Epidemiology of Mosquito-Borne Viruses in Egypt: A Systematic Review
Abstract
:1. Introduction
2. Methods
2.1. Data Sources and Search Strategy
2.2. Data Extraction
2.3. Risk of Bias Assessment
3. Results
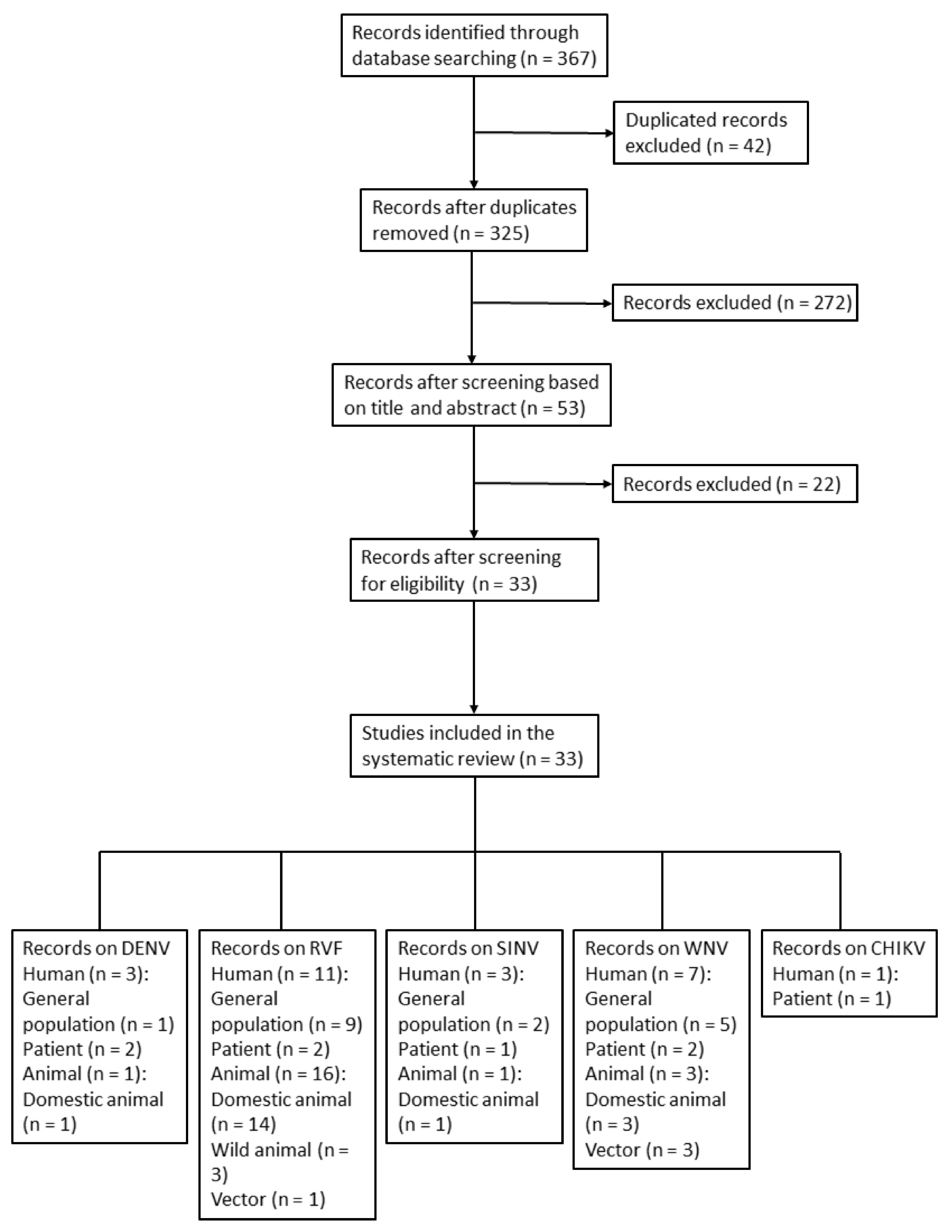
3.1. Search Results
3.2. Risk of Bias Assessment Results
3.3. MBV Prevalence among Humans, Animals, and Vectors in Egypt
3.3.1. DENV
3.3.2. RVFV
3.3.3. WNV
3.3.4. SINV
3.3.5. CHIKV
4. Discussion
4.1. DENV Resurgence and Potential on (Implications for) Continuous Outbreaks
4.2. Seroprevalence Recovery and Frequent Livestock Importation Are the Main Factors for RVFV Resurgence
4.3. Robust WNV Circulating and Extremely High Seroprevalence in Humans
4.4. The SINV Strain, Once Prevalent in Egypt, Was Phylogenetically Close to the Strains Involved in the SINV Outbreak in Northern Europe
4.5. Few of Seroprevalence Studies on CHIKV in Egypt and Severe CHIKV Outbreaks in the Red Sea Region
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.C.; Kuo, R.L.; Shih, S.R. COVID-19: The first documented coronavirus pandemic in history. Biomed. J. 2020, 43, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Ehrenberg, N.; Ehrenberg, J.; Fontes, G.; Gyapong, M.; da Rocha, E.; Steinmann, P.; Utzinger, J.; Zhou, X.-N.; Savigny, D. Neglected tropical diseases as a barometer for progress in health systems in times of COVID-19. BMJ Glob. Health 2021, 6, e004709. [Google Scholar] [CrossRef]
- Moise, I.K.; Ortiz-Whittingham, L.R.; Omachonu, V.; Clark, M.; Xue, R.-D. Fighting mosquito bite during a crisis: Capabilities of Florida mosquito control districts during the COVID-19 pandemic. BMC Public Health 2021, 21, 687. [Google Scholar] [CrossRef]
- Impoinvil, D.E.; Ahmad, S.; Troyo, A.; Keating, J.; Githeko, A.K.; Mbogo, C.M.; Kibe, L.; Githure, J.I.; Gad, A.M.; Hassan, A.N.; et al. Comparison of mosquito control programs in seven urban sites in Africa, the Middle East, and the Americas. Health Policy 2007, 83, 196–212. [Google Scholar] [CrossRef] [Green Version]
- Fawzy, M.; Helmy, Y.A. The one health approach is necessary for the control of Rift Valley fever infections in Egypt: A comprehensive review. Viruses 2019, 11, 139. [Google Scholar] [CrossRef] [Green Version]
- Kenawy, M.A.; Abdel-Hamid, Y.M.; Beier, J.C. Rift Valley fever in Egypt and other African countries: Historical review, recent outbreaks and possibility of disease occurrence in Egypt. Acta Trop. 2018, 181, 40–49. [Google Scholar] [CrossRef]
- Mahmoud, H.; Ali, A.O. Epidemiology and serological detection of Rift Valley fever disease in farm animals in Southern Egypt. Onderstepoort. J. Vet. Res. 2021, 88, e1–e5. [Google Scholar] [CrossRef]
- Mroz, C.; Gwida, M.; El-Ashker, M.; El-Diasty, M.; El-Beskawy, M.; Ziegler, U.; Eiden, M.; Groschup, M.H. Seroprevalence of Rift Valley fever virus in livestock during inter-epidemic period in Egypt, 2014/15. BMC Vet. Res. 2017, 13, 87. [Google Scholar] [CrossRef] [Green Version]
- Mroz, C.; Gwida, M.; El-Ashker, M.; Ziegler, U.; Homeier-Bachmann, T.; Eiden, M.; Groschup, M.H. Rift Valley fever virus infections in Egyptian cattle and their prevention. Transbound. Emerg. Dis. 2017, 64, 2049–2058. [Google Scholar] [CrossRef]
- Ahmed, A.; Ali, Y.; Elduma, A.; Eldigail, M.H.; Mhmoud, R.A.; Mohamed, N.S.; Ksiazek, T.G.; Dietrich, I.; Weaver, S.C. Unique outbreak of Rift Valley fever in Sudan, 2019. Emerg. Infect. Dis. 2020, 26, 3030–3033. [Google Scholar] [CrossRef]
- Sang, R.; Kioko, E.; Lutomiah, J.; Warigia, M.; Ochieng, C.; O’Guinn, M.; Lee, J.S.; Koka, H.; Godsey, M.; Hoel, D.; et al. Rift Valley fever virus epidemic in Kenya, 2006/2007: The entomologic investigations. Am. J. Trop. Med. Hyg. 2010, 83, 28–37. [Google Scholar] [CrossRef] [Green Version]
- Nathan, M.B.; Dayal-Drager, R.; Guzman, M. Epidemiology, burden of disease and transmission. In Dengue Guidelines for Diagnosis, Treatment, Prevention and Control, 1st ed.; WHO & TDR, Ed.; World Health Organization: Geneva, Switzerland, 2009; pp. 3–17. [Google Scholar]
- Wakil, A.W.; Hilmy, F. The Dengue epidemic of 1937 in Cairo. J. Egypt. Med. Assoc. 1938, 21, 716–737. [Google Scholar]
- Khater, E. Insect vector ecology and control in Egypt: History, current status, challenges and future perspectives—A short report. SOVE Newsl. 2021, 53, 7–8. [Google Scholar]
- Burdino, E.; Milia, M.G.; Sergi, G.; Gregori, G.; Allice, T.; Cazzato, M.L.; Lucchini, A.; Lipani, F.; Calleri, G.; Orofino, G.; et al. Diagnosis of dengue fever in North West Italy in travelers from endemic areas: A retrospective study. J. Clin. Virol. 2011, 51, 259–263. [Google Scholar] [CrossRef]
- Ibrahim, H.M.; Khalil, M.; Elsawy, M.; Ismail, M.S.; Alfishawy, M. 1682. Dengue fever outbreak investigation in Upper Egypt in 2015. Open Forum Infect. Dis. 2019, 6, S616. [Google Scholar] [CrossRef]
- World Health Organization. Dengue Fever–Egypt 2015. Available online: http://www.who.int/csr/don/12-november2015-dengue/en/ (accessed on 28 May 2022).
