Longitudinal Assessment of Cytokine Expression and Plasminogen Activation in Hantavirus Cardiopulmonary Syndrome Reveals Immune Regulatory Dysfunction in End-Stage Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Analyses of 23 Cytokines
2.3. Analyses of Plasma Levels of uPA and PAI-1
2.4. Assessment of Viral RNA Load with Quantitative PCR with Reverse Transcription (RT-qPCR)
2.5. Statistical Analysis
3. Results
3.1. Study Group
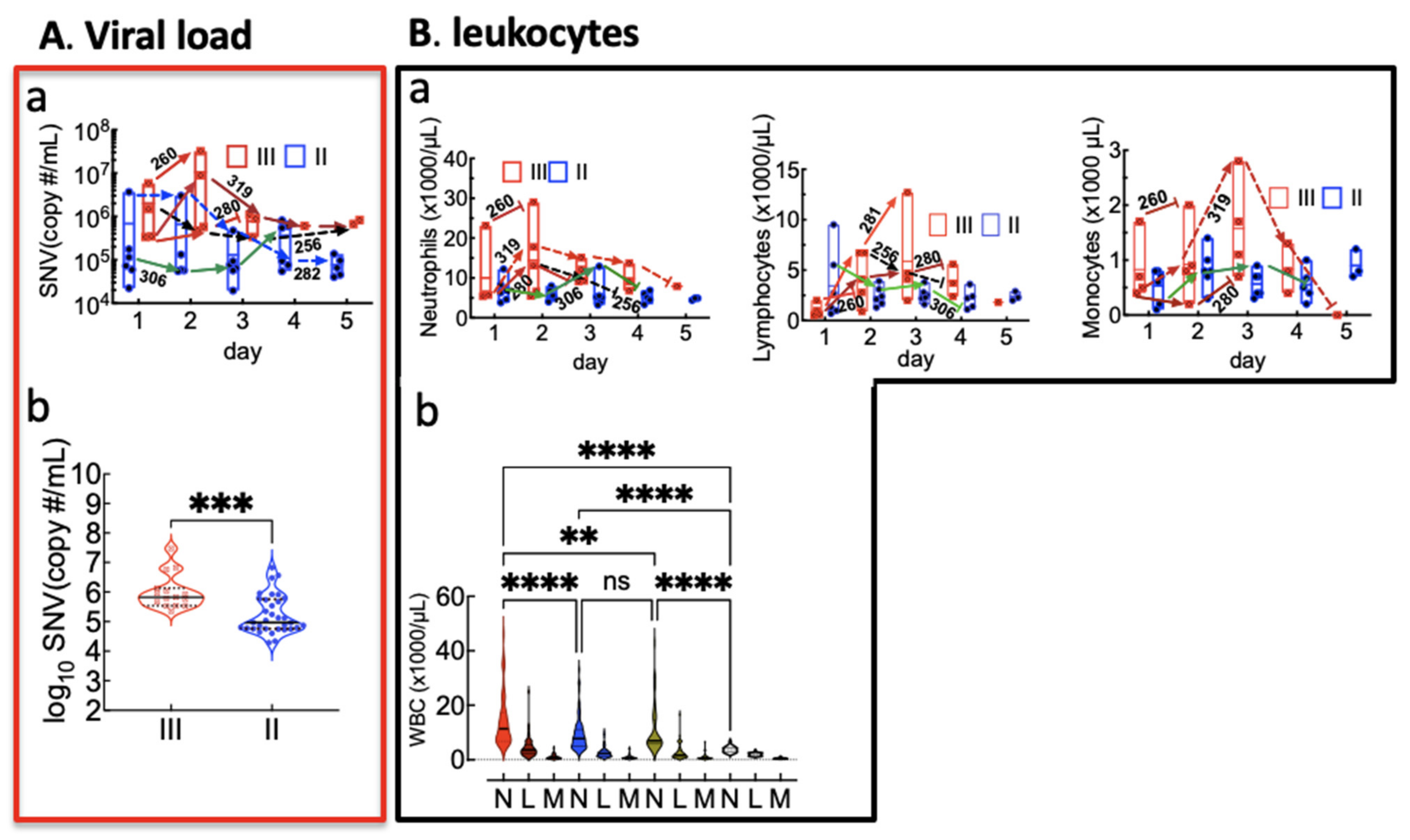
3.2. Overt Neutrophilia Is Associated with HCPS Severity and Mortality
3.3. Peak Innate and Adaptive Immune Responses in Class III Cases Are Higher Than in Class II Cases
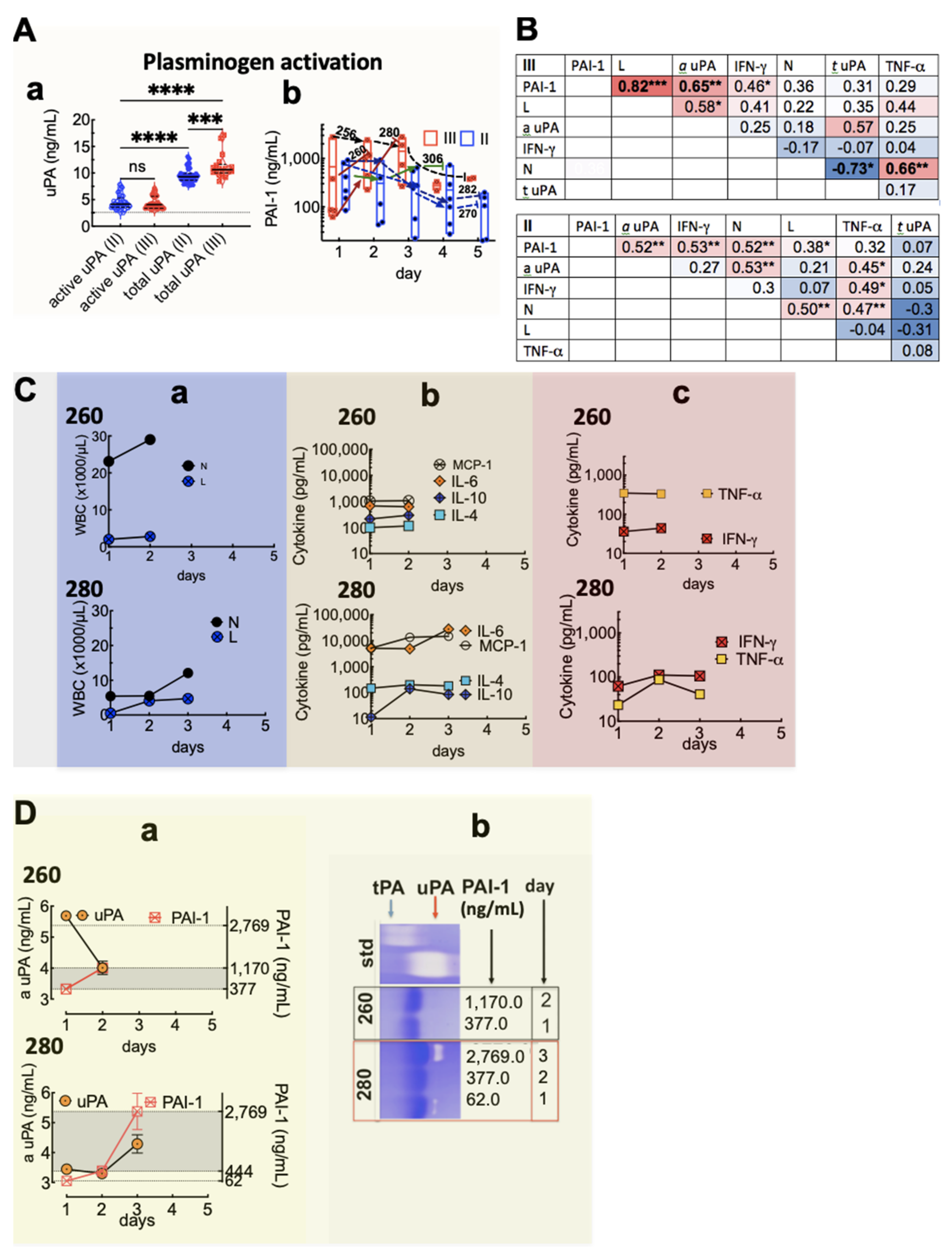
3.4. Plasma Levels of uPA and PAI-1 and Their Link to Lymphocyte and Cytokine Expression
3.5. Longitudinal Immune Profiling of Cytokine and Plasminogen Activation Factors in HCPS
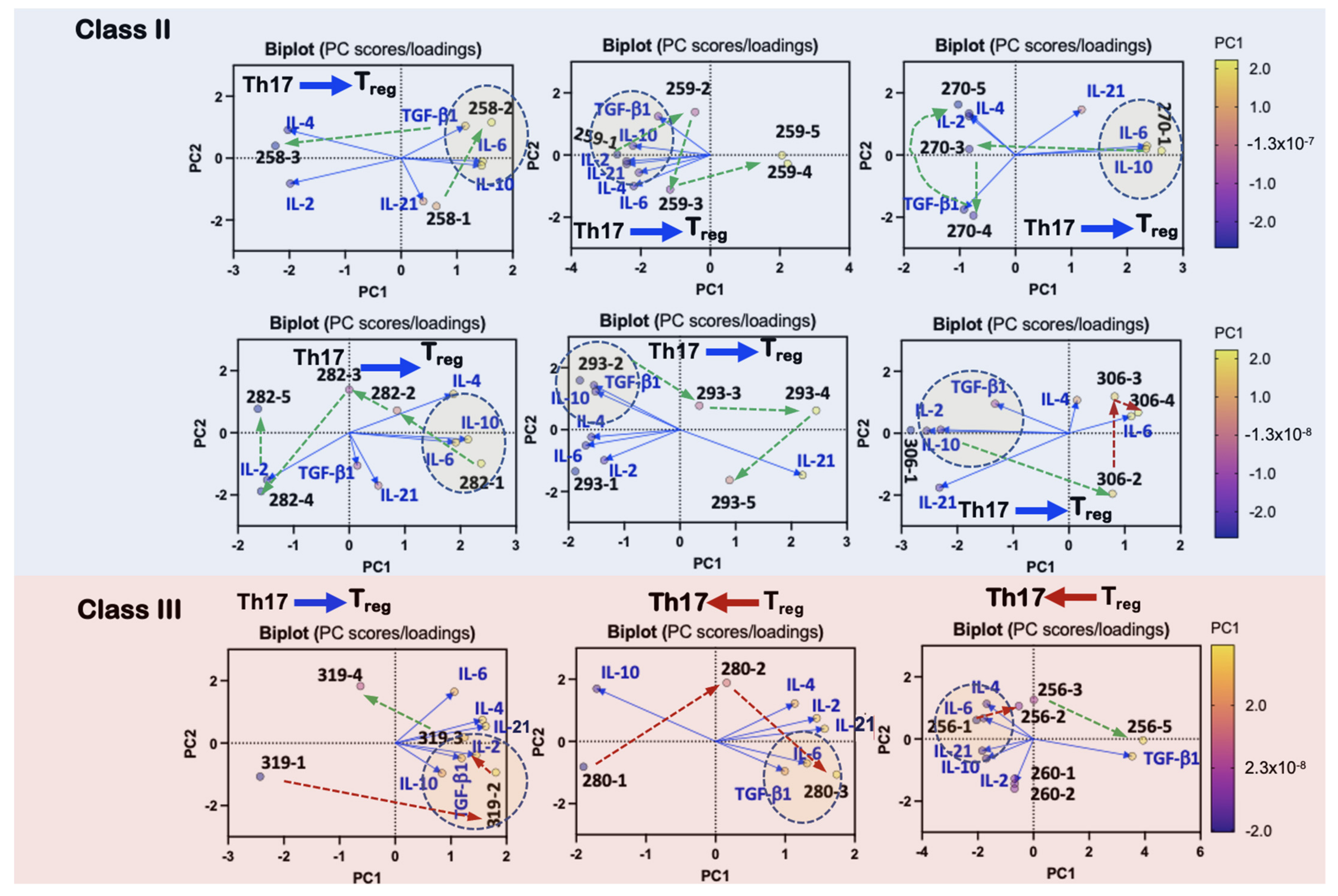
3.6. Robust Adaptive Immune Profile Is Correlated to Severity
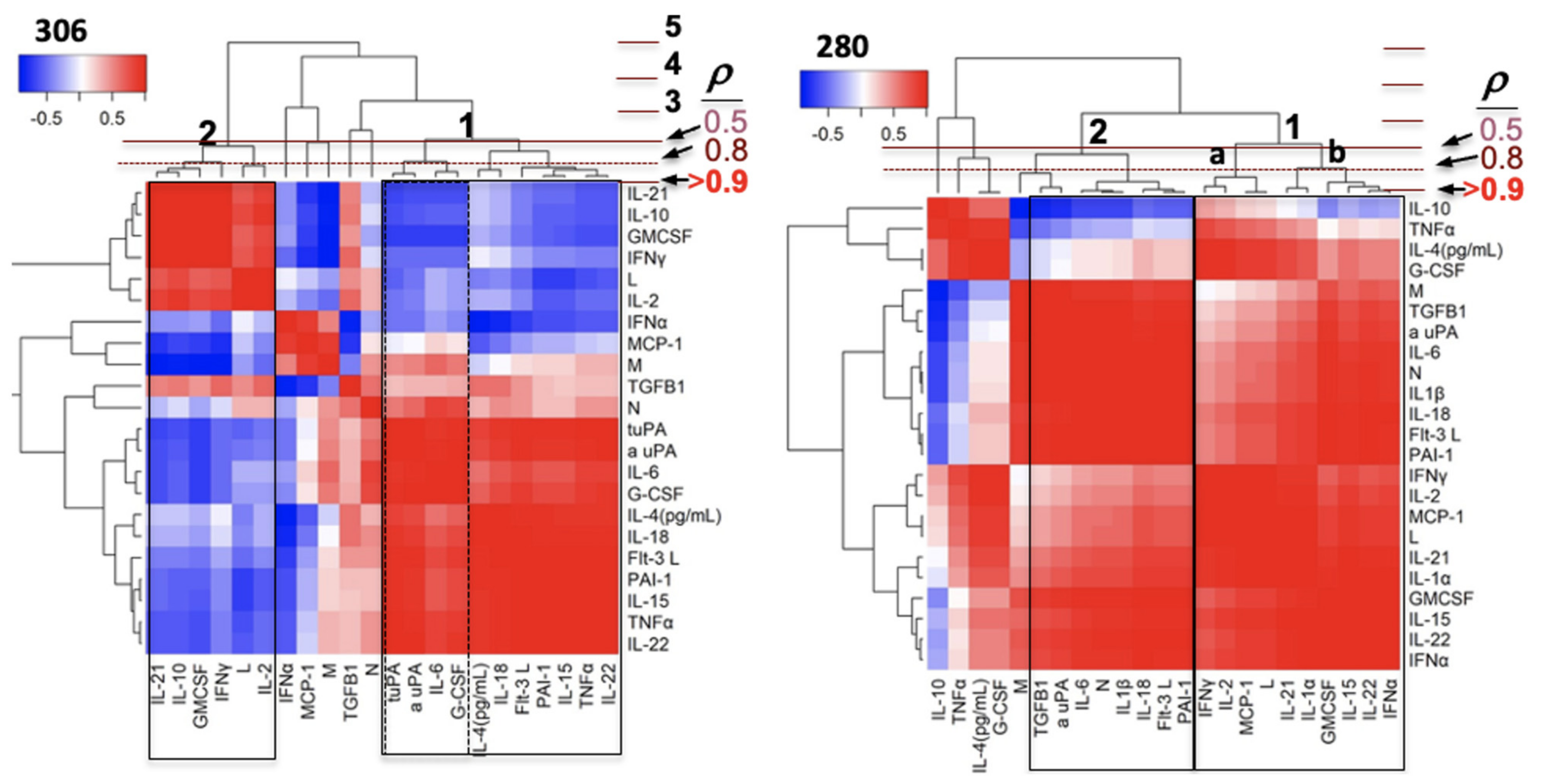
3.7. Differential Development of Innate and Adaptive Immunity Separates Survivors and Non-Survivors of HCPS
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hjelle, B.; Torres-Perez, F. Hantaviruses in the americas and their role as emerging pathogens. Viruses 2010, 2, 2559–2586. [Google Scholar] [CrossRef] [PubMed]
- Zaki, S.R.; Greer, P.W.; Coffield, L.M.; Goldsmith, C.S.; Nolte, K.B.; Foucar, K.; Feddersen, R.M.; Zumwalt, R.E.; Miller, G.L.; Khan, A.S.; et al. Hantavirus pulmonary syndrome. Pathogenesis of an emerging infectious disease. Am. J. Pathol. 1995, 146, 552–579. [Google Scholar] [PubMed]
- Rasmuson, J.; Pourazar, J.; Mohamed, N.; Lejon, K.; Evander, M.; Blomberg, A.; Ahlm, C. Cytotoxic immune responses in the lungs correlate to disease severity in patients with hantavirus infection. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.A.; Campos, G.M.; Moreli, M.L.; Souza, R.L.; Aquino, V.H.; Saggioro, F.P.; Figueiredo, L.T. Hantavirus cardiopulmonary syndrome: Immune response and pathogenesis. Microbes Infect. Inst. Pasteur 2006, 8, 2324–2330. [Google Scholar] [CrossRef]
- Klingstrom, J.; Hardestam, J.; Stoltz, M.; Zuber, B.; Lundkvist, A.; Linder, S.; Ahlm, C. Loss of cell membrane integrity in puumala hantavirus-infected patients correlates with levels of epithelial cell apoptosis and perforin. J. Virol. 2006, 80, 8279–8282. [Google Scholar] [CrossRef]
- Schonrich, G.; Kruger, D.H.; Raftery, M.J. Hantavirus-induced disruption of the endothelial barrier: Neutrophils are on the payroll. Front. Microbiol. 2015, 6, 222. [Google Scholar] [CrossRef]
- Scholz, S.; Baharom, F.; Rankin, G.; Maleki, K.T.; Gupta, S.; Vangeti, S.; Pourazar, J.; Discacciati, A.; Hoijer, J.; Bottai, M.; et al. Human hantavirus infection elicits pronounced redistribution of mononuclear phagocytes in peripheral blood and airways. PLoS Pathog. 2017, 13, e1006462. [Google Scholar] [CrossRef] [PubMed]
- Morzunov, S.P.; Khaiboullina, S.F.; St Jeor, S.; Rizvanov, A.A.; Lombardi, V.C. Multiplex Analysis of serum cytokines in humans with hantavirus pulmonary syndrome. Front. Immunol. 2015, 6, 432. [Google Scholar] [CrossRef]
