Photothermal Antibacterial and Osteoinductive Polypyrrole@Cu Implants for Biological Tissue Replacement
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials and Instruments
2.2. Preparation of Composite Coatings
2.3. Investigation of Physiological Stability of Composite Coatings
2.4. Ion Release Profile Evaluation of Composite Coatings
2.5. Evaluation of Drug Release Property of Composite Coatings
2.6. Photothermal Heating Assessment of Composite Coatings
2.7. Photothermal Conversion Experiment
- : photothermal conversion efficiency;
- h: heat transfer coefficient;
- A: surface area of the container; t: natural cooling time;
- ΔTmax, mix: maximum temperature difference between initial and 10 min;
- : maximum temperature difference in the PBS solution between initial and 10 min;
- md and Cd: mass and specific heat capacity of PBS (close to the water phase), respectively;
- ΔT: difference between the initial temperature and the cooling temperature;
- I: infrared laser power.
2.8. Photothermal Conversion Stability Test
2.9. Singlet Oxygen Detection
2.10. Antibacterial Effect Evaluation of Composite Coatings
2.11. In Vitro Effect of the Composite Coatings on Osteoblasts
2.12. Statistical Analysis
3. Results and Discussion
3.1. Characterization of PPy@Cu/PD Composite Coatings
3.2. Electrochemical Measurement
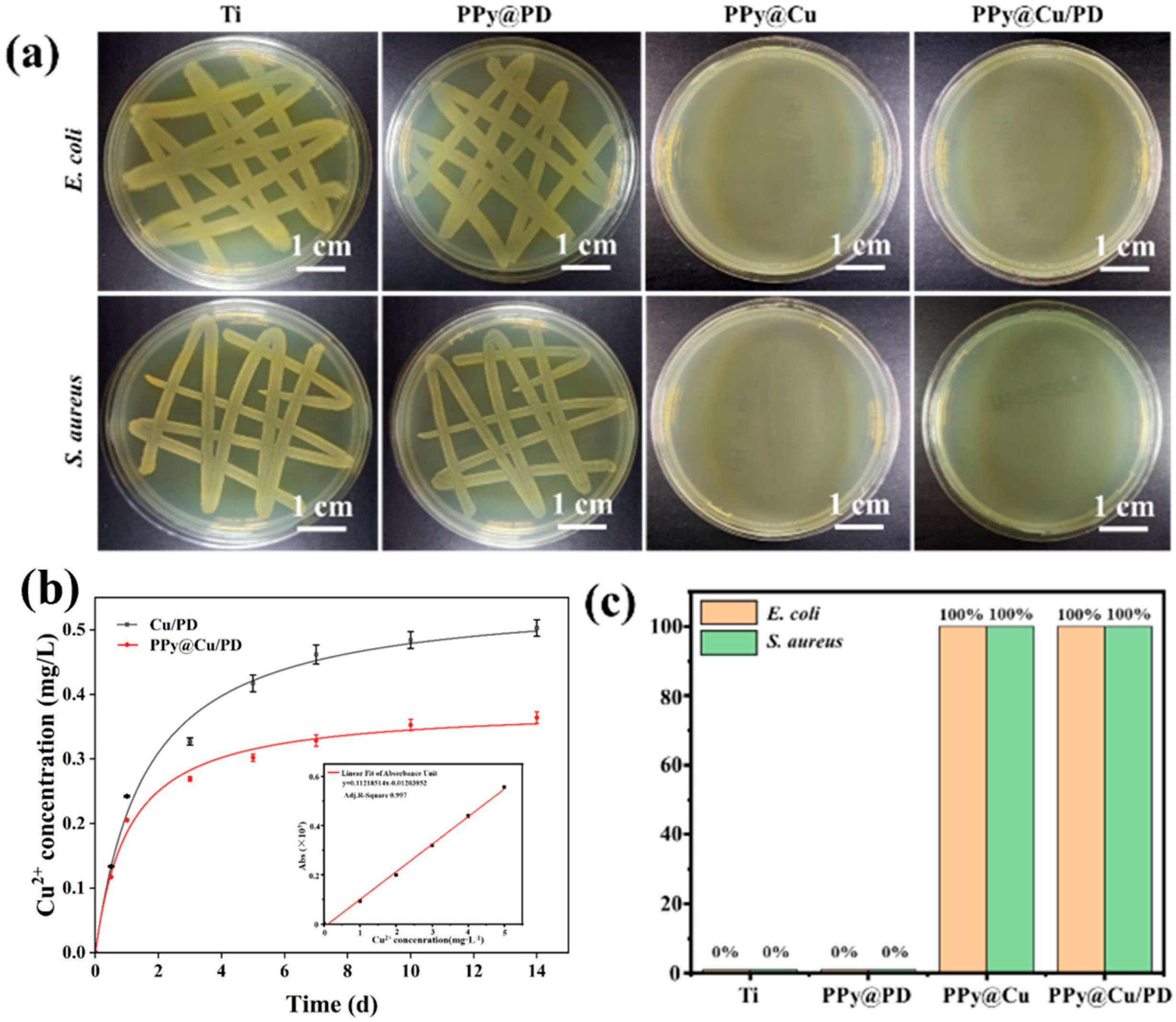
3.3. Analysis of Ion Release and Antibacterial Properties of Composite Coatings
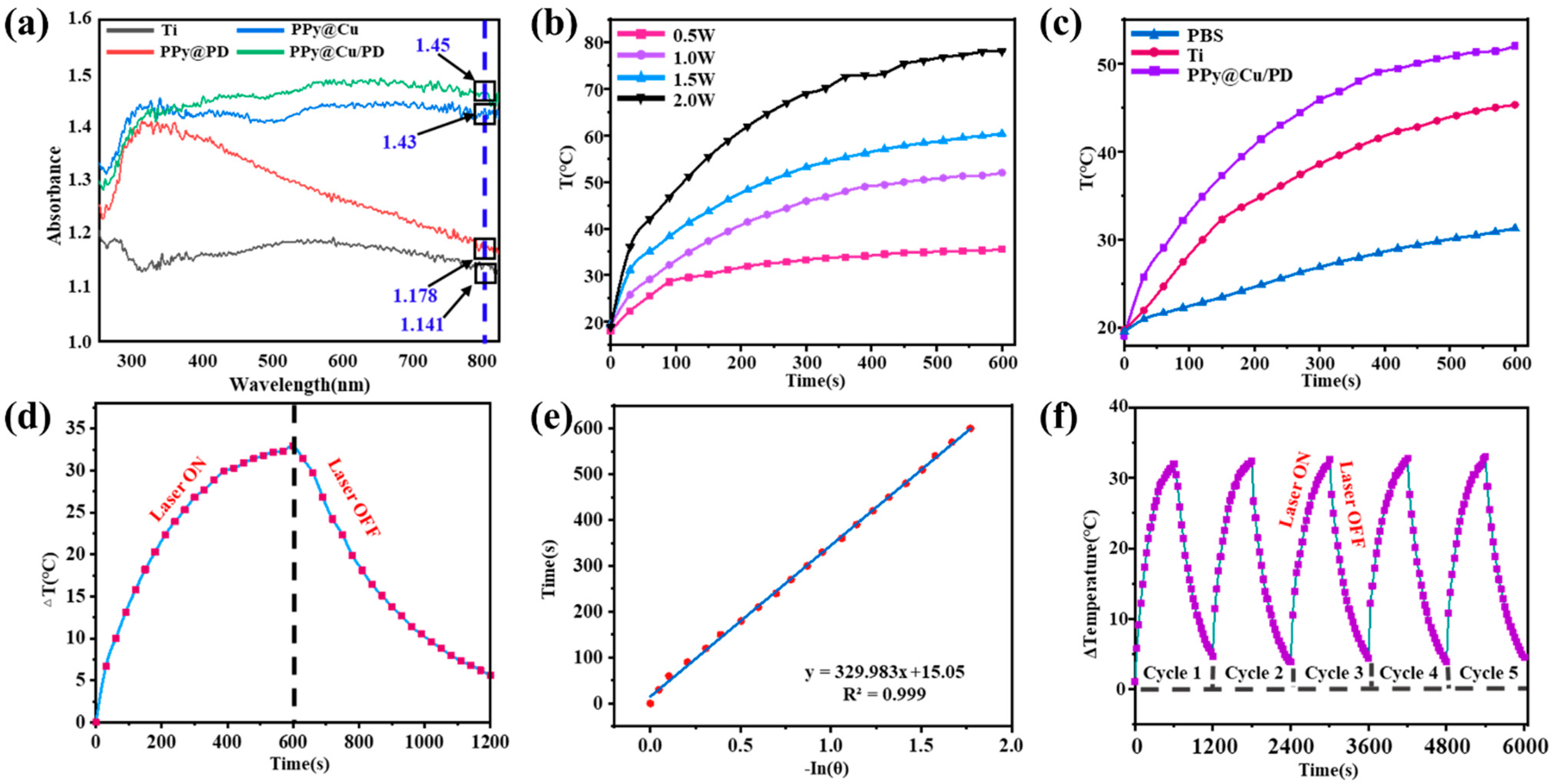
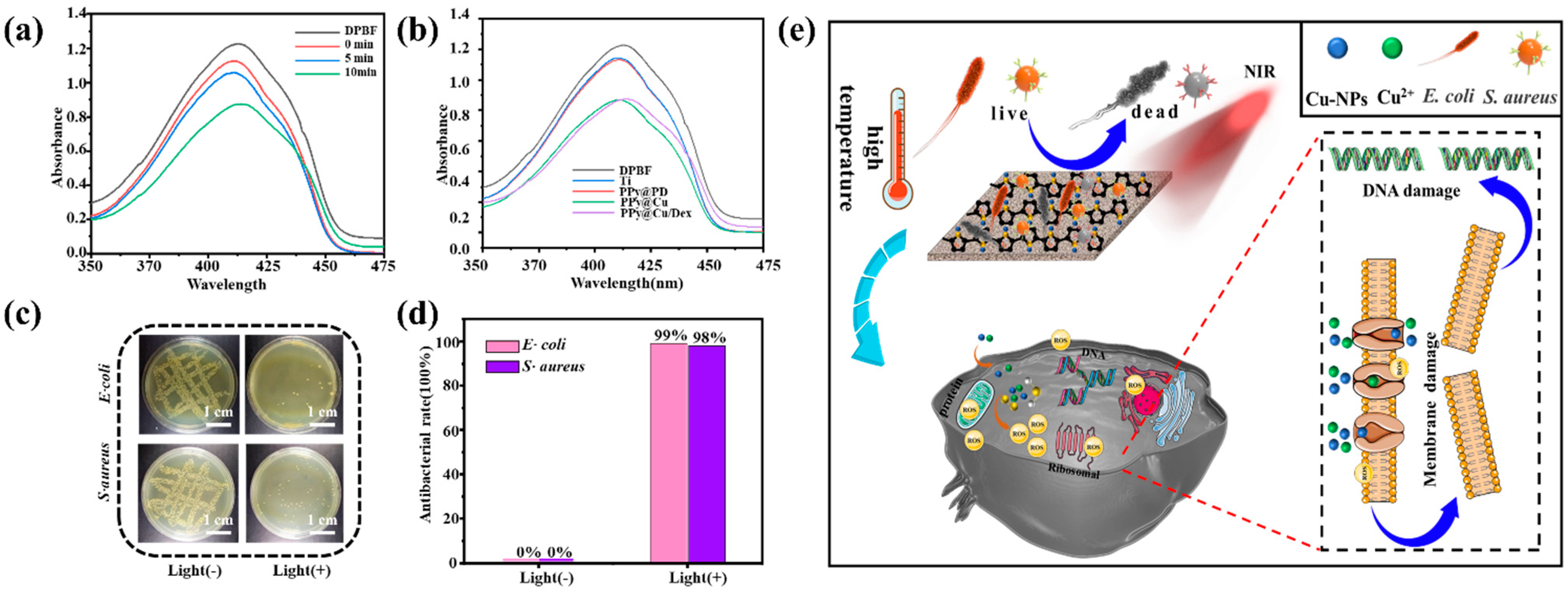
3.4. Analysis of Antibacterial Properties of PPy@Cu/PD Excited by NIR Laser
3.5. Cytocompatibility of Composite Coatings
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giglio, E.D.; Guascito, M.R.; Sabbatin, L.; Zambonin, G. Electropolymerization of pyrrole on titanium substrates for the future development of new biocompatible surfaces. Biomaterials 2001, 22, 2609–2616. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chu, P.K.; Ding, C. Surface modification of titanium, titanium alloys, and related materials for biomedical applications—ScienceDirect. Mater. Sci. Eng. R 2004, 47, 49–121. [Google Scholar] [CrossRef]
