Suitability of Direct Resin Composites in Restoring Endodontically Treated Teeth (ETT)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Resin Composites and Adhesives
2.2. Three-Point Bending Flexural Test (Elastic Modulus) of Resin Composites
2.3. Compression–Shear Test (Shear Bond Strength) of Resin Composite Samples Bonded to Dentin Discs
2.4. Endodontic Treatment and Direct Occlusal Restoration
2.5. Occlusal Fracture Load (Fmax) and Fracture Patterns of Endodontically Treated Teeth Restored with Direct Resin Composite Fillings
- Group 1.
- fractures involving a small portion of the coronal tooth tissue.
- Group 2.
- fractures involving a small portion of the coronal tooth tissue and cohesive failure of the restoration.
- Group 3.
- fractures involving the tooth tissue, cohesive and/or adhesive failure of the restoration, with root involvement that can be restored in association with periodontal surgery.
- Group 4.
- severe root and crown fracture, which determine extraction of the tooth (catastrophic fracture).
2.6. Statistical Analysis
3. Results
3.1. Three-Point Bending Flexural Test (Elastic Modulus) of Resin-Composites
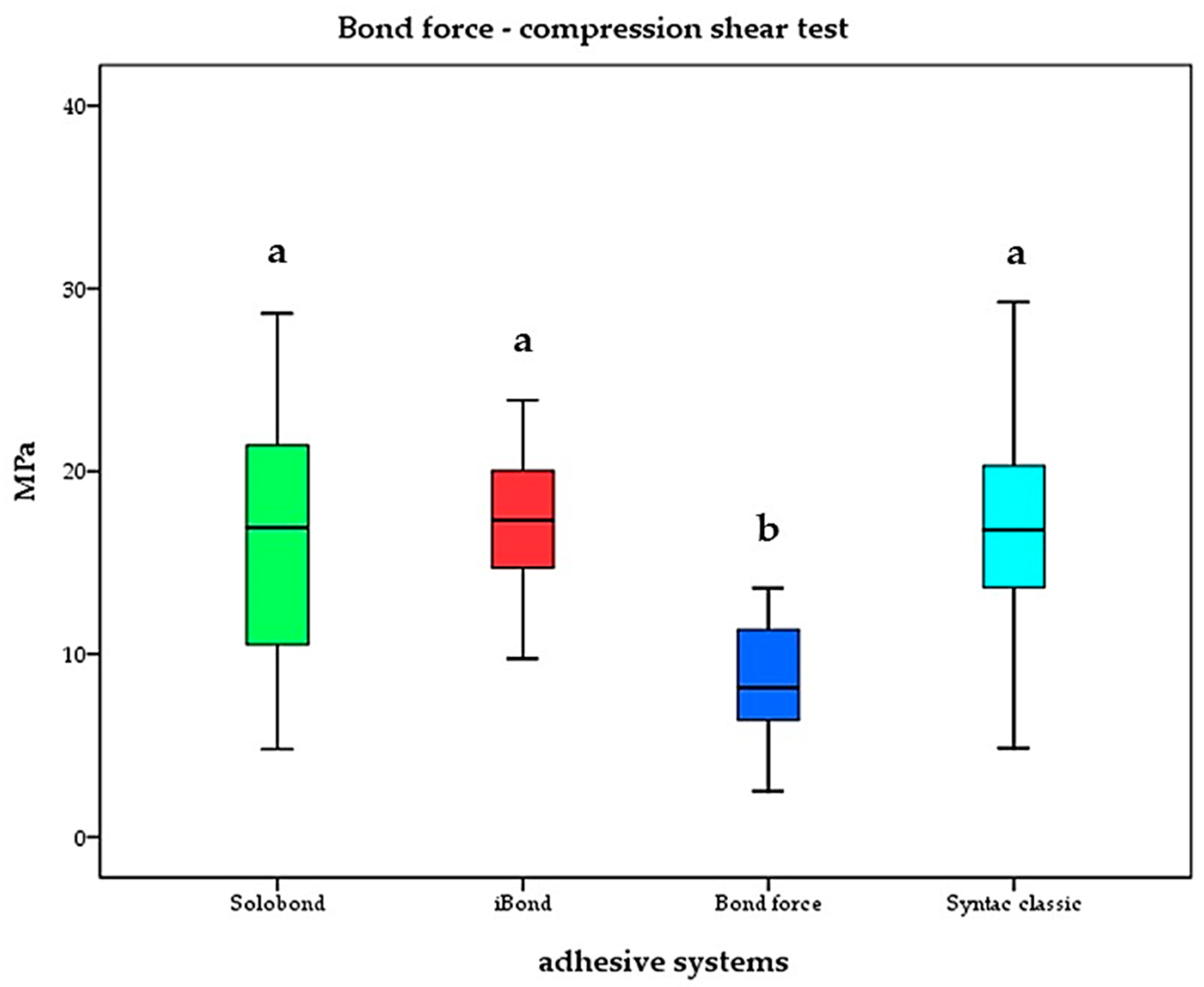
3.2. Compression–Shear Test (Shear Bond Strength) of Resin Composite Samples Bonded to Dentin Discs
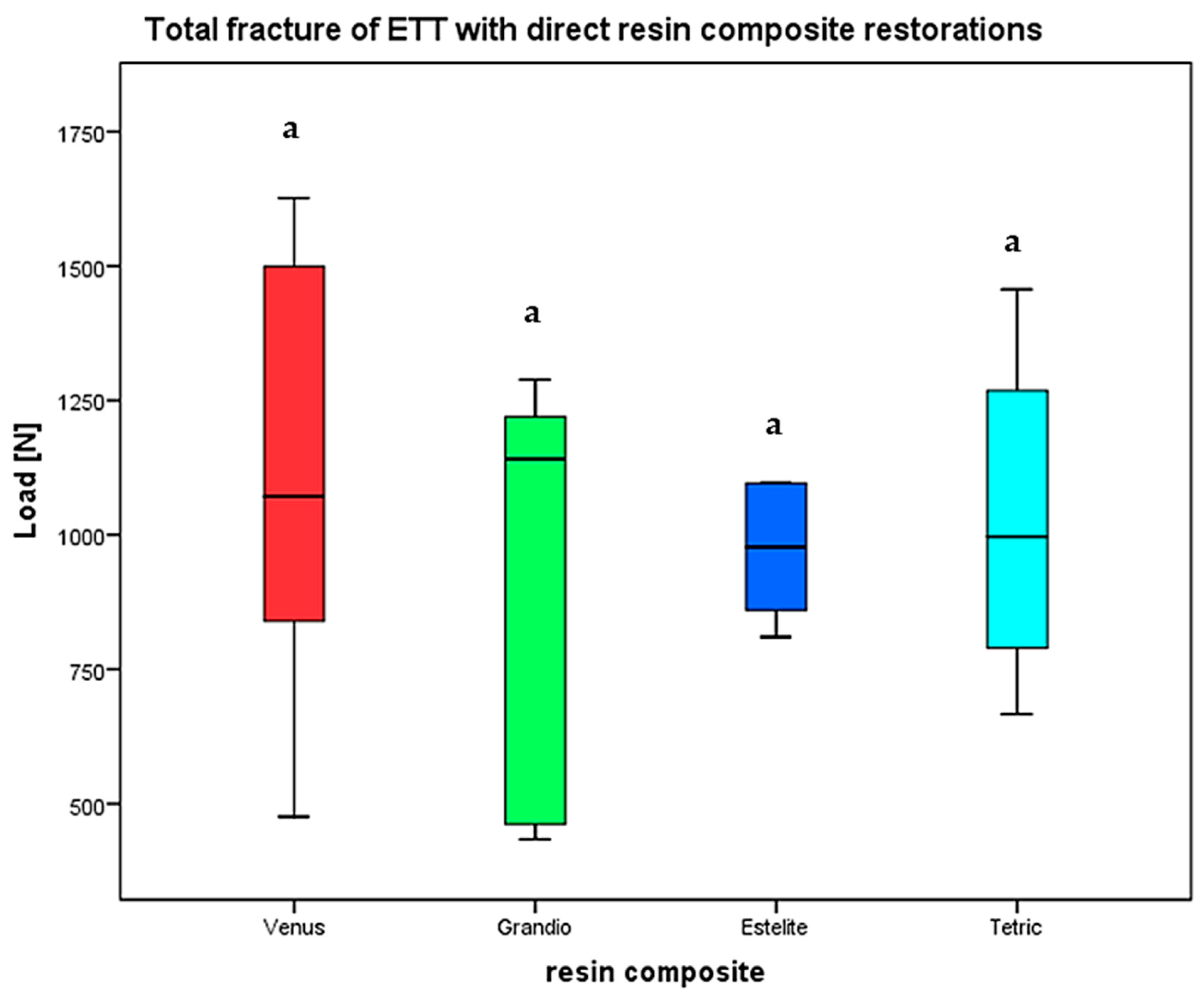
3.3. Occlusal Fracture Load (Fmax) and Fracture Patterns of Endodontically Treated Teeth Restored with Direct Resin Composite Fillings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aslan, T.; Sagsen, B.; Er, Ö.; Ustun, Y.; Cinar, F. Evaluation of fracture resistance in root canal-treated teeth restored using different techniques. Niger. J. Clin. Pract. 2018, 21, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Dietschi, D.; Duc, O.; Krejci, I.; Sadan, A. Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature—Part 1. Composition and micro- and macrostructure alterations. Quintessence Int. 2007, 38, 733–743. [Google Scholar] [PubMed]
- Ferrari, M.; Pontoriero, D.I.K.; Ferrari Cagidiaco, E.; Carboncini, F. Restorative difficulty evaluation system of endodontically treated teeth. J. Esthet. Restor. Dent. 2022, 34, 65–80. [Google Scholar] [CrossRef] [PubMed]
- Haupt, F.; Wiegand, A.; Kanzow, P. Risk Factors for and Clinical Presentations Indicative of Vertical Root Fracture in Endodontically Treated Teeth: A Systematic Review and Meta-analysis. J. Endod. 2023, 49, 940–952. [Google Scholar] [CrossRef] [PubMed]
- Bhuva, B.; Giovarruscio, M.; Rahim, N.; Bitter, K.; Mannocci, F. The restoration of root filled teeth: A review of the clinical literature. Int. Endod. J. 2021, 54, 509–535. [Google Scholar] [CrossRef]
