In Vitro Analysis of the Removability of Fractured Prosthetic Screws within Endosseous Implants Using Conventional and Mechanical Techniques
Abstract
:1. Introduction
2. Materials and Method
2.1. Study Design
2.2. Methodological Procedure
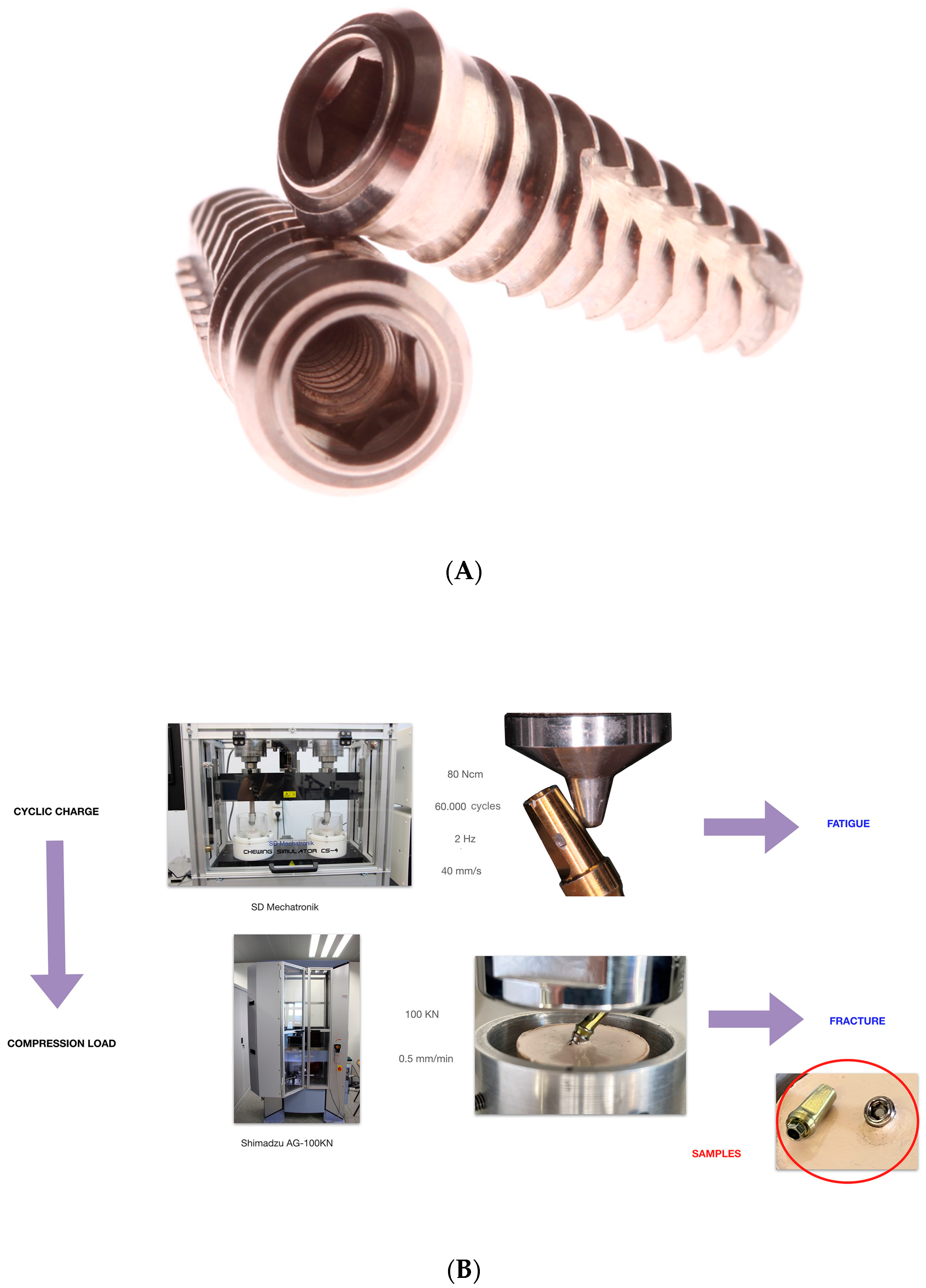
2.2.1. Mechanical Cycling Fatigue and Compression Load Workflow
2.2.2. Static Load
2.2.3. Conventional Removal Technique
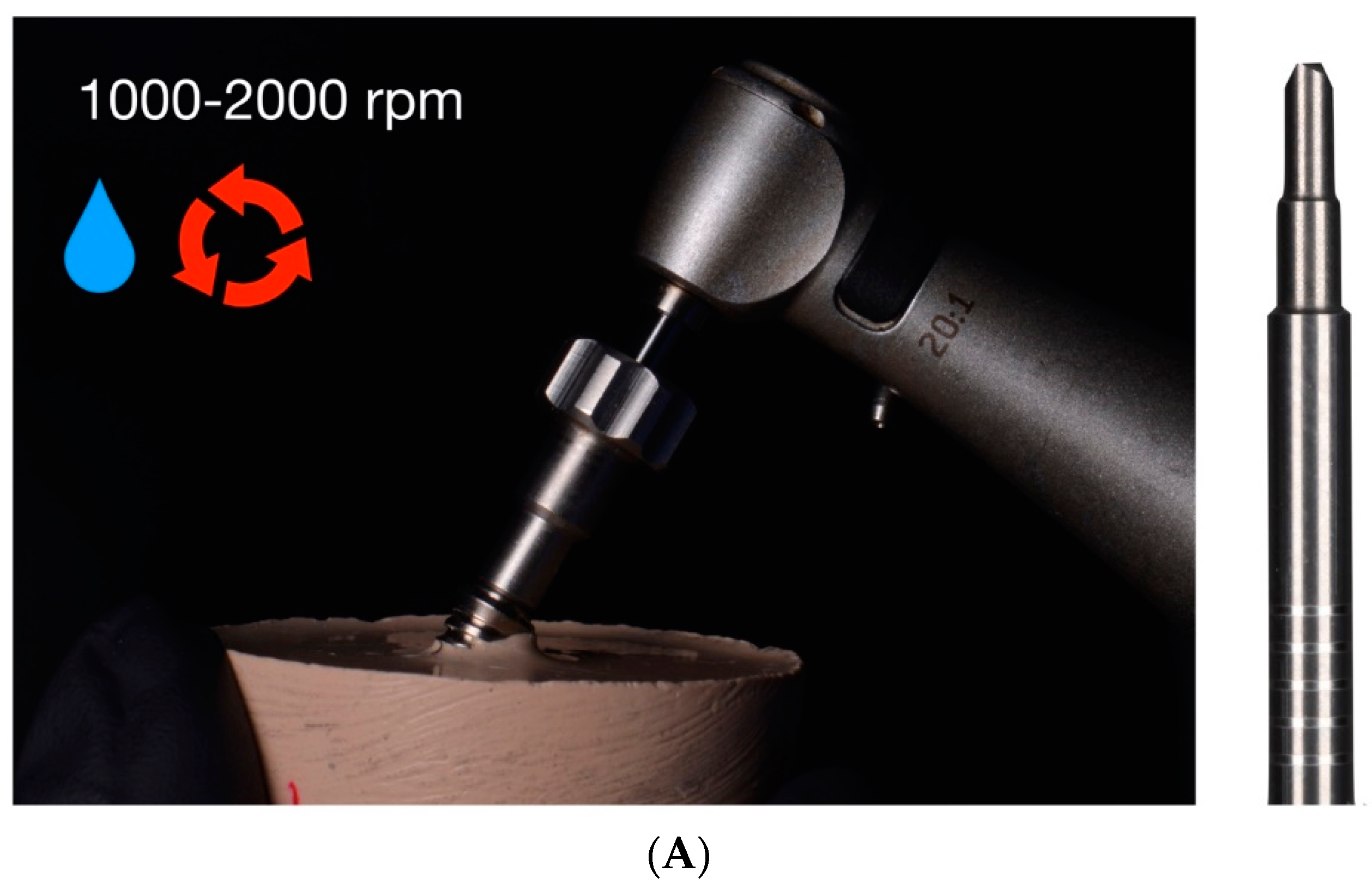
2.2.4. Drilling Removal Technique Using Rhein83® System
2.2.5. Drilling Removal Technique Using Sanhigia® System
2.2.6. Drilling Removal Technique Using Phibo® System
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zabalegui, I. Influencia de la ubicación de los implantes sobre la restauración definitiva. RCOE 2002, 7, 47–54. [Google Scholar]
- Agustín, R.; Faus, J.; Laguna, M. Complicaciones derivadas de una incorrecta planificación quirúrgico-protésica en implantología oral. Rev. Int. Prótesis Estomatol. 2012, 14, 107–113. [Google Scholar]
- Stuart, J. Dental Implant Complications: Etiology, Prevention and Treatment, 2nd ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2016. [Google Scholar]
- Kourtis, S.; Damanaki, M.; Kaitatzidou, A.; Roussou, V. Loosening of the fixing screw in single implant crowns: Predisposing factors, prevention and treatment options. J. Esthet. Restor. Dent. 2017, 29, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Ferreiroa, A.; Peñarrocha-Diago, M.; Pradíes, G.; Sola-Ruiz, M.F.; Agustín-Panadero, R. Cemented and screw-retained implant-supported single-tooth restorations in the molar mandibular region: A retrospective comparison study after an observation period of 1 to 4 years. J. Clin. Exp. Dent. 2015, 7, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.G.; Millen, C.; Brägger, U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions—A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 84–98. [Google Scholar] [CrossRef] [PubMed]
- Tsuruta, K.; Ayukawa, Y.; Matsuzaki, T.; Kihara, M.; Koyano, K. The influence of implant-abutment connection on the screw loosening and microleakage. Int. J. Implant. Dent. 2018, 4, 11. [Google Scholar] [CrossRef] [PubMed]