- Saifullin, M.A.; Laritchev, V.P.; Grigorieva, Y.E.; Zvereva, N.N.; Domkina, A.M.; Saifullin, R.F.; Bazarova, M.V.; Akinshina, Y.A.; Karan, L.S.; Butenko, A.M. Two cases of dengue fever imported from Egypt to Russia, 2017. Emerg. Infect. Dis. 2018, 24, 813–814. [Google Scholar] [CrossRef]
- Abozeid, S.; Elsayed, A.K.; Schaffner, F.; Samy, A.M. Re-emergence of Aedes aegypti in Egypt. Lancet Infect. Dis. 2018, 18, 142–143. [Google Scholar] [CrossRef] [Green Version]
- Buliva, E.; Elhakim, M.; Tran Minh, N.N.; Elkholy, A.; Mala, P.; Abubakar, A.; Malik, S.M.M.R. Emerging and reemerging diseases in the World Health Organization (WHO) Eastern Mediterranean Region—Progress, challenges, and WHO initiatives. Front. Public Health 2017, 5, 276. [Google Scholar] [CrossRef]
- Humphrey, J.M.; Cleton, N.B.; Reusken, C.B.; Glesby, M.J.; Koopmans, M.P.; Abu-Raddad, L.J. Dengue in the Middle East and North Africa: A systematic review. PLoS Negl. Trop. Dis. 2016, 10, e0005194. [Google Scholar] [CrossRef] [Green Version]
- Darwish, M.A.; Feinsod, F.M.; Scott, R.M.; Ksiazek, T.G.; Botros, B.A.; Farrag, I.H.; el Said, S. Arboviral causes of non-specific fever and myalgia in a fever hospital patient population in Cairo, Egypt. Trans. R Soc. Trop. Med. Hyg. 1987, 81, 1001–1003. [Google Scholar] [CrossRef]
- Kropman, E.; Bakker, L.J.; de Sonnaville, J.J.; Koopmans, M.P.; Raaphorst, J.; Carpay, J.A. West Nile virus poliomyelitis after a holiday in Egypt. Ned. Tijdschr. Geneeskd. 2012, 155, A4333. [Google Scholar]
- Mohammed, Y.S.; Gresiková, M.; Adamyová, K.; Ragib, A.H.e.-D.K. Studies on arboviruses in Egypt. II. Contribution of arboviruses to the aetiology of undiagnosed fever among children. J. Hyg. 1970, 68, 491–495. [Google Scholar] [CrossRef] [Green Version]
- Humphrey, J.M.; Cleton, N.B.; Reusken, C.; Glesby, M.J.; Koopmans, M.P.G.; Abu-Raddad, L.J. Urban Chikungunya in the Middle East and North Africa: A systematic review. PLoS Negl. Trop. Dis. 2017, 11, e0005707. [Google Scholar] [CrossRef] [Green Version]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane handbook for systematic reviews of interventions, 1st ed.; John Wiley & Sons: Oxford, UK, 2008; pp. 51–79. [Google Scholar]
- Hatcher, E.L.; Zhdanov, S.A.; Bao, Y.; Blinkova, O.; Nawrocki, E.P.; Ostapchuck, Y.; Schäffer, A.A.; Brister, J.R. Virus variation resource-Improved response to emergent viral outbreaks. Nucleic Acids Res. 2017, 45, D482–D490. [Google Scholar] [CrossRef]
- Walter, S.D.; Hildreth, S.W.; Beaty, B.J. Estimation of infection rates in population of organisms using pools of variable size. Am. J. Epidemiol. 1980, 112, 124–128. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Darwish, M.A.; Ibrahim, A.H. Prevalence of antibodies to arboviruses in Egypt. Results of a serologic survey among 1113 university students. Am. J. Trop. Med. Hyg. 1975, 24, 981–985. [Google Scholar] [CrossRef]
- Hussen, M.; Sayed, A.; Abushahba, M. Sero-epidemiological study on dengue fever virus in humans and camels at Upper Egypt. Vet. World 2020, 13, 2618–2624. [Google Scholar] [CrossRef] [PubMed]
- Imam, I.Z.; El-Karamany, R.; Darwish, M.A. An epidemic of Rift Valley fever in Egypt. 2. Isolation of the virus from animals. Bull. World Health Organ. 1979, 57, 441–443. [Google Scholar] [PubMed]
- Meegan, J.M. The Rift Valley fever epizootic in Egypt 1977–78. 1. Description of the epizzotic and virological studies. Trans. R Soc. Trop. Med. Hyg. 1979, 73, 618–623. [Google Scholar] [CrossRef]
- Niklasson, B.; Meegan, J.M.; Bengtsson, E. Antibodies to Rift Valley fever virus in Swedish U.N. soldiers in Egypt and the Sinai. Scand. J. Infect. Dis. 1979, 11, 313–314. [Google Scholar] [CrossRef]
- Allam, I.H.; Feinsod, F.M.; Scott, R.M.; Peters, C.J.; Saah, A.J.; Ghaffar, S.A.; el Said, S.; Darwish, M.A. Rift Valley fever surveillance in mobile sheep flocks in the Nile Delta. Am. J. Trop. Med. Hyg. 1986, 35, 1055–1060. [Google Scholar] [CrossRef]
- Botros, B.A.; Ksiazek, T.G.; Morrill, J.C.; Salib, A.W.; Soliman, A.K.; Scott, R.M.; Barakat, A. Rift Valley fever in Egypt 1986. Surveillance of sheep flocks grazing in the northeast Nile Delta. J. Trop. Med. Hyg. 1988, 91, 183–188. [Google Scholar]
- Corwin, A.; Habib, M.; Olson, J.; Scott, D.; Ksiazek, T.; Watts, D.M. The prevalence of arboviral, rickettsial, and Hantaan-like viral antibody among schoolchildren in the Nile River Delta of Egypt. Trans. R Soc. Trop. Med. Hyg. 1992, 86, 677–679. [Google Scholar] [CrossRef]
- Corwin, A.; Habib, M.; Watts, D.; Darwish, M.; Olson, J.; Botros, B.; Hibbs, R.; Kleinosky, M.; Lee, H.W.; Shope, R.; et al. Community-based prevalence profile of arboviral, rickettsial, and Hantaan-like viral antibody in the Nile River Delta of Egypt. Am. J. Trop. Med. Hyg. 1993, 48, 776–783. [Google Scholar] [CrossRef]
- Abu-Elyazeed, R.; el-Sharkawy, S.; Olson, J.; Botros, B.; Soliman, A.; Salib, A.; Cummings, C.; Arthur, R. Prevalence of anti-Rift-Valley-fever IgM antibody in abattoir workers in the Nile delta during the 1993 outbreak in Egypt. Bull. World Health Organ. 1996, 74, 155–158. [Google Scholar]
