Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures
Abstract
:1. Introduction
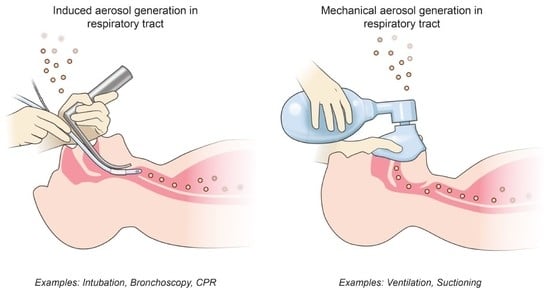
2. Aerosol-Generating Medical Procedures
3. Emerging High-Risk Viruses
3.1. Bunyavirales: Arenaviridae
3.2. Bunyavirales: Hantaviridae, Nairoviridae, Phenuiviridae
3.3. Coronaviridae
3.4. Filoviridae
3.5. Orthomyxoviridae
3.6. Paramyxoviridae
4. Designing Experiments and Assessing Risk
5. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McCarthy, M. Texas healthcare worker is diagnosed with Ebola. BMJ 2014, 349, g6200. [Google Scholar] [CrossRef] [PubMed]
- Assiri, A.; McGeer, A.; Perl, T.M.; Price, C.S.; Al Rabeeah, A.a.; Cummings, D.a.T.; Alabdullatif, Z.N.; Assad, M.; Almulhim, A.; Makhdoom, H.; et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N. Engl. J. Med. 2013, 369, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Chowell, G.; Abdirizak, F.; Lee, S.; Lee, J.; Jung, E.; Nishiura, H.; Viboud, C. Transmission characteristics of MERS and SARS in the healthcare setting: A comparative study. BMC Med. 2015, 13, 210. [Google Scholar] [CrossRef] [PubMed]
- de Wit, E.; van Doremalen, N.; Falzarano, D.; Munster, V.J. SARS and MERS: Recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016, 14, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.C.; Nguyen, D.; Aden, B.; Al Bandar, Z.; Al Dhaheri, W.; Abu Elkheir, K.; Khudair, A.; Al Mulla, M.; El Saleh, F.; Imambaccus, H.; et al. Transmission of Middle East Respiratory Syndrome Coronavirus Infections in Healthcare Settings, Abu Dhabi. Emerg. Infect. Dis. 2016, 22, 647–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pshenichnaya, N.Y.; Nenadskaya, S.A. Probable Crimean-Congo hemorrhagic fever virus transmission occurred after aerosol-generating medical procedures in Russia: Nosocomial cluster. Int. J. Infect. Dis. 2015, 33, 120–122. [Google Scholar] [CrossRef]
- Davies, A.; Thomson, G.; Walker, J.; Bennett, A. A review of the risks and disease transmission associated with aerosol generating medical procedures. J. Infect. Prev. 2009, 10, 122–126. [Google Scholar] [CrossRef]
- Judson, S.; Prescott, J.; Munster, V. Understanding Ebola Virus Transmission. Viruses 2015, 7, 511–521. [Google Scholar] [CrossRef] [Green Version]
- Thomas, R.J. Particle size and pathogenicity in the respiratory tract. Virulence 2013, 4, 847–858. [Google Scholar] [CrossRef] [Green Version]
- Tellier, R. Review of aerosol transmission of influenza A virus. Emerg. Infect. Dis. 2006, 12, 1657–1662. [Google Scholar] [CrossRef]
- Tran, K.; Cimon, K.; Severn, M.; Pessoa-Silva, C.L.; Conly, J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- Fowler, R.A.; Guest, C.B.; Lapinsky, S.E.; Sibbald, W.J.; Louie, M.; Tang, P.; Simor, A.E.; Stewart, T.E. Transmission of Severe Acute Respiratory Syndrome during Intubation and Mechanical Ventilation. Am. J. Respir. Crit. Care Med. 2004, 169, 1198–1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christian, M.D.; Loutfy, M.; McDonald, L.C.; Martinez, K.F.; Ofner, M.; Wong, T.; Wallington, T.; Gold, W.L.; Mederski, B.; Green, K.; et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg. Infect. Dis. 2004, 10, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.C.; Leung, K.S. Transmission and prevention of occupational infections in orthopaedic surgeons. J. Bone Joint Surg. Am. 2004, 86-A, 1065–1076. [Google Scholar] [CrossRef] [PubMed]