- Wernly, J.A.; Dietl, C.A.; Tabe, C.E.; Pett, S.B.; Crandall, C.; Milligan, K.; Crowley, M.R. Extracorporeal membrane oxygenation support improves survival of patients with Hantavirus cardiopulmonary syndrome refractory to medical treatment. Eur. J. Cardio Thorac. Surg. 2011, 40, 1334–1340. [Google Scholar] [CrossRef]
- Khan, A.S.; Khabbaz, R.F.; Armstrong, L.R.; Holman, R.C.; Bauer, S.P.; Graber, J.; Strine, T.; Miller, G.; Reef, S.; Tappero, J.; et al. Hantavirus pulmonary syndrome: The first 100 US cases. J. Infect. Dis. 1996, 173, 1297–1303. [Google Scholar] [CrossRef]
- Nolte, K.B.; Feddersen, R.M.; Foucar, K.; Zaki, S.R.; Koster, F.T.; Madar, D.; Merlin, T.L.; McFeeley, P.J.; Umland, E.T.; Zumwalt, R.E.; et al. Hantavirus pulmonary syndrome in the United States: A pathological description of a disease caused by a new agent. Hum. Pathol. 1995, 26, 110–120. [Google Scholar] [CrossRef]
- Hjelle, B. Epidemiology and Diagnosis of Hantavirus Infections; Wolters Kluwer; UpToDate: Wellesley, MA, USA, 2019. [Google Scholar]
- Schonrich, G.; Raftery, M.J. Dendritic cells as Achilles’ heel and Trojan horse during varicella zoster virus infection. Front. Microbiol. 2015, 6, 417. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.J.; Butcher, E.C. Rapid acquisition of tissue-specific homing phenotypes by CD4(+) T cells activated in cutaneous or mucosal lymphoid tissues. J. Exp. Med. 2002, 195, 135–141. [Google Scholar] [CrossRef]
- Sigmundsdottir, H.; Butcher, E.C. Environmental cues, dendritic cells and the programming of tissue-selective lymphocyte trafficking. Nat. Immunol. 2008, 9, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Sojka, D.K.; Lazarski, C.A.; Huang, Y.H.; Bromberg, I.; Hughson, A.; Fowell, D.J. Regulation of immunity at tissue sites of inflammation. Immunol. Res. 2009, 45, 239–250. [Google Scholar] [CrossRef]
- Bromley, S.K.; Mempel, T.R.; Luster, A.D. Orchestrating the orchestrators: Chemokines in control of T cell traffic. Nat. Immunol. 2008, 9, 970–980. [Google Scholar] [CrossRef]
- Mikhak, Z.; Strassner, J.P.; Luster, A.D. Lung dendritic cells imprint T cell lung homing and promote lung immunity through the chemokine receptor CCR4. J. Exp. Med. 2013, 210, 1855–1869. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Rothman, A.L.; Kurane, I.; Montoya, J.M.; Nolte, K.B.; Norman, J.E.; Waite, D.C.; Koster, F.T.; Ennis, F.A. High levels of cytokine-producing cells in the lung tissues of patients with fatal hantavirus pulmonary syndrome. J. Infect. Dis. 1999, 179, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Jenison, S.; Hjelle, B.; Simpson, S.; Hallin, G.; Feddersen, R.; Koster, F. Hantavirus pulmonary syndrome: Clinical, diagnostic, and virologic aspects. Semin. Respir. Infect. 1995, 10, 259–269. [Google Scholar] [PubMed]
- Koster, F.; Foucar, K.; Hjelle, B.; Scott, A.; Chong, Y.Y.; Larson, R.; McCabe, M. Rapid presumptive diagnosis of hantavirus cardiopulmonary syndrome by peripheral blood smear review. Am. J. Clin. Pathol. 2001, 116, 665–672. [Google Scholar] [CrossRef]
- Safronetz, D.; Prescott, J.; Feldmann, F.; Haddock, E.R.; Okumura, A.; Brining, D.; Dahlstrom, E.; Porcella, S.F.; Ebihara, H. Pathophysiology of hantavirus pulmonary syndrome in rhesus macaques. Proc. Natl. Acad. Sci. USA 2014, 111, 7114–7119. [Google Scholar] [CrossRef]