- Centers for Disease Control & Prevention (CDC). Rift Valley fever-Egypt, 1993. MMWR Morb. Mortal. Wkly. Rep. 1994, 43, 693, 699–700. [Google Scholar]
- Arthur, R.R.; el-Sharkawy, M.S.; Cope, S.E.; Botros, B.A.; Oun, S.; Morrill, J.C.; Shope, R.E.; Hibbs, R.G.; Darwish, M.A.; Imam, I.Z. Recurrence of Rift Valley fever in Egypt. Lancet 1993, 342, 1149–1150. [Google Scholar] [CrossRef]
- Abd el-Rahim, I.H.; Abd el-Hakim, U.; Hussein, M. An epizootic of Rift Valley fever in Egypt in 1997. Rev. Sci Tech. 1999, 18, 741–748. [Google Scholar] [CrossRef] [Green Version]
- Turkistany, A.H.; Mohamed, A.G.; Al-Hamdan, N. Seroprevalence of Rift Valley fever among slaughterhouse personnel in Makkah during Hajj 1419H (1999). J. Fam. Community Med. 2001, 8, 53–57. [Google Scholar]
- El-Esnawy, A.N. Infection by certain arboviruses among workers potentially at risk of infection. J. Egypt. Public Health Assoc. 2001, 76, 169–182. [Google Scholar]
- Youssef, B.Z.; Donia, H.A. The potential role of Rattus rattus in enzootic cycle of Rift Valley Fever in Egypt. 1-Detection of RVF antibodies in R. rattus blood samples by both enzyme linked immuno sorbent assay (ELISA) and immuno-diffusion technique (ID). J. Egypt. Public Health Assoc. 2001, 76, 431–441. [Google Scholar]
- Youssef, B.Z.; Donia, H.A. The potential role of Rattus rattus in enzootic cycle of Rift Valley fever in Egypt 2-application of reverse transcriptase polymerase chain reaction (RT-PCR) in blood samples of Rattus rattus. J. Egypt. Public Health Assoc. 2002, 77, 133–141. [Google Scholar]
- Hanafi, H.A.; Fryauff, D.J.; Saad, M.D.; Soliman, A.K.; Mohareb, E.W.; Medhat, I.; Zayed, A.B.; Szumlas, D.E.; Earhart, K.C. Virus isolations and high population density implicate Culex antennatus (Becker) (Diptera: Culicidae) as a vector of Rift Valley fever virus during an outbreak in the Nile Delta of Egypt. Acta Trop. 2011, 119, 119–124. [Google Scholar] [CrossRef] [Green Version]
- Youssef, B.Z. The potential role of pigs in the enzootic cycle of Rift Valley fever at Alexandria Governorate, Egypt. J. Egypt. Public Health Assoc. 2009, 84, 331–344. [Google Scholar]
- Horton, K.C.; Wasfy, M.; Samaha, H.; Abdel-Rahman, B.; Safwat, S.; Abdel Fadeel, M.; Mohareb, E.; Dueger, E. Serosurvey for zoonotic viral and bacterial pathogens among slaughtered livestock in Egypt. Vector Borne Zoonotic. Dis. 2014, 14, 633–639. [Google Scholar] [CrossRef] [Green Version]
- El Bahgy, H.E.K.; Abdelmegeed, H.K.; Marawan, M.A. Epidemiological surveillance of bovine viral diarrhea and Rift Valley fever infections in camel. Vet. World 2018, 11, 1331–1337. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, J.R.; Elmansoury, H.K. Natural and experimental infection of Egyptian equines with West nile virus. Ann. Trop. Med. Parasitol. 1963, 57, 415–427. [Google Scholar] [CrossRef]
- Schmidt, J.R.; Said, M.I. Isolation solation of West Nile virus from the African bird Argasid, Argas reflexus hermanni, in Egypt. J. Med. Entomol. 1964, 1, 83–86. [Google Scholar] [CrossRef]
- Turell, M.J.; Morrill, J.C.; Rossi, C.A.; Gad, A.M.; Cope, S.E.; Clements, T.L.; Arthur, R.R.; Wasieloski, L.P.; Dohm, D.J.; Nash, D.; et al. Isolation of West nile and Sindbis viruses from mosquitoes collected in the Nile Valley of Egypt during an outbreak of Rift Valley fever. J. Med. Entomol. 2002, 39, 248–250. [Google Scholar] [CrossRef]
- Soliman, A.; Mohareb, E.; Salman, D.; Saad, M.; Salama, S.; Fayez, C.; Hanafi, H.; Medhat, I.; Labib, E.; Rakha, M.; et al. Studies on West nile virus infection in Egypt. J. Infect. Public Health 2010, 3, 54–59. [Google Scholar] [CrossRef] [Green Version]
- Youssef, S.R.; Eissa, D.G.; Abo-Shady, R.A.; Aly Fouad, N.T. Seroprevalence of anti-WNV IgG antibodies and WNV-RNA in Egyptian blood donors. J. Med. Virol. 2017, 89, 1323–1329. [Google Scholar] [CrossRef]
- Selim, A.; Abdelhady, A. The first detection of anti-West Nile virus antibody in domestic ruminants in Egypt. Trop. Anim. Health Prod. 2020, 52, 3147–3151. [Google Scholar] [CrossRef]
- Selim, A.; Radwan, A.; Arnaout, F. Seroprevalence and molecular characterization of West Nile Virus in Egypt. Comp. Immunol. Microbiol. Infect. Dis. 2020, 71, 101473. [Google Scholar] [CrossRef]
- Hoogstraal, H.; Meegan, J.M.; Khalil, G.M.; Adham, F.K. The Rift Valley fever epizootic in Egypt 1977–1978. 2. Ecological and entomological studies. Trans. R Soc. Trop. Med. Hyg. 1979, 73, 624–629. [Google Scholar] [CrossRef]
- Meegan, J.M.; Khalil, G.M.; Hoogstraal, H.; Adham, F.K. Experimental transmission and field isolation studies implicating Culex pipiens as a vector of Rift Valley fever virus in Egypt. Am. J. Trop. Med. Hyg. 1980, 29, 1405–1410. [Google Scholar] [CrossRef]
- Kenawy, M.A.; Beier, J.C.; Zimmerman, J.H.; Said, S.E.; Abbassy, M.M. Host-feeding patterns of the mosquito community (Diptera: Culicidae) in Aswan Governorate, Egypt. J. Med. Entomol. 1987, 24, 35–39. [Google Scholar] [CrossRef]