- Vanlıoğlu, B.; Özkan, Y.; Kulak-Özkan, Y. Retrospective analysis of prosthetic complications of implant-supported fixed partial dentures after an observation period of 5 to 10 years. Int. J. Oral Maxillofac. Implants 2013, 28, 300–304. [Google Scholar]
- Papaspyridakos, P.; Chen, C.J.; Chuang, S.K.; Weber, H.P.; Gallucci, G.O. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int. J. Oral Maxillofac. Implants 2012, 27, 102–110. [Google Scholar]
- Katsavochristou, A.; Koumoulis, D. Incidence of abutment screw failure of single or splinted implant prostheses: A review and update on current clinical status. J. Oral Rehabil. 2019, 46, 776–786. [Google Scholar] [CrossRef]
- Cervino, G.; Germanà, A.; Fiorillo, L.; D’Amico, C.; Abbate, F.; Cicciù, M. Passant Connection Screw of Dental Implants: An In Vitro SEM Preliminary Study. Biomed. Res. Int. 2022, 2022, 9720488. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Labaig-Rueda, C.; Castillo-Rodriguez, B.; Ferreiroa, A.; Solá-Ruíz, M.F. In Vitro Evaluation of Three Methods for the Retrieval of Fractured Screw Fragments from Dental Implants. Int. J. Oral Maxillofac. Implants 2017, 32, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Williamson, R.T.; Robinson, F.G. Retrieval technique for fractured implant screws. J. Prosthet. Dent. 2001, 86, 549–550. [Google Scholar] [CrossRef] [PubMed]
- Nergiz, I.; Schmage, P.; Shahin, R. Removal of a fractured implant abutment screw: A clinical report. J. Prosthet. Dent. 2004, 91, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Agustín-Panadero, R.; Baixauli-López, M.; Gómez-Polo, M.; Cabanes-Gumbau, G.; Senent-Vicente, G.; Roig-Vanaclocha, A. In Vitro comparison of the efficacy of two fractured implant-prosthesis screw extraction methods: Conventional versus mechanical. J. Prosthet. Dent. 2020, 124, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Brisman, D.L. The effect of speed, pressure, and time on bone temperature during the drilling of implant sites. Int. J. Oral Maxillofac. Implants 1996, 11, 35–37. [Google Scholar] [PubMed]
