Evaluation of Clinical Biomarkers Related to CD4 Recovery in HIV-Infected Patients—5-Year Observation
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Assessments
2.3. Statistical Analysis
2.4. Ethics Approval
3. Results
3.1. Study Group
3.2. Antiretroviral Therapy
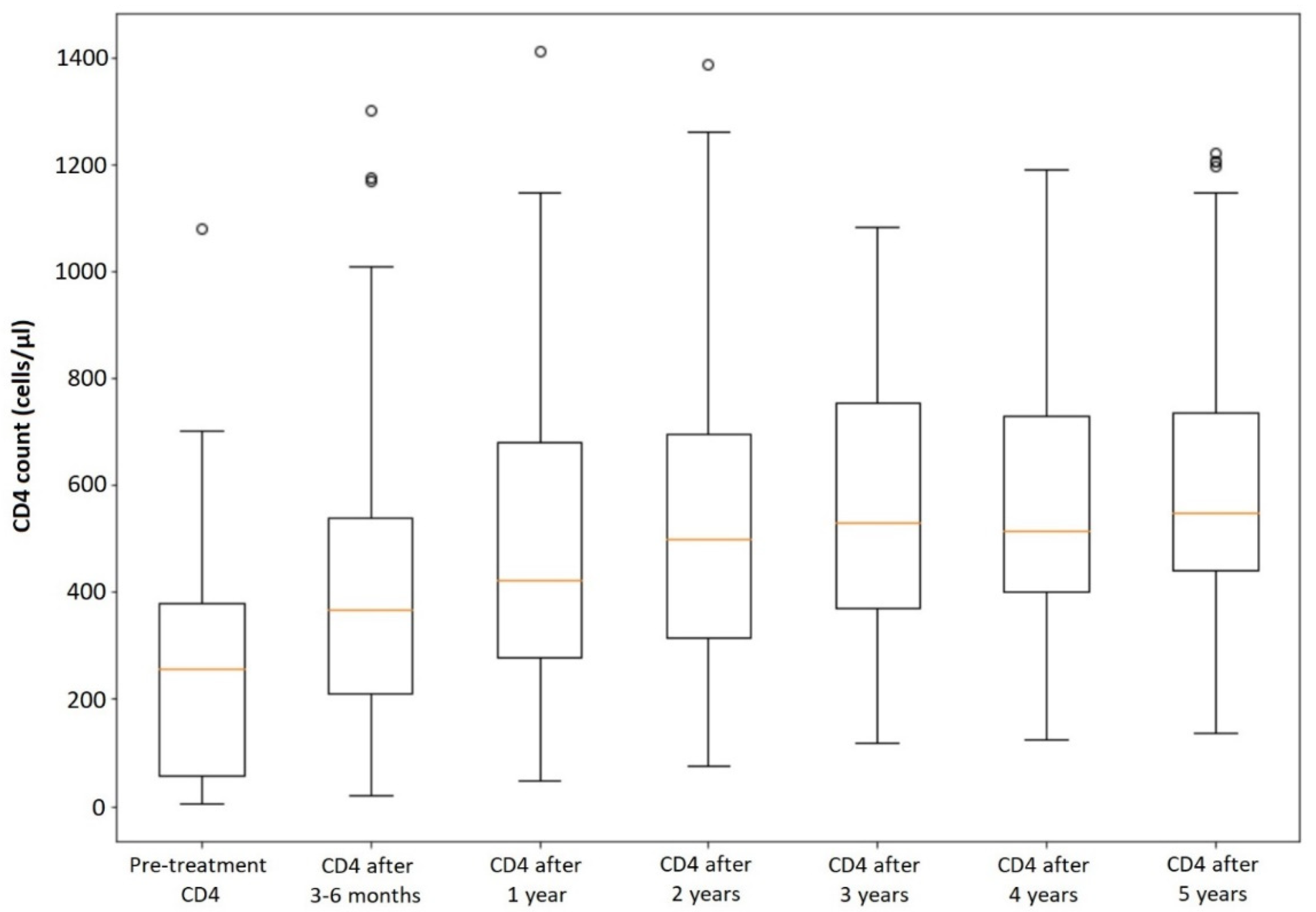
3.3. CD4 Recovery in All Patients
3.4. CD4 Recovery Depending on Clinical Biomarkers
3.5. CD4 Recovery Depending on the Regimens of Antiretroviral Therapy
4. Discussion
4.1. CD4 Recovery Depending on Patient’s Age
4.2. The Impact of Baseline CD4 Count on CD4 Recovery
4.3. CD4 Recovery in Patients Who Start ART with Acute HIV Infection
4.4. HIV Viral Load and CD4 Recovery
4.5. CD4 Recovery Depending on Patient’s Gender
4.6. The Influence of HCV/HBV Coinfection on CD4 Normalization
4.7. Comorbidities and CD4 Recovery
4.8. The Impact of the Presence of AIDS-Defining Diseases on CD4 Recovery
4.9. Applied Regimen of ART Influencing CD4 Recovery
4.10. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fact Sheet—Latest Statistics on the Status of the AIDS Epidemic. UNAIDS. 2021. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 3 August 2022).
- European Center for Disease Prevention and Control (ECDC)/WHO Regional Office for Europe. HIV/AIDS Surveillance in Europe; 2019 Data; ECDC: Stockholm, Sweden, 2020. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/hiv-surveillance-report-2020.pdf (accessed on 3 August 2022).
