Numerical Analysis of a Transtibial Prosthesis Socket Using 3D-Printed Bio-Based PLA
Abstract
:1. Introduction
2. Materials and Methods
2.1. Testing of 3D-Printed PLA Specimen’s Experimental Material Properties
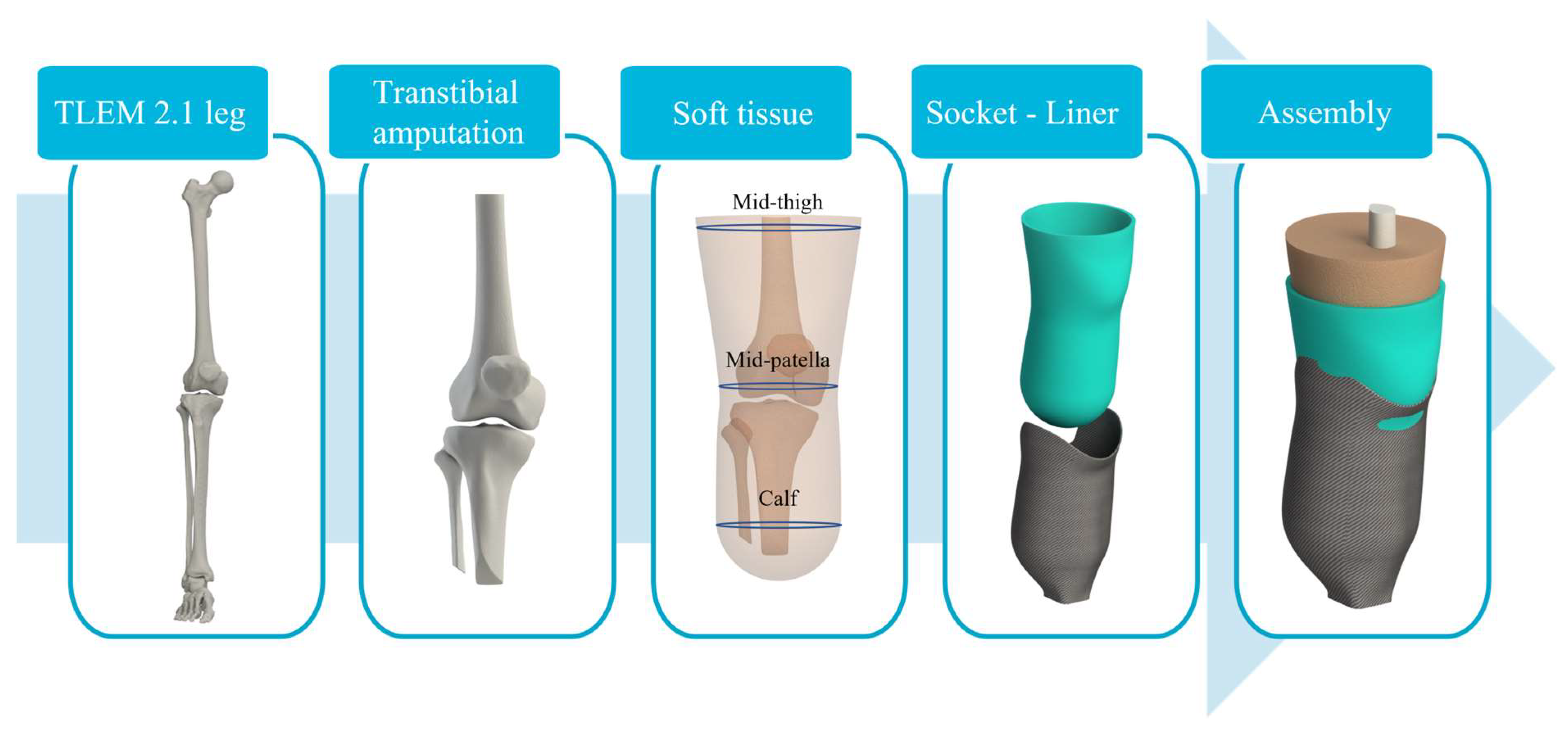
2.2. Numerical Model
2.2.1. Geometry
2.2.2. Material Models
2.2.3. Boundary Conditions
3. Results
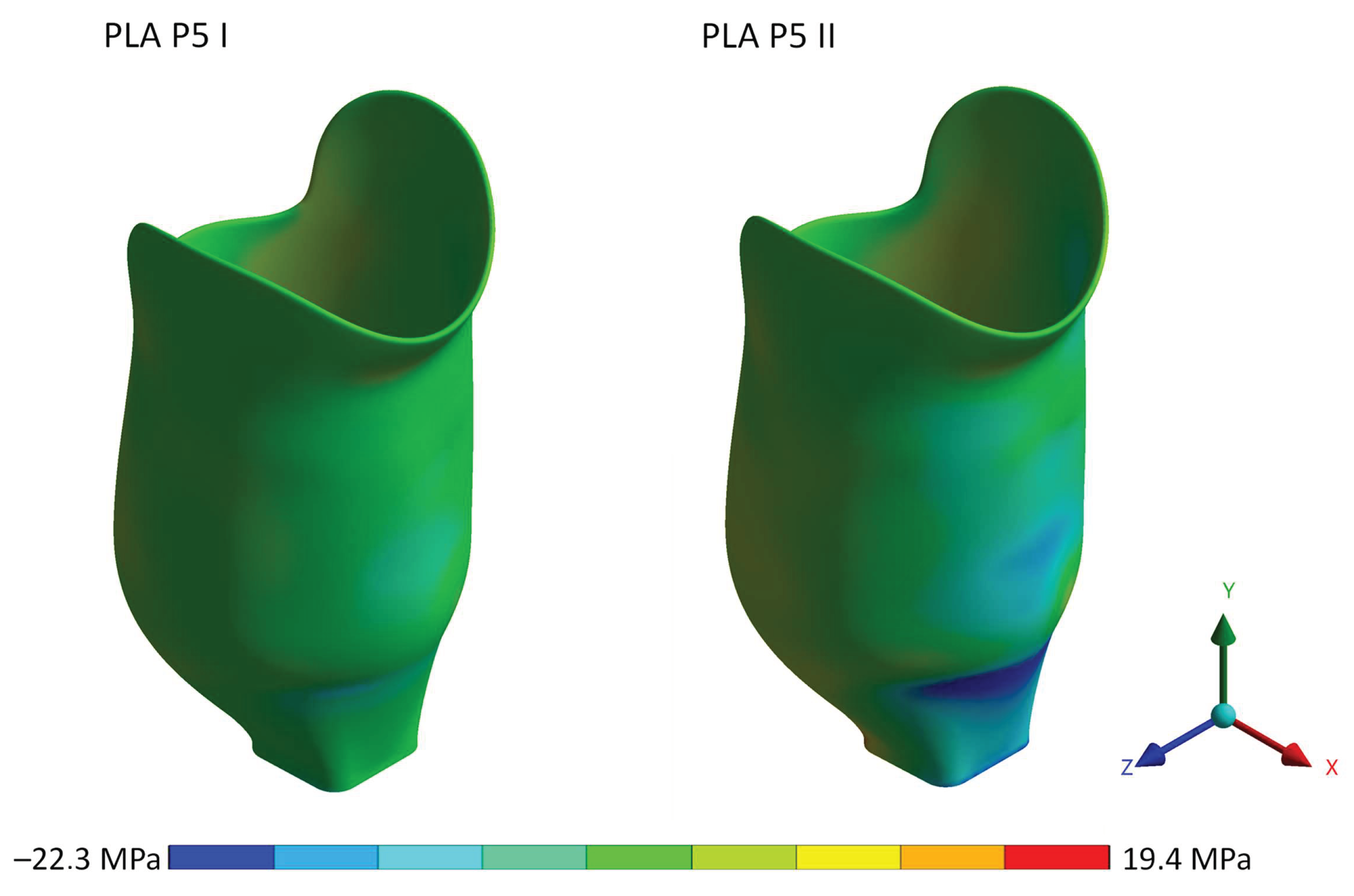
3.1. PLA Socket Strength Test
3.2. Biomechanical Analysis of Transtibial Sockets
4. Discussion
4.1. PLA Socket Strength Test
4.2. Biomechanical Analysis of Transtibial Sockets
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Eskridge, S.L.; Dougherty, A.L.; Watrous, J.R.; McCabe, C.T.; Cancio, J.M.; Mazzone, B.N.; Galarneau, M.R. Prosthesis satisfaction and quality of life in US service members with combat-related major lower-limb amputation. Prosthet. Orthot. Int. 2022, 46, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Kolossváry, E.; Björck, M.; Behrendt, C.-A. Lower Limb Major Amputation Data as a Signal of an East/West Health Divide Across Europe. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 645–646. [Google Scholar] [CrossRef]
- Creager, M.A.; Matsushita, K.; Arya, S.; Beckman, J.A.; Duval, S.; Goodney, P.P.; Gutierrez, J.A.T.; Kaufman, J.A.; Joynt Maddox, K.E.; Pollak, A.W.; et al. Reducing nontraumatic lower-extremity amputations by 20% by 2030: Time to get to our feet: A policy statement from the American Heart Association. Circulation 2021, 143, e875–e891. [Google Scholar] [CrossRef] [PubMed]
- Krajbich, J.I.; Pinzur, M.S.; Potter, B.K.; Stevens, P.M. (Eds.) Atlas of Amputations and Limb Deficiencies: Surgical, Prosthetic, and Rehabilitation Principles; Lippincott Williams & Wilkins: Rosemont, IL, USA, 2016. [Google Scholar]
- Dietrich, C.; Nehrdich, S.; Seifert, S.; Blume, K.R.; Miltner, W.H.; Hofmann, G.O.; Weiss, T. Leg prosthesis with somatosensory feedback reduces phantom limb pain and increases functionality. Front. Neurol. 2018, 9, 270. [Google Scholar] [CrossRef] [Green Version]