- Garden, J.M. Viral Disease Transmitted by Laser-Generated Plume (Aerosol). Arch. Dermatol. 2002, 138, 1303. [Google Scholar] [CrossRef] [PubMed]
- Shiu, E.Y.; Leung, N.H.; Cowling, B.J. Controversy around airborne versus droplet transmission of respiratory viruses. Curr. Opin. Infect. Dis. 2019, 32, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Mehand, M.S.; Al-Shorbaji, F.; Millett, P.; Murgue, B. The WHO R&D Blueprint: 2018 review of emerging infectious diseases requiring urgent research and development efforts. Antiviral Res. 2018, 159, 63–67. [Google Scholar] [PubMed]
- Lloyd-Smith, J.O.; George, D.; Pepin, K.M.; Pitzer, V.E.; Pulliam, J.R.C.; Dobson, A.P.; Hudson, P.J.; Grenfell, B.T. Epidemic dynamics at the human-animal interface. Science 2009, 326, 1362–1367. [Google Scholar] [CrossRef] [PubMed]
- Drosten, C. Virus ecology: A gap between detection and prediction. Emerg. Microbes Infect. 2013, 2, e31. [Google Scholar] [CrossRef] [PubMed]
- Kenyon, R.H.; McKee, K.T.; Zack, P.M.; Rippy, M.K.; Vogel, A.P.; York, C.; Meegan, J.; Crabbs, C.; Peters, C.J. Aerosol infection of rhesus macaques with Junin virus. Intervirology 1992, 33, 23–31. [Google Scholar]
- Malhotra, S.; Yen, J.Y.; Honko, A.N.; Garamszegi, S.; Caballero, I.S.; Johnson, J.C.; Mucker, E.M.; Trefry, J.C.; Hensley, L.E.; Connor, J.H. Transcriptional Profiling of the Circulating Immune Response to Lassa Virus in an Aerosol Model of Exposure. PLoS Negl. Trop. Dis. 2013, 7. [Google Scholar] [CrossRef] [PubMed]
- Bell, T.M.; Shaia, C.I.; Bunton, T.E.; Robinson, C.G.; Wilkinson, E.R.; Hensley, L.E.; Cashman, K.A. Pathology of Experimental Machupo Virus Infection, Chicava Strain, in Cynomolgus Macaques (Macaca fascicularis) by Intramuscular and Aerosol Exposure. Vet. Pathol. 2014, 52, 26–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pedrosa, P.B.S.; Cardoso, T.a.O. Viral infections in workers in hospital and research laboratory settings: A comparative review of infection modes and respective biosafety aspects. Int. J. Infect. Dis. 2011, 15, e366–e376. [Google Scholar] [CrossRef] [PubMed]
- Alimonti, J.; Leung, A.; Jones, S.; Gren, J.; Qiu, X.; Fernando, L.; Balcewich, B.; Wong, G.; Ströher, U.; Grolla, A.; et al. Evaluation of transmission risks associated with in vivo replication of several high containment pathogens in a biosafety level 4 laboratory. Sci. Rep. 2014, 4, 5824. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.M.; McCormick, J.B.; Webb, P.; Smith, E.S.; Elliott, L.H.; King, I.J. Clinical virology of Lassa fever in hospitalized patients. J. Infect. Dis. 1987, 155, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Peters, C.J.; Kuehne, R.W.; Mercado, R.R.; Le Bow, R.H.; Spertzel, R.O. Hemorrhagic fever in cochabamba, bolivia, 1971. Am J Epidemiol. 1974, 99, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.J.; Rutala, W. Risks and prevention of nosocomial transmission of rare zoonotic diseases. Clin. Infect. Dis. 2001, 32, 446–456. [Google Scholar]