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gogia, A.K. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Xu, N.; Fu, J.; Zhao, L.; Chu, P.K.; Huo, K. Biofunctional Elements Incorporated Nano/Microstructured Coatings on Titanium Implants with Enhanced Osteogenic and Antibacterial Performance. Adv. Healthc. Mater. 2020, 9, 2000681. [Google Scholar] [CrossRef] [PubMed]
- Jiang, K.; Wang, H.; Long, Y.; Han, Y.; Zhang, H.; Weng, Q. Injectable miniaturized shape-memory electronic device for continuous glucose monitoring. Device 2023, 1, 100117. [Google Scholar] [CrossRef]
- Mitra, I.; Bose, S.; Dernell, W.S.; Dasgupta, N.; Bandyopadhyay, A. 3D Printing in alloy design to improve biocompatibility in metallic implants. Mater. Today 2021, 45, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hu, K.; Xing, X.; Zhang, J.S.; Zhang, M.R.; Ma, X.H. Smart Titanium Coating Composed of Antibiotic Conjugated Peptides as an Infection-Responsive Antibacterial Agent. Macromol. Biosci. 2020, 21, 2000194. [Google Scholar] [CrossRef] [PubMed]
- Abbasizadeh, N.; Rezayan, A.H.; Nourmohammadi, J.; Kazemzadeh-Narbat, M. HHC-36 antimicrobial peptide loading on silk fibroin (SF)/hydroxyapatite (HA) nanofibrous-coated titanium for the enhancement of osteoblast and bactericidal functions. Int. J. Polym. Mater. 2019, 69, 629–639. [Google Scholar] [CrossRef]
- Tabesh, E.; Salimijazi, H.R.; Kharaziha, M.; Mahmoudi, M.; Hejazi, M. Development of an in-situ chitosancopper nanoparticle coating by electrophoretic deposition. Surf. Coat. Technol. 2019, 364, 239–247. [Google Scholar] [CrossRef]
- Wang, Y.; Yan, L.; Cheng, R.; Muhtar, M.; Cui, W. Multifunctional HA/Cu nano-coatings on titanium using PPy coordination and doping: Via pulse electrochemical polymerization. Biomater. Sci. 2018, 6, 575–585. [Google Scholar] [CrossRef] [PubMed]