- Baars, E.C.; Schrier, E.; Dijkstra, P.U.; Geertzen, J.H.B. Prosthesis satisfaction in lower limb amputees: A systematic review of associated factors and questionnaires. Medicine 2018, 97, e12296. [Google Scholar] [CrossRef]
- Dillingham, T.; Kenia, J.; Shofer, F.; Marschalek, J. A prospective assessment of an adjustable, immediate fit, transtibial prosthesis. PM&R 2019, 11, 1210–1217. [Google Scholar]
- Petrini, F.M.; Bumbasirevic, M.; Valle, G.; Ilic, V.; Mijović, P.; Čvančara, P.; Barberi, F.; Katic, N.; Bortolotti, D.; Andreu, D.; et al. Sensory feedback restoration in leg amputees improves walking speed, metabolic cost and phantom pain. Nat. Med. 2019, 25, 1356–1363. [Google Scholar] [CrossRef] [Green Version]
- Sanders, J.E.; Youngblood, R.T.; Hafner, B.J.; Ciol, M.A.; Allyn, K.J.; Gardner, D.; Cagle, J.C.; Redd, C.B.; Dietrich, C.R. Residual limb fluid volume change and volume accommodation: Relationships to activity and self-report outcomes in people with trans-tibial amputation. Prosthet. Orthot. Int. 2018, 42, 415–427. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.E.; Youngblood, R.T.; Hafner, B.J.; Cagle, J.C.; McLean, J.B.; Redd, C.B.; Dietrich, C.R.; Ciol, M.A.; Allyn, K.J. Effects of socket size on metrics of socket fit in trans-tibial prosthesis users. Med. Eng. Phys. 2017, 44, 32–43. [Google Scholar] [CrossRef]
- Paterno, L.; Ibrahimi, M.; Gruppioni, E.; Menciassi, A.; Ricotti, L. Sockets for Limb Prostheses: A Review of Existing Technologies and Open Challenges. IEEE Trans. Biomed. Eng. 2018, 65, 1996–2010. [Google Scholar] [CrossRef]
- Wang, Y.; Tan, Q.; Pu, F.; Boone, D.; Zhang, M. A Review of the Application of Additive Manufacturing in Prosthetic and Orthotic Clinics from a Biomechanical Perspective. Engineering 2020, 6, 1258–1266. [Google Scholar] [CrossRef]
- Barrios-Muriel, J.; Romero-Sánchez, F.; Alonso-Sánchez, F.J.; Salgado, D.R. Advances in Orthotic and Prosthetic Manufacturing: A Technology Review. Materials 2020, 13, 295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frossard, L.; Berg, D.; Merlo, G.; Quincey, T.; Burkett, B. Cost comparison of socket-suspended and bone-anchored transfemoral prostheses. JPO J. Prosthet. Orthot. 2017, 29, 150–160. [Google Scholar] [CrossRef]