- Walker, D.H.; McCormick, J.B.; Johnson, K.M.; Webb, P.A.; Komba-Kono, G.; Elliott, L.H.; Gardner, J.J. Pathologic and virologic study of fatal Lassa fever in man. Am. J. Pathol. 1982, 107, 349–356. [Google Scholar]
- Gaidamovich, S.Y.; Butenko, A.M.; Leschinskaya, H.V. Human Laboratory Acquired Arbo-, Arena-, and Hantavirus Infections. J. Am. Biol. Saf. Assocation 2000, 5, 5–11. [Google Scholar] [CrossRef]
- Pettersson, L.; Klingström, J.; Hardestam, J.; Lundkvist, Å.; Ahlm, C.; Evander, M. Hantavirus RNA in saliva from patients with hemorrhagic fever with renal syndrome. Emerg. Infect. Dis. 2008, 14, 406–411. [Google Scholar] [CrossRef]
- Martinez-valdebenito, C.; Calvo, M.; Vial, C.; Mansilla, R.; Marco, C.; Palma, R.E.; Vial, P.A.; Valdivieso, F.; Mertz, G.; Ferrés, M. Person-to-Person Household and Nosocomial Transmission of Andes. Emerg. Infect. Dis. 2014, 20, 1629–1636. [Google Scholar] [PubMed]
- Green, W.; Feddersen, R.; Yousef, O.; Behr, M.; Smith, K.; Nestler, J.; Jenison, S.; Yamada, T.; Hjelle, B. Tissue distribution of hantavirus antigen in naturally infected humans and deer mice. J. Infect. Dis. 1998, 177, 1696–1700. [Google Scholar] [CrossRef] [PubMed]
- Drosten, C.; Gunther, S.; Preiser, W.; van der Werf, S.; Brodt, H.R.; Becker, S.; Rabenau, H.; Panning, M.; Kolesnikova, L.; Fouchier, R.A.; et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003, 348, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- Zaki, A.M.; van Boheemen, S.; Bestebroer, T.M.; Osterhaus, A.D.M.E.; Fouchier, R. a. M. Isolation of a Novel Coronavirus from a Man with Pneumonia in Saudi Arabia. N. Engl. J. Med. 2012, 121017140031005. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, E.; Saijo, M. Animal models for Ebola and Marburg virus infections. Front. Microbiol. 2013, 4, 1–20. [Google Scholar] [CrossRef]
- Bausch, D.G.; Towner, J.S.; Dowell, S.F.; Kaducu, F.; Lukwiya, M.; Sanchez, A.; Nichol, S.T.; Ksiazek, T.G.; Rollin, P.E. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J. Infect. Dis. 2007, 196, S142–S147. [Google Scholar] [CrossRef]
- Simpson, D.I.H. Marburg Agent Disease: In Monkeys. Trans. R Soc. Trop Med. Hyg. 1969, 63, 303–309. [Google Scholar] [CrossRef]
- Martines, R.B.; Ng, D.L.; Greer, P.W.; Rollin, P.E.; Zaki, S.R. Tissue and cellular tropism, pathology and pathogenesis of Ebola and Marburg viruses. J. Pathol. 2015, 235, 153–174. [Google Scholar] [CrossRef]
- Beigel, J.H.; Farrar, J.; Han, A.M.; Hayden, F.G.; Hyer, R.; De Jong, M.D.; Lochindarat, S.; Tien, N.T.K.; Hien, N.T.; Hien, T.T.; et al. Avian influenza A (H5N1) infection in humans. N. Engl. J. Med. 2005, 353, 1374–1385. [Google Scholar]