- Ercoli, C.; Funkenbusch, P.D.; Lee, H.J.; Moss, M.E.; Graser, G.N. The influence of drill wear on cutting efficiency and heat production during osteotomy preparation for dental implants: A study of drill durability. Int. J. Oral Maxillofac. Implants 2004, 19, 335–349. [Google Scholar]
- Nayana, P.; Nayak, S.S.; Chatterjee, A.; Sivaraman, K.; Srikanth, G.; Singh, C. Retrieval of Fractured Implant Abutment Screws: A Narrative Review. J. Int. Soc. Prev. Community. Dent. 2022, 12, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Raju, S.; Nair, V.V.; Karunakaran, H.K.; Manjuran, N.G. Management of perishing implants with abutment screw fracture—A systematic review. J. Indian. Prosthodont. Soc. 2021, 21, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, A.; Aljudaibi, S.; Donnelly-Swift, E.; Polyzois, I.; Grufferty, B. An in vitro evaluation of 2 methods for retrieving fractured abutment screw fragments from the intaglio of 4 different implant systems. J. Prosthet. Dent. 2022, 9, S0022-3913(22)00466-8. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, J.; Lee, T.; Phark, J.H.; Chee, W. Removal torque and force to failure of non-axially tightened implant abutment screws. J. Prosthet. Dent. 2019, 121, 322–326. [Google Scholar] [CrossRef]
- ISO 14801:2016; Dentistry. Implants. Dynamic Loading Test for Endosseous Dental Implants. ISO: Geneva, Switzerland, 2016.
- Sim, B.K.; Kim, B.; Kim, M.J.; Jeong, G.H.; Ju, K.W.; Shin, Y.J.; Kim, M.Y.; Lee, J.H. Hollow Abutment Screw Design for Easy Retrieval in Case of Screw Fracture in Dental Implant System. J. Healthc. Eng. 2017, 2017, 4842072. [Google Scholar] [CrossRef] [PubMed]
- Quek, C.E.; Tan, K.B.; Nicholls, J.I. Load fatigue performance of a single-tooth implant abutment system: Effect of diameter. Int. J. Oral Maxillofac. Implants 2006, 21, 929–936. [Google Scholar] [PubMed]
- Gehrke, P.; Dhom, G.; Brunner, J.; Wolf, D.; Dwdigi, M.; Piatelli, A. Zirconium implant abutments: Fracture strength and influence of cycling loading on retaining-screw loosening. Quintessence Int. 2006, 37, 19–26. [Google Scholar] [PubMed]
- Oderich, E.; Boff, L.L.; Cardoso, A.C.; Magne, P. Fatigue resistance and failure mode of adhesively restored custom implant zirconia abutments. Clin. Oral Implants Res. 2012, 23, 1360–1368. [Google Scholar] [CrossRef] [PubMed]