- Melnick, J.L.; Paul, J.R.; Riordan, J.T.; Barnett, V.H.; Goldblum, N.; Zabin, E. Isolation from human sera in Egypt of a virus apparently identical to West Nile virus. Proc. Soc. Exp. Biol. Med. 1951, 77, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Selim, A.; Megahed, A.; Kandeel, S.; Alouffi, A.; Almutairi, M.M. West Nile virus seroprevalence and associated risk factors among horses in Egypt. Sci. Rep. 2021, 11, 20932. [Google Scholar] [CrossRef] [PubMed]
- Soliman, A.; Salman, D.; Dinsmore, J.; Pietzsch, H.; Refaat, R.; Hacker, C.; Chapman, G.; Graham, R. Isolation of Sindbis and West nile viruses from white storks (Ciconia ciconia) in the Sinai, Egypt. In Proceedings of the Annual Meeting of the American Society for Tropical Medicine and Hygiene, Houston, TX, USA, 29 Ocotber–2 November 2000. Abstract no. 687. [Google Scholar]
- Taylor, R.; Hurbut, H.; Work, T.; Kingston, J.; Frothingham, T. Sindbis virus: A newly recognized arthropod-transmitted virus. Am. J. Trop. Med. Hyg. 1955, 4, 844–862. [Google Scholar] [CrossRef] [PubMed]
- Eldigail, M.H.; Adam, G.K.; Babiker, R.A.; Khalid, F.; Adam, I.A.; Omer, O.H.; Ahmed, M.E.; Birair, S.L.; Haroun, E.M.; AbuAisha, H.; et al. Prevalence of dengue fever virus antibodies and associated risk factors among residents of El-Gadarif state, Sudan. BMC Public Health 2018, 18, 921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, M.H.A.; Warimwe, G.M.; Di Nardo, A.; Lyons, N.A.; Gubbins, S. Systematic literature review of Rift Valley fever virus seroprevalence in livestock, wildlife and humans in Africa from 1968 to 2016. PLoS Negl. Trop. Dis. 2018, 12, e0006627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helmy, Y.A.; El-Adawy, H.; Abdelwhab, E.M. A comprehensive review of common bacterial, parasitic and viral zoonoses at the human-animal interface in Egypt. Pathogens 2017, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Napp, S.; Chevalier, V.; Busquets, N.; Calistri, P.; Casal, J.; Attia, M.; Elbassal, R.; Hosni, H.; Farrag, H.; Hassan, N.; et al. Understanding the legal trade of cattle and camels and the derived risk of Rift Valley fever introduction into and transmission within Egypt. PLoS Negl. Trop. Dis. 2018, 12, e0006143. [Google Scholar] [CrossRef] [Green Version]
- Bird, B.H.; Khristova, M.L.; Rollin, P.E.; Ksiazek, T.G.; Nichol, S.T. Complete genome analysis of 33 ecologically and biologically diverse Rift Valley fever virus strains reveals widespread virus movement and low genetic diversity due to recent common ancestry. J. Virol. 2007, 81, 2805–2816. [Google Scholar] [CrossRef] [Green Version]
- Ikegami, T. Molecular biology and genetic diversity of Rift Valley fever virus. Antivir. Res. 2012, 95, 293–310. [Google Scholar] [CrossRef] [Green Version]
- Botros, B.; Omar, A.; Elian, K.; Mohamed, G.; Soliman, A.; Salib, A.; Salman, D.; Saad, M.; Earhart, K. Adverse response of non-indigenous cattle of European breeds to live attenuated Smithburn Rift Valley fever vaccine. J. Med. Virol. 2006, 78, 787–791. [Google Scholar] [CrossRef]
- Grobbelaar, A.A.; Weyer, J.; Leman, P.A.; Kemp, A.; Paweska, J.T.; Swanepoel, R. Molecular epidemiology of Rift Valley fever virus. Emerg. Infect. Dis. 2011, 17, 2270–2276. [Google Scholar] [CrossRef]
- Bob, N.S.; Bâ, H.; Fall, G.; Ishagh, E.; Diallo, M.Y.; Sow, A.; Sembene, P.M.; Faye, O.; El Kouri, B.; Sidi, M.L.; et al. Detection of the Northeastern African Rift Valley fever virus lineage during the 2015 outbreak in Mauritania. Open Forum Infect. Dis. 2017, 4, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Turell, M.J.; Presley, S.M.; Gad, A.M.; Cope, S.E.; Dohm, D.J.; Morrill, J.C.; Arthur, R.R. Vector competence of Egyptian mosquitoes for Rift Valley fever virus. Am. J. Trop. Med. Hyg. 1996, 54, 136–139. [Google Scholar] [CrossRef]
- Gad, A.M.; Farid, H.A.; Ramzy, R.R.; Riad, M.B.; Presley, S.M.; Cope, S.E.; Hassan, M.M.; Hassan, A.N. Host feeding of mosquitoes (Diptera: Culicidae) associated with the recurrence of Rift Valley fever in Egypt. J. Med. Entomol 1999, 36, 709–714. [Google Scholar] [CrossRef]
- Turell, M.J.; Linthicum, K.J.; Patrican, L.A.; Davies, F.G.; Kairo, A.; Bailey, C.L. Vector competence of selected African mosquito (Diptera: Culicidae) species for Rift Valley fever virus. J. Med. Entomol. 2008, 45, 102–108. [Google Scholar] [CrossRef]
- Seufi, A.M.; Galal, F.H. Role of Culex and Anopheles mosquito species as potential vectors of Rift Valley fever virus in Sudan outbreak, 2007. BMC Infect. Dis. 2010, 10, 65. [Google Scholar] [CrossRef] [Green Version]
- Mansfield, K.L.; Banyard, A.C.; McElhinney, L.; Johnson, N.; Horton, D.L.; Hernández-Triana, L.M.; Fooks, A.R. Rift Valley fever virus: A review of diagnosis and vaccination, and implications for emergence in Europe. Vaccine 2015, 33, 5520–5531. [Google Scholar] [CrossRef] [Green Version]
- Ahmed Kamal, S. Observations on Rift Valley fever virus and vaccines in Egypt. Virol. J. 2011, 8, 532. [Google Scholar] [CrossRef] [Green Version]