- Gérard, C.; Bordeleau, L.J.; Barralet, J.; Doillon, C.J. The stimulation of angiogenesis and collagen deposition by copper. Biomaterials 2010, 31, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Rivera, L.R.; Cochis, A.; Biser, S.; Canciani, E.; Ferraris, S.; Rimondini, L.; Boccaccini, A.R. Antibacterial, pro-angiogenic and pro-osteointegrative zein-bioactive glass/copper based coatings for implantable stainless steel aimed at bone healing. Bioact. Mater. 2021, 6, 12. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Wu, X.; Luo, J.; Yang, G.; Lu, Y.; Lin, S.; Jiang, F.; Zhang, W.; Jiang, X. Copper peptide-incorporated 3D-printed silk-based scaffolds promote vascularized bone regeneration. Chem. Eng. J. 2021, 422, 130147. [Google Scholar] [CrossRef]
- Mitra, D.; Li, M.; Kang, E.-T.; Neoh, K.G. Transparent Copper-based Antibacterial Coatings with Enhanced Efficacy against Pseudomonas aeruginosa. ACS Appl. Mater. Interfaces 2019, 11, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Z.; He, Y.; Lin, C.; Liu, P.; Cai, K. Antibacterial surface design of biomedical titanium materials for orthopedic applications. J. Mater. Sci. Technol. 2021, 78, 51–67. [Google Scholar] [CrossRef]
- Yang, Y.; He, P.; Wang, Y.; Bai, H.; Wang, S.; Xu, J.F.; Zhang, X. Supramolecular radical anions triggered by bacteria in situ for selective photothermal therapy. Angew. Chem. 2017, 129, 16457–16460. [Google Scholar] [CrossRef]
- Yang, Y.; Ma, L.; Cheng, C.; Deng, Y.; Huang, J.; Fan, X.; Nie, C.; Zhao, W.; Zhao, C. Nonchemotherapic and Robust Dual-Responsive Nanoagents with On-Demand Bacterial Trapping, Ablation, and Release for Efficient Wound Disinfection. Adv. Funct. Mater. 2018, 28, 1705708. [Google Scholar] [CrossRef]
- Hu, D.; Li, H.; Wang, B.; Ye, Z.; Lei, W.; Jia, F.; Jin, Q.; Ren, K.F.; Ji, J. Surface-Adaptive Gold Nanoparticles with Effective Adherence and Enhanced Photothermal Ablation of Methicillin-Resistant Staphylococcus aureus Biofilm. ACS Nano 2017, 11, 9330–9339. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Wang, C.; Zhu, L.; Yu, C.; Lu, B.; Wang, Y.; Ding, Y.; Dong, C.M.; Yao, Y. Polydopamine-drug conjugate nanocomposites based on ZIF-8 for targeted cancer photothermal-chemotherapy. J. Biomed. Mater. Res. Part A 2022, 110, 954–963. [Google Scholar] [CrossRef]