- Stimmelmayr, M.; Sagerer, S.; Erdelt, K.; Beuer, F. In Vitro fatigue and fracture strength testing of one piece zirconia implant abutments and zirconia implant abutments connected to titanium cores. Int. J. Oral Maxillofac. Implants 2013, 28, 488–493. [Google Scholar] [CrossRef]
- Kim, S.; Kim, H.I.; Brewer, J.D.; Monaco, E.A. Comparison of fracture resistance of pressable metal ceramic custom implant abutments with CAD/CAM commercially fabricated zirconia implant abutments. J. Prosthet. Dent. 2009, 101, 226–230. [Google Scholar] [CrossRef]
- Bufalá Pérez, M.; Zubizarreta-Macho, Á.; Borrajo Sánchez, J.; Hernández Rodríguez, J.; Alonso Pérez-Barquero, J.; Riad Deglow, E.; Hernández Montero, S. Removal capability, implant-abutment connection damage and thermal effect using ultrasonic and drilling techniques for the extraction of fractured abutment screws: An in vitro study. BMC Oral Health 2022, 22, 603. [Google Scholar] [CrossRef]








| Method | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Conventional | Rhein83 | Sanhigia | Phibo | ||||||
| N | % | N | % | N | % | N | % | N | % | |
| Total | 180 | 100.0% | 45 | 100.0% | 45 | 100.0% | 45 | 100.0% | 45 | 100.0% |
| Coronal | 93 | 51.7% | 23 | 51.1% | 25 | 55.6% | 26 | 57.8% | 19 | 42.2% |
| Half | 63 | 35.0% | 15 | 33.3% | 13 | 28.9% | 15 | 33.3% | 20 | 44.4% |
| Apical | 24 | 13.3% | 7 | 15.6% | 7 | 15.6% | 4 | 8.9% | 6 | 13.3% |
| Total | No | Yes | |||||
|---|---|---|---|---|---|---|---|
| Method | Total | Operator | Total | N | 180 | 57 | 123 |
| % | 100.0% | 31.7% | 68.3% | ||||
| Op. 1 | N | 60 | 20 | 40 | |||
| % | 100.0% | 33.3% | 66.7% | ||||
| Op. 2 | N | 60 | 22 | 38 | |||
| % | 100.0% | 36.7% | 63.3% | ||||
| Op. 3 | N | 60 | 15 | 45 | |||
| % | 100.0% | 25.0% | 75.0% | ||||
| Conventional | Operator | Total | N | 45 | 13 | 32 | |
| % | 100.0% | 28.9% | 71.1% | ||||
| Op. 1 | N | 15 | 3 | 12 | |||
| % | 100.0% | 20.0% | 80.0% | ||||
| Op. 2 | N | 15 | 6 | 9 | |||
| % | 100.0% | 40.0% | 60.0% | ||||
| Op. 3 | N | 15 | 4 | 11 | |||
| % | 100.0% | 26.7% | 73.3% | ||||
| Rhein83 | Operator | Total | N | 45 | 7 | 38 | |
