Fitting of Different Intraradicular Composite Posts to Oval Tooth Root Canals: A Preliminary Assessment
Abstract
:1. Introduction
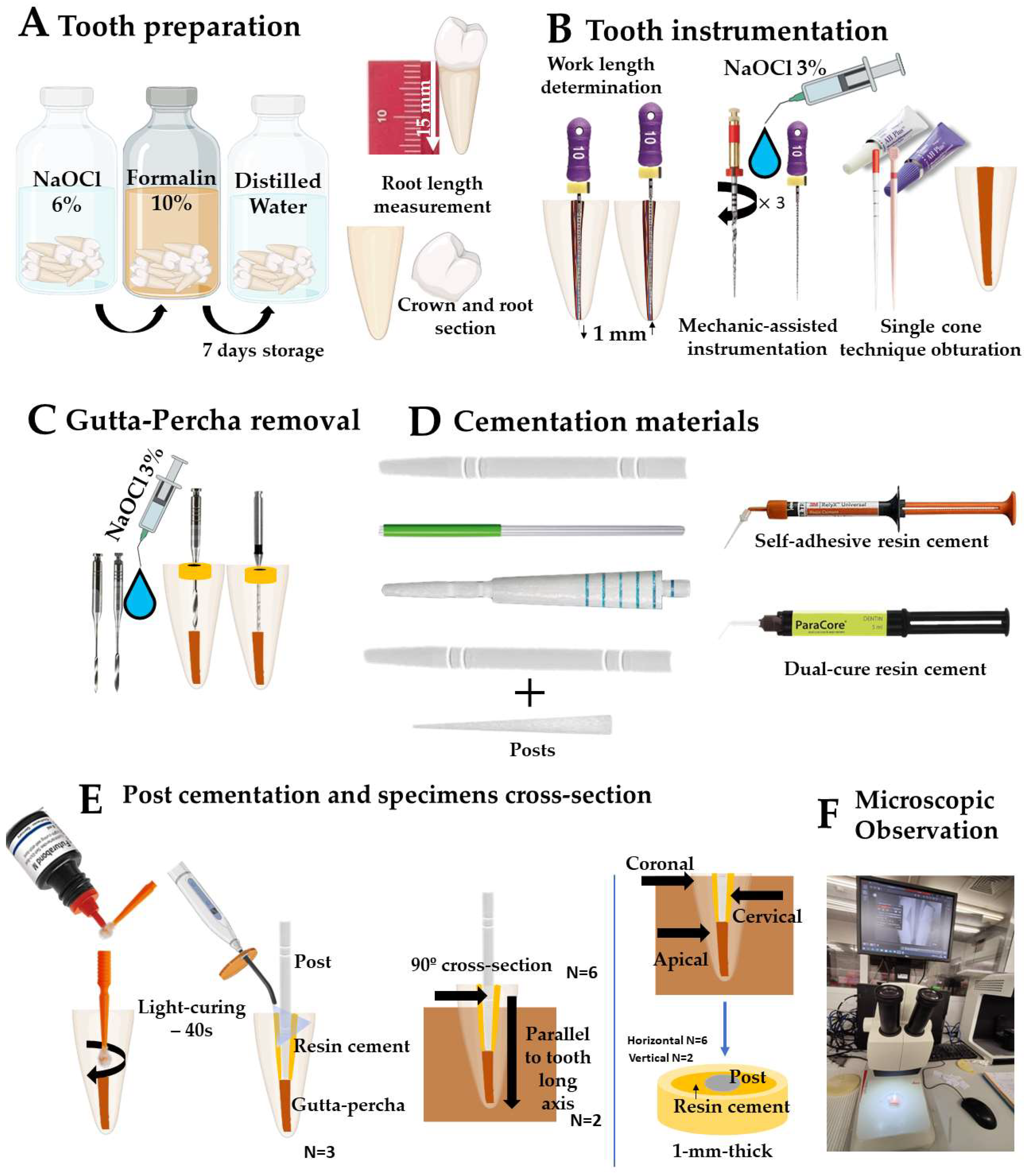
2. Materials and Methods
2.1. Preparation of Specimens
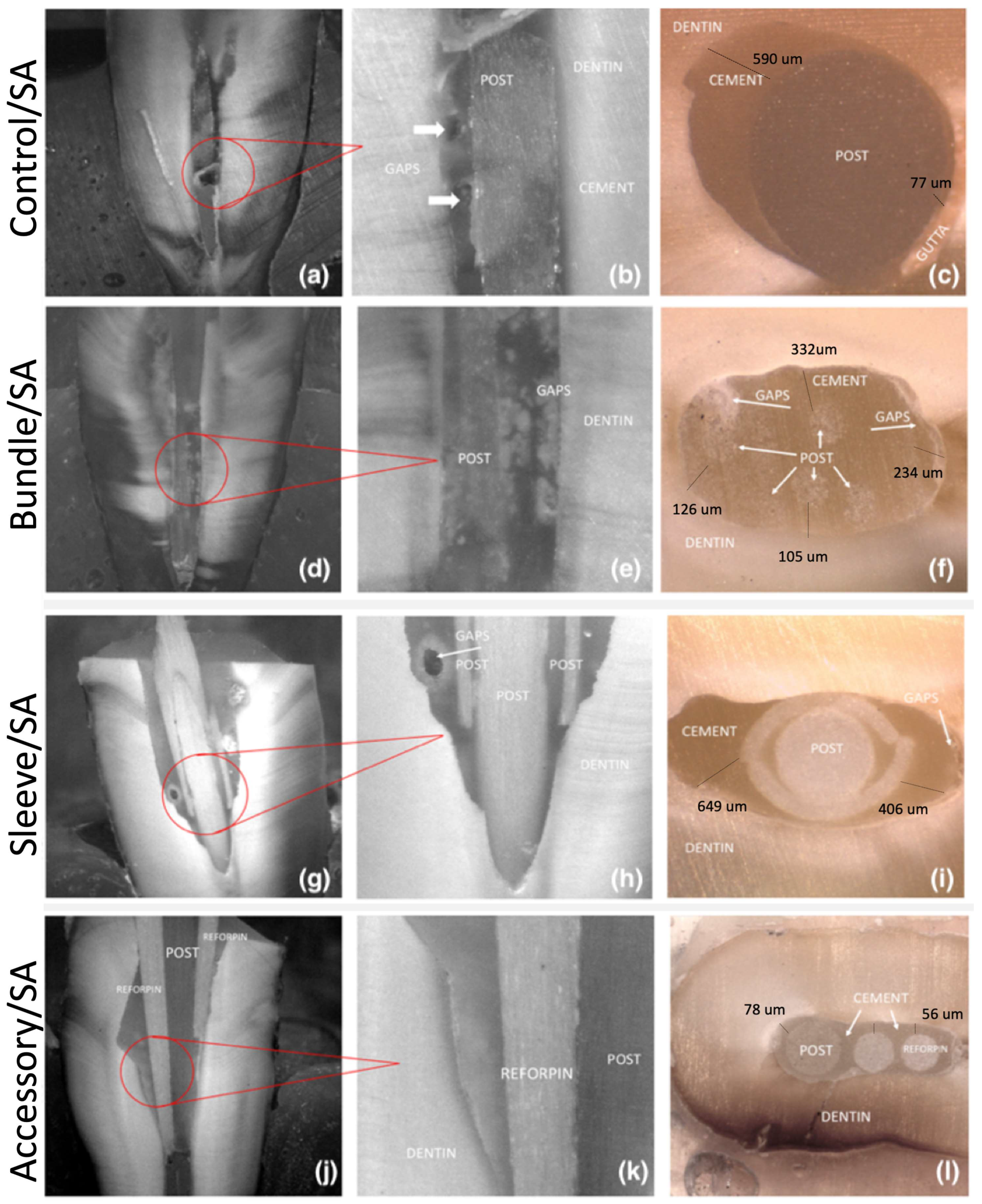
2.2. Microscopic Analysis
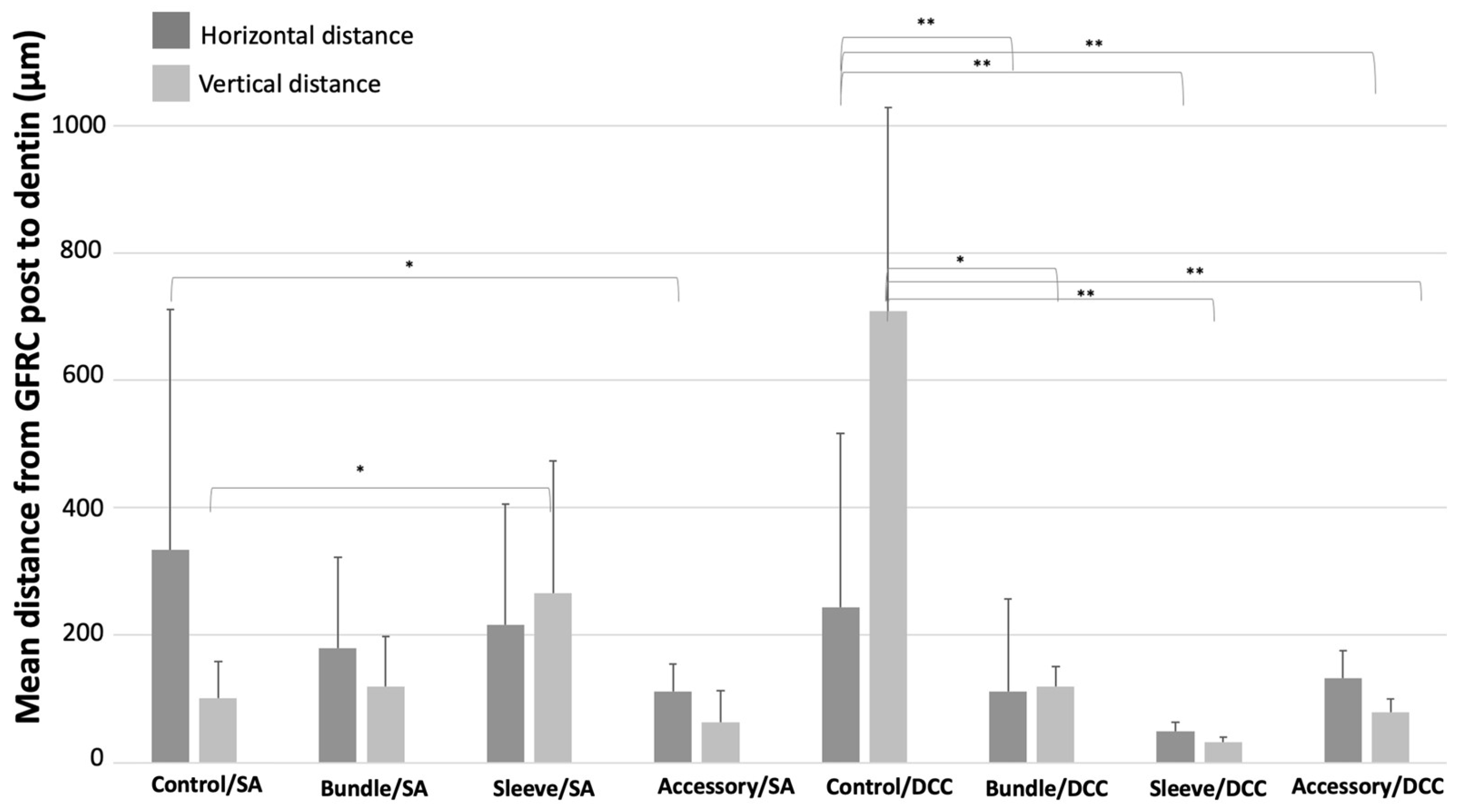
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Landys Borén, D.; Jonasson, P.; Kvist, T. Long-Term Survival of Endodontically Treated Teeth at a Public Dental Specialist Clinic. J. Endod. 2015, 41, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.-L.; Mann, V.; Gulabivala, K. A Prospective Study of the Factors Affecting Outcomes of Non-Surgical Root Canal Treatment: Part 2: Tooth Survival. Int. Endod. J. 2011, 44, 610–625. [Google Scholar] [CrossRef] [PubMed]
- Sartoretto, S.C.; Shibli, J.A.; Javid, K.; Cotrim, K.; Canabarro, A.; Louro, R.S.; Lowenstein, A.; Mourão, C.F.; Moraschini, V. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J. Funct. Biomater. 2023, 14, 142. [Google Scholar] [CrossRef] [PubMed]
- Alkhalidi, E.F. Fracture Resistance of New Fiber Post System (Rebilda GT). Indian J. Forensic Med. Toxicol. 2020, 14, 2632–2638. [Google Scholar] [CrossRef]
- Krastl, G.; Lorch, H.; Zitzmann, N.U.; Addison, O.; Dietrich, T.; Weiger, R. Do Oval Posts Improve Fracture Resistance of Teeth with Oval Root Canals? Dent. Traumatol. 2014, 30, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Hegde, V.; Arora, N. Fracture Resistance of Endodontically Treated Teeth Restored Using Three Different Esthetic Post Systems. J. Oper. Dent. Endod. 2019, 4, 10–13. [Google Scholar] [CrossRef]
- Komabayashi, T.; Ahn, C.; Zhang, S.; Zhu, Q.; Spångberg, L.S.W. Chronologic Comparison of Root Dentin Moisture in Extracted Human Teeth Stored in Formalin, Sodium Azide, and Distilled Water. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, e50–e54. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, G.; Brondani, L.P.; Wandscher, V.F.; Pereira, G.K.R.; Valandro, L.F.; Bergoli, C.D. Influence of Remaining Coronal Thickness and Height on Biomechanical Behavior of Endodontically Treated Teeth: Survival Rates, Load to Fracture and Finite Element Analysis. J. Appl. Oral Sci. 2018, 26, e20170313. [Google Scholar] [CrossRef]
- Rengo, C.; Spagnuolo, G.; Ametrano, G.; Juloski, J.; Rengo, S.; Ferrari, M. Micro-Computerized Tomographic Analysis of Premolars Restored with Oval and Circular Posts. Clin. Oral Investig. 2014, 18, 571–578. [Google Scholar] [CrossRef]