- Hammoud, D.A.; Lentz, M.R.; Lara, A.; Bohannon, J.K.; Feuerstein, I.; Huzella, L.; Jahrling, P.B.; Lackemeyer, M.; Laux, J.; Rojas, O.; et al. Aerosol exposure to intermediate size Nipah virus particles induces neurological disease in African green monkeys. PLoS Negl. Trop. Dis. 2018, 12, e0006978. [Google Scholar] [CrossRef]
- Chua, K.B.; Lam, S.K.; Goh, K.J.; Hooi, P.S.; Ksiazek, T.G.; Kamarulzaman, A.; Olson, J.; Tan, C.T. The presence of nipah virus in respiratory secretions and urine of patients during an outbreak of nipah virus encephalitis in Malaysia. J. Infect. 2001, 42, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Sazzad, H.M.S.; Hossain, M.J.; Gurley, E.S.; Ameen, K.M.H.; Parveen, S.; Islam, M.S.; Faruque, L.I.; Podder, G.; Banu, S.S.; Lo, M.K.; et al. Nipah virus infection outbreak with nosocomial and corpse-to-human transmission, Bangladesh. Emerg. Infect. Dis. 2013, 19, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.T.; Robertson, T.; Ong, B.B.; Chong, J.W.; Yaiw, K.C.; Wang, L.F.; Ansford, J.; Tannenberg, A. Human Hendra virus infection causes acute and relapsing encephalitis. Neuropathol. Appl. Neurobiol. 2009, 35, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Mekibib, B.; Ariën, K.K. Aerosol Transmission of Filoviruses. Viruses 2016, 8, 148. [Google Scholar] [CrossRef] [PubMed]
- Richard, M.; Fouchier, R.A.M. Influenza A virus transmission via respiratory aerosols or droplets as it relates to pandemic potential. FEMS Microbiol. Rev. 2016, 40, 68–85. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Liu, S.; Liu, J.; Chai, C.; Mao, H.; Yu, Z.; Tang, Y.; Zhu, G.; Chen, H.X.; Zhu, C.; et al. Nosocomial Co-Transmission of Avian Influenza A(H7N9) and A(H1N1)pdm09 Viruses between 2 Patients with Hematologic Disorders. Emerg. Infect. Dis. 2016, 22, 598–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, C.-F.; Ma, M.-J.; Zhan, B.-D.; Lai, S.-M.; Hu, Y.; Yang, X.-X.; Li, J.; Cao, G.-P.; Zhou, J.-J.; Zhang, J.-M.; et al. Nosocomial transmission of avian influenza A (H7N9) virus in China: Epidemiological investigation. BMJ 2015, 351, h5765. [Google Scholar] [CrossRef] [PubMed]
- Lietz, J.; Westermann, C.; Nienhaus, A.; Schablon, A. The Occupational Risk of Influenza A (H1N1) Infection among Healthcare Personnel during the 2009 Pandemic: A Systematic Review and Meta-Analysis of Observational Studies. PLoS ONE 2016, 11, e0162061. [Google Scholar] [CrossRef]
- Schultsz, C.; Dong, V.C.; Chau, N.V.V.; Le, N.T.H.; Lim, W.; Thanh, T.T.; Dolecek, C.; de Jong, M.D.; Hien, T.T.; Farrar, J. Avian influenza H5N1 and healthcare workers. Emerg. Infect. Dis. 2005, 11, 1158–1159. [Google Scholar] [CrossRef]
- van Riel, D.; Munster, V.J.; de Wit, E.; Rimmelzwaan, G.F.; Fouchier, R.A.M.; Osterhaus, A.D.M.E.; Kuiken, T. H5N1 Virus Attachment to Lower Respiratory Tract. Science 2006, 312, 399. [Google Scholar] [CrossRef]