- Bialy, M.; Targonska, S.; Szust, A.; Wiglusz, R.J.; Dobrzynski, M. In Vitro Fracture Resistance of Endodontically Treated Premolar Teeth Restored with Prefabricated and Custom-Made Fibre-Reinforced Composite Posts. Materials 2021, 14, 6214. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Winter, J.; Dudek, M.C.; Naumann, M.; Amend, S.; Braun, A.; Krämer, N.; Roggendorf, M.J. Post-Fatigue Fracture and Marginal Behavior of Endodontically Treated Teeth: Partial Crown vs. Full Crown vs. Endocrown vs. Fiber-Reinforced Resin Composite. Materials 2021, 14, 7733. [Google Scholar] [CrossRef] [PubMed]
- Kanzler Abdel Raouf, V.; Jockusch, J.; Al-Haj Husain, N.; Dydyk, N.; Özcan, M. Push-Out Bond Strength Assessment of Different Post Systems at Different Radicular Levels of Endodontically Treated Teeth. Materials 2022, 15, 5134. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.A.; Lazari, P.C.; Gresnigt, M.; Del Bel Cury, A.A.; Magne, P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz. Oral. Res. 2018, 32, e74. [Google Scholar] [CrossRef]
- de Kuijper, M.; Cune, M.S.; Özcan, M.; Gresnigt, M.M.M. Clinical performance of direct composite resin versus indirect restorations on endodontically treated posterior teeth: A systematic review and meta-analysis. J. Prosthet. Dent. 2023, 130, 295–306. [Google Scholar] [CrossRef]
- Heyder, M.; Kranz, S.; Beck, J.; Wettemann, M.; Hennig, C.L.; Schulze-Späte, U.; Sigusch, B.W.; Reise, M. Influence of Layer Thickness and Shade on the Transmission of Light through Contemporary Resin Composites. Materials 2024, 17, 1554. [Google Scholar] [CrossRef]
- Montag, R.; Dietz, W.; Nietzsche, S.; Lang, T.; Weich, K.; Sigusch, B.W.; Gaengler, P. Clinical and Micromorphologic 29-year Results of Posterior Composite Restorations. J. Dent. Res. 2018, 97, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Pflaum, T.; Kranz, S.; Montag, R.; Güntsch, A.; Völpel, A.; Mills, R.; Jandt, K.; Sigusch, B. Clinical long-term success of contemporary nano-filled resin composites in class I and II restorations cured by LED or halogen light. Clin. Oral. Investig. 2018, 22, 1651–1662. [Google Scholar] [CrossRef] [PubMed]
- Sigusch, B.W.; Pflaum, T.; Völpel, A.; Gretsch, K.; Hoy, S.; Watts, D.C.; Jandt, K.D. Resin-composite cytotoxicity varies with shade and irradiance. Dent. Mater. 2012, 28, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Sigusch, B.W.; Völpel, A.; Braun, I.; Uhl, A.; Jandt, K.D. Influence of different light curing units on the cytotoxicity of various dental composites. Dent. Mater. 2007, 23, 1342–1348. [Google Scholar] [CrossRef]