- Bhatt, S.; Joshi, D.; Rakesh, P.K.; Godiyal, A.K. Advances in additive manufacturing processes and their use for the fabrication of lower limb prosthetic devices. Expert Rev. Med. Devices 2023, 20, 17–27. [Google Scholar] [CrossRef]
- Ribeiro, D.; Cimino, S.R.; Mayo, A.L.; Ratto, M.; Hitzig, S.L. 3D printing and amputation: A scoping review. Disabil. Rehabil. Assist. Technol. 2021, 16, 221–240. [Google Scholar] [CrossRef]
- van der Stelt, M.; Grobusch, M.P.; Koroma, A.R.; Papenburg, M.; Kebbie, I.; Slump, C.H.; Maal, T.J.; Brouwers, L. Pioneering low-cost 3D-printed transtibial prosthetics to serve a rural population in Sierra Leone–an observational cohort study. EClinicalMedicine 2021, 35, 100874. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Wontorcik, L. Stereolithography and Prosthetic Test Socket Manufacture: A Cost/Benefit Analysis. JPO J. Prosthet. Orthot. 1998, 10, 17–20. Available online: https://journals.lww.com/jpojournal/Fulltext/1998/01010/Stereolithography_and_Prosthetic_Test_Socket.5.aspx (accessed on 12 December 2022). [CrossRef]
- Rogers, B. Double-wall, transtibial prosthetic socket fabricated using selective laser sintering: A case study. J. Prosthet. Orthot. 2000, 12, 97–103. [Google Scholar] [CrossRef]
- Herbert, N.; Simpson, D.; Spence, W.D.; Ion, W. A preliminary investigation into the development of 3-D printing of prosthetic sockets. J. Rehabil. Res. Dev. 2005, 42, 141–146. [Google Scholar] [CrossRef]
- Hsu, L.H.; Huang, G.F.; Lu, C.T.; Hong, D.Y.; Liu, S.H. The Development of a Rapid Prototyping Prosthetic Socket Coated with a Resin Layer for Transtibial Amputees. Prosthet. Orthot. Int. 2010, 34, 37–45. [Google Scholar] [CrossRef] [Green Version]
- Ouassil, S.-E.; El Magri, A.; Vanaei, H.R.; Vaudreuil, S. Investigating the effect of printing conditions and annealing on the porosity and tensile behavior of 3D-printed polyetherimide material in Z-direction. J. Appl. Polym. Sci. 2023, 140, e53353. [Google Scholar] [CrossRef]