- Ma, S.; Luo, X.; Ran, G.; Zhou, Z.; Xie, J.; Li, Y.; Li, X.; Yan, J.; Cai, W.; Wang, L. Copper stabilized bimetallic alloy Cu–Bi by convenient strategy fabrication: A novel Fenton-like and photothermal synergistic antibacterial platform. J. Clean. Prod. 2022, 336, 130431. [Google Scholar] [CrossRef]
- Jin, C.; Su, K.; Tan, L.; Liu, X.; Cui, Z.; Yang, X.; Li, Z.; Liang, Y.; Zhu, S.; Yeung, K.W.K. Near-infrared light photocatalysis and photothermy of carbon quantum dots and au nanoparticles loaded titania nanotube array. Mater. Des. 2019, 177, 107845. [Google Scholar] [CrossRef]
- Tao, B.; Lin, C.; Deng, Y.; Yuan, Z.; Shen, X.; Chen, M.; He, Y.; Peng, Z.; Hu, Y.; Cai, K. Copper-nanoparticle-embedded hydrogel for killing bacteria and promoting wound healing with photothermal therapy. J. Mater. Chem. B 2019, 7, 2534–2548. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Tang, F.; Tang, L.; Li, L. Synthesis of Cu-Nanoparticle Hydrogel with Self-Healing and Photothermal Properties. ACS Appl. Mater. Interfaces 2017, 9, 20895–20903. [Google Scholar] [CrossRef] [PubMed]
- Harmankaya, N.; Karlsson, J.; Palmquist, A.; Halvarsson, M.; Igawa, K.; Andersson, M.; Tengvall, P. Raloxifene and alendronate containing thin mesoporous titanium oxide films improve implant fixation to bone. Acta Biomater. 2013, 9, 7064–7073. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Luo, Z.; Hu, Y.; Shen, X.; Cai, K. Enhancement of Local Bone Remodeling in Osteoporotic Rabbits by Biomimic Multilayered Structures on Ti6Al4V Implants. J. Biomed. Mater. Res. Part A 2016, 104, 1437–1451. [Google Scholar] [CrossRef] [PubMed]
- Yoshinari, M.; Oda, Y.; Ueki, H.; Yokose, S. Immobilization of bisphosphonates on surface modified titanium. Biomaterials 2001, 22, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, D.; Srinivasan, B.; Anbu, J.; Azamthulla, M.; Lakkawar, A. Pamidronate functionalized mucoadhesive compact for treatment of osteoporosis-in vitro and in vivo characterization. J. Drug Deliv. Sci. Technol. 2019, 52, 915–926. [Google Scholar] [CrossRef]