- Fernandes, V.; Silva, A.S.; Carvalho, O.; Henriques, B.; Silva, F.S.; Özcan, M.; Souza, J.C.M. The Resin-Matrix Cement Layer Thickness Resultant from the Intracanal Fitting of Teeth Root Canal Posts: An Integrative Review. Clin. Oral Investig. 2021, 25, 5595–5612. [Google Scholar] [CrossRef]
- Prado, M.; Marques, J.N.; Pereira, G.D.; da Silva, E.M.; Simão, R.A. Evaluation of Different Surface Treatments on Fiber Post Cemented with a Self-Adhesive System. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 77, 257–262. [Google Scholar] [CrossRef]
- Meshni, A.A.; Al Moaleem, M.M.; Mattoo, K.A.; Halboub, E.; Alharisi, S.M.; Shatifi, A.E.; Al Amriee, S.A.; Ghazali, N. Al Radiographic Evaluation of Post-Core Restorations Fabricated by Dental Students at Jazan University. J. Contemp. Dent. Pract. 2018, 19, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, A.; Kishen, A. Antibacterial Nanoparticles in Endodontics: A Review. J. Endod. 2016, 42, 1417–1426. [Google Scholar] [CrossRef]
- Abraham, S.B.; Gopinath, V.K. Root Canal Anatomy of Mandibular First Premolars in an Emirati Subpopulation: A Laboratory Study. Eur. J. Dent. 2015, 9, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Lazari, P.C.; de Carvalho, M.A.; Del Bel Cury, A.A.; Magne, P. Survival of Extensively Damaged Endodontically Treated Incisors Restored with Different Types of Posts-and-Core Foundation Restoration Material. J. Prosthet. Dent. 2018, 119, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Reeh, E.S.; Messer, H.H.; Douglas, W.H. Reduction in Tooth Stiffness as a Result of Endodontic and Restorative Procedures. J. Endod. 1989, 15, 512–516. [Google Scholar] [CrossRef]
- Clark, D.; Khademi, J. Modern Molar Endodontic Access and Directed Dentin Conservation. Dent. Clin. N. Am. 2010, 54, 249–273. [Google Scholar] [CrossRef]
- Sreedevi, S.; Sanjeev, R.; Raghavan, R.; Abraham, A.; Rajamani, T.; Govind, G.K.; Samran, A.; Al-Afandi, M.; Kadour, J.-A.; Kern, M.; et al. Rationale for Low-Modulus Endodontic Posts. J. Endod. 2010, 29, 909–928. [Google Scholar] [CrossRef]
- Da Silveira Teixeira, C.; Santos Felippe, M.C.; Silva-Sousa, Y.T.C.; de Sousa-Neto, M.D. Interfacial Evaluation of Experimentally Weakened Roots Restored with Adhesive Materials and Fibre Posts: An SEM Analysis. J. Dent. 2008, 36, 672–682. [Google Scholar] [CrossRef]
