Surface Analysis of Ti-Alloy Micro-Grooved 12/14 Tapers Assembled to Non-Sleeved and Sleeved Ceramic Heads: A Comparative Study of Retrieved Hip Prostheses
Abstract
1. Introduction
2. Materials and Methods
2.1. Retrieved Implants
- Head must be made of fourth-generation ceramic;
- Head must have a sleeve made of Ti-alloy with a 12/14 internal taper (sleeved ceramic head);
- Stem must have a micro-grooved 12/14 taper and be made of Ti-alloy.
- Head must be made of fourth-generation ceramic;
- Stem must have a micro-grooved 12/14 taper and be made of Ti-alloy;
- The implant must be cementless.
- 4.
- The total implantation time must be comparable, i.e., with a difference smaller than one year, to that of the corresponding implant with sleeved ceramic head;
- 5.
- Patient body mass index (BMI) must be as close as possible to that of the patient from whom the corresponding implant with the sleeve/taper junction was retrieved;
- 6.
- Patient age must be as close as possible to that of the patient from whom the corresponding implant with the sleeve/taper junction was retrieved.
2.2. Surface Damage Scoring
2.3. Surface Roughness Measurement
2.4. Scanning Electron Microscope Analysis
2.5. Statistical Analysis
3. Results
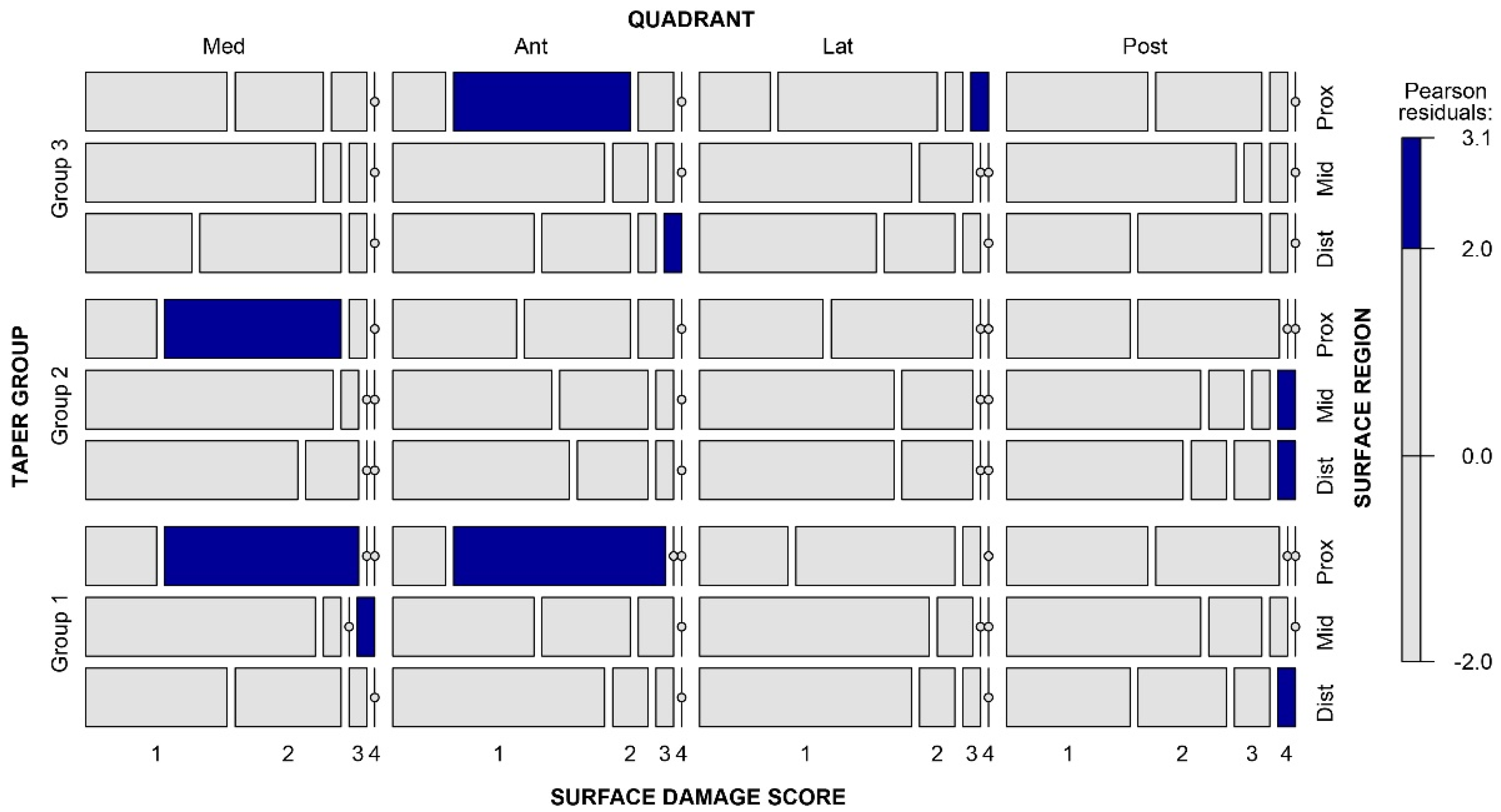
3.1. Surface Damage Scoring
3.2. Surface Roughness Measurement
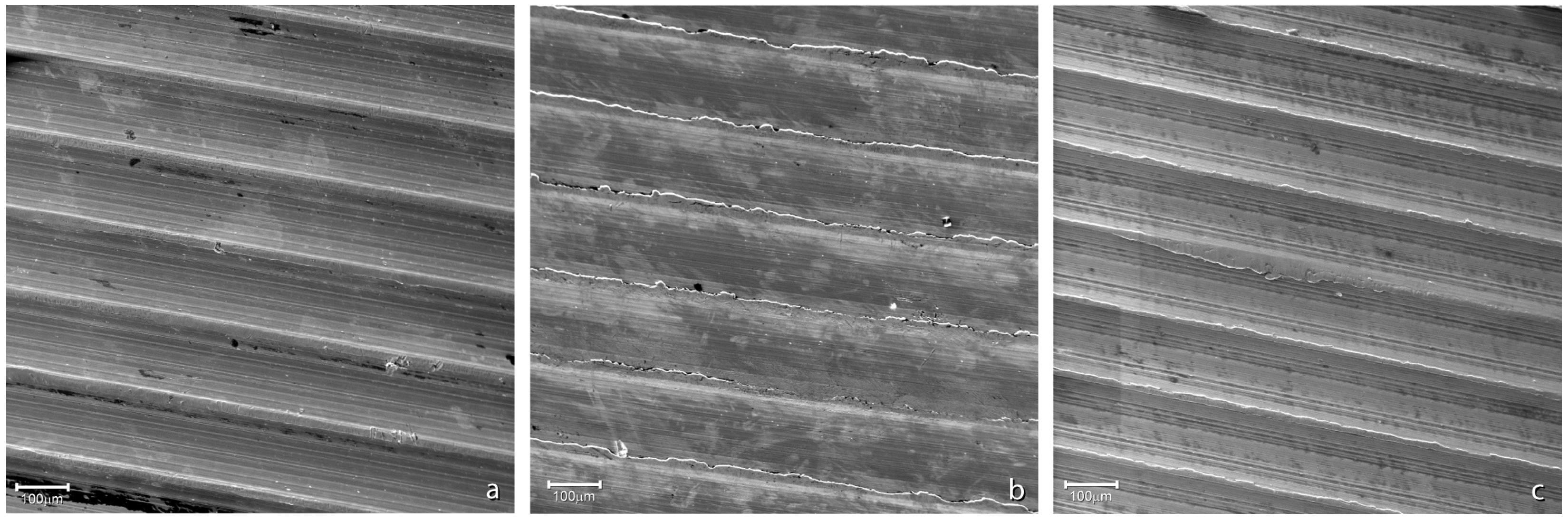
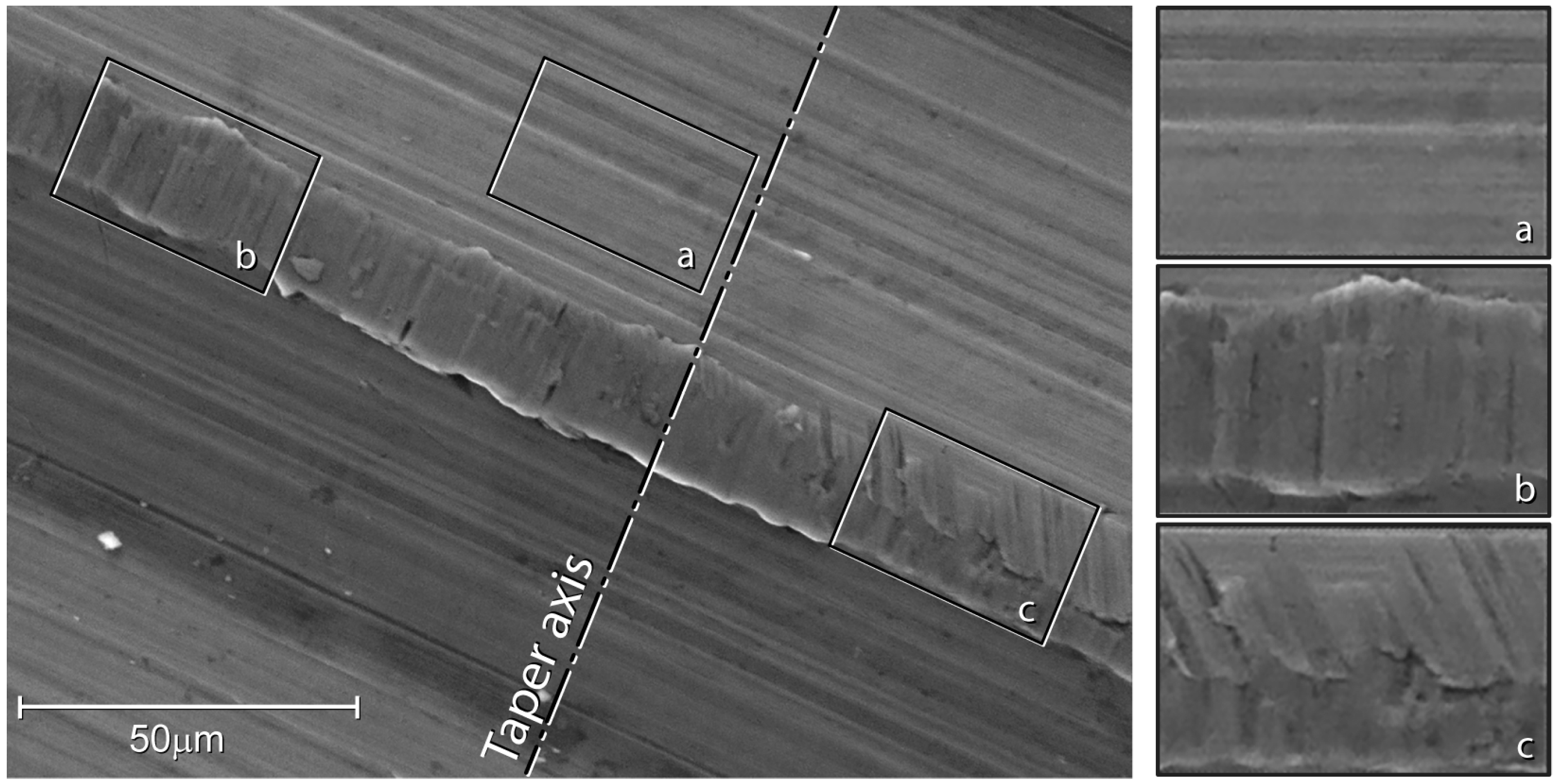
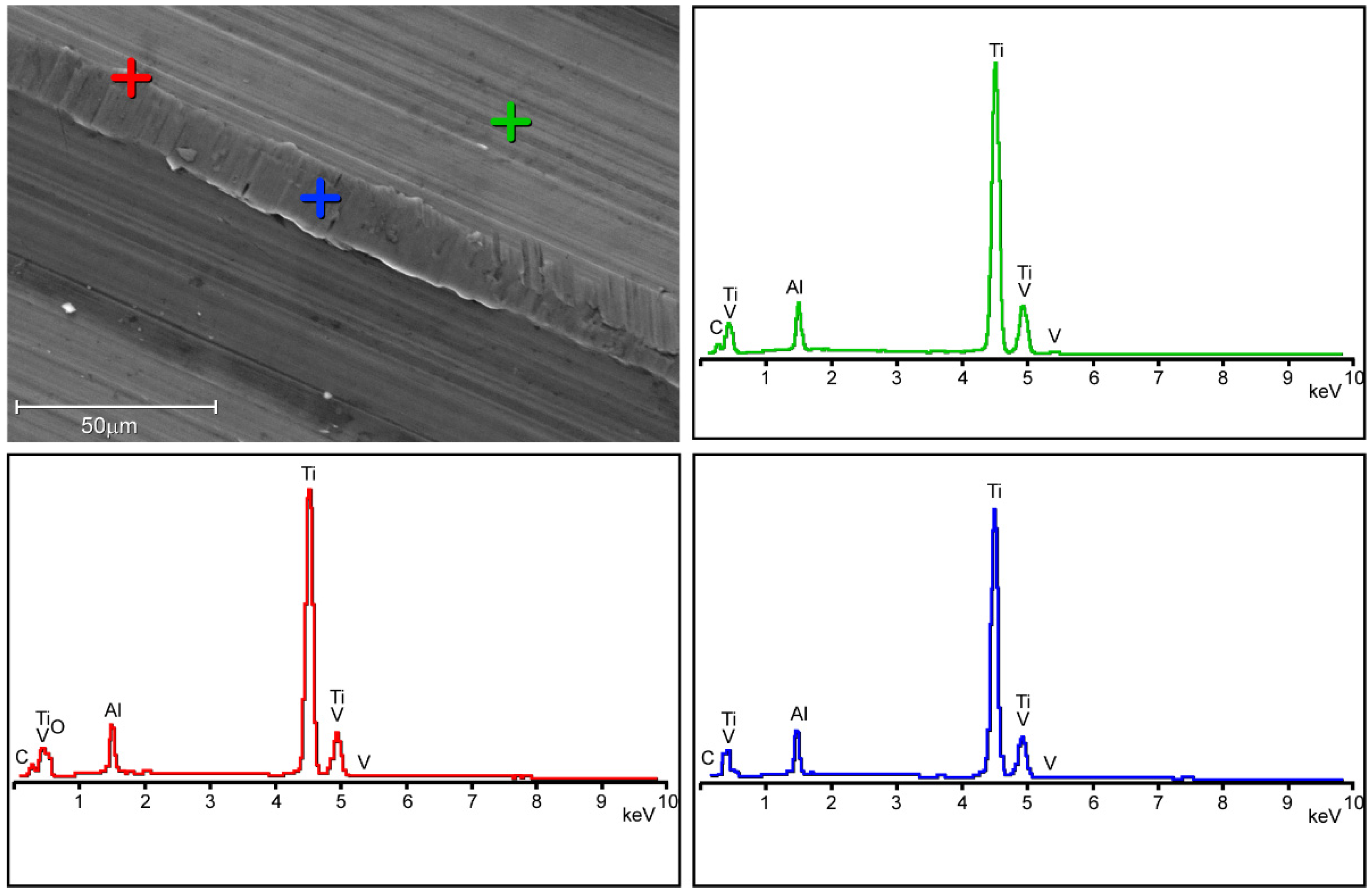
3.3. Scanning Electron Microscope Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Long, M.; Rack, H.J. Titanium Alloys in Total Joint Replacement—A Materials Science Perspective. Biomaterials 1998, 19, 1621–1639. [Google Scholar] [CrossRef] [PubMed]
- Merola, M.; Affatato, S. Materials for Hip Prostheses: A Review of Wear and Loading Considerations. Materials 2019, 12, 495. [Google Scholar] [CrossRef] [PubMed]