- Vaheri, A.; Strandin, T.; Hepojoki, J.; Sironen, T.; Henttonen, H.; Makela, S.; Mustonen, J. Uncovering the mysteries of hantavirus infections. Nat. Rev. Microbiol. 2013, 11, 539–550. [Google Scholar] [CrossRef]
- Ennis, F.A.; Cruz, J.; Spiropoulou, C.F.; Waite, D.; Peters, C.J.; Nichol, S.T.; Kariwa, H.; Koster, F.T. Hantavirus pulmonary syndrome: CD8+ and CD4+ cytotoxic T lymphocytes to epitopes on Sin Nombre virus nucleocapsid protein isolated during acute illness. Virology 1997, 238, 380–390. [Google Scholar] [CrossRef]
- Kilpatrick, E.D.; Terajima, M.; Koster, F.T.; Catalina, M.D.; Cruz, J.; Ennis, F.A. Role of specific CD8+ T cells in the severity of a fulminant zoonotic viral hemorrhagic fever, hantavirus pulmonary syndrome. J. Immunol. 2004, 172, 3297–3304. [Google Scholar] [CrossRef] [PubMed]
- Terajima, M.; Hayasaka, D.; Maeda, K.; Ennis, F.A. Immunopathogenesis of hantavirus pulmonary syndrome and hemorrhagic fever with renal syndrome: Do CD8+ T cells trigger capillary leakage in viral hemorrhagic fevers? Immunol. Lett. 2007, 113, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Brocato, R.L.; Hammerbeck, C.D.; Bell, T.M.; Wells, J.B.; Queen, L.A.; Hooper, J.W. A lethal disease model for hantavirus pulmonary syndrome in immunosuppressed Syrian hamsters infected with Sin Nombre virus. J. Virol. 2014, 88, 811–819. [Google Scholar] [CrossRef] [PubMed]
- Hammerbeck, C.D.; Brocato, R.L.; Bell, T.M.; Schellhase, C.W.; Mraz, S.R.; Queen, L.A.; Hooper, J.W. Depletion of Alveolar macrophages does not prevent hantavirus disease pathogenesis in golden syrian hamsters. J. Virol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Bondu, V.; Schrader, R.; Gawinowicz, M.A.; McGuire, P.; Lawrence, D.A.; Hjelle, B.; Buranda, T. Elevated cytokines, thrombin and PAI-1 in severe HCPS Patients due to sin nombre virus. Viruses 2015, 7, 559–589. [Google Scholar] [CrossRef] [PubMed]
- Osterholzer, J.J.; Christensen, P.J.; Lama, V.; Horowitz, J.C.; Hattori, N.; Subbotina, N.; Cunningham, A.; Lin, Y.; Murdock, B.J.; Morey, R.E.; et al. PAI-1 promotes the accumulation of exudate macrophages and worsens pulmonary fibrosis following type II alveolar epithelial cell injury. J. Pathol. 2012, 228, 170–180. [Google Scholar] [CrossRef]
- Knudsen, E.C.; Seljeflot, I.; Abdelnoor, M.; Eritsland, J.; Mangschau, A.; Muller, C.; Arnesen, H.; Andersen, G.O. Elevated levels of PAI-1 activity and t-PA antigen are associated with newly diagnosed abnormal glucose regulation in patients with ST-elevation myocardial infarction. J. Thromb. Haemost. 2011, 9, 1468–1474. [Google Scholar] [CrossRef]
- Czekay, R.P.; Wilkins-Port, C.E.; Higgins, S.P.; Freytag, J.; Overstreet, J.M.; Klein, R.M.; Higgins, C.E.; Samarakoon, R.; Higgins, P.J. PAI-1: An Integrator of cell signaling and migration. Int. J. Cell Biol. 2011, 2011, 562481. [Google Scholar] [CrossRef]
- Vaughan, D.E. PAI-1 and atherothrombosis. J. Thromb. Haemost. 2005, 3, 1879–1883. [Google Scholar] [CrossRef]
- Dellas, C.; Loskutoff, D.J. Historical analysis of PAI-1 from its discovery to its potential role in cell motility and disease. Thromb. Haemost. 2005, 93, 631–640. [Google Scholar] [CrossRef]