- Vaudreuil, S.; Bencaid, S.-E.; Vanaei, H.R.; El Magri, A. Effects of Power and Laser Speed on the Mechanical Properties of AlSi7Mg0.6 Manufactured by Laser Powder Bed Fusion. Materials 2022, 15, 8640. [Google Scholar] [CrossRef] [PubMed]
- Rogers, B.; Bosker, G.; Faustini, M.; Walden, G.; Neptune, R.R.; Crawford, R. Case report: Variably compliant transtibial prosthetic socket fabricated using solid freeform fabrication. J. Prosthet. Orthot. 2008, 20, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Sengeh, D.M.; Herr, H. A variable-impedance prosthetic socket for a transtibial amputee designed from magnetic resonance imaging data. J. Prosthet. Orthot. 2013, 25, 129–137. [Google Scholar] [CrossRef] [Green Version]
- Algarni, M.; Ghazali, S. Comparative study of the sensitivity of pla, abs, peek, and petg’s mechanical properties to fdm printing process parameters. Crystals 2021, 11, 995. [Google Scholar] [CrossRef]
- Bellehumeur, C.; Li, L.; Sun, Q.; Gu, P. Modeling of Bond Formation Between Polymer Filaments in the Fused Deposition Modeling Process. J. Manuf. Process. 2004, 6, 170–178. [Google Scholar] [CrossRef]
- Dickinson, A.S.; Steer, J.W.; Worsley, P.R. Finite element analysis of the amputated lower limb: A systematic review and recommendations. Med. Eng. Phys. 2017, 43, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Colombo, G.; Rizzi, C.; Regazzoni, D.; Vitali, A. 3D interactive environment for the design of medical devices. Int. J. Interact. Des. Manuf. 2018, 12, 699–715. Available online: https://link.springer.com/article/10.1007/s12008-018-0458-8 (accessed on 25 February 2023). [CrossRef]
- Silver-Thorn, B.; Childress, D. Generic, geometric finite element analysis of the transtibial residual limb and prosthetic socket. J. Rehabil. Res. Dev. 1997, 34, 171–186. [Google Scholar]
- Silver-Thorn, M.B.; Childress, D.S. Parametric analysis using the finite element method to investigate prosthetic interface stresses for persons with trans-tibial amputation. J. Rehabil. Res. Dev. 1996, 33, 227–238. Available online: https://epublications.marquette.edu/bioengin_fac/307/ (accessed on 25 February 2023).