- Munster, V.J.; de Wit, E.; van den Brand, J.M.A.; Herfst, S.; Schrauwen, E.J.A.; Bestebroer, T.M.; van de Vijver, D.; Boucher, C.A.; Koopmans, M.; Rimmelzwaan, G.F.; et al. Pathogenesis and Transmission of Swine-Origin 2009 A(H1N1) Influenza Virus in Ferrets. Science 2009, 325, 481–483. [Google Scholar] [CrossRef] [Green Version]
- Verreault, D.; Moineau, S.; Duchaine, C. Methods for sampling of airborne viruses. Microbiol. Mol. Biol. Rev. 2008, 72, 413–444. [Google Scholar] [CrossRef] [PubMed]
- Rule, A.M.; Apau, O.; Ahrenholz, S.H.; Brueck, S.E.; Lindsley, W.G.; de Perio, M.A.; Noti, J.D.; Shaffer, R.E.; Rothman, R.; Grigorovitch, A.; et al. Healthcare personnel exposure in an emergency department during influenza season. PLoS ONE 2018, 13, e0203223. [Google Scholar] [CrossRef] [PubMed]
- Thompson, K.-A.; Pappachan, J.V.; Bennett, A.M.; Mittal, H.; Macken, S.; Dove, B.K.; Nguyen-Van-Tam, J.S.; Copley, V.R.; O’Brien, S.; Hoffman, P.; et al. Influenza aerosols in UK hospitals during the H1N1 (2009) pandemic--the risk of aerosol generation during medical procedures. PLoS ONE 2013, 8, e56278. [Google Scholar] [CrossRef] [PubMed]
- Blachere, F.M.; Lindsley, W.G.; McMillen, C.M.; Beezhold, D.H.; Fisher, E.M.; Shaffer, R.E.; Noti, J.D. Assessment of influenza virus exposure and recovery from contaminated surgical masks and N95 respirators. J. Virol. Methods 2018, 260, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Simonds, A.; Hanak, A.; Chatwin, M.; Morrell, M.; Hall, A.; Parker, K.; Siggers, J.; Dickinson, R. Evaluation of droplet dispersion during non-invasive ventilation, oxygen therapy, nebuliser treatment and chest physiotherapy in clinical practice: Implications for management of pandemic influenza and other airborne infections. Health Technol. Assess. 2010, 14. [Google Scholar] [CrossRef] [PubMed]
- Fischer, R.J.; Bushmaker, T.; Judson, S.; Munster, V.J. Comparison of the Aerosol Stability of 2 Strains of Zaire ebolavirus From the 1976 and 2013 Outbreaks. J. Infect. Dis. 2016, 214, S290–S293. [Google Scholar] [CrossRef]
- Piercy, T.J.; Smither, S.J.; Steward, J. a.; Eastaugh, L.; Lever, M.S. The survival of filoviruses in liquids, on solid substrates and in a dynamic aerosol. J. Appl. Microbiol. 2010, 109, 1531–1539. [Google Scholar] [CrossRef] [PubMed]
- Garibaldi, B.T.; Chertow, D.S. High-Containment Pathogen Preparation in the Intensive Care Unit. Infect. Dis. Clin. North Am. 2017, 31, 561–576. [Google Scholar] [CrossRef]
- Infection Prevention and Control Recommendations for Hospitalized Patients Under Investigation (PUIs) for Ebola Virus Disease (EVD) in U.S. Hospitals | Ebola Hemorrhagic Fever | CDC. Available online: http://www.cdc.gov/vhf/ebola/healthcare-us/hospitals/infection-control.html (accessed on 4 October 2019).
- 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Available online: http://www.cdc.gov/hicpac/pdf/isolation/Isolation2007.pdf (accessed on 4 October 2019).
- MERS-CoV | Interim Guidance for Health Professionals | CDC. Available online: http://www.cdc.gov/coronavirus/mers/interim-guidance.html (accessed on 4 October 2019).