- Tekçe, N.; Aydemir, S.; Demirci, M.; Tuncer, S.; Sancak, E.; Baydemir, C. Clinical Performance of Direct Posterior Composite Restorations with and without Short Glass-fiber-reinforced Composite in Endodontically Treated Teeth: 3-year Results. J. Adhes. Dent. 2020, 22, 127–137. [Google Scholar] [CrossRef]
- Mergulhão, V.A.; de Mendonça, L.S.; de Albuquerque, M.S.; Braz, R. Fracture Resistance of Endodontically Treated Maxillary Premolars Restored with Different Methods. Oper. Dent. 2019, 44, E1–E11. [Google Scholar] [CrossRef]
- Comba, A.; Baldi, A.; Carossa, M.; Michelotto Tempesta, R.; Garino, E.; Llubani, X.; Rozzi, D.; Mikonis, J.; Paolone, G.; Scotti, N. Post-Fatigue Fracture Resistance of Lithium Disilicate and Polymer-Infiltrated Ceramic Network Indirect Restorations over Endodontically-Treated Molars with Different Preparation Designs: An In-Vitro Study. Polymers 2022, 14, 5084. [Google Scholar] [CrossRef] [PubMed]
- Gerogianni, P.; Lien, W.; Bompolaki, D.; Verrett, R.; Haney, S.; Mattie, P.; Johnson, R. Fracture Resistance of Pressed and Milled Lithium Disilicate Anterior Complete Coverage Restorations Following Endodontic Access Preparation. J. Prosthodont. 2019, 28, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Krifka, S.; Anthofer, T.; Fritzsch, M.; Hiller, K.A.; Schmalz, G.; Federlin, M. Ceramic inlays and partial ceramic crowns: Influence of remaining cusp wall thickness on the marginal integrity and enamel crack formation in vitro. Oper. Dent. 2009, 34, 32–42. [Google Scholar] [CrossRef]
- ISO 4049:2019; Dentistry—Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2019.
- ISO 3630-1:2019; Dentistry—Endodontic Instruments—Part 1: General Requirements. ISO: Geneva, Switzerland, 2019.
- Burke, F.J. Tooth fracture in vivo and in vitro. J. Dent. 1992, 20, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.V.; Santos-Filho, P.C.; Martins, L.R.; Soares, C.J. Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part I: Fracture resistance and fracture mode. J. Prosthet. Dent. 2008, 99, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Shibasaki, S.; Takamizawa, T.; Nojiri, K.; Imai, A.; Tsujimoto, A.; Endo, H.; Suzuki, S.; Suda, S.; Barkmeier, W.W.; Latta, M.A.; et al. Polymerization Behavior and Mechanical Properties of High-Viscosity Bulk Fill and Low Shrinkage Resin Composites. Oper. Dent. 2017, 42, E177–E187. [Google Scholar] [CrossRef] [PubMed]
- Bar-On, B.; Wagner, H.D. Elastic modulus of hard tissues. J. Biomech. 2012, 45, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Kucher, M.; Dannemann, M.; Modler, N.; Bernhard, M.R.; Hannig, C.; Weber, M.T. Mapping of the Micro-Mechanical Properties of Human Root Dentin by Means of Microindentation. Materials 2021, 14, 505. [Google Scholar] [CrossRef] [PubMed]