- Shenoy, N.; Ramapuram, J.; Shenoy, A.; Ahmed, J.; Srikant, N. Incidence of Opportunistic Infections among HIV-Positive Adults on Highly Active Antiretroviral Therapy in a Teaching Hospital, India: Prospective Study. J. Int. Assoc. Provid. AIDS Care 2017, 16, 309–311. [Google Scholar] [CrossRef]
- Gaines, H.; von Sydow, M.A.; von Stedingk, L.V.; Biberfeld, G.; Böttiger, B.; Hansson, L.O.; Lundbergh, P.; Sönnerborg, A.B.; Wasserman, J.; Strannegård, O. Immunological changes in primary HIV-1 infection. AIDS 1990, 4, 995–1000. [Google Scholar] [CrossRef] [PubMed]
- Sobrino-Vegas, P.; Moreno, S.; Rubio, R.; Viciana, P.; Bernardino, J.I.; Blanco, J.R.; Bernal, E.; Asensi, V.; Pulido, F.; del Amo, J.; et al. Impact of late presentation of HIV infection on short-, mid- and long-term mortality and causes of death in a multicenter national cohort: 2004–2013. J. Infect. 2016, 72, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Marcus, J.L.; Leyden, W.A.; Alexeeff, S.E.; Anderson, A.N.; Hechter, R.C.; Hu, H.; Lam, J.O.; Towner, W.J.; Yuan, Q.; Horberg, M.A.; et al. Comparison of Overall and Comorbidity-Free Life Expectancy Between Insured Adults with and Without HIV Infection, 2000-2016. JAMA Netw. Open 2020, 3, e207954. [Google Scholar] [CrossRef]
- CDC. Revised Guidelines for Performing CD4+ T-Cell Determinations in Persons Infected with Human Immunodeficiency Virus (HIV). 1997. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00045580.htm (accessed on 10 August 2022).
- Gazzola, L.; Tincati, C.; Bellistrì, G.M.; Monforte, A.D.; Marchetti, G.C. The Absence of CD4+ T Cell Count Recovery Despite Receipt of Virologically Suppressive Highly Active Antiretroviral Therapy: Clinical Risk, Immunological Gaps, and Therapeutic Options. Clin. Infect. Dis. 2009, 48, 328–337. [Google Scholar] [CrossRef]
- Gunda, D.W.; Kilonzo, S.B.; Kamugisha, E.; Rauya, E.Z.; Mpondo, B.C. Prevalence and risk factors of poor immune recovery among adult HIV patients attending care and treatment centre in northwestern Tanzania following the use of highly active antiretroviral therapy: A retrospective study. BMC Res. Notes 2017, 10, 197. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Su, B.; Zhang, X.; Liu, Y.; Wu, H.; Zhang, T. Incomplete immune reconstitution in HIV/AIDS patients on antiretroviral therapy: Challenges of immunological non-responders. J. Leukoc. Biol. 2020, 107, 597–612. [Google Scholar] [CrossRef]
- Caby, F.; Guihot, A.; Lambert-Niclot, S.; Guiguet, M.; Boutolleau, D.; Agher, R.; Valantin, M.-A.; Tubiana, R.; Calvez, V.; Marcelin, A.-G.; et al. Determinants of a Low CD4/CD8 Ratio in HIV-1–Infected Individuals Despite Long-term Viral Suppression. Clin. Infect. Dis. 2016, 62, 1297–1303. [Google Scholar] [CrossRef]
- Han, W.M.; Apornpong, T.; Kerr, S.J.; Hiransuthikul, A.; Gatechompol, S.; Do, T.; Ruxrungtham, K.; Avihingsanon, A. CD4/CD8 ratio normalization rates and low ratio as prognostic marker for non-AIDS defining events among long-term virologically suppressed people living with HIV. AIDS Res. Ther. 2018, 15, 13. [Google Scholar] [CrossRef]
- Milanés-Guisado, Y.; Gutiérrez-Valencia, A.; Rodríguez, M.T.; Espinosa, N.; Viciana, P.; López-Cortés, L.F. Absolute CD4+ T cell count overstate immune recovery assessed by CD4+/CD8+ ratio in HIV-infected patients on treatment. PLoS ONE 2018, 13, e0205777. [Google Scholar] [CrossRef]
- Serrano-Villar, S.; Deeks, S.G. CD4/CD8 ratio: An emerging biomarker for HIV. Lancet HIV 2015, 2, e76–e77. [Google Scholar] [CrossRef]