- Morlock, M.M.; Hube, R.; Wassilew, G.; Prange, F.; Huber, G.; Perka, C. Taper Corrosion: A Complication of Total Hip Arthroplasty. EFORT Open Rev. 2020, 5, 776–784. [Google Scholar] [CrossRef] [PubMed]
- Kocagoz, S.B.; Underwood, R.J.; Macdonald, D.W.; Gilbert, J.L.; Kurtz, S.M. Ceramic Heads Decrease Metal Release Caused by Head-Taper Fretting and Corrosion. Clin. Orthop. Relat. Res. 2016, 474, 985–994. [Google Scholar] [CrossRef]
- Baleani, M.; Erani, P.; Bordini, B.; Zuccheri, F.; Kordian, M.; De Pasquale, D.; Beraudi, A.; Stea, S. In Vivo Damage of the Head-Neck Junction in Hard-on-Hard Total Hip Replacements: Effect of Femoral Head Size, Metal Combination, and 12/14 Taper Design. Materials 2017, 10, 733. [Google Scholar] [CrossRef]
- Berstock, J.R.; Whitehouse, M.R.; Duncan, C.P. Trunnion Corrosion: What Surgeons Need to Know in 2018. Bone Jt. J. 2018, 100B, 44–49. [Google Scholar] [CrossRef]
- Eichler, D.; Barry, J.; Lavigne, M.; Massé, V.; Vendittoli, P.A. No Radiological and Biological Sign of Trunnionosis with Large Diameter Head Ceramic Bearing Total Hip Arthroplasty after 5 Years. Orthop. Traumatol. Surg. Res. 2021, 107, 102543. [Google Scholar] [CrossRef]
- Bitter, T.; Khan, I.; Marriott, T.; Lovelady, E.; Verdonschot, N.; Janssen, D. The Effects of Manufacturing Tolerances and Assembly Force on the Volumetric Wear at the Taper Junction in Modular Total Hip Arthroplasty. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 1061–1072. [Google Scholar] [CrossRef]
- Ashkanfar, A.; Langton, D.J.; Joyce, T.J. A Large Taper Mismatch Is One of the Key Factors behind High Wear Rates and Failure at the Taper Junction of Total Hip Replacements: A Finite Element Wear Analysis. J. Mech. Behav. Biomed. Mater. 2017, 69, 257–266. [Google Scholar] [CrossRef]