- Kajiwara, H.; Yamaza, T.; Yoshinari, M.; Goto, T.; Iyama, S.; Atsuta, I.; Kido, M.A.; Tanaka, T. The bisphosphonate pamidronate on the surface of titanium stimulates bone formation around tibial implants in rats. Biomaterials 2005, 26, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Cui, W.; Wang, X.; Lu, X.; Zhang, L.; Li, X.; Li, W.; Zhang, W.; Chen, J. Poly-l-lysine/Sodium Alginate Coating Loading Nanosilver for Improving the Antibacterial Effect and Inducing Mineralization of Dental Implants. ACS Omega 2020, 5, 10562–10571. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Mu, C.; Shen, X.; Zhang, Y.; Cai, K. Peptide LL-37 coating on micro-structured titanium implants to facilitate bone formation in vivo via mesenchymal stem cell recruitment. Acta Biomater. 2018, 80, 412–424. [Google Scholar]
- Wang, C.; Yang, X.; Xiao, Z.; Zhu, X.; Zhang, K.; Fan, Y.; Zhang, X. Construction of surface HA/TiO2 coating on porous titanium scaffolds and its preliminary biological evaluation. Mater. Sci. Eng. C 2017, 70, 1047–1056. [Google Scholar]
- Luo, J.; Mamat, B.; Yue, Z.; Zhang, N.; Xu, X.; Li, Y.; Su, Z.; Ma, C.; Zhang, F.; Wang, Y. Multi-metal ions doped hydroxyapatite coatings via electrochemical methods for antibacterial and osteogenesis. Colloid Interface Sci. Commun. 2021, 43, 100435. [Google Scholar] [CrossRef]
- Kim, S.; Jang, L.K.; Jang, M.; Lee, S.; Hardy, J.G.; Lee, J.Y. Electrically Conductive Polydopamine-Polypyrrole as High Performance Biomaterials for Cell Stimulation in Vitro and Electrical Signal Recording in Vivo. ACS Appl. Mater. Interfaces 2018, 10, 33032–33042. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Liang, Y.; Ding, S.; Zhang, K.; Yang, Y. Application of conductive PPy/SF composite scaffold and electrical stimulation for neural tissue engineering. Biomaterials 2020, 255, 120164. [Google Scholar] [CrossRef]
- Zhou, T.; Yan, L.; Xie, C.; Li, P.; Jiang, L.; Fang, J.; Zhao, C.; Ren, F.; Wang, K.; Wang, Y.; et al. A mussel-inspired persistent ROS-scavenging, electroactive, and osteoinductive scaffold based on electrochemical-driven in situ nanoassembly. Small 2019, 15, 1805440. [Google Scholar] [CrossRef] [PubMed]