- Santos, T.d.S.A.; Abu Hasna, A.; Abreu, R.T.; Tribst, J.P.M.; de Andrade, G.S.; Borges, A.L.S.; Torres, C.R.G.; Carvalho, C.A.T. Fracture Resistance and Stress Distribution of Weakened Teeth Reinforced with a Bundled Glass Fiber-Reinforced Resin Post. Clin. Oral Investig. 2022, 26, 1725–1735. [Google Scholar] [CrossRef]
- Grandini, S.; Goracci, C.; Monticelli, F.; Tay, F.R.; Ferrari, M. Fatigue Resistance and Structural Characteristics of Fiber Posts: Three-Point Bending Test and SEM Evaluation. Dent. Mater. 2005, 21, 75–82. [Google Scholar] [CrossRef] [PubMed]
- De Souza Guimarães, M.; da Silveira Bueno, C.E.; de Martin, A.S.; Fontana, C.E.; Pelegrine, R.A.; Pinheiro, S.L.; Rocha, D.G.P. In Vitro Evaluation of Bond Strength to Dentin of Two Post Systems: Computer-Aided Design and Computer-Aided Manufacturing Fiber Posts vs. Splendor Single Adjustable Post. J. Contemp. Dent. Pract. 2022, 23, 388–392. [Google Scholar] [CrossRef]
- Carvalho, I.; Marques, T.; Araújo, F.; Azevedo, L.; Donato, H.; Correia, A. Clinical Performance of CAD/CAM Tooth-Supported Ceramic Restorations: A Systematic Review. Int. J. Periodontics Restor. Dent. 2018, 38. [Google Scholar] [CrossRef]
- Ausiello, P.; Ciaramella, S.; Martorelli, M.; Lanzotti, A.; Zarone, F.; Watts, D.; Gloria, A. Mechanical Behavior of Endodontically Restored Canine Teeth: Effects of Ferrule, Post Material and Shape. Dent. Mater. 2017, 33, 1466–1472. [Google Scholar] [CrossRef] [PubMed]
- Sivieri-Araujo, G.; Tanomaru-Filho, M.; Guerreiro-Tanomaru, J.M.; Bortoluzzi, E.A.; Jorge, É.G.; Reis, J.M.D.S.N. Fracture Resistance of Simulated Immature Teeth after Different Intra-Radicular Treatments. Braz. Dent. J. 2015, 26, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, L.M.; de Andrade, A.M.; Machuca, M.F.G.; da Silva, P.M.B.; da Silva, R.V.C.; Veronezi, M.C. Influence of Different Adhesive Systems on the Pull-out Bond Strength of Glass Fiber Posts. J. Appl. Oral Sci. 2008, 16, 232–235. [Google Scholar] [CrossRef]
- Moosavi, H.; Maleknejad, F.; Kimyai, S. Fracture Resistance of Endodontically-Treated Teeth Restored Using Three Root-Reinforcement Methods. J. Contemp. Dent. Pract. 2008, 9, 30–37. [Google Scholar] [PubMed]
- Christodoulou, A.; Mikrogeorgis, G.; Vouzara, T.; Papachristou, K.; Angelopoulos, C.; Nikolaidis, N.; Pitas, I.; Lyroudia, K. A New Methodology for the Measurement of the Root Canal Curvature and Its 3D Modification after Instrumentation. Acta Odontol. Scand. 2018, 76, 488–492. [Google Scholar] [CrossRef]