- Kamal, S.A. Pathological studies on postvaccinal reactions of Rift Valley fever in goats. Virol. J. 2009, 6, 94. [Google Scholar] [CrossRef] [Green Version]
- Himeidan, Y.E.; Kweka, E.J.; Mahgoub, M.M.; El Rayah, E.A.; Ouma, J.O. Recent outbreaks of Rift Valley fever in East Africa and the Middle East. Front. Public Health 2014, 2, 169. [Google Scholar] [CrossRef] [Green Version]
- Malkinson, M.; Banet, C. The role of birds in the ecology of West nile virus in Europe and Africa. Curr. Top. Microbiol. Immunol. 2002, 267, 309–322. [Google Scholar]
- Rappole, J.H.; Derrickson, S.R.; Hubalek, Z. Migratory birds and spread of West Nile virus in the Western Hemisphere. Emerg Infect. Dis. 2000, 6, 319–328. [Google Scholar] [CrossRef]
- Gabriel, M.; Emmerich, P.; Frank, C.; Fiedler, M.; Rashidi-Alavijeh, J.; Jochum, C.; Günther, S.; Auerhammer, K.; Rupprecht, H.J.; Blank, R.T.; et al. Increase in West Nile virus infections imported to Germany in 2012. J. Clin. Virol. 2013, 58, 587–589. [Google Scholar] [CrossRef]
- Lanciotti, R.S.; Ebel, G.D.; Deubel, V.; Kerst, A.J.; Murri, S.; Meyer, R.; Bowen, M.; McKinney, N.; Morrill, W.E.; Crabtree, M.B.; et al. Complete genome sequences and phylogenetic analysis of West Nile virus strains isolated from the United States, Europe, and the Middle East. Virology 2002, 298, 96–105. [Google Scholar] [CrossRef] [Green Version]
- Chancey, C.; Grinev, A.; Volkova, E.; Rios, M. The global ecology and epidemiology of West nile virus. Biomed. Res. Int. 2015, 2015, 376230. [Google Scholar] [CrossRef] [Green Version]
- Li, X.L.; Fu, S.H.; Liu, W.B.; Wang, H.Y.; Lu, Z.; Tong, S.X.; Li, Z.X.; Nasci, R.S.; Kosoy, O.; Cui, Y.; et al. West nile virus infection in Xinjiang, China. Vector Borne Zoonotic. Dis. 2013, 13, 131–133. [Google Scholar] [CrossRef]
- Adouchief, S.; Smura, T.; Sane, J.; Vapalahti, O.; Kurkela, S. Sindbis virus as a human pathogen-epidemiology, clinical picture and pathogenesis. Rev. Med. Virol. 2016, 26, 221–241. [Google Scholar] [CrossRef]
- Kurkela, S.; Manni, T.; Vaheri, A.; Vapalahti, O. Causative agent of Pogosta disease isolated from blood and skin lesions. Emerg. Infect. Dis. 2004, 10, 889–894. [Google Scholar] [CrossRef]
- Ziegler, U.; Fischer, D.; Eiden, M.; Reuschel, M.; Rinder, M.; Müller, K.; Schwehn, R.; Schmidt, V.; Groschup, M.H.; Keller, M. Sindbis virus–a wild bird associated zoonotic arbovirus circulates in Germany. Vet. Mikrobiyol. 2019, 239, 108453. [Google Scholar] [CrossRef]
- Kurkela, S.; Manni, T.; Myllynen, J.; Vaheri, A.; Vapalahti, O. Clinical and laboratory manifestations of Sindbis virus infection: Prospective study, Finland, 2002–2003. J. Infect. Dis. 2005, 191, 1820–1829. [Google Scholar] [CrossRef]
- Sigei, F.; Nindo, F.; Mukunzi, S.; Ng’ang’a, Z.; Sang, R. Evolutionary analyses of Sindbis virus strains isolated from mosquitoes in Kenya. Arch. Virol. 2018, 163, 2465–2469. [Google Scholar] [CrossRef] [PubMed]
- Storm, N.; Weyer, J.; Markotter, W.; Kemp, A.; Leman, P.A.; Dermaux-Msimang, V.; Nel, L.H.; Paweska, J.T. Human cases of Sindbis fever in South Africa, 2006–2010. Epidemiol. Infect. 2014, 142, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Volk, S.M.; Chen, R.; Tsetsarkin, K.A.; Adams, A.P.; Garcia, T.I.; Sall, A.A.; Nasar, F.; Schuh, A.J.; Holmes, E.C.; Higgs, S.; et al. Genome-scale phylogenetic analyses of Chikungunya virus reveal independent emergences of recent epidemics and various evolutionary rates. J. Virol. 2010, 84, 6497–6504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andayi, F.; Charrel, R.N.; Kieffer, A.; Richet, H.; Pastorino, B.; Leparc-Goffart, I.; Ahmed, A.A.; Carrat, F.; Flahault, A.; de Lamballerie, X. A sero-epidemiological study of arboviral fevers in Djibouti, Horn of Africa. PLoS Negl. Trop. Dis. 2014, 8, e3299. [Google Scholar] [CrossRef] [Green Version]
- Bower, H.; El Karsany, M.; Adam, A.; Idriss, M.I.; Alzain, M.A.; Alfakiyousif, M.E.A.; Mohamed, R.; Mahmoud, I.; Albadri, O.; Mahmoud, S.A.A.; et al. “Kankasha” in Kassala: A prospective observational cohort study of the clinical characteristics, epidemiology, genetic origin, and chronic impact of the 2018 epidemic of Chikungunya virus infection in Kassala, Sudan. PLoS Negl. Trop. Dis. 2021, 15, e0009387. [Google Scholar] [CrossRef]
- Ciccozzi, M.; Lo Presti, A.; Cella, E.; Giovanetti, M.; Lai, A.; El-Sawaf, G.; Faggioni, G.; Vescio, F.; Al Ameri, R.; De Santis, R.; et al. Phylogeny of dengue and Chikungunya viruses in Al Hudayda Governorate, Yemen. Infect. Genet. Evol. 2014, 27, 395–401. [Google Scholar] [CrossRef]
- Dash, P.K.; Parida, M.M.; Santhosh, S.R.; Verma, S.K.; Tripathi, N.K.; Ambuj, S.; Saxena, P.; Gupta, N.; Chaudhary, M.; Babu, J.P.; et al. East Central South African genotype as the causative agent in reemergence of Chikungunya outbreak in India. Vector Borne Zoonotic. Dis. 2007, 7, 519–528. [Google Scholar] [CrossRef]