- Maimaiti, B.; Zhang, N.; Yan, L.; Luo, J.; Xie, C.; Wang, Y.; Ma, C.; Ye, T. Stable ZnO-doped hydroxyapatite nanocoating for anti-infection and osteogenic on titanium—ScienceDirect. Colloids Surf. B Biointerfaces 2020, 186, 110731. [Google Scholar] [CrossRef] [PubMed]
- Ren, W.; Yan, Y.; Zeng, L.; Shi, Z.; Gong, A.; Schaaf, P.; Wang, D.; Zhao, J.; Zou, B.; Yu, H.; et al. A Near Infrared Light Triggered Hydrogenated Black TiO2 for Cancer Photothermal Therapy. Adv. Healthc. Mater. 2015, 4, 1526–1536. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Cheng, X.; Xiao, L.; Wang, Q.; Yan, K.; Su, Z.; Wang, L.; Ma, C.; Wang, Y. Inside-outside Ag nanoparticles-loaded polylactic acid electrospun fiber for long-term antibacterial and bone regeneration. Int. J. Biol. Macromol. 2021, 167, 1338–1348. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ding, Y.; Yuan, Y.; Cao, A.; He, X.; Peng, Q.; Li, Y. Multifunctional, Highly Flexible, Free-Standing 3D Polypyrrole Foam. Small 2016, 12, 4070–4076. [Google Scholar] [CrossRef] [PubMed]
- Panek, P.T.; Jacob, C.R. Anharmonic Theoretical Vibrational Spectroscopy of Polypeptides. J. Phys. Chem. Lett. 2016, 7, 3084–3090. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.; Wang, Y.; Zhou, Q.; Ding, Z.; Liu, J.; He, Q.; Zhang, H. Microstructure, Wettability, Corrosion Resistance and Antibacterial Property of Cu-MTa2O5 Multilayer Composite Coatings with Different Cu Incorporation Contents. Biomolecules 2019, 10, 68. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.J.; Mandakhbayar, N.; Kang, M.S.; Yoon, J.Y.; Kim, H.W. Antibacterial, proangiogenic, and osteopromotive nanoglass paste coordinates regenerative process following bacterial infection in hard tissue. Biomaterials 2021, 268, 120593. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Song, T.; Wang, T.; Zeng, H. In-situ synthesis of Cu nanoparticles hybridized with carbon quantum dots as a broad spectrum photocatalyst for improvement of photocatalytic H-2 evolution. Appl. Catal. B Environ. Int. J. Devoted Catal. Sci. Appl. 2017, 206, 328–335. [Google Scholar] [CrossRef]
