First Indications of Omsk Haemorrhagic Fever Virus beyond Russia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Human Sample Collection
2.2. Tick Collection
2.3. Rodent Collection
2.4. Homogenisation and Extraction of Viral RNA
2.5. Real-Time RT-PCR
2.6. Statistical Analysis:
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kovalev, S.Y.; Mazurina, E.A.; Yakimenko, V.V. Molecular Variability and Genetic Structure of Omsk Hemorrhagic Fever Virus, Based on Analysis of the Complete Genome Sequences. Ticks Tick Borne Dis. 2021, 12, 101627. [Google Scholar] [CrossRef]
- Ruzek, D.; Holbrook, M.R.; Yakimenko, V.V.; Karan, L.S.; Tkachev, S.E. Omsk Hemorrhagic Fever Virus. In Manual of Securtiy Sensitive Microbes and Toxins; Dongyou, L., Ed.; CRC Press Inc.: Boca Raton, FL, USA, 2013; pp. 193–200. ISBN 978-1-4665-5396-5. [Google Scholar]
- Růžek, D.; Yakimenko, V.V.; Karan, L.S.; Tkachev, S.E. Omsk Haemorrhagic Fever. Lancet 2010, 376, 2104–2113. [Google Scholar] [CrossRef]
- Akhrem-Akhremovich, R.M. Spring-autumn fever in Omsk region. Proc. Omsk Inst. Epidemiol. Microbiol. Gig. 1948, 3, 13. [Google Scholar]
- Jelínková-Skalová, E.; Tesarová, J.; Buresová, D.; Kouba, K.; Hronovský, V. Laboratory infection with virus of Omsk haemorrhagic fever with neurological and psychiatric symptomatology (author’s transl). Cesk Epidemiol. Mikrobiol. Imunol. 1974, 23, 290–293. [Google Scholar] [PubMed]
- CDC Centers for Disease Control and Prevention Omsk Hemorrhagic Fever (OHF). Available online: https://www.cdc.gov/vhf/omsk/index.html (accessed on 24 January 2022).
- Belov, G.F.; Tofaniuk, E.V.; Kurzhukov, G.P.; Kuznetsova, V.G. The clinico-epidemiological characteristics of Omsk hemorrhagic fever in 1988–1992. Zhurnal Mikrobiol. Epidemiol. Immunobiol. 1995, 4, 88–91. [Google Scholar]
- Shah, S.Z.; Jabbar, B.; Ahmed, N.; Rehman, A.; Nasir, H.; Nadeem, S.; Jabbar, I.; Rahman, Z.U.; Azam, S. Epidemiology, Pathogenesis, and Control of a Tick-Borne Disease-Kyasanur Forest Disease: Current Status and Future Directions. Front. Cell. Infect. Microbiol. 2018, 8, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, D.; Li, L.; Dick, D.; Shope, R.E.; Feldmann, H.; Barrett, A.D.T.; Holbrook, M.R. Analysis of the Complete Genome of the Tick-Borne Flavivirus Omsk Hemorrhagic Fever Virus. Virology 2003, 313, 81–90. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Rollin, P.E.; Nichol, S.T.; Shope, R.E.; Barrett, A.D.T.; Holbrook, M.R. Molecular Determinants of Antigenicity of Two Subtypes of the Tick-Borne Flavivirus Omsk Haemorrhagic Fever Virus. J. Gen. Virol. 2004, 85, 1619–1624. [Google Scholar] [CrossRef]