- Lee, S.S.; Wong, N.S.; Wong, B.C.K.; Wong, K.H.; Chan, K.C.W. Combining CD4 recovery and CD4: CD8 ratio restoration as an indicator for evaluating the outcome of continued antiretroviral therapy: An observational cohort study. BMJ Open 2017, 7, e016886. [Google Scholar] [CrossRef]
- Zhabokritsky, A.; Szadkowski, L.; Cooper, C.; Loutfy, M.; Wong, A.; McClean, A.; Hogg, R.S.; Walmsley, S.L.; Brumme, Z.; Burchell, A.N.; et al. Increased CD4: CD8 ratio normalization with implementation of current ART management guidelines. J. Antimicrob. Chemother. 2021, 76, 729–737. [Google Scholar] [CrossRef]
- Leung, V.; Gillis, J.; Raboud, J.; Cooper, C.; Hogg, R.S.; Loutfy, M.R.; Machouf, N.; Montaner, J.S.G.; Rourke, S.B.; Tsoukas, C.; et al. Predictors of CD4: CD8 Ratio Normalization and Its Effect on Health Outcomes in the Era of Combination Antiretroviral Therapy. PLoS ONE 2013, 8, e77665. [Google Scholar] [CrossRef]
- Mussini, C.; Lorenzini, P.; Cozzi-Lepri, A.; Lapadula, G.; Marchetti, G.; Nicastri, E.; Cingolani, A.; Lichtner, M.; Antinori, A.; Gori, A.; et al. CD4/CD8 ratio normalisation and non-AIDS-related events in individuals with HIV who achieve viral load suppression with antiretroviral therapy: An observational cohort study. Lancet HIV 2015, 2, e98–e106. [Google Scholar] [CrossRef]
- Yu, H.L.; Yang, Y.C.; Zhao, Y.; Cao, D.D.; Jin, C.; Ye, R.H.; Cao, Y.F.; Liu, X.J.; Yao, S.T.; Chen, C.; et al. Prevalence and related factors of CD4+ T lymphocytes immune recovery among adult HIV/AIDS on an-tiretroviral therapy in Dehong Dai and Jingpo Autonomous Prefecture. Zhonghua Liu Xing Bing Xue Za Zhi 2021, 42, 1050–1055. [Google Scholar] [CrossRef]
- Chen, J.; Titanji, K.; Sheth, A.N.; Gandhi, R.; McMahon, D.; Ofotokun, I.; Weitzmann, M.N.; De Paris, K.; Dumond, J.B. The effect of age on CD4+ T-cell recovery in HIV-suppressed adult participants: A sub-study from AIDS Clinical Trial Group (ACTG) A5321 and the Bone Loss and Immune Reconstitution (BLIR) study. Immun. Ageing 2022, 19, 4. [Google Scholar] [CrossRef]
- Ezeamama, A.E.; Mupere, E.; Oloya, J.; Martinez, L.; Kakaire, R.; Yin, X.; Sekandi, J.N.; Whalen, C.C. Age, sex, and nutritional status modify the CD4+ T-cell recovery rate in HIV–tuberculosis co-infected patients on combination antiretroviral therapy. Int. J. Infect. Dis. 2015, 35, 73–79. [Google Scholar] [CrossRef]
- Han, W.M.; Apornpong, T.; Handoko, R.; Jantarabenjakul, W.; Gatechompol, S.; Ubolyam, S.; Kerr, S.J.; Avihingsanon, A.; Ruxrungtham, K.; Phanuphak, P.; et al. CD4/CD8 Ratio Recovery of Children and Adolescents Living with HIV With Virological Suppression: A Prospective Cohort Study. J. Pediatr. Infect. Dis. Soc. 2021, 10, 88–96. [Google Scholar] [CrossRef]
- Simms, V.; Rylance, S.; Bandason, T.; Dauya, E.; McHugh, G.; Munyati, S.; Mujuru, H.; Rowland-Jones, S.L.; Weiss, H.A.; Ferrand, R.A. CD4+ cell count recovery following initiation of HIV antiretroviral therapy in older childhood and adolescence. AIDS 2018, 32, 1977–1982. [Google Scholar] [CrossRef]
- Bahemana, E.; The AFRICOS Study Group; Esber, A.; Dear, N.; Ganesan, K.; Parikh, A.; Reed, D.; Maganga, L.; Khamadi, S.; Mizinduko, M.; et al. Impact of age on CD4 recovery and viral suppression over time among adults living with HIV who initiated antiretroviral therapy in the African Cohort Study. AIDS Res. Ther. 2020, 17, 23. [Google Scholar] [CrossRef]
- Polish AIDS Society. Polish AIDS Society Recommendations; PTN AIDS: Warszawa-Wrocław, Poland, 2015. Available online: http://www.ptnaids.pl/attachments/article/20/Rekomendacje%20PTN%20AIDS%202015.pdf (accessed on 21 September 2022).