- Shareef, N.; Levine, D. Effect of Manufacturing Tolerances on the Micromotion at the Morse Taper Interface in Modular Hip Implants Using the Finite Element Technique. Biomaterials 1996, 17, 623–630. [Google Scholar] [CrossRef]
- Diaz-Lopez, R.A.; Wen, P.H.; Shelton, J.C. Influence of Taper Design and Loading on Taper Micromotion. J. Mech. Behav. Biomed. Mater. 2022, 128, 105106. [Google Scholar] [CrossRef]
- Gührs, J.; Körner, M.; Bechstedt, M.; Krull, A.; Morlock, M.M. Stem Taper Mismatch Has a Critical Effect on Ceramic Head Fracture Risk in Modular Hip Arthroplasty. Clin. Biomech. 2017, 41, 106–110. [Google Scholar] [CrossRef]
- Feyzi, M.; Fallahnezhad, K.; Taylor, M.; Hashemi, R. An Overview of the Stability and Fretting Corrosion of Microgrooved Necks in the Taper Junction of Hip Implants. Materials 2022, 15, 8396. [Google Scholar] [CrossRef]
- Bechstedt, M.; Gustafson, J.A.; Mell, S.P.; Gührs, J.; Morlock, M.M.; Levine, B.R.; Lundberg, H.J. Contact Conditions for Total Hip Head-Neck Modular Taper Junctions with Microgrooved Stem Tapers. J. Biomech. 2020, 103, 109689. [Google Scholar] [CrossRef]
- Gührs, J.; Krull, A.; Witt, F.; Morlock, M.M. The Influence of Stem Taper Re-Use upon the Failure Load of Ceramic Heads. Med. Eng. Phys. 2015, 37, 545–552. [Google Scholar] [CrossRef]
- Helwig, P.; Konstantinidis, L.; Hirschmüller, A.; Bernstein, A.; Hauschild, O.; Südkamp, N.P.; Ochs, B.G. Modular Sleeves with Ceramic Heads in Isolated Acetabular Cup Revision in Younger Patients—Laboratory and Experimental Analysis of Suitability and Clinical Outcomes. Int. Orthop. 2013, 37, 15–19. [Google Scholar] [CrossRef]
- Falkenberg, A.; Dickinson, E.C.; Morlock, M.M. Adapter Sleeves Are Essential for Ceramic Heads in Hip Revision Surgery. Clin. Biomech. 2020, 71, 1–4. [Google Scholar] [CrossRef]