| % | 100.0% | 15.6% | 84.4% | ||||
| Op. 1 | N | 15 | 4 | 11 | |||
| % | 100.0% | 26.7% | 73.3% | ||||
| Op. 2 | N | 15 | 3 | 12 | |||
| % | 100.0% | 20.0% | 80.0% | ||||
| Op. 3 | N | 15 | 0 | 15 | |||
| % | 100.0% | 0.0% | 100.0% | ||||
| Sanhigia | Operator | Total | N | 45 | 24 | 21 | |
| % | 100.0% | 53.3% | 46.7% | ||||
| Op. 1 | N | 15 | 9 | 6 | |||
| % | 100.0% | 60.0% | 40.0% | ||||
| Op. 2 | N | 15 | 8 | 7 | |||
| % | 100.0% | 53.3% | 46.7% | ||||
| Op. 3 | N | 15 | 7 | 8 | |||
| % | 100.0% | 46.7% | 53.3% | ||||
| Phibo | Operator | Total | N | 45 | 13 | 32 | |
| % | 100.0% | 28.9% | 71.1% | ||||
| Op. 1 | N | 15 | 4 | 11 | |||
| % | 100.0% | 26.7% | 73.3% | ||||
| Op. 2 | N | 15 | 5 | 10 | |||
| % | 100.0% | 33.3% | 66.7% | ||||
| Op. 3 | N | 15 | 4 | 11 | |||
| % | 100.0% | 26.7% | 73.3% | ||||
| Method | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Conventional | Rhein83 | Sanhigia | Phibo | ||||||
| N | % | N | % | N | % | N | % | N | % | |
| Total | 123 | 100.0% | 32 | 100.0% | 38 | 100.0% | 21 | 100.0% | 32 | 100.0% |
| No | 111 | 90.2% | 27 | 84.4% | 35 | 92.1% | 19 | 90.5% | 30 | 93.8% |
| Yes | 12 | 9.8% | 5 | 15.6% | 3 | 7.9% | 2 | 9.5% | 2 | 6.3% |
| Method | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Conventional | Rhein83 | Sanhigia | Phibo | ||||||||||||||||
| Operator | Operator | Operator | Operator | Operator | ||||||||||||||||
| Total | Op. 1 | Op. 2 | Op. 3 | Total | Op. 1 | Op. 2 | Op. 3 | Total | Op. 1 | Op. 2 | Op. 3 | Total | Op. 1 | Op. 2 | Op. 3 | Total | Op. 1 | Op. 2 | Op. 3 | |
| N | 123 | 40 | 38 | 45 | 32 | 12 | 9 | 11 | 38 | 11 | 12 | 15 | 21 | 6 | 7 | 8 | 32 | 11 | 10 | 11 |
| Average | 3.17 | 2.73 | 3.17 | 3.55 | 2.58 | 3.48 | 0.99 | 2.90 | 2.57 | 1.72 | 3.08 | 2.78 | 4.32 | 4.09 | 4.10 | 4.68 | 3.70 | 2.19 | 4.58 | 4.41 |
| Standard deviation | 2.52 | 2.18 | 2.70 | 2.65 | 2.50 | 2.97 | 0.72 | 2.42 | 1.78 | 1.21 | 2.25 | 1.57 | 3.04 | 2.23 | 3.58 | 3.39 | 2.67 | 1.27 | 2.65 | 3.22 |
| Minimo | 0.22 | 0.22 | 0.30 | 0.22 | 0.30 | 0.68 | 0.30 | 0.73 | 0.22 | 0.22 | 0.50 | 0.43 | 0.98 | 1.47 | 1.00 | 0.98 | 0.22 | 1.25 | 1.98 | 0.22 |