- Bellissimo, F.; Pinzone, M.R.; Celesia, B.M.; Cacopardo, B.; Nunnari, G. Baseline CD4/CD8 T-cell Ratio Predicts Prompt Immune Restoration upon cART Initiation. Curr. HIV Res. 2016, 14, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Mutoh, Y.; Nishijima, T.; Inaba, Y.; Tanaka, N.; Kikuchi, Y.; Gatanaga, H.; Oka, S. Incomplete Recovery of CD4 Cell Count, CD4 Percentage, and CD4/CD8 Ratio in Patients with Human Immunodeficiency Virus Infection and Suppressed Viremia During Long-term Antiretroviral Therapy. Clin. Infect. Dis. 2018, 67, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Bishop, J.D.; DeShields, S.; Cunningham, T.; Troy, S.B. CD4 Count Recovery After Initiation of Antiretroviral Therapy in Patients Infected with Human Immunodeficiency Virus. Am. J. Med Sci. 2016, 352, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Song, A.; Li, Z.; Luo, Z.; Lu, X.; Wang, R.; Liu, L.; Xia, W.; Wan, Z.; Zhang, T.; Su, B.; et al. Effects of Early and Delayed Antiretroviral Therapy on Plasma Anti-CD4 Autoreactive IgG and Its Association with CD4+ T-Cell Recovery in Acute HIV-Infected Individuals. Front. Pharmacol. 2020, 11, 449. [Google Scholar] [CrossRef] [PubMed]
- Little, S.J. Treatment of Acute HIV Infection and the Potential Role of Acutely HIV-Infected Persons in Cure Studies. Top. Antivir. Med. 2015, 23, 156–160. [Google Scholar]
- Leyre, L.; Kroon, E.; Vandergeeten, C.; Sacdalan, C.; Colby, D.J.; Buranapraditkun, S.; Schuetz, A.; Chomchey, N.; de Souza, M.; Bakeman, W.; et al. Abundant HIV-infected cells in blood and tissues are rapidly cleared upon ART initiation during acute HIV infection. Sci. Transl. Med. 2020, 12, eaav3491. [Google Scholar] [CrossRef]
- Badura, R.; Foxall, R.B.; Ligeiro, D.; Rocha, M.; Godinho-Santos, A.; Trombetta, A.C.; Sousa, A.E. Early ART in Acute HIV-1 Infection: Impact on the B-Cell Compartment. Front. Cell. Infect. Microbiol. 2020, 10, 347. [Google Scholar] [CrossRef]
- Chan, P.; Kerr, S.J.; Kroon, E.; Colby, D.; Sacdalan, C.; Hellmuth, J.; Reiss, P.; Vasan, S.; Ananworanich, J.; Valcour, V.; et al. Cognitive trajectories after treatment in acute HIV infection. AIDS 2021, 35, 883–888. [Google Scholar] [CrossRef]
- Gelpi, M.; Hartling, H.J.; Thorsteinsson, K.; Gerstoft, J.; Ullum, H.; Nielsen, S.D. Immune recovery in acute and chronic HIV infection and the impact of thymic stromal lymphopoietin. BMC Infect. Dis. 2016, 16, 591. [Google Scholar] [CrossRef]
- Handoko, R.; Colby, D.J.; Kroon, E.; Sacdalan, C.; de Souza, M.; Pinyakorn, S.; Prueksakaew, P.; Munkong, C.; Ubolyam, S.; Akapirat, S.; et al. Determinants of suboptimal CD4+ T cell recovery after antiretroviral therapy initiation in a prospective cohort of acute HIV-1 infection. J. Int. AIDS Soc. 2020, 23, e25585. [Google Scholar] [CrossRef]
- Muscatello, A.; Nozza, S.; Fabbiani, M.; De Benedetto, I.; Ripa, M.; Dell’Acqua, R.; Antinori, A.; Pinnetti, C.; Calcagno, A.; Ferrara, M.; et al. Enhanced Immunological Recovery with Early Start of Antiretroviral Therapy During Acute or Early HIV Infection–Results of Italian Network of ACuTe HIV InfectiON (INACTION) Retrospective Study. Pathog. Immun. 2020, 5, 8–33. [Google Scholar] [CrossRef]
- Marconi, V.C.; Grandits, G.; Okulicz, J.F.; Wortmann, G.; Ganesan, A.; Crum-Cianflone, N.; Polis, M.; Landrum, M.; Dolan, M.J.; Ahuja, S.K.; et al. Cumulative Viral Load and Virologic Decay Patterns after Antiretroviral Therapy in HIV-Infected Subjects Influence CD4 Recovery and AIDS. PLoS ONE 2011, 6, e17956. [Google Scholar] [CrossRef]
- Novelli, S.; Delobel, P.; Bouchaud, O.; Avettand-Fenoel, V.; Fialaire, P.; Cabié, A.; Souala, F.; Raffi, F.; Catalan, P.; Weiss, L.; et al. Enhanced immunovirological response in women compared to men after antiretroviral therapy initiation during acute and early HIV-1 infection: Results from a longitudinal study in the French ANRS Primo cohort. J. Int. AIDS Soc. 2020, 23, e25485. [Google Scholar] [CrossRef]