- Gritsun, T.S.; Nuttall, P.A.; Gould, E.A. Tick-Borne Flaviviruses. In Advances in Virus Research; Chambers, T.J., Monath, T.P., Eds.; The Flaviviruses: Detection, Diagnosis, and Vaccine Development; Academic Press: Cambridge, MA, USA, 2003; Volume 61, pp. 317–371. [Google Scholar]
- Busygin, F.F. Omsk hemorrhagic fever—Current status of the problem. Vopr. Virusol. 2000, 45, 4–9. [Google Scholar]
- Im, J.; Baek, J.-H.; Durey, A.; Kwon, H.; Chung, M.-H.; Lee, J.-S. Geographic Distribution of Tick-Borne Encephalitis Virus Complex. J. Vector Borne Dis. 2020, 57, 14. [Google Scholar] [CrossRef]
- Thiel, H.; Collett, M.; Gould, E.A.; Fauquet, C.; Mayo, M.; Desselberger, U.; Ball, L. Family Falviviridae. In Virus Taxonomy: VIIIth Report of the International Committee on the Taxonomy Viruses; Elsevier: Amsterdam, The Netherlands, 2005; pp. 981–998. [Google Scholar]
- Pattnaik, P. Kyasanur Forest Disease: An Epidemiological View in India. Rev. Med. Virol. 2006, 16, 151–165. [Google Scholar] [CrossRef]
- Zaki, A.M. Isolation of a Flavivirus Related to the Tick-Borne Encephalitis Complex from Human Cases in Saudi Arabia. Trans. R. Soc. Trop. Med. Hyg. 1997, 91, 179–181. [Google Scholar] [CrossRef]
- Ternovoi, V.A.; Kurzhukov, G.P.; Sokolov, Y.V.; Ivanov, G.Y.; Ivanisenko, V.A.; Loktev, A.V.; Ryder, R.W.; Netesov, S.V.; Loktev, V.B. Tick-Borne Encephalitis with Hemorrhagic Syndrome, Novosibirsk Region, Russia, 1999. Emerg. Infect. Dis. J. 2003, 9, 743. [Google Scholar] [CrossRef]
- Shestopalova, N.M.; Reingold, V.N.; Gavrilovskaya, I.N.; Belyaeva, A.P.; Chumakov, M.P. Electron Microscope Studies into the Morphology and Localization of Omsk Hemorrhagic Fever Virus in Infected Tissue Culture Cells. Vopr. Virus. 1965, 4, 425–430. [Google Scholar]
- Tikhomirova, T.; Reingold, V.; Rubin, S.; Gavrilovskaya, I.; Shestopalova, N. Electron-Microscopic Study of the Virion Structure in B Group Arboviruses by the Negative Staining Method. Vopr. Virus 1971, 2, 92–93. [Google Scholar]
- Clarke, D.H. Further Studies on Antigenic Relationships among the Viruses of the Group B Tick-Borne Complex. Bull. World Health Organ. 1964, 31, 45–56. [Google Scholar]
- Gritsun, T.S.; Venugopal, K.; de A Zanotto, P.M.; Mikhailov, M.V.; Sall, A.A.; Holmes, E.C.; Polkinghorne, I.; Frolova, T.V.; Pogodina, V.V.; Lashkevich, V.A.; et al. Complete Sequence of Two Tick-Borne Flaviviruses Isolated from Siberia and the UK: Analysis and Significance of the 5′ and 3′-UTRs. Virus Res. 1997, 49, 27–39. [Google Scholar] [CrossRef]