- Steer, J.W.; Worsley, P.R.; Browne, M.; Dickinson, A.S. Predictive prosthetic socket design: Part 1—Population-based evaluation of transtibial prosthetic sockets by FEA-driven surrogate modelling. Biomech. Model. Mechanobiol. 2019, 19, 1331–1346. [Google Scholar] [CrossRef] [Green Version]
- Ramalho, A.; Ferraz, M.; Gaspar, M.; Capela, C. Development of a preliminary finite element model to assess the effects of friction on the residual limb of a transfemoral amputee. Mater. Today Proc. 2020, 33, 1859–1863. [Google Scholar] [CrossRef]
- Plesec, V.; Harih, G. Development of a generic numerical transtibial model for limb–prosthesis system evaluation. Appl. Sci. 2023, 13, 2339. [Google Scholar] [CrossRef]
- Goh, J.; Lee, P.; Ng, P. Structural integrity of polypropylene prosthetic sockets manufactured using the polymer deposition technique. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2002, 216, 359–368. [Google Scholar] [CrossRef]
- Vitali, A.; Regazzoni, D.; Rizzi, C.; Colombo, G. Design and additive manufacturing of lower limb prosthetic socket. ASME Int. Mech. Eng. Congr. Expo. 2017, 58462, V011T15A021. [Google Scholar]
- Campbell, A.; Sexton, S.; Schaschke, C.; Kinsman, H.; McLaughlin, B.; Boyle, M. Prosthetic limb sockets from plant-based composite materials. Prosthet. Orthot. Int. 2012, 36, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Neo, L.; Lee, P.; Goh, J. Principal structural testing of trans tibial prosthetic assemblies: Specimen preparation. Prosthet. Orthot. Int. 2000, 24, 241–245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Current, T.; Kogler, G.; Earth, D. Static structural testing of trans-tibial composite sockets. Prosthet. Orthot. Int. 1999, 23, 113–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bombek, M.; Vesenjak, U.; Pisek, M.; Vidmar, G.; Knez, S.; Medved, S. Mechanical testing of laminated composite materials for prosthetic sockets. Mater. Technol. 2021, 55, 655–661. [Google Scholar] [CrossRef]
- Polystyrene|Properties, Price & Application|Material Properties. Available online: https://material-properties.org/polystyrene-properties-application-price/ (accessed on 28 October 2022).