- Scully, E.P. Sex Differences in HIV Infection. Curr. HIV/AIDS Rep. 2018, 15, 136–146. [Google Scholar] [CrossRef]
- Meditz, A.L.; MaWhinney, S.; Allshouse, A.; Feser, W.; Markowitz, M.; Little, S.; Hecht, R.; Daar, E.S.; Collier, A.C.; Margolick, J.; et al. Sex, Race, and Geographic Region Influence Clinical Outcomes Following Primary HIV-1 Infection. J. Infect. Dis. 2011, 203, 442–451. [Google Scholar] [CrossRef]
- Aziz, M.; Livak, B.; Burke-Miller, J.; French, A.L.; Glesby, M.J.; Sharma, A.; Young, M.; Villacres, M.C.; Tien, P.C.; Golub, E.T.; et al. Vitamin D insufficiency may impair CD4 recovery among Women’s Interagency HIV Study participants with advanced disease on HAART. AIDS 2013, 27, 573–578. [Google Scholar] [CrossRef]
- Akhtar, A.; Fatima, S.; Saeed, H.; Soo, C.T.; Khan, A.H. HIV-HCV Coinfection: Prevalence and Treatment Outcomes in Malaysia. Intervirology 2022, 65, 87–93. [Google Scholar] [CrossRef]
- Skinner, N.E.; Vergara, C.; El-Diwany, R.; Paul, H.; Skaist, A.; Wheelan, S.J.; Thomas, D.L.; Ray, S.C.; Balagopal, A.; Bailey, J.R. Decreased Activated CD4+ T Cell Repertoire Diversity After Antiretroviral Therapy in HIV-1/HCV Coinfection Correlates with CD4+ T Cell Recovery. Viral Immunol. 2021, 34, 622–631. [Google Scholar] [CrossRef]
- Emmanuel, B.; El-Kamary, S.S.; Magder, L.S.; Stafford, K.A.; Charurat, M.E.; Poonia, B.; Chairez, C.; McLaughlin, M.; Hadigan, C.; Masur, H.; et al. Immunological recovery in T-cell activation after sustained virologic response among HIV positive and HIV negative chronic Hepatitis C patients. Hepatol. Int. 2019, 13, 270–276. [Google Scholar] [CrossRef]
- Bandera, A.; Lorenzini, P.; Taramasso, L.; Cozzi-Lepri, A.; Lapadula, G.; Mussini, C.; Saracino, A.; Ceccherini-Silberstein, F.; Puoti, M.; Quiros-Roldan, E.; et al. The impact of DAA-mediated HCV eradication on CD4+ and CD8+ T lymphocyte trajectories in HIV/HCV coinfected patients: Data from the ICONA Foundation Cohort. J. Viral Hepat. 2021, 28, 779–786. [Google Scholar] [CrossRef]
- McPhee, C.F.; Sainz, T.; Navarro, M.L. Recovery of CD4 T Cells in HIV/HCV Coinfected Children: Is it Really Impaired? Pediatr. Infect. Dis. J. 2018, 37, 278. [Google Scholar] [CrossRef]
- Malagnino, V.; Cerva, C.; Teti, E.; Campogiani, L.; Compagno, M.; Biland, L.F.; Saderi, L.; Armenia, D.; Salpini, R.; Svicher, V.; et al. Poor CD4/CD8 ratio recovery in HBcAb-positive HIV patients with worse immune status is associated with significantly higher CD8 cell numbers. Sci. Rep. 2021, 11, 3965. [Google Scholar] [CrossRef] [PubMed]
- Nie, Y.; Deng, X.; Lan, Y.; Li, L.; Cai, W.; Li, F.; Hu, F. Impact of HBeAg status on immune recovery in HIV/HBV co-infected patients after highly active antiretroviral therapy. Infect. Genet. Evol. 2021, 91, 104781. [Google Scholar] [CrossRef]
- Houghtaling, L.; Moh, R.; Chekaraou, M.A.; Gabillard, D.; Anglaret, X.; Eholié, S.P.; Zoulim, F.; Danel, C.; Lacombe, K.; Boyd, A. CD4+ T Cell Recovery and Hepatitis B Virus Coinfection in HIV-Infected Patients from Côte d’Ivoire Initiating Antiretroviral Therapy. AIDS Res. Hum. Retrovir. 2018, 34, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Peebles, B.K.; Nchimba, L.; Chilengi, R.; Moore, C.B.; Mubiana-Mbewe, M.; Vinikoor, M.J. Pediatric HIV–HBV Coinfection in Lusaka, Zambia: Prevalence and Short-Term Treatment Outcomes: Table 1. J. Trop. Pediatr. 2015, 61, 464–467. [Google Scholar] [CrossRef][Green Version]
- Kwofie, T.B.; Adigbli, D.; Osei-Yeboah, J.; Ativi, E.; Lokpo, S.Y. Hepatitis B and C infections in HIV-1 patients on combination antiretroviral therapy (cART) in Ghana: Implications for immunologic recovery, clinical response to treatment, and hepatotoxicity. Heliyon 2021, 7, e07172. [Google Scholar] [CrossRef] [PubMed]