- Baxmann, M.; Jauch, S.Y.; Schilling, C.; Blömer, W.; Grupp, T.M.; Morlock, M.M. The Influence of Contact Conditions and Micromotions on the Fretting Behavior of Modular Titanium Alloy Taper Connections. Med. Eng. Phys. 2013, 35, 676–683. [Google Scholar] [CrossRef]
- Grupp, T.M.; Weik, T.; Bloemer, W.; Knaebel, H.P. Modular Titanium Alloy Neck Adapter Failures in Hip Replacement—Failure Mode Analysis and Influence of Implant Material. BMC Musculoskelet. Disord. 2010, 11, 3. [Google Scholar] [CrossRef]
- Jauch, S.Y.; Huber, G.; Hoenig, E.; Baxmann, M.; Grupp, T.M.; Morlock, M.M. Influence of Material Coupling and Assembly Condition on the Magnitude of Micromotion at the Stem-Neck Interface of a Modular Hip Endoprosthesis. J. Biomech. 2011, 44, 1747–1751. [Google Scholar] [CrossRef]
- Viceconti, M.; Baleani, M.; Squarzoni, S.; Toni, A. Fretting Wear in a Modular Neck Hip Prosthesis. J. Biomed. Mater. Res. 1997, 35, 207–216. [Google Scholar] [CrossRef]
- Gilbert, J.L.; Mali, S.A. Medical Implant Corrosion: Electrochemistry at Metallic Biomaterial Surfaces. In Degradation of Implant Materials; Springer: New York, NY, USA, 2012; Volume 9781461439424, pp. 1–28. [Google Scholar] [CrossRef]
- Jacobs, J.J.; Skipor, A.K.; Patterson, L.M.; Hallab, N.J.; Paprosky, W.G.; Black, J.; Galante, J.O. Metal Release in Patients Who Have Had a Primary Total Hip Arthroplasty. A Prospective, Controlled, Longitudinal Study. J. Bone Jt. Surg. Am. 1998, 80, 1447–1458. [Google Scholar] [CrossRef]
- Srinivasan, A.; Jung, E.; Levine, B.R. Modularity of the Femoral Component in Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. 2012, 20, 214–222. [Google Scholar] [CrossRef]
- Swaminathan, V.; Gilbert, J.L. Fretting Corrosion of CoCrMo and Ti6Al4V Interfaces. Biomaterials 2012, 33, 5487–5503. [Google Scholar] [CrossRef] [PubMed]