- Rees, J.S.; Jacobsen, P.H.; Hickman, J. The elastic modulus of dentine determined by static and dynamic methods. Clin. Mater. 1994, 17, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Benetti, A.R.; Peutzfeldt, A.; Lussi, A.; Flury, S. Resin composites: Modulus of elasticity and marginal quality. J. Dent. 2014, 42, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- El-Safty, S.; Akhtar, R.; Silikas, N.; Watts, D.C. Nanomechanical properties of dental resin-composites. Dent. Mater. 2012, 28, 1292–1300. [Google Scholar] [CrossRef] [PubMed]
- Niem, T.; Frankenberger, R.; Amend, S.; Wöstmann, B.; Krämer, N. Damping Behaviour and Mechanical Properties of Restorative Materials for Primary Teeth. Materials 2022, 15, 7698. [Google Scholar] [CrossRef]
- Amsler, F.; Peutzfeldt, A.; Lussi, A.; Flury, S. Bond Strength of Resin Composite to Dentin with Different Adhesive Systems: Influence of Relative Humidity and Application Time. J. Adhes. Dent. 2015, 17, 249–256. [Google Scholar] [CrossRef]
- Chasqueira, A.F.; Arantes-Oliveira, S.; Portugal, J. Bonding Performance of Simplified Dental Adhesives with Three Application Protocols: An 18-month In Vitro Study. J. Adhes. Dent. 2020, 22, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Harnirattisai, C.; Roengrungreang, P.; Rangsisiripaiboon, U.; Senawongse, P. Shear and micro-shear bond strengths of four self-etching adhesives measured immediately and 24 hours after application. Dent. Mater. J. 2012, 31, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, H.A.; Al-Ibraheemi, Z.A.; Hanoon, Z.A.; Haider, J. Evaluation of Shear Bond Strength of Resin-Based Composites to Biodentine with Three Types of Seventh-Generation Bonding Agents: An In Vitro Study. Int. J. Dent. 2022, 2022, 2830299. [Google Scholar] [CrossRef] [PubMed]
- Beloica, M.; Goracci, C.; Carvalho, C.A.; Radovic, I.; Margvelashvili, M.; Vulicevic, Z.R.; Ferrari, M. Microtensile vs microshear bond strength of all-in-one adhesives to unground enamel. J. Adhes. Dent. 2010, 12, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Kusakabe, S.; Rawls, H.R.; Hotta, M. Relationship between thin-film bond strength as measured by a scratch test, and indentation hardness for bonding agents. Dent. Mater. 2016, 32, e55–e62. [Google Scholar] [CrossRef] [PubMed]
- Lorenzoni, E.S.F.; Pamato, S.; Kuga, M.C.; Só, M.V.; Pereira, J.R. Bond strength of adhesive resin cement with different adhesive systems. J. Clin. Exp. Dent. 2017, 9, e96–e100. [Google Scholar] [CrossRef] [PubMed]