- Azzoni, L.; Foulkes, A.S.; Firnhaber, C.; Yin, X.; Crowther, N.J.; Glencross, D.; Lawrie, D.; Stevens, W.; Papasavvas, E.; Sanne, I.; et al. Metabolic and anthropometric parameters contribute to ART-mediated CD4+ T cell recovery in HIV-1-infected individuals: An observational study. J. Int. AIDS Soc. 2011, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.P.-C.; Lee, M.-P.; Wong, N.-S.; Leung, R.K.-K.; Naftalin, C.M.; Lee, S.-S. Association of immune recovery with hyperlipidaemia and apolipoprotein gene polymorphisms following highly active antiretroviral therapy in a cohort of Chinese HIV patients. BMJ Open 2016, 6, e010998. [Google Scholar] [CrossRef]
- Rodríguez-Gallego, E.; Gómez, J.; Pacheco, Y.M.; Peraire, J.; Viladés, C.; Beltrán-Debón, R.; Mallol, R.; López-Dupla, M.; Veloso, S.; Alba, V.; et al. A baseline metabolomic signature is associated with immunological CD4+ T-cell recovery after 36 months of antiretroviral therapy in HIV-infected patients. AIDS 2018, 32, 565–573. [Google Scholar] [CrossRef]
- Manfredi, R.; Calza, L.; Chiodo, F. Prolonged statin administration does not act on the cell-mediated immunity of HIV-infected dyslipidemic patients treated with a steady and effective highly active antiretroviral therapy. A two-year prospective study of statin versus fibrate administration. J. Biol. Regul. Homeost. Agents 2006, 20, 1–9. [Google Scholar]
- Bursztyn, M.; Israel, S. Is CD4+ T-cell recovery—Associated with hypertension during initial antiretroviral therapy in human immunodeficiency virus patients? J. Clin. Hypertens. 2020, 22, 1563–1564. [Google Scholar] [CrossRef]
- Aibibula, W.; Cox, J.; Hamelin, A.-M.; Moodie, E.E.M.; Anema, A.; Klein, M.B.; Brassard, P. The Canadian Co-infection Cohort Investigators Association between depressive symptoms, CD4 count and HIV viral suppression among HIV-HCV co-infected people. AIDS Care 2018, 30, 643–649. [Google Scholar] [CrossRef]
- Shmagel, N.G.; Shmagel, K.V.; Saidakova, E.V.; Korolevskaya, L.B.; Chereshnev, V.A. Discordant response of CD4+ T cells to antiretroviral therapy in HIV-infected patients coinfected with hepatitis C virus is accompanied by increased liver damage. Dokl. Biochem. Biophys. 2015, 465, 358–360. [Google Scholar] [CrossRef]
- Kang, F.; Chen, W.; Zhang, X.; Nie, W.; Fu, J.; Xu, X.; Zhao, P.; Zhang, X.; Li, W.; Wang, F.-S.; et al. Transient Liver Injury Associated with the Early Recovery of HCV-Specific T-Cell Responses and HCV Rebound in HIV-1/HCV Coinfected Patients Undergoing Highly Active Antiretroviral Therapy. JAIDS J. Acquir. Immune Defic. Syndr. 2013, 62, 135–142. [Google Scholar] [CrossRef]
- Bayarsaikhan, S.; Jagdagsuren, D.; Gunchin, B.; Sandag, T. Survival, CD4 T lymphocyte count recovery and immune reconstitution pattern during the first-line combination antiretroviral therapy in patients with HIV-1 infection in Mongolia. PLoS ONE 2021, 16, e0247929. [Google Scholar] [CrossRef]
- Nakanjako, D.; Kiragga, A.N.; Musick, B.S.; Yiannoutsos, C.T.; Wools-Kaloustian, K.; Diero, L.; Oyaro, P.; Lugina, E.; Ssali, J.C.; Kambugu, A.; et al. Frequency and impact of suboptimal immune recovery on first-line antiretroviral therapy within the International Epidemiologic Databases to Evaluate AIDS in East Africa. AIDS 2016, 30, 1913–1922. [Google Scholar] [CrossRef]
- Corbeau, P.; Reynes, J. Immune reconstitution under antiretroviral therapy: The new challenge in HIV-1 infection. Blood 2011, 117, 5582–5590. [Google Scholar] [CrossRef]
- Kim, K.-H.; Yi, J.; Lee, S.H. The CD4 slope can be a predictor of immunologic recovery in advanced HIV patients: A case-control study. Korean J. Intern. Med. 2015, 30, 705–713. [Google Scholar] [CrossRef]
- Fabbiani, M.; Borghetti, A.; Squillace, N.; Colafigli, M.; Taramasso, L.; Lombardi, A.; Rossetti, B.; Ciccullo, A.; Colella, E.; Picarelli, C.; et al. Integrase Inhibitors Use and Cytomegalovirus Infection Predict Immune Recovery in People Living with HIV Starting First-Line Therapy. JAIDS J. Acquir. Immune Defic. Syndr. 2021, 86, 119–127. [Google Scholar] [CrossRef]
- De Salvador-Guillouet, F.; Sakarovitch, C.; Durant, J.; Risso, K.; Demonchy, E.; Roger, P.M.; Fontas, E. Antiretroviral Regimens and CD4/CD8 Ratio Normalization in HIV-Infected Patients during the Initial Year of Treatment: A Cohort Study. PLoS ONE 2015, 10, e0140519. [Google Scholar] [CrossRef]