- Mosharraf, R.; Baghaei Yazdi, N. Comparative Evaluation of Effects of Different Surface Treatment Methods on Bond Strength between Fiber Post and Composite Core. J. Adv. Prosthodont. 2012, 4, 103–108. [Google Scholar] [CrossRef]
- Skapska, A.; Komorek, Z.; Cierech, M.; Mierzwinska-Nastalska, E. Comparison of Mechanical Properties of a Self-Adhesive Composite Cement and a Heated Composite Material. Polymers 2022, 14, 2686. [Google Scholar] [CrossRef]
- Al-Nuaimi, N.; Ciapryna, S.; Chia, M.; Patel, S.; Mannocci, F. A Prospective Study on the Effect of Coronal Tooth Structure Loss on the 4-Year Clinical Survival of Root Canal Retreated Teeth and Retrospective Validation of the Dental Practicality Index. Int. Endod. J. 2020, 53, 1040–1049. [Google Scholar] [CrossRef] [PubMed]
- Samran, A.; El Bahra, S.; Kern, M. The Influence of Substance Loss and Ferrule Height on the Fracture Resistance of Endodontically Treated Premolars. An in Vitro Study. Dent. Mater. 2013, 29, 1280–1286. [Google Scholar] [CrossRef]
- Fuss, Z.; Lustig, J.; Tamse, A. Prevalence of Vertical Root Fractures in Extracted Endodontically Treated Teeth. Int. Endod. J. 1999, 32, 283–286. [Google Scholar] [CrossRef]
- Signore, A.; Kaitsas, V.; Ravera, G.; Angiero, F.; Benedicenti, S. Clinical Evaluation of an Oval-Shaped Prefabricated Glass Fiber Post in Endodontically Treated Premolars Presenting an Oval Root Canal Cross-Section: A Retrospective Cohort Study. Int. J. Prosthodont. 2011, 24, 255–263. [Google Scholar] [PubMed]
- Eid, R.Y.; Koken, S.; Baba, N.Z.; Ounsi, H.; Ferrari, M.; Salameh, Z. Effect of Fabrication Technique and Thermal Cycling on the Bond Strength of CAD/CAM Milled Custom Fit Anatomical Post and Cores: An In Vitro Study. J. Prosthodont. 2019, 28, 898–905. [Google Scholar] [CrossRef] [PubMed]
- Silva, N.; Aguiar, G.; Rodrigues, M.; Bicalho, A.; Soares, P.; Verissimo, C.; Soares, C. Effect of Resin Cement Porosity on Retention of Glass-Fiber Posts to Root Dentin: An Experimental and Finite Element Analysis. Braz. Dent. J. 2015, 26, 630–636. [Google Scholar] [CrossRef]
- Perez, B.E.M.; Barbosa, S.H.; Melo, R.M.; Zamboni, S.C.; Özcan, M.; Valandro, L.F.; Bottino, M.A. Does the Thickness of the Resin Cement Affect the Bond Strength of a Fiber Post to the Root Dentin? Int. J. Prosthodont. 2006, 19, 606–609. [Google Scholar]
- Alaboodi, R.A.; Srivastava, S.; Javed, M.Q. Cone-Beam Computed Tomographic Analysis of Root Canal Morphology of Permanent Mandibular Incisors—Prevalence and Related Factors. Pak. J. Med. Sci. 2022, 38, 1563. [Google Scholar] [CrossRef]