- Kornilova, K.; Gagarina, A.; Chumakov, M. Comparative characteristics of Omsk hemorrhagic fever virus strains isolated from different objects of a natural focus. Vopr. Virusol. 1970, 15, 232–236. [Google Scholar]
- Lvov, D.K.; Shchelkanov, M.Y.; Alkhovsky, S.V.; Deryabin, P.G. Single-Stranded RNA Viruses. In Zoonotic Viruses in Northern Eurasia; Elsevier: Amsterdam, The Netherlands, 2015; pp. 135–392. ISBN 978-0-12-801742-5. [Google Scholar]
- Chumakov, M. Results of the study made of omsk hemorrhagic fever by an expedition of the institute of neurology. Vestn. Akad. Med. Nauk. SSSR 1948, 2, 19–28. [Google Scholar]
- Földvári, G.; Široký, P.; Szekeres, S.; Majoros, G.; Sprong, H. Dermacentor Reticulatus: A Vector on the Rise. Parasites Vectors 2016, 9, 1–29. [Google Scholar] [CrossRef] [Green Version]
- Rubel, F.; Brugger, K.; Belova, O.A.; Kholodilov, I.S.; Didyk, Y.M.; Kurzrock, L.; García-Pérez, A.L.; Kahl, O. Vectors of Disease at the Northern Distribution Limit of the Genus Dermacentor in Eurasia: D. Reticulatus and D. Silvarum. Exp. Appl. Acarol. 2020, 82, 95–123. [Google Scholar] [CrossRef]
- Gagarina, A.V.; Netsky, G.I. Data on Distribution and Vectors of Hemorrhagic Fever in Western Siberia. In Prirod Ochag Bolezn Chelovek Krayev Epidemiol; Naval Medical Research Unit No3 Cairo (Egypt) Dept of Medical Zoology; State Publishing House of Medical Literature: Moscow, Russia, 1955. [Google Scholar]
- Gagarina, A. The spontaneous carriage of Omsk hemorrhagic fever virus by Dermacentor marginatus Sulz. ticks. Proc. OmGMI 1957, 4, 15–21. [Google Scholar]
- Kharitonova, N.N.; Leonov, Y.A. Omsk Hemorrhagic Fever. Ecology of the Agent and Epizootiology. In Omsk Hemorrhagic Fever. Ecology of the Agent and Epizootiology; Oxonian Press PVT Ltd.: Delhi, India, 1986. [Google Scholar]
- Kondrashova, Z.N. A study of the survival of the virus of Omsk hemorrhagic fever in Ixodes persulcatus in conditions of their massive infection. Med. Parazitol. 1970, 39, 274–278. [Google Scholar]
- GBIF-the Global Biodiversity Information Facility. Available online: https://www.gbif.org/species/5219858 (accessed on 13 January 2022).
- Worldometer-Population Kazakhstan. Available online: https://www.worldometers.info/world-population/kazakhstan-population/ (accessed on 15 January 2022).
- Atshabar, B.; Burdelov, L.A.; Ageyev, V.S.; Aubakirov, S.A.; Dubyanskiy, V.M.; Grazhadanov, A.K.; Zhumadilova, Z.B.; Isbanova, U.A.; Kuznetsov, A.N.; Kunitsa, T.N.; et al. Atlas of Bacterial and Virus Zoonotic Infections Distribution in Kazakhstan; ISTC: Astana, Kazakhstan, 2010; ISBN 9965-15-876-2. [Google Scholar]