- Serrano-Villar, S.; Zhou, Y.; Rodgers, A.J.; Moreno, S. Different impact of raltegravir versus efavirenz on CD4/CD8 ratio recovery in HIV-infected patients. J. Antimicrob. Chemother. 2016, 72, 235–239. [Google Scholar] [CrossRef]
- Ambrosioni, J.; Farrera, J.; De Lazzari, E.; Nicolás, D.; Manzardo, C.; Hernández-Meneses, M.M.; Mosquera, M.M.; Ligero, C.; Marcos, M.A.; Sánchez-Palomino, S.; et al. Immunological and virological efficacy of different antiretroviral regimens initiated during acute/recent HIV infection. AIDS 2020, 34, 2269–2274. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, T.; Li, A.; Li, Z.; Hou, J.; Gao, M.; Huang, X.; Su, B.; Wu, H.; Zhang, T.; et al. Adjunct Therapy for CD4+ T-Cell Recovery, Inflammation and Immune Activation in People Living With HIV: A Systematic Review and Meta-Analysis. Front. Immunol. 2021, 12, 632119. [Google Scholar] [CrossRef] [PubMed]




| Variable (n = 68) | Mean (Range) |
|---|---|
| Age | |
| Age of HIV diagnosis (years) | 36.21 (18–65) |
| Age of initiation of ART (years) | 36.78 (18–65) |
| CD4 count and CD4:CD8 ratio | |
| CD4 count at the initiation of ART (cells/µL) | 260.67 (5–1081) |
| CD4:CD8 ratio at the initiation of ART (proportion) | 0.33 (0.01–1.09) |
| CD4 count after 5 years of ART (cells/µL) | 596.93 (136–1223) |
| CD4:CD8 ratio after 5 years of ART (proportion) | 1.04 (0.19–4.95) |
| HIV viral load | |
| HIV viral load at the initiation of ART (copies/mL) | 1,526,393 (106–26,600,930) |
| HIV viral load after 5 years of ART (copies/mL) | undetectable |
| Treatment Regimen | Occurrence n (%) |
|---|---|
| 2 NRTI + PI | 47 (69.12) |
| 2 NRTI + NNRTI | 31 (45.59) |
| 2 NRTI + InSTI | 18 (26.47) |
| 1 NRTI + InSTI | 7 (10.29) |
| Group of Patients | CD4 Cell Count Increase (ΔCD4 Cell Count) | p | CD4:CD8 Ratio Increase (ΔCD4:CD8 Ratio) | p |
|---|---|---|---|---|
| Age of initiation of ART < 35 (n = 33) | 349.85 (247.74) | 0.640 | 0.64 (0.41) | 0.264 |
| Age of initiation of ART ≥ 35 (n = 35) | 323.14 (220.88) | 0.50 (0.50) | ||
| Male gender (n = 61) | 320.00 (225.06) | 0.093 | 0.54 (0.52) | 0.097 |
| Female gender (n = 7) | 476.43 (271.45) | 1.11 (0.94) | ||
| CD4 < 200 cells/µL (n = 30) | 347.50 (218.50) | 0.087 | 0.43 (0.50) | 0.018 |
| CD4 ≥ 200 cells/µL (n = 38) | 302.45 (246.30) | 0.65 (0.50) | ||
| CD4 < 350 cells/µL (n = 46) | 339.00 (197.00) | 0.082 | 0.53 (0.47) | 0.181 |
| CD4 ≥ 350 cells/µL (n = 22) | 274.36 (282.96) | 0.63 (0.74) | ||
| HIV viral load < 1 mln copies/mL (n = 52) | 319.48 (236.42) | 0.292 | 0.54 (0.55) | 0.284 |
| HIV viral load ≥ 1 mln copies/mL (n = 16) | 390.13 (219.58) | 0.70 (0.56) | ||
| Acute HIV infection (n = 8) | 384.50 (53.00) | 0.150 | 0.75 (0.74) | 0.294 |
| No acute HIV infection (n = 60) | 331.13 (245.31) | 0.54 (0.54) | ||
| HCV/HBV coinfection (n = 12) | 321.67 (268.91) | 0.815 | 0.58 (0.36) | 0.292 |
| No HCV/HBV coinfection (n = 56) | 339.20 (227.09) | 0.58 (0.53) | ||
| Any comorbidity (n = 22) | 344.41 (239.01) | 0.199 | 0.51 (0.59) | 0.412 |
| No comorbidities (n = 46) | 311.5 (232.25) | 0.62 (0.38) | ||
| Any opportunistic infection and CD4 < 200 cells/µL (n = 23) | 364.00 (216.00) | 0.490 | 0.43 (0.49) | 0.303 |
| No opportunistic infection and CD4 < 200 cells/µL (n = 7) | 354.00 (169.55) | 0.59 (0.36) |
| Group of Patients | CD4 Count Normalization (≥500 Cells/µL) (n/%) | p | CD4:CD8 Ratio Normalization (≥1) (n/%) | p |
|---|---|---|---|---|
| Age of initiation of ART < 35 (n = 28) | 20 (71.43%) | 0.034 | 16 (57.14%) | 0.063 |
| Age of initiation of ART ≥ 35 (n = 30) | 11 (36.67%) | 7 (23.33%) | ||
| Male gender (n = 52) | 28 (53.85%) | 1.000 | 20 (38.46%) | 0.673 |
| Female gender (n = 6) | 3 (50.00%) | 3 (50.00%) | ||
| CD4 < 200 cells/µL (n = 30) | 11 (36.67%) | 0.034 | 6 (20.00%) | 0.022 |
| CD4 ≥ 200 cells/µL (n = 28) | 20 (71.43%) | 17 (60.71%) | ||
| CD4 < 350 cells/µL (n = 46) | 22 (47.83%) | 0.115 | 16 (34.78%) | 0.006 |