- Bajou, K.; Maillard, C.; Jost, M.; Lijnen, R.H.; Gils, A.; Declerck, P.; Carmeliet, P.; Foidart, J.M.; Noel, A. Host-derived plasminogen activator inhibitor-1 (PAI-1) concentration is critical for in vivo tumoral angiogenesis and growth. Oncogene 2004, 23, 6986–6990. [Google Scholar] [CrossRef]
- Smith, H.W.; Marshall, C.J. Regulation of cell signalling by uPAR. Nat. Rev. Mol. Cell. Bio. 2010, 11, 23–36. [Google Scholar] [CrossRef]
- Bondu, V.; Bitting, C.; Poland, V.L.; Hanson, J.A.; Harkins, M.S.; Lathrop, S.; Nolte, K.B.; Lawrence, D.A.; Buranda, T. Upregulation of P2Y2R, Active uPA and PAI-1 Are Essential Components of Hantavirus Cardiopulmonary Syndrome. Front. Cell. Infect. Microbiol. 2018, 8, 169. [Google Scholar] [CrossRef]
- Pannell, R.; Gurewich, V. Activation of Plasminogen by single-chain urokinase or by 2-chain urokinase-a demonstration that single-chain urokinase has a low catalytic activity (prourokinase). Blood 1987, 69, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Kasai, S.; Arimura, H.; Nishida, M.; Suyama, T. Proteolytic Cleavage of single-chain pro-urokinase induces conformational change which follows activation of the zymogen and reduction of its high-affinity for fibrin. J. Biol. Chem. 1985, 260, 2377–2381. [Google Scholar] [CrossRef]
- Higazi, A.A.; Mazar, A.; Wang, J.; Reilly, R.; Henkin, J.; Kniss, D.; Cines, D. Single-chain urokinase-type plasminogen activator bound to its receptor is relatively resistant to plasminogen activator inhibitor type 1. Blood 1996, 87, 3545–3549. [Google Scholar] [CrossRef] [PubMed]
- Gyetko, M.R.; Todd, R.F.; Wilkinson, C.C.; Sitrin, R.G. The Urokinase receptor is required for human monocyte chemotaxis in-vitro. J. Clin. Investig. 1994, 93, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Gyetko, M.R.; Shollenberger, S.B.; Sitrin, R.G. Urokinase Expression in mononuclear phagocytes-cytokine-specific modulation by interferon-gamma and tumor-necrosis-factor-alpha. J. Leukoc. Biol. 1992, 51, 256–263. [Google Scholar] [CrossRef][Green Version]
- Gyetko, M.R.; Sud, S.; Sonstein, J.; Polak, T.; Sud, A.; Curtis, J.L. Cutting edge: Antigen-driven lymphocyte recruitment to the lung is diminished in the absence of urokinase-type plasminogen activator (uPA) receptor, but is independent of uPA. J. Immunol. 2001, 167, 5539–5542. [Google Scholar] [CrossRef]
- Kindzelskii, A.L.; Amhad, I.; Keller, D.; Zhou, M.J.; Haugland, R.P.; Garni-Wagner, B.A.; Gyetko, M.R.; Todd, R.F.; Petty, H.R. Pericellular proteolysis by leukocytes and tumor cells on substrates: Focal activation and the role of urokinase-type plasminogen activator. Histochem. Cell Biol. 2004, 121, 299–310. [Google Scholar] [CrossRef]
- Connolly, B.M.; Choi, E.Y.; Gardsvoll, H.; Bey, A.L.; Currie, B.M.; Chavakis, T.; Liu, S.; Molinolo, A.; Ploug, M.; Leppla, S.H.; et al. Selective abrogation of the uPA-uPAR interaction in vivo reveals a novel role in suppression of fibrin-associated inflammation. Blood 2010, 116, 1593–1603. [Google Scholar] [CrossRef] [PubMed]
- Manchanda, N.; Schwartz, B.S. Interaction of single-chain urokinase and plasminogen activator inhibitor type 1. J. Biol. Chem. 1995, 270, 20032–20035. [Google Scholar] [CrossRef]