- Tan, L.; Li, J.; Liu, X.; Cui, Z.; Yang, X.; Zhu, S.; Li, Z.; Yuan, X.; Zheng, Y.; Yeung, K.W.K.; et al. Rapid Biofilm Eradication on Bone Implants Using Red Phosphorus and Near-Infrared Light. Adv. Mater. 2018, 30, 1801808. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Chen, L.; Yu, Y.; Qin, X.; Li, K.; Tian, H.; Yi, W.; Dei, D.; Chen, L. Fabrication of copper ions-substituted hydroxyapatite/polydopamine nanocomposites with high antibacterial and angiogenesis effects for promoting infected wound healing. J. Ind. Eng. Chem. 2021, 104, 345–355. [Google Scholar]
- Lu, S.; Li, R.; Chai, M.; Wang, J.; Duan, W.; Yao, X.; Zhang, X.; Tang, B. Nanostructured Cu-doped TiO2 with photothermal effect for prevention of implant-associated infection. Colloids Surf. B Biointerfaces 2022, 217, 112695. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.S.I.; Sheng, M.H.; Lau, K.-H.W.; Wilson, S.M.; Wongworawat, M.D.; Tang, X.; Ghahramanpouri, M.; Nehme, A.; Xu, Y.; Abdipour, A. Calcium released by osteoclastic resorption stimulates autocrine/paracrine activities in local osteogenic cells to promote coupled bone formation. Am. J. Physiol. Cell Physiol. 2022, 322, C977–C990. [Google Scholar] [CrossRef] [PubMed]



| Ecorr (V) | Icorr (A/cm2) | |
|---|---|---|
| Ti | −0.78 | 1.584 × 10−7 |
| PPy@/Cu/PD | −0.06 | 3.98 × 10−7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, T.; Zhou, Z.; Wang, Y. Photothermal Antibacterial and Osteoinductive Polypyrrole@Cu Implants for Biological Tissue Replacement. Materials 2024, 17, 3882. https://doi.org/10.3390/ma17153882
Zhou T, Zhou Z, Wang Y. Photothermal Antibacterial and Osteoinductive Polypyrrole@Cu Implants for Biological Tissue Replacement. Materials. 2024; 17(15):3882. https://doi.org/10.3390/ma17153882
Chicago/Turabian StyleZhou, Tianyou, Zeyan Zhou, and Yingbo Wang. 2024. "Photothermal Antibacterial and Osteoinductive Polypyrrole@Cu Implants for Biological Tissue Replacement" Materials 17, no. 15: 3882. https://doi.org/10.3390/ma17153882
APA StyleZhou, T., Zhou, Z., & Wang, Y. (2024). Photothermal Antibacterial and Osteoinductive Polypyrrole@Cu Implants for Biological Tissue Replacement. Materials, 17(15), 3882. https://doi.org/10.3390/ma17153882