- Peintner, L.; Wagner, E.; Shin, A.; Tukhanova, N.; Turebekov, N.; Abdiyeva, K.; Spaiser, O.; Serebrennikova, Y.; Tintrup, E.; Dmitrovskiy, A.; et al. Eight Years of Collaboration on Biosafety and Biosecurity Issues Between Kazakhstan and Germany as Part of the German Biosecurity Programme and the G7 Global Partnership Against the Spread of Weapons and Materials of Mass Destruction. Front. Public Health 2021, 9, 649393. [Google Scholar] [CrossRef]
- Perfilyeva, Y.V.; Shapiyeva, Z.Z.; Ostapchuk, Y.O.; Berdygulova, Z.A.; Bissenbay, A.O.; Kulemin, M.V.; Ismagulova, G.A.; Skiba, Y.A.; Sayakova, Z.Z.; Mamadaliyev, S.M.; et al. Tick-Borne Pathogens and Their Vectors in Kazakhstan—A Review. Ticks Tick-Borne Dis. 2020, 11, 101498. [Google Scholar] [CrossRef]
- Rathore, A.P.S.; St John, A.L. Cross-Reactive Immunity Among Flaviviruses. Front. Immunol. 2020, 11, 334. [Google Scholar] [CrossRef] [Green Version]
- Shin, A.; Tukhanova, N.; Ndenkeh, J., Jr.; Shapieva, Z.; Yegemberdiyeva, R.; Yeraliyeva, L.; Nurmakhanov, T.; Froeschl, G.; Hoelscher, M.; Musralina, L.; et al. Tick-Borne Encephalitis Virus (TBEV) and West-Nile Fever Virus (WNFV) as Causes of Serous Meningitis of Unknown Origin in Kazakhstan. Zoonoses Public Health 2022, 1–12. [Google Scholar] [CrossRef]
- Abdiyeva, K.; Turebekov, N.; Yegemberdiyeva, R.; Dmitrovskiy, A.; Yeraliyeva, L.; Shapiyeva, Z.; Nurmakhanov, T.; Sansyzbayev, Y.; Froeschl, G.; Hoelscher, M.; et al. Vectors, Molecular Epidemiology and Phylogeny of TBEV in Kazakhstan and Central Asia. Parasites Vectors 2020, 13, 504. [Google Scholar] [CrossRef]
- Pomerantzev, B.I. Ixodid Ticks [Ixodidae] (Fauna of the USSR.Arachnida); American Institute of Biological Sciences: Washington, DC, USA, 1959. [Google Scholar]
- Fedorova, S.J. Key Identification of Ixodidae at Kirghizstan. Issled. Zhivoy Prrody Khirghizstana 2013, 1, 47–54. [Google Scholar]
- Philippova, N.A. Ixodid ticks. Ixodinae. In Fauna SSSR Fauna of the USSR. Arachnids, 3rd ed.; Nauka: Moscow, Russia, 1977. [Google Scholar]
- Abdiyeva, K.; Turebekov, N.; Dmitrovsky, A.; Tukhanova, N.; Shin, A.; Yeraliyeva, L.; Heinrich, N.; Hoelscher, M.; Yegemberdiyeva, R.; Shapiyeva, Z.; et al. Seroepidemiological and Molecular Investigations of Infections with Crimean-Congo Haemorrhagic Fever Virus in Kazakhstan. Int. J. Infect. Dis. 2019, 78, 121–127. [Google Scholar] [CrossRef] [Green Version]
- Gu, W.; Unnasch, T.R.; Katholi, C.R.; Lampman, R.; Novak, R.J. Fundamental Issues in Mosquito Surveillance for Arboviral Transmission. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 817–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hijmans, R.J.; Guarino, L.; Cruz, M.; Rojas, E. Computer Tools for Spatial Analysis of Plant Genetic Resources Data: 1. DIVA-GIS. In Plant Genetic Resources Newsletter; Bioversity International: Rome, Italy, 2001; pp. 15–19. [Google Scholar]