- Moskal, J.; Stover, M. Mechanically Assisted Crevice Corrosion of the Head-Neck Taper in a Large Head Metal-on-Metal Total Hip Arthroplasty. Arthroplast. Today 2015, 1, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, J.L.; Buckley, C.A.; Jacobs, J.J. In Vivo Corrosion of Modular Hip Prosthesis Components in Mixed and Similar Metal Combinations. The Effect of Crevice, Stress, Motion, and Alloy Coupling. J. Biomed. Mater. Res. 1993, 27, 1533–1544. [Google Scholar] [CrossRef]
- Deny, A.; Barry, J.; Hutt, J.R.B.; Lavigne, M.; Massé, V.; Vendittoli, P.A. Effect of Sleeved Ceramic Femoral Heads on Titanium Ion Release. HIP Int. 2018, 28, 139–144. [Google Scholar] [CrossRef]
- Baleani, M.; Toni, A.; Ancarani, C.; Stea, S.; Bordini, B. Long-Term Survivorship of an Exchangeable-Neck Hip Prosthesis with a Ti-Alloy/Ti-Alloy Neck–Stem Junction. Arch. Orthop. Trauma Surg. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Lalor, P.A.; Revell, P.A.; Gray, A.B.; Wright, S.; Railton, G.T.; Freeman, M.A.R. Sensitivity to Titanium. A Cause of Implant Failure? J. Bone Jt. Surg.-Ser. B 1991, 73, 25–28. [Google Scholar] [CrossRef]
- Mistry, J.B.; Chughtai, M.; Elmallah, R.K.; Diedrich, A.; Le, S.; Thomas, M.; Mont, M.A. Trunnionosis in Total Hip Arthroplasty: A Review. J. Orthop. Traumatol. 2016, 17, 1–6. [Google Scholar] [CrossRef]
- Cooper, H.J.; Della Valle, C.J.; Berger, R.A.; Tetreault, M.; Paprosky, W.G.; Sporer, S.M.; Jacobs, J.J. Corrosion at the Head-Neck Taper as a Cause for Adverse Local Tissue Reactions after Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2012, 94, 1655–1661. [Google Scholar] [CrossRef]
- MacDonald, D.W.; Chen, A.F.; Lee, G.C.; Klein, G.R.; Mont, M.A.; Kurtz, S.M.; Cates, H.E.; Kraay, M.J.; Rimnac, C.M. Fretting and Corrosion Damage in Taper Adapter Sleeves for Ceramic Heads: A Retrieval Study. J. Arthroplast. 2017, 32, 2887–2891. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, J.R.; Gilbert, J.L.; Jacobs, J.J.; Bauer, T.W.; Paprosky, W.; Leurgans, S. A Multicenter Retrieval Study of the Taper Interfaces of Modular Hip Prostheses. Clin. Orthop. Relat. Res. 2002, 401, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Koch, C.N.; Figgie, M.; Figgie, M.P.; Elpers, M.E.; Wright, T.M.; Padgett, D.E. Ceramic Bearings with Titanium Adapter Sleeves Implanted During Revision Hip Arthroplasty Show Minimal Fretting or Corrosion: A Retrieval Analysis. HSS J. 2017, 13, 241–247. [Google Scholar] [CrossRef]
- Wyles, C.C.; Kolz, J.M.; Van Citters, D.W.; Berry, D.J.; Trousdale, R.T. In Vivo Corrosion of Sleeved Ceramic Femoral Heads: A Retrieval Study. J. Arthroplast. 2021, 36, 1133–1137. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Kurtz, S.M.; Kocagöz, S.B.; Hanzlik, J.A.; Underwood, R.J.; Gilbert, J.L.; MacDonald, D.W.; Lee, G.C.; Mont, M.A.; Kraay, M.J.; Klein, G.R.; et al. Do Ceramic Femoral Heads Reduce Taper Fretting Corrosion in Hip Arthroplasty? A Retrieval Study. Clin. Orthop. Relat. Res. 2013, 471, 3270–3282. [Google Scholar] [CrossRef] [PubMed]
- Stockhausen, K.E.; Riedel, C.; Belinski, A.V.; Rothe, D.; Gehrke, T.; Klebig, F.; Gebauer, M.; Amling, M.; Citak, M.; Busse, B. Variability in Stem Taper Surface Topography Affects the Degree of Corrosion and Fretting in Total Hip Arthroplasty. Sci. Rep. 2021, 11, 9348. [Google Scholar] [CrossRef]
- Pu, J.; Wu, D.; Zhang, Y.; Zhang, X.; Jin, Z.; Wu, J.; Zhang, D.; Zhang, Y.; Jin, X.; An, Z. An Experimental Study on the Fretting Corrosion Behaviours of Three Material Pairs at Modular Interfaces for Hip Joint Implants. Lubricants 2021, 9, 12. [Google Scholar] [CrossRef]
- Qu, J.; Blau, P.J.; Watkins, T.R.; Cavin, O.B.; Kulkarni, N.S. Friction and Wear of Titanium Alloys Sliding against Metal, Polymer, and Ceramic Counterfaces. Wear 2005, 258, 1348–1356. [Google Scholar] [CrossRef]