- Teesalu, T.; Kulla, A.; Simisker, A.; Siren, V.; Lawrence, D.A.; Asser, T.; Vaheri, A. Tissue plasminogen activator and neuroserpin are widely expressed in the human central nervous system. Thromb. Haemost. 2004, 92, 358–368. [Google Scholar] [CrossRef]
- Botten, J.; Mirowsky, K.; Kusewitt, D.; Bharadwaj, M.; Yee, J.; Ricci, R.; Feddersen, R.M.; Hjelle, B. Experimental infection model for Sin Nombre hantavirus in the deer mouse (peromyscus maniculatus). Proc. Natl. Acad. Sci. USA 2000, 97, 10578–10583. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Guo, Y.; Sheng, Q.; Shyr, Y. Advanced heat map and clustering analysis using heatmap3. Biomed. Res. Int. 2014, 2014, 986048. [Google Scholar] [CrossRef] [PubMed]
- Xiao, R.; Yang, S.; Koster, F.; Ye, C.; Stidley, C.; Hjelle, B. Sin nombre viral RNA load in patients with hantavirus cardiopulmonary syndrome. J. Infect. Dis. 2006, 194, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- Terajima, M.; Hendershot III, J.D.; Kariwa, H.; Koster, F.T.; Hjelle, B.; Goade, D.; DeFronzo, M.C.; Ennis, F.A. High levels of viremia in patients with the Hantavirus pulmonary syndrome. J. Infect. Dis. 1999, 180, 2030–2034. [Google Scholar] [CrossRef]
- Iwasaki, A.; Medzhitov, R. Control of adaptive immunity by the innate immune system. Nat. Immunol. 2015, 16, 343–353. [Google Scholar] [CrossRef]
- Zhu, J.; Yamane, H.; Paul, W.E. Differentiation of effector CD4 T cell populations (*). Annu. Rev. Immunol. 2010, 28, 445–489. [Google Scholar] [CrossRef]
- Zhou, L.; Lopes, J.E.; Chong, M.M.; Ivanov, I.I.; Min, R.; Victora, G.D.; Shen, Y.; Du, J.; Rubtsov, Y.P.; Rudensky, A.Y.; et al. TGF-beta-induced Foxp3 inhibits T(H)17 cell differentiation by antagonizing RORgammat function. Nature 2008, 453, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Dang, E.V.; Barbi, J.; Yang, H.Y.; Jinasena, D.; Yu, H.; Zheng, Y.; Bordman, Z.; Fu, J.; Kim, Y.; Yen, H.R.; et al. Control of T(H)17/T(reg) balance by hypoxia-inducible factor 1. Cell 2011, 146, 772–784. [Google Scholar] [CrossRef] [PubMed]
- Denney, L.; Branchett, W.; Gregory, L.G.; Oliver, R.A.; Lloyd, C.M. Epithelial-derived TGF-beta1 acts as a pro-viral factor in the lung during influenza A infection. Mucosal Immunol. 2018, 11, 523–535. [Google Scholar] [CrossRef]
- Cohen, S.D.; Israel, E.; Spiess-Meier, B.; Wainberg, M.A. Plasminogen activator is an apparent lymphocyte mitogen. J. Immunol. 1981, 126, 1415–1420. [Google Scholar] [PubMed]
- Banys-Paluchowski, M.; Witzel, I.; Aktas, B.; Fasching, P.A.; Hartkopf, A.; Janni, W.; Kasimir-Bauer, S.; Pantel, K.; Schon, G.; Rack, B.; et al. The prognostic relevance of urokinase-type plasminogen activator (uPA) in the blood of patients with metastatic breast cancer. Sci. Rep. 2019, 9, 2318. [Google Scholar] [CrossRef] [PubMed]
- Chandler, W.L. A kinetic model of the circulatory regulation of tissue plasminogen activator. Thromb. Haemost. 1991, 66, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.M.; Stocki, S.; Jiang, L.; Brew, K.; Gordon, S.; Vaughan, D.E.; Brown, N.J.; Poku, K.A.; Moore, J.H. A population-based study in Ghana to investigate inter-individual variation in plasma t-PA and PAI-1. Ethn. Dis. 2007, 17, 492–497. [Google Scholar]