| CD4 ≥ 350 cells/µL (n = 12) | 9 (75.00%) | 7 (58.33%) | ||
| HIV viral load < 1 mln copies/mL (n = 45) | 24 (53.33%) | 1.000 | 16 (35.55%) | 0.006 |
| HIV viral load ≥ 1 mln copies/mL (n = 13) | 7 (53.85%) | 7 (53.85%) | ||
| Acute HIV infection (n = 7) | 7 (100.00%) | 0.012 | 6 (85.71%) | 0.013 |
| No acute HIV infection (n = 51) | 24 (47.06%) | 17 (33.33%) | ||
| HCV/HBV coinfection (n = 9) | 6 (66.66%) | 0.481 | 3 (33.33%) | 0.686 |
| No HCV/HBV coinfection (n = 49) | 25 (51.02%) | 20 (40.82%) | ||
| Any comorbidity (n = 18) | 9 (50.00%) | 0.083 | 7 (38.88%) | 0.061 |
| No comorbidities (n = 40) | 22 (55.00%) | 16 (40.00%) | ||
| Any opportunistic infection and CD4 <200 cells/µL (n = 23) | 8 (34.78%) | 1.000 | 3 (13.04%) | 0.336 |
| No opportunistic infection and CD4 < 200 cells/µL (n = 7) | 3 (42.86%) | 3 (42.86%) |
| Variable | CD4 Cell Count Increase (ΔCD4 Cell Count) | CD4:CD8 Ratio Increase (ΔCD4:CD8 Ratio) | CD4 Cell Count Normalization | CD4:CD8 Ratio Normalization | ||||
|---|---|---|---|---|---|---|---|---|
| b’ | p | b’ | p | b’ | p | b’ | p | |
| Age of initiation of ART | −0.247 | 0.082 | −0.160 | 0.104 | −0.331 | 0.018 | −0.083 | 0.540 |
| Gender | 0.177 | 0.197 | 0.023 | 0.801 | 0.048 | 0.703 | 0.176 | 0.163 |
| Baseline CD4 cell count | −0.286 | 0.089 | 0.342 | 0.003 | 0.212 | 0.220 | 0.077 | 0.651 |
| HIV viral load | −0.077 | 0.677 | 0.151 | 0.196 | −0.023 | 0.886 | 0.012 | 0.938 |
| Acute HIV infection | 0.185 | 0.310 | 0.259 | 0.030 | 0.290 | 0.084 | 0.238 | 0.150 |
| HCV/HBV coinfection | −0.043 | 0.763 | −0.017 | 0.854 | 0.099 | 0.439 | −0.038 | 0.765 |
| Comorbidities | 0.066 | 0.665 | 0.044 | 0.644 | 0.029 | 0.824 | −0.004 | 0.973 |
| Opportunistic infections | 0.136 | 0.449 | −0.219 | 0.082 | 0.072 | 0.685 | −0.331 | 0.065 |
| Variable | PI-Based Therapy (n = 47) | InSTI-Based Therapy (n = 23) | NNRTI-Based Therapy (n = 31) | p |
|---|---|---|---|---|
| CD4 cell count increase | 345.89 (228.52) | 337.43 (265.16) | 328.61 (254.71) | 0.784 |
| CD4:CD8 ratio increase | 0.59 (0.61) | 0.69 (0.51) | 0.50 (0.51) | 0.433 |
| Variable | PI-Based Therapy (n = 39) | InSTI-Based Therapy (n = 19) | NNRTI-Based Therapy (n = 26) | p |
|---|---|---|---|---|
| CD4 count normalization (≥500 cells/µL) (n/%) | 21 (53.85) | 12 (52.17) | 13 (50.00) | 0.251 |
| CD4:CD8 ratio normalization (≥1) (n/%) | 15 (38.46) | 12 (52.17) | 11 (42.31) | 0.150 |
| Variable | No Changes of Regimen (n = 36) | 1 or 2 Changes of Regimen (n = 32) | p |
|---|---|---|---|
| CD4 cell count increase | 319.94 (207.28) | 354.28 (260.96) | 0.159 |
| CD4:CD8 ratio increase | 0.59 (0.37) | 0.62 (0.55) | 0.209 |
| Variable | No Changes of Regimen (n = 32) | 1 or 2 Changes of Regimen (n = 26) | p |
|---|---|---|---|
| CD4 count normalization (≥500 cells/µL) (n/%) | 17 (53.13) | 14 (53.85) | 0.564 |
| CD4:CD8 ratio normalization (≥1) (n/%) | 10 (31.25) | 13 (50.00) | 0.128 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lembas, A.; Załęski, A.; Mikuła, T.; Dyda, T.; Stańczak, W.; Wiercińska-Drapało, A. Evaluation of Clinical Biomarkers Related to CD4 Recovery in HIV-Infected Patients—5-Year Observation. Viruses 2022, 14, 2287. https://doi.org/10.3390/v14102287
Lembas A, Załęski A, Mikuła T, Dyda T, Stańczak W, Wiercińska-Drapało A. Evaluation of Clinical Biomarkers Related to CD4 Recovery in HIV-Infected Patients—5-Year Observation. Viruses. 2022; 14(10):2287. https://doi.org/10.3390/v14102287
Chicago/Turabian StyleLembas, Agnieszka, Andrzej Załęski, Tomasz Mikuła, Tomasz Dyda, Wojciech Stańczak, and Alicja Wiercińska-Drapało. 2022. "Evaluation of Clinical Biomarkers Related to CD4 Recovery in HIV-Infected Patients—5-Year Observation" Viruses 14, no. 10: 2287. https://doi.org/10.3390/v14102287
APA StyleLembas, A., Załęski, A., Mikuła, T., Dyda, T., Stańczak, W., & Wiercińska-Drapało, A. (2022). Evaluation of Clinical Biomarkers Related to CD4 Recovery in HIV-Infected Patients—5-Year Observation. Viruses, 14(10), 2287. https://doi.org/10.3390/v14102287