- Gould, L.H.; Osman, M.S.; Farnon, E.C.; Griffith, K.S.; Godsey, M.S.; Karch, S.; Mulenda, B.; El Kholy, A.; Grandesso, F.; de Radiguès, X.; et al. An outbreak of Yellow fever with concurrent Chikungunya virus transmission in South Kordofan, Sudan, 2005. Trans. R Soc. Trop. Med. Hyg. 2008, 102, 1247–1254. [Google Scholar] [CrossRef]
- Njenga, M.; Nderitu, L.; Ledermann, J.; Ndirangu, A.; Logue, C.; Kelly, C.; Sang, R.; Sergon, K.; Breiman, R.; Powers, A. Tracking epidemic Chikungunya virus into the Indian Ocean from East Africa. J. Gen. Virol. 2008, 89, 2754–2760. [Google Scholar] [CrossRef]
- Pastorino, B.; Muyembe-Tamfum, J.J.; Bessaud, M.; Tock, F.; Tolou, H.; Durand, J.P.; Peyrefitte, C.N. Epidemic resurgence of Chikungunya virus in democratic Republic of the Congo: Identification of a new central African strain. J. Med. Virol. 2004, 74, 277–282. [Google Scholar] [CrossRef]
- Peyrefitte, C.N.; Bessaud, M.; Pastorino, B.A.; Gravier, P.; Plumet, S.; Merle, O.L.; Moltini, I.; Coppin, E.; Tock, F.; Daries, W.; et al. Circulation of Chikungunya virus in Gabon, 2006–2007. J. Med. Virol. 2008, 80, 430–433. [Google Scholar] [CrossRef]
- Zayed, A.; Awash, A.A.; Esmail, M.A.; Al-Mohamadi, H.A.; Al-Salwai, M.; Al-Jasari, A.; Medhat, I.; Morales-Betoulle, M.E.; Mnzava, A. Detection of Chikungunya virus in Aedes aegypti during 2011 outbreak in Al Hodayda, Yemen. Acta Trop. 2012, 123, 62–66. [Google Scholar] [CrossRef]
- Rossi, G.; Karki, S.; Smith, R.L.; Brown, W.M.; Ruiz, M.O.H. The spread of mosquito-borne viruses in modern times: A spatio-temporal analysis of Dengue and Chikungunya. Spat. Spatiotemp. Epidemiol. 2018, 26, 113–125. [Google Scholar] [CrossRef] [Green Version]

| Virus | Year, Ref. | Region/City/ Governorate | Species | Sample Size | Participants Characteristics | Assay | Elisa (IgG) | VI | NT | IF | HAI | CF | RT-PCR | AGPT | Remarks | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male/ Female | Age Range | Male/ Female | Age Range | |||||||||||||||
| DENV | 1968, [26] | Alexandria | Human | 120 | 60 60 | 3–13 | CF HAI | 0.00 | 0.00 | Acute blood samples from children | ||||||||
| 1969, [33] | Throughout Egypt | Human | 1113 | 1113 (male) | HAI | 0.30 | University students Abstract | |||||||||||
| 2019, [34] | Upper Egypt (Sohag and Assiut) | Human | 91 | 57 34 | 8 (<21) 53 (21–40) 30 (>40) | 14.03 8.82 | 25.00 11.32 10.00 | 70 individuals with breakbone fever | ||||||||||
| Camel | 91 | 76 15 | 2.63 6.67 | |||||||||||||||
| RVFV | 1977, [35] | Qalyoubiya Sharqiya Giza Menia Aswan Sohag Cairo | Sheep Cow Camel Goat Horse Rat | 58 17 30 9 18 8 | VI | 46.55 5.88 3.33 11.11 5.56 12.50 | Sera or tissue from sick feverish and died herds | |||||||||||
| 1977, [36] | Qalyoubiya Sharqiya Giza | Human | 91 | VI | 59.34 | Acute febrile and/or fatal haemorrhagic | ||||||||||||
| Sharqiya | Sheep | 4 | VI | 50.00 | Aborting sheep | |||||||||||||
| 1977–1978, [37] | Sinai Peninsula | Human | 170 | HAI | 4.71 | Abstract Swedish soldiers serving in Egypt | ||||||||||||
| 1984, [38] | Nile Delta | Sheep | 406 | HAI NT | 5.91 | 5.91 | Abstract | |||||||||||
| 1984, [24] | Giza (from Cairo or surrounding areas) | Human | 55 | VI HAI | 0.00 | 0.00 (IgM) 1.82 (IgG) | Serum samples of non-specific fever and myalgia patient | |||||||||||
| 1986, [39] | Daqahliya | Sheep | 1714 | ELISA (IgM) HAI NT | 0.00 | 1.17 | 1.17 | Unvaccinated Abstract | ||||||||||
| 1989, [40] | Sharqiya | Human | 223 | 99 124 | 8–14 | ELISA | 3.03 4.03 | School children | ||||||||||
| NA (1993 a), [41] | Nile River Valley | Human | 915 | ELISA | 14.97 | Abstract | ||||||||||||
| 1993, [42] | Behera Beni Suef Cairo Damietta Daqahliya Gharbiya Giza North Sinai Ismailia Kafr El-Sheikh Menoufiya Port Said Qalyoubiya Sharqiya South Sinai | Human | 46 65 100 100 99 100 68 47 100 100 100 99 100 26 31 | ELISA (IgM) | 0.00 0.00 0.00 1.00 2.02 3.00 0.00 0.00 10.00 1.00 2.00 3.03 0.00 7.69 0.00 | Abattoir workers | ||||||||||||
| 1993, [43] | Aswan | Village 1 | Human | ELISA | 11.96 | IgM | ||||||||||||
| Village 2 | 8.36 | |||||||||||||||||
| 1993, [44] | Aswan | Sheep Goat Cow Buffalo | 22 7 8 1 | IF | 36.36 28.57 50.00 100.00 | |||||||||||||
| 1997, [45] | Aswan and Assiut | Sheep Cattle | 57 93 | NT, IF, CF, AGPT | 100.00 100.00 | 100.00 100.00 | 100.00 100.00 | 84.21 74.19 | Aborted sheep fetuses and sera from affected herds | |||||||||
| 1999, [46] | Egypt | Human | 52 | ELISA | 21.15 | Slaughter house personnel in Makkah during Hajj 1419 (1999) | ||||||||||||
| 1999, [47] | NA | Human | 264 | ELISA | 7.95 | Worker of sewage treatment plants Abstract | ||||||||||||
| NA (2001 a), [48,49] | Behera Alexandria Menia | Rat | ELISA, IF, RT-PCT | 29.33 | 6.00 | 9.67 | Abstract | |||||||||||
| 2003, [50] | Aswan, Beni Suef, Behera, Cairo, Daqahliya, Kafr El-Sheikh, Qalyoubiya, Qena, and Sharqiya | Human | 375 | VI, RT-PCR | 4.00 | 5.06 | Sera or cerebrospinal fluid from suspected cases of RVF | |||||||||||
| Kafr El-Sheikh | Cow Sheep Goat Buffalo | 48 36 9 8 | ELISA (IgM) | 10.42 5.55 0.00 0.00 | ||||||||||||||