- Kallin, S.; Rashid, A.; Salomonsson, K.; Hansbo, P. Comparison of mechanical conditions in a lower leg model with 5 or 6 tissue types while exposed to prosthetic sockets applying finite element analysis. arXiv 2019. [Google Scholar] [CrossRef]
- Cagle, J.C.; Reinhall, P.G.; Allyn, K.J.; McLean, J.; Hinrichs, P.; Hafner, B.J.; Saanders, J.E. A finite element model to assess transtibial prosthetic sockets with elastomeric liners. Med. Biol. Eng. Comput. 2018, 56, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.C.C.; Zhang, M.; Jia, X.; Cheung, J.T.M. Finite element modeling of the contact interface between trans-tibial residual limb and prosthetic socket. Med. Eng. Phys. 2004, 26, 655–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDowell, M.A.; Fryar, C.D.; Ogden, C.L.; Flegal, K.M. Anthropometric reference data for children and adults: United States, 2003–2006. Natl. Health Stat. Rep. 2008, 10, 5. [Google Scholar]
- Cagle, J. A Computational Tool to Enhance Clinical Selection of Prosthetic Liners for People with Lower Limb Amputation. Ph.D. Thesis, University of Washington, Ann Arbor, MI, USA, 2016. [Google Scholar]
- Cagle, J.C.; Hafner, B.J.; Taflin, N.; Sanders, J.E. Characterization of prosthetic liner products for people with transtibial amputation. J. Prosthet. Orthot. 2018, 30, 187–199. [Google Scholar] [CrossRef]
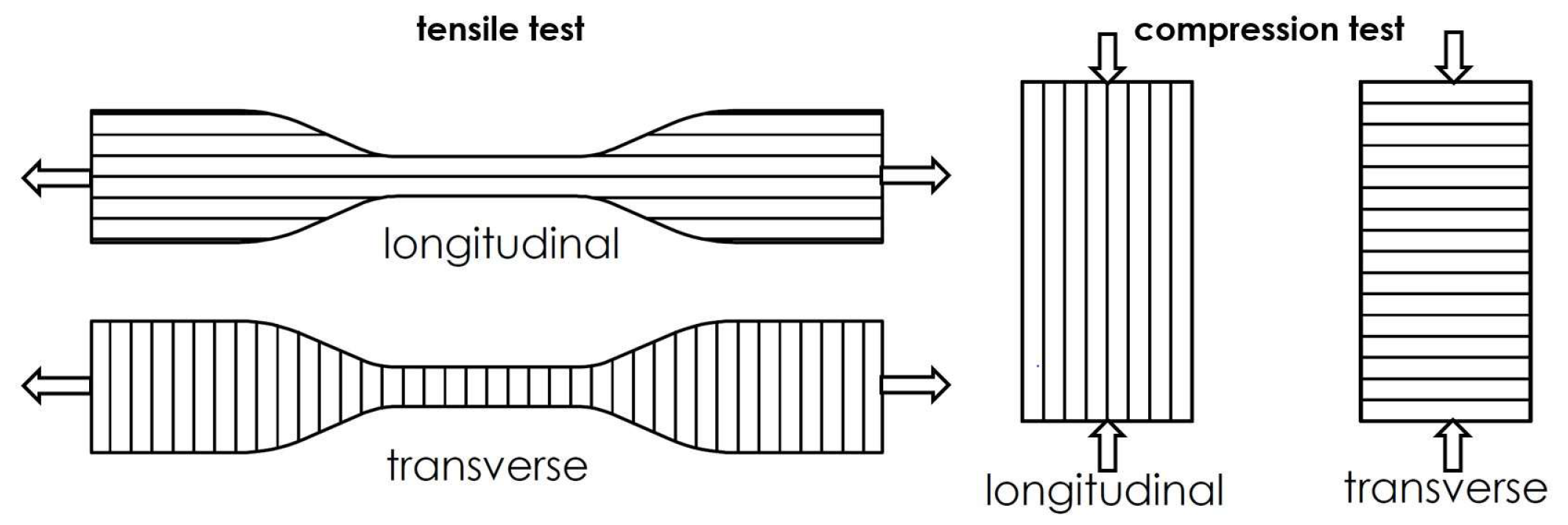









| Yield Strain (%) | Yield Stress (MPa) | |||
|---|---|---|---|---|
| Tensile | Compression | Tensile | Compression | |
| PLA longitudinal | 3 | 7.4 | 60.9 | 81 |
| PLA transverse | 1 | 5.4 | 24.9 | 69 |
| Yield Strain (%) | Yield Stress (MPa) | E (MPa) | Poisson’s Ratio | |
|---|---|---|---|---|
| Composite | N/A | 193 | 4991 | 0.3 |
| Polystyrene | 1.4 | 48 | 3400 | 0.34 |
| Loading Case | Donning of the Socket | ISO P5 I (Heel Strike) | ISO P5 II (Push-Off) | ||