- Turebekov, N.; Abdiyeva, K.; Yegemberdiyeva, R.; Dmitrovsky, A.; Yeraliyeva, L.; Shapiyeva, Z.; Amirbekov, A.; Oradova, A.; Kachiyeva, Z.; Ziyadina, L.; et al. Prevalence of Rickettsia Species in Ticks Including Identification of Unknown Species in Two Regions in Kazakhstan. Parasites Vectors 2019, 12, 197. [Google Scholar] [CrossRef] [PubMed]
- Neronov, V.M.; Khlyap, L.A.; Bobrov, V.V.; Warshavsky, A.A. Alien Species of Mammals and Their Impact on Natural Ecosystems in the Biosphere Reserves of Russia. Integr. Zool. 2008, 3, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Avakyan, A.; Lebedov, A.; Ravdonikas, O.; Chumakov, M. On the Question of Importance of Mammals in Forming Natural Reservoirs of Omsk Hemorrhagic Fever. Zool. Zhurnal 1955, 34, 605–609. [Google Scholar]
- Kovalev, S.Y.; Mazurina, E.A. Omsk Hemorrhagic Fever Virus Is a Tick-borne Encephalitis Virus Adapted to Muskrat through Host-jumping. J. Med. Virol. 2022, jmv.27581. [Google Scholar] [CrossRef]
- Shestopalova, N.M.; Reingold, V.N.; Gagarina, A.V.; Kornilova, E.A.; Popov, G.V.; Chumakov, M.P. Electron Microscopic Study of the Central Nervous System in Mice Infected by Omsk Hemorrhagic Fever (OHF) Virus. Virus Reproduction in Cerebellum Neurons. J. Ultrastruct. Res. 1972, 40, 458–469. [Google Scholar] [CrossRef]
- Reed, K.D.; Meece, J.K.; Henkel, J.S.; Shukla, S.K. Birds, Migration and Emerging Zoonoses: West Nile Virus, Lyme Disease, Influenza A and Enteropathogens. Clin. Med. Res. 2003, 1, 5–12. [Google Scholar] [CrossRef] [Green Version]
- Tang, K.; Li, Z.; Li, W.; Chen, L. China’s Silk Road and Global Health. Lancet 2017, 390, 2595–2601. [Google Scholar] [CrossRef]
- Mandl, C.W.; Holbrook, M.R. Tick-Borne Encephalitis and Omsk Hemorrhagic Fever—Chapter 77. In Tropical Infectious Diseases: Principles, Pathogens and Practice, 3rd ed.; Guerrant, R.L., Walker, D.H., Weller, P.F., Eds.; W.B. Saunders: Edinburgh, Scotland, 2011; pp. 515–518. ISBN 978-0-7020-3935-5. [Google Scholar]
- Whitehouse, C.A. Crimean–Congo Hemorrhagic Fever. Antivir. Res. 2004, 64, 145–160. [Google Scholar] [CrossRef]
- Tukhanova, N.; Shin, A.; Abdiyeva, K.; Turebekov, N.; Yeraliyeva, L.; Yegemberdiyeva, R.; Shapiyeva, Z.; Froeschl, G.; Hoelscher, M.; Wagner, E.; et al. Serological Investigation of Orthohantaviruses in Patients with Fever of Unknown Origin in Kazakhstan. Zoonoses Public Health 2020, 67, 271–279. [Google Scholar] [CrossRef]