| Maximum | 9.92 | 9.42 | 9.92 | 9.67 | 9.67 | 9.42 | 2.18 | 9.67 | 7.62 | 4.27 | 7.62 | 6.03 | 9.67 | 6.83 | 9.67 | 9.67 | 9.92 | 5.88 | 9.92 | 8.90 |
| 25th percentile | 1.50 | 1.49 | 1.38 | 1.98 | 0.81 | 1.70 | 0.40 | 2.08 | 1.50 | 0.50 | 1.55 | 1.53 | 2.17 | 1.75 | 2.00 | 2.25 | 1.85 | 1.50 | 2.93 | 1.12 |
| Median | 2.22 | 2.01 | 2.30 | 2.50 | 2.08 | 2.47 | 0.78 | 2.23 | 2.03 | 1.62 | 2.61 | 2.22 | 2.70 | 4.13 | 2.32 | 3.02 | 2.65 | 1.92 | 3.36 | 4.27 |
| 75th percentile | 4.17 | 3.16 | 3.95 | 4.33 | 2.88 | 4.30 | 1.38 | 2.98 | 3.47 | 2.07 | 4.06 | 3.47 | 6.83 | 6.23 | 8.90 | 8.13 | 5.32 | 2.22 | 6.00 | 7.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Senent-Vicente, G.; Baixauli-López, M.; González-Angulo, E.; Fernández-Bravo, L.; Zubizarreta-Macho, Á.; Gómez-Polo, M.; Selva-Otaolaurruchi, E.J.; Agustín-Panadero, R. In Vitro Analysis of the Removability of Fractured Prosthetic Screws within Endosseous Implants Using Conventional and Mechanical Techniques. Materials 2023, 16, 7317. https://doi.org/10.3390/ma16237317
Senent-Vicente G, Baixauli-López M, González-Angulo E, Fernández-Bravo L, Zubizarreta-Macho Á, Gómez-Polo M, Selva-Otaolaurruchi EJ, Agustín-Panadero R. In Vitro Analysis of the Removability of Fractured Prosthetic Screws within Endosseous Implants Using Conventional and Mechanical Techniques. Materials. 2023; 16(23):7317. https://doi.org/10.3390/ma16237317
Chicago/Turabian StyleSenent-Vicente, Gisela, Mar Baixauli-López, Eva González-Angulo, Luisa Fernández-Bravo, Álvaro Zubizarreta-Macho, Miguel Gómez-Polo, Eduardo J. Selva-Otaolaurruchi, and Rubén Agustín-Panadero. 2023. "In Vitro Analysis of the Removability of Fractured Prosthetic Screws within Endosseous Implants Using Conventional and Mechanical Techniques" Materials 16, no. 23: 7317. https://doi.org/10.3390/ma16237317
APA StyleSenent-Vicente, G., Baixauli-López, M., González-Angulo, E., Fernández-Bravo, L., Zubizarreta-Macho, Á., Gómez-Polo, M., Selva-Otaolaurruchi, E. J., & Agustín-Panadero, R. (2023). In Vitro Analysis of the Removability of Fractured Prosthetic Screws within Endosseous Implants Using Conventional and Mechanical Techniques. Materials, 16(23), 7317. https://doi.org/10.3390/ma16237317