- Sitrin, R.G.; Todd, R.F.; Mizukami, I.F.; Gross, T.J.; Shollenberger, S.B.; Gyetko, M.R. Cytokine-Specific regulation of urokinase receptor (Cd87) expression by U937 mononuclear phagocytes. Blood 1994, 84, 1268–1275. [Google Scholar]
- Kaplanski, G.; Marin, V.; Montero-Julian, F.; Mantovani, A.; Farnarier, C. IL-6: A regulator of the transition from neutrophil to monocyte recruitment during inflammation. Trends Immunol. 2003, 24, 25–29. [Google Scholar] [CrossRef]
- Jones, S.A. Directing transition from innate to acquired immunity: Defining a role for IL-6. J. Immunol. 2005, 175, 3463–3468. [Google Scholar] [CrossRef]
- Hunter, C.A.; Jones, S.A. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 2015, 16, 448–457. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.C. NF-kappaB signaling in inflammation. Signal Transduct. Target. Ther. 2017, 2. [Google Scholar] [CrossRef]
- Yoo, J.K.; Kwon, H.; Khil, L.Y.; Zhang, L.; Jun, H.S.; Yoon, J.W. IL-18 induces monocyte chemotactic protein-1 production in macrophages through the phosphatidylinositol 3-kinase/Akt and MEK/ERK1/2 pathways. J. Immunol. 2005, 175, 8280–8286. [Google Scholar] [CrossRef] [PubMed]
- Cicchese, J.M.; Evans, S.; Hult, C.; Joslyn, L.R.; Wessler, T.; Millar, J.A.; Marino, S.; Cilfone, N.A.; Mattila, J.T.; Linderman, J.J.; et al. Dynamic balance of pro- and anti-inflammatory signals controls disease and limits pathology. Immunol. Rev. 2018, 285, 147–167. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Chong, M.M.; Littman, D.R. Plasticity of CD4+ T cell lineage differentiation. Immunity 2009, 30, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Baker, S.K.; Strickland, S. A critical role for plasminogen in inflammation. J. Exp. Med. 2020, 217. [Google Scholar] [CrossRef] [PubMed]
- Vaday, G.G.; Lider, O. Extracellular matrix moieties, cytokines, and enzymes: Dynamic effects on immune cell behavior and inflammation. J. Leukoc. Biol. 2000, 67, 149–159. [Google Scholar] [CrossRef]
- Santibanez, J.F.; Krstic, J. Transforming growth factor-beta and urokinase type plasminogen interplay in cancer. Curr. protein Pept. Sci. 2018, 19, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Cantrell, D. Signaling in lymphocyte activation. Cold Spring Harb. Perspect. Biol. 2015, 7. [Google Scholar] [CrossRef]
- Mondino, A.; Blasi, F. UPA and uPAR in fibrinolysis, immunity and pathology. Trends Immunol. 2004, 25, 450–455. [Google Scholar] [CrossRef]
- Mahmood, N.; Mihalcioiu, C.; Rabbani, S.A. Multifaceted Role of the urokinase-type plasminogen activator (uPA) and its receptor (uPAR): Diagnostic, prognostic and therapeutic applications. Front. Oncol. 2018, 8, 24. [Google Scholar] [CrossRef] [PubMed]
- Leliefeld, P.H.; Wessels, C.M.; Leenen, L.P.; Koenderman, L.; Pillay, J. The role of neutrophils in immune dysfunction during severe inflammation. Crit. Care 2016, 20, 73. [Google Scholar] [CrossRef]
- Pillay, J.; Tak, T.; Kamp, V.M.; Koenderman, L. Immune suppression by neutrophils and granulocytic myeloid-derived suppressor cells: Similarities and differences. Cell. Mol. Life Sci. 2013, 70, 3813–3827. [Google Scholar] [CrossRef]