- Mueller, U.; Braun, S.; Schroeder, S.; Sonntag, R.; Kretzer, J.P. Same Same but Different? 12/14 Stem and Head Tapers in Total Hip Arthroplasty. J. Arthroplast. 2017, 32, 3191–3199. [Google Scholar] [CrossRef]
- Haschke, H.; Falkenberg, A.; Morlock, M.M.; Huber, G. Do SiNx Coatings Bear the Potential to Reduce the Risk of Micromotion in Modular Taper Junctions? Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2020, 234, 897–908. [Google Scholar] [CrossRef]
- Hager, C.H.; Sanders, J.H.; Sharma, S. Characterization of Mixed and Gross Slip Fretting Wear Regimes in Ti6Al4V Interfaces at Room Temperature. Wear 2004, 257, 167–180. [Google Scholar] [CrossRef]
- Falkenberg, A.; Biller, S.; Morlock, M.M.; Huber, G. Micromotion at the Head-Stem Taper Junction of Total Hip Prostheses Is Influenced by Prosthesis Design-, Patient- and Surgeon-Related Factors. J. Biomech. 2020, 98, 109424. [Google Scholar] [CrossRef]
- Haschke, H.; Konow, T.; Huber, G.; Morlock, M.M. Influence of Flexural Rigidity on Micromotion at the Head-Stem Taper Interface of Modular Hip Prostheses. Med. Eng. Phys. 2019, 68, 1–10. [Google Scholar] [CrossRef]
- Rieker, C.B.; Wahl, P. What the Surgeon Can Do to Reduce the Risk of Trunnionosis in Hip Arthroplasty: Recommendations from the Literature. Materials 2020, 13, 1950. [Google Scholar] [CrossRef] [PubMed]
- Fallahnezhad, K.; Farhoudi, H.; Oskouei, R.H.; Taylor, M. A Finite Element Study on the Mechanical Response of the Head-Neck Interface of Hip Implants under Realistic Forces and Moments of Daily Activities: Part 2. J. Mech. Behav. Biomed. Mater. 2018, 77, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, J.A.; Mell, S.P.; Levine, B.R.; Pourzal, R.; Lundberg, H.J. Interaction of Surface Topography and Taper Mismatch on Head-Stem Modular Junction Contact Mechanics during Assembly in Modern Total Hip Replacement. J. Orthop. Res. 2023, 41, 418–425. [Google Scholar] [CrossRef]