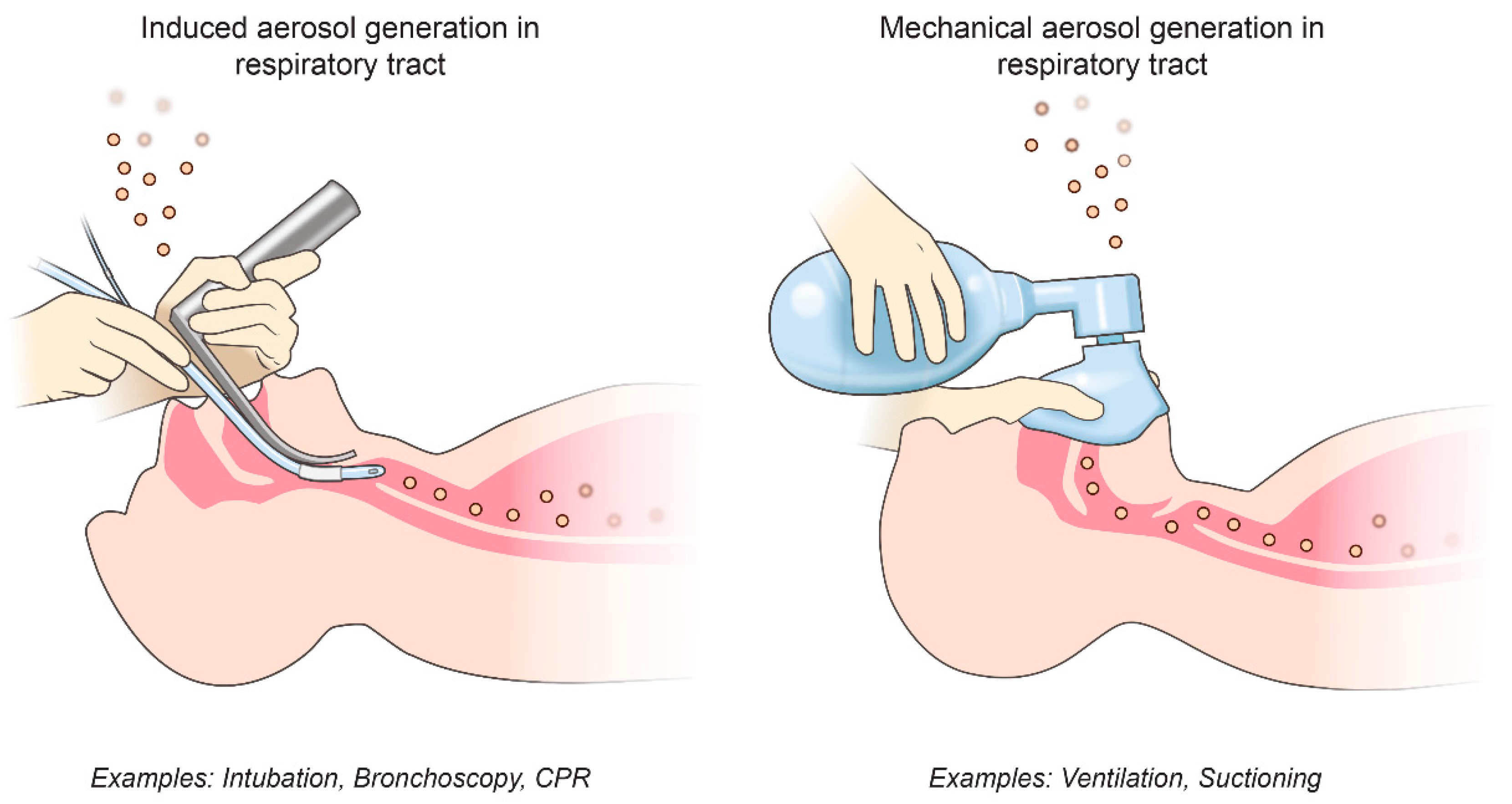
| AGMP | How/Where Aerosols May Be Generated |
|---|---|
| Bronchoscopy * | Induced cough, respiratory tract |
| Cardiopulmonary resuscitation * | Induced cough, respiratory tract |
| Noninvasive ventilation * (BiPAP, CPAP, HFOV) | Possible mechanical dispersal of aerosols, respiratory tract |
| Tracheal intubation * | Induced cough, respiratory tract |
| Manual ventilation * | Possible mechanical dispersal of aerosols, respiratory tract |
| Surgery | Cutting bone and tendon, and irrigation aerosolize blood |
| Sputum induction | Induced cough, respiratory tract |
| Nebulizer treatment | Possible mechanical dispersal of aerosols, respiratory tract |
| Suctioning | Possible mechanical dispersal of aerosols, respiratory tract |
| Laser plume | Mechanical dispersal of aerosols |
| Family, Virus | Infectious via Aerosol? | Evidence in Respiratory Tract? | Nosocomial Transmission/AGMPs? |
|---|---|---|---|
| Arenaviridae i. Junin virus ii. Lassa virus iii. Machupo virus | i, ii, iii. NHPs infected by aerosol administration [20,21,22] ii. Laboratory workers infected by inhaling aerosols [23] | Upper respiratory: i. Viral RNA in NHP oral and nasal swabs [24] ii. Virus isolated from human throat swabs [25] | ii, iii. Nosocomial transmission [26,27] |
| Lower respiratory: ii. Virus isolated from human lung [28] | |||
| Hantaviridae, Nairoviridae, Phenuiviridae i. CCHF virus ii. Hantaviruses iii. Rift valley fever virus | i, ii, iii. Laboratory workers infected by inhaling aerosols [23,29] | Upper respiratory: i, iii. Viral RNA in NHP nasal swabs [24] iii. Viral RNA in NHP oral swabs [24] ii. Viral RNA in human saliva [30] Lower respiratory: | i, ii. Nosocomial transmission [6,31] i. Likely association with AGMPs [6] |
| ii. Causes human respiratory disease. Viral antigen in human lung [32] | |||