| Kafr El-Sheikh | Culex antennatus Cx. pipiens Cx. perexiguus Ae. detritus Anopheles tenebrosus An. pharoensis | 8798 (218) 102 (27) 6 (3) 1 (1) 248 (41) 24 (17) | RT-PCR | 1.38 0.00 0.00 0.00 0.00 0.00 | ||||||||||||||
| NA (2009 a), [51] | Alexandria | Pig | 245 | ELISA, HAI | 15.10 | 8.16 | Abstract | |||||||||||
| Human | 43 | ELISA HAI | 13.95 | 6.98 | Veterinarian and their assistants, butchers and abattoir workers | |||||||||||||
| 2009, [52] | Giza (originated from governorates throughout Egypt) | Cattle Buffalo Sheep Camel | 161 153 174 10 | ELISA | 1.24 3.26 0.00 0.00 | |||||||||||||
| 2013–2015, [11] | Nile Delta (Damietta, Port Said, Daqahliya) | Cattle (immunized) | 2743 | 2–7 | ELISA IF NT | 16.00 | 58.25 | 66.84 | Farms | |||||||||
| Nile Delta (Daqahliya, Gharbia, Damietta, Port said) | Cattle (non-immunized) | 1289 | 2–7 | ELISA IF NT | 7.29 | 26.87 | 56.76 | Small holders | ||||||||||
| 2014–2015, [10] | Daqahliya Daqahliya Daqahliya Ismailiya Cairo Red Sea | Sheep (small holder) Goat Buffalo (small holder) Buffalo (farms) Camels (local abattoir) Camels imported from Sudan | 438 26 88 100 71 150 | 2–10 2–3 3–7 4–6 5–7 2–7 | ELISA NT IF | 0.72 0.00 10.26 1.05 100.00 0.00 | 0.00 0.00 3.57 0.00 10.17 0.00 | 3.41 NA 25.00 0.00 2.82 0.00 | Non-vaccinated (born after RVF epidemic in 2003) | |||||||||
| NA (2018 a), [53] | From different herds in Egypt and originated from Sudan | Camel | 200 (120: origin from Sudan 80: local breed) | 70 130 | ≤1 2–5 5–9 ≥9 | ELISA | 21.43 9.23 | 19.23 3.33 13.93 25.71 | ||||||||||
| 2017–2019, [9] | Aswan, Qena and Luxor | Cattle Sheep Goat Camel Donkey | 92 92 92 92 92 | 0.5–3 | ELISA | 5.55 65.21 14.44 20.65 0.00 | Unvaccinated | |||||||||||
| WNV | 1959, [54] | Nile Delta and Upper Egypt | Horse Donkey mule | 102 154 27 | NT | 56.86 35.71 44.44 | ||||||||||||
| 1960, [55] | Kafr El-Sheikh | Argas refiexus hermanni | 1400 | Nymph: 14 pools Adult: 14 | VI HAI CF NT | 7.14 7.14 | 7.14 7.14 | 7.14 7.14 | tick | |||||||||
| 1968, [26] | Alexandria | Human | 120 | 60 60 | 3–13 | CF HAI | 4.00 | 4.00 | Acute blood samples from children | |||||||||
| 1969, [33] | Throughout Egypt | Human | 1113 | 1113 (male) | HAI | 51.21 | University students Abstract | |||||||||||
| 1984, [24] | Giza (from Cairo or surrounding areas) | Human | 55 | VI HAI | 0.00 | 1.82 (IgM) 58.18 (IgG) | Serum samples of non-specific fever and myalgia patient | |||||||||||
| 1989, [40] | Sharqiya | Human | 437 | 215 222 | 8–14 | ELISA | 2.32 4.50 | School children | ||||||||||
| NA (1993 a), [41] | Nile River Valley | Human | 915 | ELISA | 20.00 | Abstract | ||||||||||||
| 1993, [56] | Aswan | An. multicolor An. pharoensis An. tenebrosus Cx. antennatus Cx. perexiguus Cx. pipiens Cx. poicilipes Ochlerotatus caspius Urranotaenia unguiculata | 5 145 245 2691 9011 6982 26 16,889 30 (up to 88/pool) | VI | 0.00 0.00 0.00 1.90 2.60 0.30 0.00 0.00 0.00 0.00 0.00 0.00 | Minimum infection rate | ||||||||||||
| 1999, [47] | NA | Human | 264 | ELISA | 54.14 | Workers of sewage treatment plants, Abstract | ||||||||||||
| 1999–2002, [57] | Upper Egypt (Qena) Middle Egypt (Fayoum) Lower Egypt (Sharqiya) North Sinai South Sinai | Human | 2203 1593 1292 202 675 | ELISA | 35.00 27.31 13.78 0.99 6.67 | |||||||||||||
| Upper Egypt (Qena) Middle Egypt (Fayoum) Lower Egypt (Sharqiya) North Sinai (Al-Areesh), South Sinai (Nuweiba) | Culex (81%) Culex (99%) Aedes (56%) Culex (37%) Culex (97%) Culex (99%) | 880 (216) 9398 (484) 40,937 (1686) 34,770 (1897) 26,170 (731) | RT-PCR | 0.00 0.00 0.18 0.58 0.14 | Cx. pepiens, Cx. perexiguus Cx. perexiguus, Cx. antennatus, Cx. poicilipes, An. pharoensis, sand files Cx. antennatus | |||||||||||||
| 2013–2014, [58] | Throughout Egypt | Human | 160 | ELISA RT-PCR | 55.00 | 0.00 | Blood donors from the blood bank of Ain Shams University Hospitals | |||||||||||
| 2018–2019, [59] | Qalyoubiya, Menoufiya, Kafr El-Sheikh, Gharbiya | Cattle Buffalo Camel Sheep Goats | 100 50 50 85 75 | ELISA | 18.00 0.00 40.00 3.53 5.33 | |||||||||||||
| 2019, [60] | Qalyoubiya Menoufia Kafr El-Sheikh Gharbiya | Horse | 90 120 160 130 | ELISA RT-PCR | 25.56 17.50 21.25 14.62 | 0.00 0.00 0.63 0.00 | ||||||||||||
| Kafr El-Sheikh Gharbiya | Cx. spp. | 5 pools | RT-PCR | 20.00 | ||||||||||||||
| SINV | 1968, [26] | Alexandria | Human | 120 | 60 60 | 3–13 | CF HAI | 4.00 | 4.00 | Acute blood samples from children | ||||||||
| 1969, [33] | Throughout Egypt | Human | 1113 | 1113 (male) | HAI | 6.47 | University students Abstract | |||||||||||
| 1993, [56] | Aswan | An. multicolor An. pharoensis An. tenebrosus Cx. antennatus Cx. perexiguus Cx. pipiens Cx. poicilipes Oc. (=Aedes) caspius Ur. unguiculata | 5 145 245 2691 9011 6982 26 16,889 30 (up to 88/pool) | VI | 0.00 0.00 0.00 0.00 0.30 0.00 0.00 0.00 0.00 0.00 0.00 0.00 | |||||||||||||
| 1999, [47] | NA | Human | 264 | ELISA | 1.13 | Workers of sewage treatment plants Abstract | ||||||||||||