- Warol, F.; Vieira, V.T.L. Comparison of Conventional Fiberglass and Splendor Sap Post Systems. Res. Soc. Dev. 2022, 11, e167111130991. [Google Scholar] [CrossRef]
- Kılınç, H.I.; Aslan, T.; Kılıç, K.; Er, Ö.; Esim, E.; Yıldırım, Ş. Fracture Resistance of Teeth with Oval Canal Morphology Restored Using Oval and Circular Posts. J. Oral Sci. 2016, 58, 339–345. [Google Scholar] [CrossRef]
- Bonfante, G.; Kaizer, O.B.; Pegoraro, L.F.; do Valle, A.L. Fracture Strength of Teeth with Flared Root Canals Restored with Glass Fibre Posts. Int. Dent. J. 2007, 57, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-S.; Lee, J.-S.; Park, J.-W.; Chung, W.-G.; Choi, E.-H.; Lee, Y. Comparison of Push-out Bond Strength of Fiber-Reinforced Composite Resin Posts According to Cement Thickness. J. Prosthet. Dent. 2017, 118, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, G.; Ferrari Cagidiaco, E.; Lo Giudice, R.; Puleio, F.; Nicita, F.; Calapaj, M. Evaluation of Mechanical Properties of a Hollow Endodontic Post by Three Point Test and SEM Analysis: A Pilot Study. Materials 2019, 12, 1983. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, S.; Karki, S.; Agrawal, N.; Vikram, M.; Singh, V.; Shrestha, A. Prevalence of Different Types of Apical Root Canal Morphology and Their Treatment Recommendations in an Institute. JNMA J. Nepal. Med. Assoc. 2018, 56, 616–620. [Google Scholar] [CrossRef] [PubMed]
- Fidalgo-Pereira, R.; Torres, O.; Carvalho, Ó.; Silva, F.S.; Catarino, S.O.; Özcan, M.; Souza, J.C.M. A Scoping Review on the Polymerization of Resin-Matrix Cements Used in Restorative Dentistry. Materials 2023, 16, 1560. [Google Scholar] [CrossRef] [PubMed]
- Lise, D.P.; Van Ende, A.; De Munck, J.; Yoshihara, K.; Nagaoka, N.; Cardoso Vieira, L.C.; Van Meerbeek, B. Light Irradiance through Novel CAD-CAM Block Materials and Degree of Conversion of Composite Cements. Dent. Mater. 2018, 34, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L.; Stansbury, J.W.; Burke, F.J. Self-Adhesive Resin Cements—Chemistry, Properties and Clinical Considerations. J. Oral Rehabil. 2011, 38, 295–314. [Google Scholar] [CrossRef]
- Aguiar, T.R.; Di Francescantonio, M.; Bedran-Russo, A.K.; Giannini, M. Inorganic Composition and Filler Particles Morphology of Conventional and Self-Adhesive Resin Cements by SEM/EDX. Microsc. Res. Tech. 2012, 75, 1348–1352. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.; Fidalgo-Pereira, R.C.; Torres, O.; Silva, F.; Henriques, B.; Özcan, M.; Souza, J.C.M. Toxicity of Resin-Matrix Cements in Contact with Fibroblast or Mesenchymal Cells. Odontology 2022, 111, 310–327. [Google Scholar] [CrossRef] [PubMed]