| Group 1 | Group 2 | Group 3 | ||
|---|---|---|---|---|
| Clinical Information | Kruskal–Wallis | |||
| Median (Range) | p-Value | |||
| Total implant. Time | ||||
| (years) | 4.1 (0.2–9.6) | 3.9 (0.5–10.0) | 4.2 (0.4–10.2) | 0.92 |
| BMI | ||||
| (kg/m2) | 30.1 (23.4–35.6) | 29.4 (23.7–36.4) | 29.6 (22.8–37.7) | 0.82 |
| Age at retrieval | ||||
| (years) | 61 (35–79) | 68 (30–70) | 56 (38–77) | 0.06 |
| Ceramic head configuration | ||||
| Number of retrieved heads | ||||
| Diameter (mm) | ||||
| 32/36/40 | 2003/8/4 | 2002/8/5 | 2004/8/3 | / |
| Neck length | ||||
| S/M/L | 2005/7/3 | 2005/6/4 | 2004/8/3 | / |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martelli, A.; Erani, P.; Pazzagli, N.; Cannillo, V.; Baleani, M. Surface Analysis of Ti-Alloy Micro-Grooved 12/14 Tapers Assembled to Non-Sleeved and Sleeved Ceramic Heads: A Comparative Study of Retrieved Hip Prostheses. Materials 2023, 16, 1067. https://doi.org/10.3390/ma16031067
Martelli A, Erani P, Pazzagli N, Cannillo V, Baleani M. Surface Analysis of Ti-Alloy Micro-Grooved 12/14 Tapers Assembled to Non-Sleeved and Sleeved Ceramic Heads: A Comparative Study of Retrieved Hip Prostheses. Materials. 2023; 16(3):1067. https://doi.org/10.3390/ma16031067
Chicago/Turabian StyleMartelli, Andrea, Paolo Erani, Nicola Pazzagli, Valeria Cannillo, and Massimiliano Baleani. 2023. "Surface Analysis of Ti-Alloy Micro-Grooved 12/14 Tapers Assembled to Non-Sleeved and Sleeved Ceramic Heads: A Comparative Study of Retrieved Hip Prostheses" Materials 16, no. 3: 1067. https://doi.org/10.3390/ma16031067
APA StyleMartelli, A., Erani, P., Pazzagli, N., Cannillo, V., & Baleani, M. (2023). Surface Analysis of Ti-Alloy Micro-Grooved 12/14 Tapers Assembled to Non-Sleeved and Sleeved Ceramic Heads: A Comparative Study of Retrieved Hip Prostheses. Materials, 16(3), 1067. https://doi.org/10.3390/ma16031067