- Turebekov, N.; Abdiyeva, K.; Yegemberdiyeva, R.; Kuznetsov, A.; Dmitrovskiy, A.; Yeraliyeva, L.; Shapiyeva, Z.; Batyrbayeva, D.; Tukhanova, N.; Shin, A.; et al. Occurrence of Anti-Rickettsia Spp. Antibodies in Hospitalized Patients with Undifferentiated Febrile Illness in the Southern Region of Kazakhstan. Am. J. Trop. Med. Hyg. 2021, 104, 2000–2008. [Google Scholar] [CrossRef]
- Girl, P.; Bestehorn-Willmann, M.; Zange, S.; Borde, J.P.; Dobler, G.; von Buttlar, H. Tick-Borne Encephalitis Virus Nonstructural Protein 1 IgG Enzyme-Linked Immunosorbent Assay for Differentiating Infection versus Vaccination Antibody Responses. J. Clin. Microbiol. 2020, 58, e01783-19. [Google Scholar] [CrossRef]
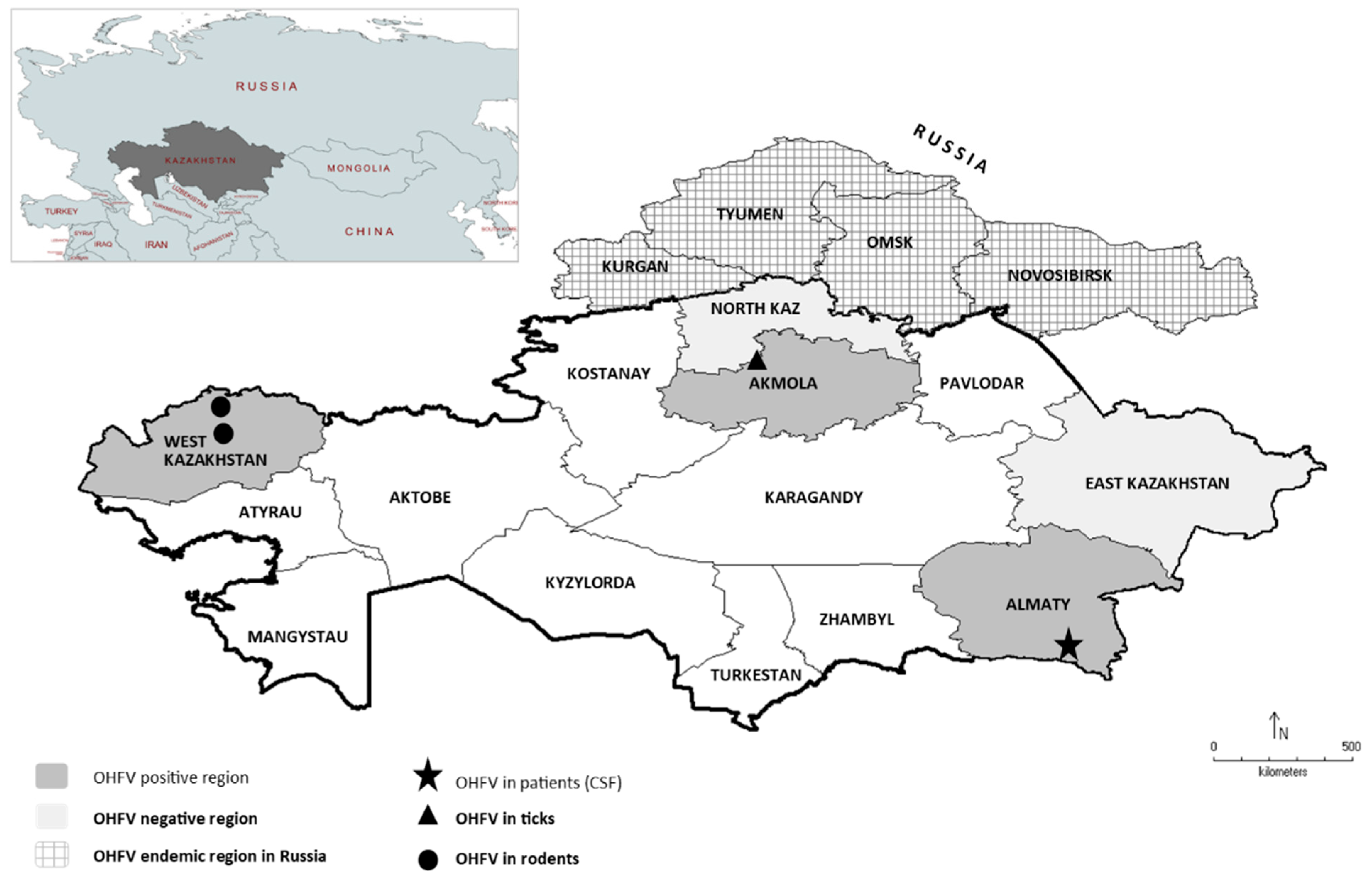
| Region | Year | Collected Species | Positive Species (#Of Pools) |
|---|---|---|---|
| Almaty region | 2018/2019 | 1 | 0 |
| Almaty city | 2018/2019 | 2 | 0 |
| Akmola region | 2016/2018/2019 | 4 | D. marginatus (2), D. reticulatus (6), I. persulcatus (1) |
| North Kazakhstan | 2018/2019 | 4 | 0 |
| Region | Year | Collected Species | Positive Species (#of positive) |
|---|---|---|---|
| Almaty region | 2018/2019 | 6 | 0 |
| Almaty city | 2018/2019 | 7 | 0 |
| West Kazakhstan | 2018/2019 | 6 | A. uralensis (2), M. musculus (2), C. glareolus (3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wagner, E.; Shin, A.; Tukhanova, N.; Turebekov, N.; Nurmakhanov, T.; Sutyagin, V.; Berdibekov, A.; Maikanov, N.; Lezdinsh, I.; Shapiyeva, Z.; et al. First Indications of Omsk Haemorrhagic Fever Virus beyond Russia. Viruses 2022, 14, 754. https://doi.org/10.3390/v14040754
Wagner E, Shin A, Tukhanova N, Turebekov N, Nurmakhanov T, Sutyagin V, Berdibekov A, Maikanov N, Lezdinsh I, Shapiyeva Z, et al. First Indications of Omsk Haemorrhagic Fever Virus beyond Russia. Viruses. 2022; 14(4):754. https://doi.org/10.3390/v14040754
Chicago/Turabian StyleWagner, Edith, Anna Shin, Nur Tukhanova, Nurkeldi Turebekov, Talgat Nurmakhanov, Vitaliy Sutyagin, Almas Berdibekov, Nurbek Maikanov, Ilmars Lezdinsh, Zhanna Shapiyeva, and et al. 2022. "First Indications of Omsk Haemorrhagic Fever Virus beyond Russia" Viruses 14, no. 4: 754. https://doi.org/10.3390/v14040754
APA StyleWagner, E., Shin, A., Tukhanova, N., Turebekov, N., Nurmakhanov, T., Sutyagin, V., Berdibekov, A., Maikanov, N., Lezdinsh, I., Shapiyeva, Z., Shevtsov, A., Freimüller, K., Peintner, L., Ehrhardt, C., & Essbauer, S. (2022). First Indications of Omsk Haemorrhagic Fever Virus beyond Russia. Viruses, 14(4), 754. https://doi.org/10.3390/v14040754