| Coronaviridae i. MERS-CoV ii. SARS-CoV | ii. Laboratory and health-care workers infected by inhaling aerosols [23] i, ii. Known human-to-human aerosol transmission | Upper respiratory: ii. Viral RNA in nasal/throat swabs [33] | i, ii. Nosocomial transmission [2,11,12] ii. Significant association with AGMPs [11,12,13] |
| Lower respiratory: i, ii. Causes human respiratory disease. Virus isolated from lung and sputum [33,34] | |||
| Filoviridae i. Ebolaviruses ii. Marburg virus | i, ii. NHPs infected by aerosol administration [35] | Upper respiratory: i. Isolated from human saliva [36] ii. Isolated from NHP saliva [37] | i. Nosocomial transmission [1] i. Possible association with AGMPs [1] |
| Lower respiratory: i. Virus particles detected in human alveolar space [38] | |||
| Orthomyxoviridae i. Influenza A virus (H5N1, H7N9, pandemic H1N1) | i. Known human-to-human aerosol transmission | Upper respiratory: i. Viral RNA in pharyngeal and nasal swabs. [39] | i. Nosocomial transmission [39] |
| Lower respiratory: i. Causes human respiratory disease [10] | |||
| Paramyxoviridae i. Hendra virus ii. Nipah virus | i. ii. Suspected aerosol transmission i. NHPs infected by aerosol administration [40] | Upper respiratory: ii. Isolated from human nasal and throat secretions [41] | ii. Nosocomial transmission [42] |
| Lower respiratory: i, ii Causes human respiratory disease.i. Viral antigen in human lung [43] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Judson, S.D.; Munster, V.J. Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures. Viruses 2019, 11, 940. https://doi.org/10.3390/v11100940
Judson SD, Munster VJ. Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures. Viruses. 2019; 11(10):940. https://doi.org/10.3390/v11100940
Chicago/Turabian StyleJudson, Seth D., and Vincent J. Munster. 2019. "Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures" Viruses 11, no. 10: 940. https://doi.org/10.3390/v11100940
APA StyleJudson, S. D., & Munster, V. J. (2019). Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures. Viruses, 11(10), 940. https://doi.org/10.3390/v11100940