- Steiner, R.; Edelhoff, D.; Stawarczyk, B.; Dumfahrt, H.; Lente, I. Effect of Dentin Bonding Agents, Various Resin Composites and Curing Modes on Bond Strength to Human Dentin. Materials 2019, 12, 3395. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Yoshihara, K.; Van Landuyt, K.; Yoshida, Y.; Peumans, M. From Buonocore’s Pioneering Acid-Etch Technique to Self-Adhering Restoratives. A Status Perspective of Rapidly Advancing Dental Adhesive Technology. J. Adhes. Dent. 2020, 22, 7–34. [Google Scholar] [CrossRef]
- Vieira, B.R.; Dantas, E.L.A.; Cavalcanti, Y.W.; Santiago, B.M.; Sousa, F.B. Comparison of Self-Etching Adhesives and Etch-and-Rinse Adhesives on the Failure Rate of Posterior Composite Resin Restorations: A Systematic Review and Meta-Analysis. Eur. J. Dent. 2022, 16, 258–265. [Google Scholar] [CrossRef]
- Moezizadeh, M.; Mokhtari, N. Fracture resistance of endodontically treated premolars with direct composite restorations. J. Conserv. Dent. 2011, 14, 277–281. [Google Scholar] [CrossRef]
- Kassis, C.; Khoury, P.; Mehanna, C.Z.; Baba, N.Z.; Bou Chebel, F.; Daou, M.; Hardan, L. Effect of Inlays, Onlays and Endocrown Cavity Design Preparation on Fracture Resistance and Fracture Mode of Endodontically Treated Teeth: An In Vitro Study. J. Prosthodont. 2021, 30, 625–631. [Google Scholar] [CrossRef]
- Chan, T.; Küçükkaya Eren, S.; Wong, R.; Parashos, P. In vitro fracture strength and patterns in root-filled teeth restored with different base materials. Aust. Dent. J. 2018, 63, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, H.; Krithikadatta, J. Fracture Resistance of Endodontically Treated Teeth Restored with Short Fiber Reinforced Composite and a Low Viscosity Bulk Fill Composite in Class II Mesial-Occlusal-Distal Access Cavities: An Ex-vivo Study. Cureus 2023, 15, e42798. [Google Scholar] [CrossRef]
- Abdulamir, S.W.; Majeed, M.A. Fracture Resistance of Endodontically Treated Maxillary Premolar Teeth Restored with Wallpapering Technique: A Comparative In Vitro Study. Int. J. Dent. 2023, 2023, 6159338. [Google Scholar] [CrossRef]
- Ahmed, B.; Wafaie, R.A.; Hamama, H.H.; Mahmoud, S.H. 3-year randomized clinical trial to evaluate the performance of posterior composite restorations lined with ion-releasing materials. Sci. Rep. 2024, 14, 4942. [Google Scholar] [CrossRef] [PubMed]
- Thongbai-On, N.; Chotvorrarak, K.; Banomyong, D.; Burrow, M.F.; Osiri, S.; Pattaravisitsate, N. Fracture resistance, gap and void formation in root-filled mandibular molars restored with bulk-fill resin composites and glass-ionomer cement base. J. Investig. Clin. Dent. 2019, 10, e12435. [Google Scholar] [CrossRef] [PubMed]
