtained by Physical Methods. Polymers 2019, 11, 1629. [Google Scholar] [CrossRef]
- Takeuchi, M.; Kinoshita, A.; Yamaguchi, A.; Utsumi, Y. Molecular Structure Evaluation of Bulk Polytetrafluoroethylene Modified by X-ray Irradiation. J. Photopolym. Sci. Technol. 2020, 33, 295–299. [Google Scholar] [CrossRef]
- Zanini, S.; Bami, R.; Della Pergola, R.; Riccardi, C. Development of super-hydrophobic PTFE and PET surfaces by means of plasma processes. J. Phys. Conf. Ser. 2014, 550, 012029. [Google Scholar] [CrossRef]
- Janík, R.; Kohutiar, M.; Dubec, A.; Eckert, M.; Moricová, K.; Pajtášová, M.; Ondrušová, D.; Krbata, M. DMA Analysis of Plasma Modified PVC Films and the Nature of Initiated Surface Changes. Materials 2022, 15, 4658. [Google Scholar] [CrossRef] [PubMed]
- Belinger, A.; Naudé, N.; Gherardi, N. Transition from diffuse to self-organized discharge in a high frequency dielectric barrier discharge. Eur. Phys. J. Appl. Phys. 2017, 79, 10802. [Google Scholar] [CrossRef]
- Khorasani, M.; Mirzadeh, H. Effect of oxygen plasma treatment on surface charge and wettability of PVC blood bag—In vitro assay. Radiat. Phys. Chem. 2007, 76, 1011–1016. [Google Scholar] [CrossRef]
- Cheng, Y.H.; Lin, T.L.; Pan, Y.J.; Wang, Y.P.; Lin, Y.T.; Wang, J.T. Colistin resistance mechanisms in Klebsiella pneumoniae strains from Taiwan. Antimicrob. Agents Chemother. 2015, 59, 2909–2913. [Google Scholar] [CrossRef]
- View of Comparative Scanning Electron Microscope Study of the Degradation of a Plasticized Polyvinyl Chloride Waterproofing Membrane in Different Conditions|Materiales de Construcción. Available online: https://materconstrucc.revistas.csic.es/index.php/materconstrucc/article/view/2163/2675 (accessed on 2 July 2023).
- Babukutty, Y.; Prat, R.; Endo, K.; Kogoma, M.; Okazaki, S.; Kodama, M. Poly(vinyl chloride) Surface Modification Using Tetrafluoroethylene in Atmospheric Pressure Glow Discharge. Langmuir 1999, 15, 7055–7062. [Google Scholar] [CrossRef]
- Mrad, O.; Saloum, S.; Al-Mariri, A. Effect of a new low pressure SF6 plasma sterilization system on polymeric devices. Vacuum 2013, 88, 11–16. [Google Scholar] [CrossRef]
- Gengenbach, T.R.; Xie, X.; Chatelier, R.C.; Griesser, H.J. Evolution of the surface composition and topography of perfluorinated polymers following ammonia-plasma treatment. J. Adhes. Sci. Technol. 1994, 8, 305–328. [Google Scholar] [CrossRef]
- Gengenbach, T.R.; Vasic, Z.R.; Li, S.; Chatelier, R.C.; Griesser, H.J. Contributions of restructuring and oxidation to the aging of the surface of plasma polymers containing heteroatoms. Plasmas Polym. 1997, 2, 91–114. [Google Scholar] [CrossRef]
- Guarrotxena, N.; Schue, F.; Collet, A.; Millán, J.-L. On the stereochemical composition of poly(vinyl chloride) (PVC) and polypropylene (PP): A phenomenological study. Polym. Int. 2003, 52, 420–428. [Google Scholar] [CrossRef]
- Mijangos, C.; Calafel, I.; Santamaría, A. Poly(vinyl chloride), a historical polymer still evolving. Polymer 2023, 266, 125610. [Google Scholar] [CrossRef]
- Tomaszewska, J.; Sterzyński, T.; Woźniak-Braszak, A.; Banaszak, M. Review of Recent Developments of Glass Transition in PVC Nanocomposites. Polymers 2021, 13, 4336. [Google Scholar] [CrossRef] [PubMed]
- Kendall, M.J.; Siviour, C.R. Rate dependence of poly(vinyl chloride), the effects of plasticizer and time–temperature superposition. Proc. R. Soc. A Math. Phys. Eng. Sci. 2014, 470, 20140012. [Google Scholar] [CrossRef]
- Czogała, J.; Pankalla, E.; Turczyn, R. Recent Attempts in the Design of Efficient PVC Plasticizers with Reduced Migration. Materials 2021, 14, 844. [Google Scholar] [CrossRef]
- Gama, N.; Santos, R.; Godinho, B.; Silva, R.; Ferreira, A. Triacetin as a Secondary PVC Plasticizer. J. Polym. Environ. 2019, 27, 1294–1301. [Google Scholar] [CrossRef]
- Amankwah, S.; Adisu, M.; Gorems, K.; Abdella, K.; Kassa, T. Assessment of Phage-Mediated Inhibition and Removal of Multidrug-Resistant Pseudomonas aeruginosa Biofilm on Medical Implants. Infect. Drug Resist. 2022, 15, 2797–2811. [Google Scholar] [CrossRef]