- Alhajj, M.N.; Salim, N.S.; Johari, Y.; Syahrizal, M.; Abdul-Muttlib, N.A.; Ariffin, Z. Push-out Bond Strength of Two Types of Dental Post Luted with Two Types of Cement at Two Different Root Levels. Acta Stomatol. Croat. 2020, 54, 263–272. [Google Scholar] [CrossRef]
- Amiri, E.M.; Balouch, F.; Atri, F. Effect of Self-Adhesive and Separate Etch Adhesive Dual Cure Resin Cements on the Bond Strength of Fiber Post to Dentin at Different Parts of the Root. J. Dent. 2017, 14, 153–158. [Google Scholar]
- Liu, C.; Liu, H.; Qian, Y.-T.; Zhu, S.; Zhao, S.-Q. The Influence of Four Dual-Cure Resin Cements and Surface Treatment Selection to Bond Strength of Fiber Post. Int. J. Oral Sci. 2014, 6, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Nima, B.G.; Makishi, P.; Fronza, B.; Ferreira, P.; Braga, R.; Reis, A.; Giannini, M. Polymerization Kinetics, Shrinkage Stress, and Bond Strength to Dentin of Conventional and Self-Adhesive Resin Cements. J. Adhes. Dent. 2022, 24, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Santi, M.R.; Lins, R.B.E.; Sahadi, B.O.; Soto-Montero, J.R.; Martins, L.R.M. Comparison of the Mechanical Properties and Push-out Bond Strength of Self-Adhesive and Conventional Resin Cements on Fiber Post Cementation. Oper. Dent. 2022, 47, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Kinney, J.H.; Marshall, S.J.; Marshall, G.W. The Mechanical Properties of Human Dentin: A Critical Review and Re-Evaluation of the Dental Literature. Crit. Rev. Oral Biol. Med. 2003, 14, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Akcay, I.; Sen, B.H. The Effect of Surfactant Addition to EDTA on Microhardness of Root Dentin. J. Endod. 2012, 38, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Souza, E.M.; Quadros, J.d.R.P.; Silva, E.J.N.L.; De-Deus, G.; Belladonna, F.G.; Maia-Filho, E.M. Volume and/or Time of NaOCl Influences the Fracture Strength of Endodontically Treated Bovine Teeth. Braz. Dent. J. 2019, 30, 31–35. [Google Scholar] [CrossRef]
- Ballal, N.V.; Mala, K.; Bhat, K.S. Evaluation of the Effect of Maleic Acid and Ethylenediaminetetraacetic Acid on the Microhardness and Surface Roughness of Human Root Canal Dentin. J. Endod. 2010, 36, 1385–1388. [Google Scholar] [CrossRef] [PubMed]