- Monteleone, M.; Stanley, A.C.; Chen, K.W.; Brown, D.L.; Bezbradica, J.S.; von Pein, J.B.; Holley, C.L.; Boucher, D.; Shakespear, M.R.; Kapetanovic, R.; et al. Interleukin-1beta maturation triggers its relocation to the plasma membrane for gasdermin-d-dependent and -independent secretion. Cell Rep. 2018, 24, 1425–1433. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.W.; Gross, C.J.; Sotomayor, F.V.; Stacey, K.J.; Tschopp, J.; Sweet, M.J.; Schroder, K. The neutrophil NLRC4 inflammasome selectively promotes IL-1beta maturation without pyroptosis during acute Salmonella challenge. Cell Rep. 2014, 8, 570–582. [Google Scholar] [CrossRef] [PubMed]
- Boucher, D.; Monteleone, M.; Coll, R.C.; Chen, K.W.; Ross, C.M.; Teo, J.L.; Gomez, G.A.; Holley, C.L.; Bierschenk, D.; Stacey, K.J. Caspase-1 self-cleavage is an intrinsic mechanism to terminate inflammasome activity. J. Exp. Med. 2018, 215, 827–840. [Google Scholar] [CrossRef] [PubMed]
- Rathinam, V.A.; Fitzgerald, K.A. Inflammasome complexes: Emerging mechanisms and effector functions. Cell 2016, 165, 792–800. [Google Scholar] [CrossRef]
- Chen, K.W.; Schroder, K. Antimicrobial functions of inflammasomes. Curr. Opin. Microbiol. 2013, 16, 311–318. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Bryce, C.; Grimes, Z.; Pujadas, E.; Ahuja, S.; Beasley, M.B.; Albrecht, R.; Hernandez, T.; Stock, A.; Zhao, Z.; AlRasheed, M.R.; et al. Pathophysiology of SARS-CoV-2: The mount sinai COVID-19 autopsy experience. Mod. Pathol. 2021. [Google Scholar] [CrossRef]
- van der Poll, T.; van de Veerdonk, F.L.; Scicluna, B.P.; Netea, M.G. The immunopathology of sepsis and potential therapeutic targets. Nat. Rev. Immunol. 2017, 17, 407–420. [Google Scholar] [CrossRef]
- Lucas, C.; Wong, P.; Klein, J.; Castro, T.B.R.; Silva, J.; Sundaram, M.; Ellingson, M.K.; Mao, T.; Oh, J.E.; Israelow, B.; et al. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature 2020, 584, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Tanaka, T.; Inoue, H.; Ono, C.; Hashimoto, S.; Kioi, Y.; Matsumoto, H.; Matsuura, H.; Matsubara, T.; Shimizu, K.; et al. IL-6 trans-signaling induces plasminogen activator inhibitor-1 from vascular endothelial cells in cytokine release syndrome. Proc. Natl. Acad. Sci. USA 2020, 117, 22351–22356. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Y.; Warnock, M.; Harbaugh, A.; Yalavarthi, S.; Gockman, K.; Zuo, M.; Madison, J.A.; Knight, J.S.; Kanthi, Y.; Lawrence, D.A. Plasma tissue plasminogen activator and plasminogen activator inhibitor-1 in hospitalized COVID-19 patients. Sci. Rep. 2021, 11, 1580. [Google Scholar] [CrossRef] [PubMed]
- Maleki, K.T.; Garcia, M.; Iglesias, A.; Alonso, D.; Ciancaglini, M.; Hammar, U.; Ljunggren, H.G.; Schierloh, P.; Martinez, V.P.; Klingstrom, J. Serum markers associated with severity and outcome of hantavirus pulmonary syndrome. J. Infect. Dis. 2019, 219, 1832–1840. [Google Scholar] [CrossRef]
- de Biasi, S.; Meschiari, M.; Gibellini, L.; Bellinazzi, C.; Borella, R.; Fidanza, L.; Gozzi, L.; Iannone, A.; Lo Tartaro, D.; Mattioli, M.; et al. Marked T cell activation, senescence, exhaustion and skewing towards TH17 in patients with COVID-19 pneumonia. Nat. Commun. 2020, 11, 3434. [Google Scholar] [CrossRef]