| CHIKV | 1984, [24] | Giza (from Cairo or surrounding areas) | Human | 55 | VI HAI | 0.00 | 0.00 (IgM) 5.45 (IgG) | Serum samples of non-specific fever and myalgia patient | ||||||||||
| Virus | Author, Year | Region/City/Governorate | Species | Sampling Approach | Risk of Bias Assessment | Precision | Ref. | |
|---|---|---|---|---|---|---|---|---|
| Sampling | Assay | |||||||
| DENV | Hussen, 2020 | Upper Egypt (Sohag and Assiut) | Human Camel | MSCS MSCS | Low | High | Low | [34] |
| DENV, SINV, WNV | Mohammed, 1970 | Alexandria | Human | Conv. | High | High | High | [26] |
| DENV, SINV, WNV | Darwish, 1975 | Throughout Egypt | Human | CS | Low | Low | High | [33] |
| RVFV | Mroz, 2017 | Nile Delta | Cattle | MSCS | Low | Low | High | [11] |
| Mroz, 2017 | Throughout Egypt | Different livestock | MSCS | Low | Low | High | [10] | |
| El-Bahgy, 2018 | From different herds in Egypt and originated from Sudan | Camel | MSCS | Low | High | High | [53] | |
| Meegan, 1979 | Qalyoubiya, Sharqiya, Giza | Human | Conv. | High | Low | Low | [36] | |
| Abdel-Rahim, 1999 | Aswan and Assiut | Sheep Cattle | Conv. Conv. | High High | Low Low | Low Low | [45] | |
| Imam, 1979 | Qalyoubiya, Sharqiya, Giza, Menia, Aswan, Sohag, Cairo | Different animals | Conv. | High | Low | High | [35] | |
| Hanafi, 2011 | Aswan, Beni Suef, Behera, Cairo, Daqahliya, Kafr El-Sheikh, Qalyoubiya, Qena, and Sharqiya | Human | Conv. | High | Low | High | [50] | |
| Kafr El-Sheikh | Different livestock | Cluster | Low | High | High | |||
| Kafr El-Sheikh | Mosquito | Cluster | Low | Low | High | |||
| Youssef, 2001 | Behera Alexandria Menia | Rat | Cluster | Low | High | High | [48] | |
| Youssef, 2002 | Behera Alexandria Menia | Rat | Cluster | Low | Low | High | [49] | |
| Niklasson, 1979 | Swedish soldiers serving in Egypt | Human | Cluster | Low | High | High | [37] | |
| Mahmoud, 2021 | Aswan, Qena, and Luxor | Different livestock | Cluster | Low | High | Low | [9] | |
| Horton, 2014 | Giza (originated from governorates throughout Egypt) | Different livestock | Cluster | Low | High | High | [52] | |
| Turkistany, 2001 | Slaughterhouse personnel in Makkah from Egypt | Human | Cluster | Low | High | Low | [46] | |
| Abu-Elyazeed, 1996 | Behera, Beni Suef, Cairo, Damietta, Daqahliya, Gharbiya, Giza, North Sinai, Ismailia, Kafr El-Sheikh, Menoufiya, Port Said, Qalyoubiya, Sharqiya, South Sinai | Human | Cluster | Low | High | High | [42] | |
| Youssef, 2009 | Alexandria | Pig Human | Cluster Cluster | Low Low | High High | High Low | [51] | |
| Allam, 1986 | Nile Delta | Sheep | Cluster | Low | Low | High | [38] | |
| Arthur, 1993 | Aswan | Different livestock | Conv. | High | Low | Low | [44] | |
| Botros, 1988 | Daqahliya | Sheep | Cluster | Low | Low | High | [39] | |
| Centers for Disease Control & Prevention (CDC), 1994 | Aswan | Human | Cluster | Low | High | High | [43] | |
| RVFV, SINV | El-Esnawy, 2001 | NA | Human | Cluster | Low | High | High | [47] |
| RVFV, WNV, CHIKV | Darwish, 1987 | Giza | Human | Conv. | High | Low | Low | [24] |
| RVFV, WNV | Corwin, 1992 | Sharqiya | Human | MSCS | Low | High | High | [40] |
| RVFV, WNV | Corwin, 1993 | Nile River Valley | Human | Random | Low | High | High | [41] |
| SINV, WNV | Turell, 2002 | Aswan | Mosquitoes | Random | Low | Low | High | [56] |
| WNV | Selim, 2020 | Qalyoubiya, Menoufia, Kafr El-Sheikh, Gharbia | Horse | Random | Low | Low | High | [60] |
| Selim, 2020 | Qalyoubiya, Menoufia, Kafr El-Sheikh, Gharbia | Different livestock | Random | Low | High | High | [59] | |
| Soliman, 2010 | Upper Egypt (Qena), Middle Egypt (Fayoum), Lower Egypt (Sharqiya), North Sinai (Al-Areesh), South Sinai (Nuweiba) | Human | Random | Low | High | High | [57] | |
| Youssef, 2017 | Blood donors from the blood bank of Ain Shams University Hospitals | Human | Random | Low | Low | High | [58] | |
| Schmidt, 1964 | Kafr El-Sheikh | Tick | MSCS | High | Low | High | [55] | |
| Schmidt, 1963 | Upper and Lower Egypt | Equine | Random | Low | Low | High | [54] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fang, Y.; Khater, E.I.M.; Xue, J.-B.; Ghallab, E.H.S.; Li, Y.-Y.; Jiang, T.-G.; Li, S.-Z. Epidemiology of Mosquito-Borne Viruses in Egypt: A Systematic Review. Viruses 2022, 14, 1577. https://doi.org/10.3390/v14071577
Fang Y, Khater EIM, Xue J-B, Ghallab EHS, Li Y-Y, Jiang T-G, Li S-Z. Epidemiology of Mosquito-Borne Viruses in Egypt: A Systematic Review. Viruses. 2022; 14(7):1577. https://doi.org/10.3390/v14071577
Chicago/Turabian StyleFang, Yuan, Emad I. M. Khater, Jing-Bo Xue, Enas H. S. Ghallab, Yuan-Yuan Li, Tian-Ge Jiang, and Shi-Zhu Li. 2022. "Epidemiology of Mosquito-Borne Viruses in Egypt: A Systematic Review" Viruses 14, no. 7: 1577. https://doi.org/10.3390/v14071577
APA StyleFang, Y., Khater, E. I. M., Xue, J.-B., Ghallab, E. H. S., Li, Y.-Y., Jiang, T.-G., & Li, S.-Z. (2022). Epidemiology of Mosquito-Borne Viruses in Egypt: A Systematic Review. Viruses, 14(7), 1577. https://doi.org/10.3390/v14071577