- Dotto, L.; Sarkis Onofre, R.; Bacchi, A.; Rocha Pereira, G.K. Effect of Root Canal Irrigants on the Mechanical Properties of Endodontically Treated Teeth: A Scoping Review. J. Endod. 2020, 46, 596–604.e3. [Google Scholar] [CrossRef]
- Mao, H.; Chen, Y.; Yip, K.H.-K.; Smales, R.J. Effect of Three Radicular Dentine Treatments and Two Luting Cements on the Regional Bond Strength of Quartz Fibre Posts. Clin. Oral Investig. 2011, 15, 869–878. [Google Scholar] [CrossRef]
- Faria-e-Silva, A.L.; Menezes, M.d.S.; Silva, F.P.; dos Reis, G.R.; de Moraes, R.R. Intra-Radicular Dentin Treatments and Retention of Fiber Posts with Self-Adhesive Resin Cements. Braz. Oral Res. 2013, 27, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, N.S.; de Souza, L.C.; Feitosa, V.P.; Loguercio, A.D.; D’Arcangelo, C.; Sauro, S.; Saboia, V.d.P.A. Effect of Different Conditioning/Deproteinization Protocols on the Bond Strength and Degree of Conversion of Self-Adhesive Resin Cements Applied to Dentin. Int. J. Adhes. Adhes. 2018, 81, 98–104. [Google Scholar] [CrossRef]
- Baena, E.; Flores, A.; Ceballos, L. Influence of Root Dentin Treatment on the Push-out Bond Strength of Fiber Posts. Odontology 2017, 105, 170–177. [Google Scholar] [CrossRef] [PubMed]
- De Souza, L.C.; Rodrigues, N.S.; Feitosa, V.P.; Luque-Martinez, I.V.; Loguercio, A.D.; de Saboia, V.P.A. Deproteinization Stabilises Dentin Bonding of Self-Adhesive Resin Cements after Thermocycling. Int. J. Adhes. Adhes. 2016, 66, 53–58. [Google Scholar] [CrossRef]


| Group; Material (Brand, Manufacturer, Country) | Organic Matrix (wt.%) | Inorganic Fillers (wt.%) | Filler Shape and Type | Elastic Modulus and Fracture Load |
|---|---|---|---|---|
| Control group, Standard GFRC post (RebildaTM, VOCO, Cuxhaven, Germany) | UDMA; DMA (20 wt.%) [1] | 70–80 | Glass fibers (10–20 μm) with SiO2, SnO2, B2O3, Al2O3 alkali oxides Coronal diameter: 2 mm Apical diameter: 1.02 1.5 mm diameter | E: 18–30 GPa; F: 400–600 N |
| Bundle GFRC post (Rebilda GTTM, VOCO, Cuxhaven, Germany) | UDMA; DMA (20 wt.%) | 70–80 [1] | Glass fibers (10–20 μm) with SiO2, SnO2, B2O3, Al2O3 alkali oxides 12 single narrow GFRC filaments 1.4 mm diameter Single GFRC filament diameter: 0.3 mm [2] | E: 31.5 GPa; F: 1040 N |
| Sleeve-system GFRC (Splendor SAPTM, Angelus, Londrina, Brazil) | Epoxy resin (19–20 wt.%) | 50–80 | Glass fibers, type E or E-glass, with SiO2 (55–65%),CaO (9–25%), B2O3, Al2O3 (15–30%) alkali oxide metals a [3] Main Post Diameter: 1.0 mm Sleeve Diameter: 1.4 mm Sleeve taper: 0.8 mm | E: 37 GPa [4]; F: 835.9 N |