|---|---|---|---|---|---|
| Settling Force | Proof Force | Settling Force | Proof Force | ||
| Load (N) | Interference fit | 1024 | 2240 | 920 | 2013 |
| Donning | Settling | Proof | ||||
|---|---|---|---|---|---|---|
| P5 I | P5 II | P5 I | P5 II | P5 I | P5 II | |
| Von-Mises stress (MPa) | 3.4 | 3.4 | 5.4 | 10.8 | 11.4 | 25.5 |
| Tensile stress (y-axis) (MPa) | 3.0 | 3.0 | 2.3 | 8.7 | 3.2 | 19.4 |
| Compression stress (y-axis) (MPa) | 3.0 | 3.0 | 4.4 | 9.3 | 9.3 | 22.3 |
| Von-Mises strain (%) | 0.11 | 0.11 | 0.18 | 0.37 | 0.38 | 0.86 |
| Tensile strain (y-axis) (%) | 0.09 | 0.09 | 0.07 | 0.26 | 0.10 | 0.58 |
| Compression strain (y-axis) (%) | 0.08 | 0.08 | 0.14 | 0.30 | 0.32 | 0.72 |
| Global Deformation (mm) | 3D-Printed PLA | Polystyrene | Composite |
|---|---|---|---|
| P5 I—settling test force | 0.74 | 0.67 | 0.49 |
| P5 II—settling test force | 2.66 | 2.52 | 2.18 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plesec, V.; Humar, J.; Dobnik-Dubrovski, P.; Harih, G. Numerical Analysis of a Transtibial Prosthesis Socket Using 3D-Printed Bio-Based PLA. Materials 2023, 16, 1985. https://doi.org/10.3390/ma16051985
Plesec V, Humar J, Dobnik-Dubrovski P, Harih G. Numerical Analysis of a Transtibial Prosthesis Socket Using 3D-Printed Bio-Based PLA. Materials. 2023; 16(5):1985. https://doi.org/10.3390/ma16051985
Chicago/Turabian StylePlesec, Vasja, Jani Humar, Polona Dobnik-Dubrovski, and Gregor Harih. 2023. "Numerical Analysis of a Transtibial Prosthesis Socket Using 3D-Printed Bio-Based PLA" Materials 16, no. 5: 1985. https://doi.org/10.3390/ma16051985
APA StylePlesec, V., Humar, J., Dobnik-Dubrovski, P., & Harih, G. (2023). Numerical Analysis of a Transtibial Prosthesis Socket Using 3D-Printed Bio-Based PLA. Materials, 16(5), 1985. https://doi.org/10.3390/ma16051985