- van de Sande, F.H.; Rodolpho, P.A.; Basso, G.R.; Patias, R.; da Rosa, Q.F.; Demarco, F.F.; Opdam, N.J.; Cenci, M.S. 18-year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent. Mater. 2015, 31, 669–675. [Google Scholar] [CrossRef]
- Taha, N.A.; Palamara, J.E.; Messer, H.H. Cuspal deflection, strain and microleakage of endodontically treated premolar teeth restored with direct resin composites. J. Dent. 2009, 37, 724–730. [Google Scholar] [CrossRef]




| Resin Composite | Base Monomers | Filler Content | Filler Type |
|---|---|---|---|
| Tetric Evo Ceram® | Bis-GMA, Bis-EMA, UDMA | 60–61 vol% 82.5 wt% | barium glass particles Ø 0.6 μm |
| Venus Diamond® | TCD-DI-HEA, UDMA | 64 vol% 80–82 wt% | barium aluminium fluoride glass particles Ø 5 nm–20 μm |
| Grandio® | Bis-GMA, Bis-EMA, TEGDMA | 71.4 vol% 87 wt% | glass ceramic particles Ø 1 μm, silicon dioxide nanoparticles Ø 20–40 nm |
| Estelite® Sigma Quick (lot…) | Bis-GMA, TEGDMA | 71 vol% 82 wt% | pre-polymer Ø 2 μm, silicon-zirconia- particles Ø 0.2 μm |
| Resin Composite | Adhesive System | Mode of Etching | Primer | Adhesive | Bonding |
|---|---|---|---|---|---|
| Tetric Evo Ceram® | Syntac classic® | ortho-phosphoric acid (Etch and Rinse) | Syntac Primer® | Syntac Adhäsiv® | Heliobond® |
| Venus Diamond® | iBond total etch® | ortho-phosphoric acid (Etch and Rinse) | iBond total etch® | ||
| Grandio® | Solobond M® | ortho-phosphoric acid (Etch abd Rinse) | Solobond M® | ||
| Estelite® Sigma Quick | Bond Force® | Bond Force® | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heyder, M.; Kranz, S.; Wehle, B.; Schulze-Späte, U.; Beck, J.; Hennig, C.-L.; Sigusch, B.W.; Reise, M. Suitability of Direct Resin Composites in Restoring Endodontically Treated Teeth (ETT). Materials 2024, 17, 3707. https://doi.org/10.3390/ma17153707
Heyder M, Kranz S, Wehle B, Schulze-Späte U, Beck J, Hennig C-L, Sigusch BW, Reise M. Suitability of Direct Resin Composites in Restoring Endodontically Treated Teeth (ETT). Materials. 2024; 17(15):3707. https://doi.org/10.3390/ma17153707
Chicago/Turabian StyleHeyder, Markus, Stefan Kranz, Bruno Wehle, Ulrike Schulze-Späte, Julius Beck, Christoph-Ludwig Hennig, Bernd W. Sigusch, and Markus Reise. 2024. "Suitability of Direct Resin Composites in Restoring Endodontically Treated Teeth (ETT)" Materials 17, no. 15: 3707. https://doi.org/10.3390/ma17153707
APA StyleHeyder, M., Kranz, S., Wehle, B., Schulze-Späte, U., Beck, J., Hennig, C.-L., Sigusch, B. W., & Reise, M. (2024). Suitability of Direct Resin Composites in Restoring Endodontically Treated Teeth (ETT). Materials, 17(15), 3707. https://doi.org/10.3390/ma17153707