| Accessory GFRC posts (ReforpinTM, Angelus, Londrina, Brazil) | Epoxy resin (19–20 wt.%) | 80 | Glass fibers, type E or E-glass, with SiO2 (55–65%),CaO (9–25%), B2O3,Al2O3 (15–30%) alkali oxides metals a [3] Diameter: 1.3 mm Length: 14 mm | E: 35–45 GPa; F: 569.5 N |
| Self-adhesive resin cement (RelyX U200TM, 3M, Maplewood, MN, USA) | TEGDMA, 3-propanediyl dimethacrylate and phosphorus oxid, propyl and phenyltrimethoxy silane, propenoic acid, 2-methyl-, 2-hydroxy-1, 3-propanediyl dimethacrylate and phosphorus oxide and phosphoric acid groups (28 wt.%) [5,6] | 72 [5] | Trisilane-treated silica, powdered glass, chemical glass oxides (non-fibrous), glass fillers, glass fibers, acetic acid, copper sodium monohydrate [7] | E: 15.99 GPa; FS: 81.29 MPa [8]; VMH: 58.64 HV (cervical) and 56.1 HV (apical) [9] |
| Group CDD, Dual-cured resin cement (ParacoreTM, Coltene Whaledent, Cuyahoga Falls, OH, USA) | Bis-GMA, UDMA, TEGDMA, DDDMA, TMPTMA, BHT, dibenzyl peroxide, CQ, accelerators [10] | 74 [11] | Amorphous silica, zinc oxide, barium glass, and sodium fluoride particles Particle size: 0.01–5 μm [10,12] | E: 9.2 GPa [10]; FS: 120 MPa [11] BS: 280 MPa; VMH, 43.2 HV [13] |
| (ParabondTM, Coltene Whaledent, Cuyahoga Falls, OH, USA) | Adhesive A: Methacrylate (HEMA) (39%), Maleic acid (1.5%), Benzoyl peroxide (1.5%). Adhesive B: Ethanol (80%), Water and Initiators. [14,15] PH: 0.9–1.3 [16] | 52 | Micro-scale barium glass ceramic and zirconium glass ceramic micro-scale particles at 1 μm Nano-scale SiO2 particles at around 20–40 nm [16] | E: -; FS: -; SBS: 5.44 MPa |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, V.; Fidalgo-Pereira, R.; Edwards, J.; Silva, F.; Özcan, M.; Carvalho, Ó.; Souza, J.C.M. Fitting of Different Intraradicular Composite Posts to Oval Tooth Root Canals: A Preliminary Assessment. Materials 2024, 17, 2520. https://doi.org/10.3390/ma17112520
Fernandes V, Fidalgo-Pereira R, Edwards J, Silva F, Özcan M, Carvalho Ó, Souza JCM. Fitting of Different Intraradicular Composite Posts to Oval Tooth Root Canals: A Preliminary Assessment. Materials. 2024; 17(11):2520. https://doi.org/10.3390/ma17112520
Chicago/Turabian StyleFernandes, Valter, Rita Fidalgo-Pereira, Jane Edwards, Filipe Silva, Mutlu Özcan, Óscar Carvalho, and Júlio C. M. Souza. 2024. "Fitting of Different Intraradicular Composite Posts to Oval Tooth Root Canals: A Preliminary Assessment" Materials 17, no. 11: 2520. https://doi.org/10.3390/ma17112520