- Rimondini, L.; Cochis, A.; Varoni, E.; Azzimonti, B.; Carrassi, A. Biofilm Formation on Implants and Prosthetic Dental Materials. In Handbook of Bioceramics and Biocomposites; Antoniac, I.V., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 991–1027. ISBN 978-3-319-12460-5. [Google Scholar]
- Khatoon, Z.; McTiernan, C.D.; Suuronen, E.J.; Mah, T.-F.; Alarcon, E.I. Bacterial biofilm formation on implantable devices and approaches to its treatment and prevention. Heliyon 2018, 4, e01067. [Google Scholar] [CrossRef]
- Achinas, S.; Charalampogiannis, N.; Euverink, G.J.W. A Brief Recap of Microbial Adhesion and Biofilms. Appl. Sci. 2019, 9, 2801. [Google Scholar] [CrossRef]
- Chen, H.; Zhou, X.; Ren, B.; Cheng, L. The regulation of hyphae growth in Candida albicans. Virulence 2020, 11, 337–348. [Google Scholar] [CrossRef]
- Salari, R.; Salari, R. Investigation of the Best Saccharomyces cerevisiae Growth Condition. Electron. Physician 2017, 9, 3592–3597. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, I.D.; Wilson, D.; Wächtler, B.; Brunke, S.; Naglik, J.R.; Hube, B. Candida albicans dimorphism as a therapeutic target. Expert Rev. Anti-Infect. Ther. 2012, 10, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Rai, L.S.; Wijlick, L.V.; Bougnoux, M.-E.; Bachellier-Bassi, S.; d’Enfert, C. Regulators of Commensal and Pathogenic Life-Styles of an Opportunistic Fungus-Candida Albicans. Yeast 2021, 38, 243–250. [Google Scholar] [CrossRef] [PubMed]
















| Element | Atomic Composition (%) | ||
|---|---|---|---|
| ED0 | ED1 | ED2 | |
| C1s | 77.8 | 58.9 | 69.8 |
| O1s | 13.7 | 12.9 | 11.4 |
| Cl2p | 5.4 | 0.3 | - |
| Si2p | 2.8 | 2.7 | - |
| F1s | - | 23.1 | 11.9 |
| N1s | - | 1.7 | - |
| I3d | - | - | 3.0 |
| Zn2p3 | - | - | 3.7 |
| Glass Transition | Relaxation Enthalpy | Melting Enthalpy | R750 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ton | Tg | ΔCp | Ton | Tmax | ΔHm | Ton | Tmax | ΔHm | N2 | Air | |
| °C | °C | J/(g °C) | °C | °C | J/g | °C | °C | J/g | % | % | |
| ED0, 1st heating | −35.9 | −15.1 | 0.25 | – | – | – | 48.4 | 66.2 | 1.81 | 1.85 | 0.01 |
| ED0, cooling | 7.8 | −15.0 | 0.31 | - | - | - | - | - | - | ||
| ED0, 2nd heating | −33.7 | −6.7 | 0.32 | - | - | - | - | - | - | ||
| ED1, 1st heating | −38.8 | −19.9 | 0.25 | 116.1 | 121.8 | 0.57 | 50.4 | 67.4 | 1.73 | 2.41 | 0.01 |
| ED1, cooling | 9.8 | −9.3 | 0.34 | 79.0 | 73.8 | 0.61 | - | - | - | ||
| ED1, 2nd heating | −36.0 | −13.0 | 0.31 | - | - | - | 113.4 | 120.4 | 0.70 | ||
| ED2, 1st heating | −39.1 | −19.2 | 0.24 | 115.9 | 121.7 | 0.58 | 51.3 | 67.5 | 1.93 | 3.98 | 0.02 |
| ED2, cooling | 8.1 | −20.8 | 0.33 | 79.0 | 73.8 | 0.59 | |||||
| ED2, 2nd heating | −35.7 | −11.3 | 0.30 | - | - | - | 113.4 | 120.4 | 0.73 | ||
| Sample | Density (g/cm3) | Hardness Shore (°Sh A) |
|---|---|---|
| ED0 | 1.23 | 83 |
| ED1 | 1.21 | 81 |
| ED2 | 1.21 | 79 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcut, L.; Mohan, A.G.; Corneschi, I.; Grosu, E.; Paltanea, G.; Avram, I.; Badaluta, A.V.; Vasilievici, G.; Nicolae, C.-A.; Ditu, L.M. Improving the Hydrophobicity of Plasticized Polyvinyl Chloride for Use in an Endotracheal Tube. Materials 2023, 16, 7089. https://doi.org/10.3390/ma16227089
Marcut L, Mohan AG, Corneschi I, Grosu E, Paltanea G, Avram I, Badaluta AV, Vasilievici G, Nicolae C-A, Ditu LM. Improving the Hydrophobicity of Plasticized Polyvinyl Chloride for Use in an Endotracheal Tube. Materials. 2023; 16(22):7089. https://doi.org/10.3390/ma16227089
Chicago/Turabian StyleMarcut, Lavinia, Aurel George Mohan, Iuliana Corneschi, Elena Grosu, Gheorghe Paltanea, Ionela Avram, Alexandra Valentina Badaluta, Gabriel Vasilievici, Cristian-Andi Nicolae, and Lia Mara Ditu. 2023. "Improving the Hydrophobicity of Plasticized Polyvinyl Chloride for Use in an Endotracheal Tube" Materials 16, no. 22: 7089. https://doi.org/10.3390/ma16227089