- Gladstone, D.E.; Kim, B.S.; Mooney, K.; Karaba, A.H.; D’Alessio, F.R. Regulatory T Cells for treating patients with COVID-19 and acute respiratory distress syndrome: Two case reports. Ann. Intern. Med. 2020, 173, 852–853. [Google Scholar] [CrossRef]




| ID | Age/Sex | PMH | BMI | On-Set | 1st Blood Draw | On ECMO | off ECMO | Outcome |
|---|---|---|---|---|---|---|---|---|
| 256 | 69/WF | 27.1 | dy0 | dy4 | dy4 | dy8 | III; MOSF, died dy9 | |
| 258 | 61/WF | 21.4 | dy0 | dy7 | dy10 | dy12 | II; discharged dy22 | |
| 259 | 62/WF | 22.8 | dy0 | dy4 | dy4 | dy9 | II; discharged dy17 | |
| 260 * | 63/NAF | UTI, Diabetes, asthma, COPD | dy0 | dy6 | n/a | n/a | III; died dy7 | |
| 270 | 26 NAF | 31.2 | dy0 | dy3 | dy3 | dy8 | II; discharged dy26 | |
| 280 | 30/M | 32.1 | dy0 | dy3 | dy4 | dy6 | III; MSOF, DIC, died dy6 | |
| 281 | 37/NAM | Diabetes, tobacco use disorder | 32.9 | dy0 | dy3 | dy4 | dy6 | III; Hemorrhagic shock died dy6 |
| 282 | 16/NAM | none | 23.0 | dy0 | dy4 | dy4 | dy7 | II; discharged dy30 |
| 293 | 18/HM | enlarged right axillary lymph node and smaller left axillary lymph nodes. | 20.9 | dy0 | dy6 | dy7 | dy9 | II; discharged from ICU dy14 |
| 306 * | 65/WM | Enterococcus, Candidiasis of Mouth | 28.8 | dy0 | dy5 | dy5 | dy11 | II; transferred to SNIF dy35 |
| 319 * | 51/WF | Candidiasis of skin, nails, septicemia, pneumonia, herpes simplex | 27.1 | dy0 | dy5 | dy6 | dy13 | III; post ECMO complications died dy29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simons, P.; Guo, Y.; Bondu, V.; Tigert, S.L.; Harkins, M.; Goodfellow, S.; Tompkins, C.; Chabot-Richards, D.; Yang, X.O.; Bosc, L.G.; et al. Longitudinal Assessment of Cytokine Expression and Plasminogen Activation in Hantavirus Cardiopulmonary Syndrome Reveals Immune Regulatory Dysfunction in End-Stage Disease. Viruses 2021, 13, 1597. https://doi.org/10.3390/v13081597
Simons P, Guo Y, Bondu V, Tigert SL, Harkins M, Goodfellow S, Tompkins C, Chabot-Richards D, Yang XO, Bosc LG, et al. Longitudinal Assessment of Cytokine Expression and Plasminogen Activation in Hantavirus Cardiopulmonary Syndrome Reveals Immune Regulatory Dysfunction in End-Stage Disease. Viruses. 2021; 13(8):1597. https://doi.org/10.3390/v13081597
Chicago/Turabian StyleSimons, Peter, Yan Guo, Virginie Bondu, Susan L. Tigert, Michelle Harkins, Samuel Goodfellow, Cana Tompkins, Devon Chabot-Richards, Xuexian O. Yang, Laura Gonzalez Bosc, and et al. 2021. "Longitudinal Assessment of Cytokine Expression and Plasminogen Activation in Hantavirus Cardiopulmonary Syndrome Reveals Immune Regulatory Dysfunction in End-Stage Disease" Viruses 13, no. 8: 1597. https://doi.org/10.3390/v13081597
APA StyleSimons, P., Guo, Y., Bondu, V., Tigert, S. L., Harkins, M., Goodfellow, S., Tompkins, C., Chabot-Richards, D., Yang, X. O., Bosc, L. G., Bradfute, S., Lawrence, D. A., & Buranda, T. (2021). Longitudinal Assessment of Cytokine Expression and Plasminogen Activation in Hantavirus Cardiopulmonary Syndrome Reveals Immune Regulatory Dysfunction in End-Stage Disease. Viruses, 13(8), 1597. https://doi.org/10.3390/v13081597









