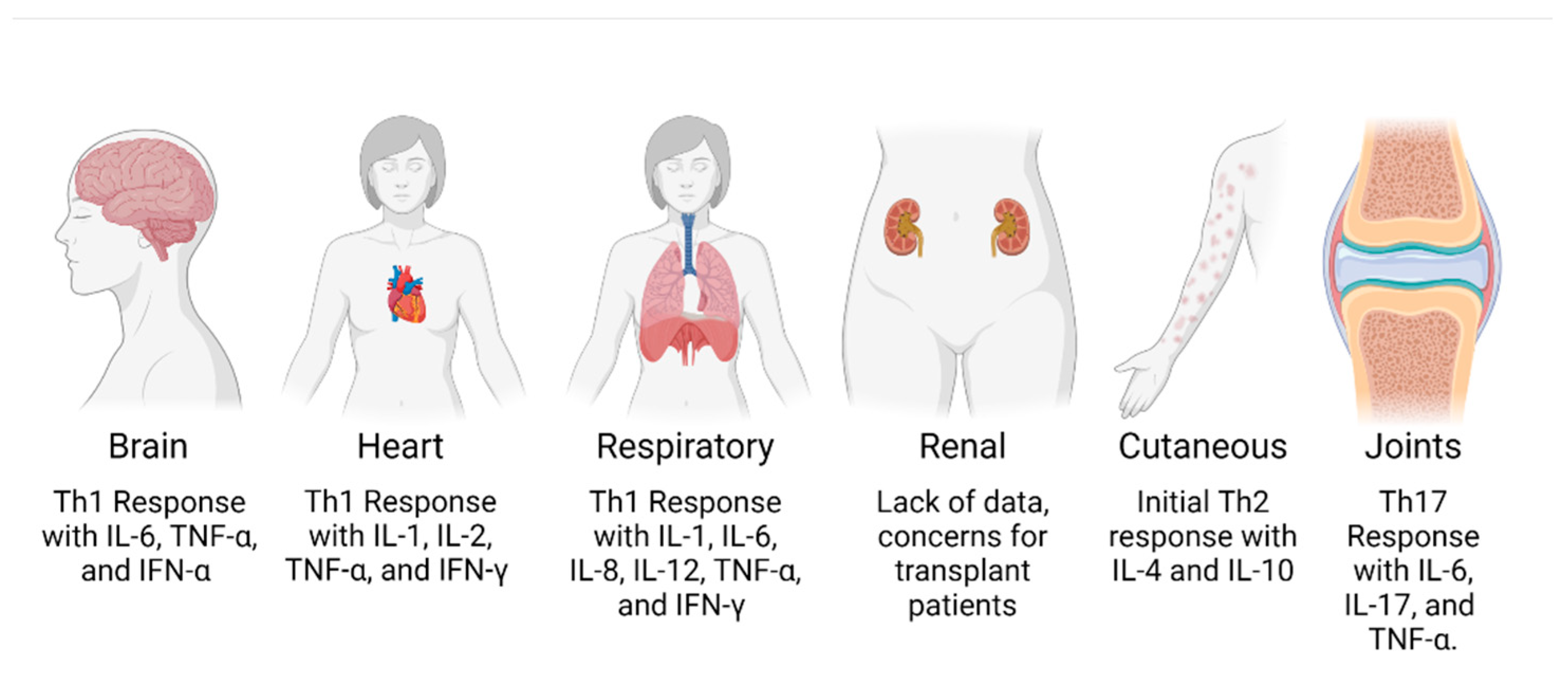
Chikungunya Immunopathology as It Presents in Different Organ Systems
Abstract
:1. Introduction
2. General Chikungunya Infection of the Human Host
3. Clinically Disturbing Neurological Complications
4. Increasingly Common Cardiovascular Presentations
5. Rare Respiratory Complications
6. Potential Renal Complications and Concerns for Organ Transplantation
7. Cutaneous and Mucocutaneous Presentations
8. Joint Inflammation and Arthritis, the Most Common Presentation
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Constant, L.E.C.; Rajsfus, B.F.; Carneiro, P.H.; Sisnande, T.; Mohana-Borges, R.; Allonso, D. Overview on Chikungunya Virus Infection: From Epidemiology to State-of-the-Art Experimental Models. Front. Microbiol. 2021, 12, 744164. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.V.J.; Ludwig-Begall, L.F.; de Oliveira-Filho, E.F.; Oliveira, R.A.S.; Durães-Carvalho, R.; Lopes, T.R.R.; Silva, D.E.A.; Gil, L.H.V.G. A Scoping Review of Chikungunya Virus Infection: Epidemiology, Clinical Characteristics, Viral Co-Circulation Complications, and Control. Acta Trop. 2018, 188, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Zeller, H.; Van Bortel, W.; Sudre, B. Chikungunya: Its History in Africa and Asia and Its Spread to New Regions in 2013–2014. J. Infect. Dis. 2016, 214, S436–S440. [Google Scholar] [CrossRef] [PubMed]
- Vega-Rúa, A.; Marconcini, M.; Madec, Y.; Manni, M.; Carraretto, D.; Gomulski, L.M.; Gasperi, G.; Failloux, A.-B.; Malacrida, A.R. Vector Competence of Aedes Albopictus Populations for Chikungunya Virus Is Shaped by Their Demographic History. Commun. Biol. 2020, 3, 326. [Google Scholar] [CrossRef]
- World Health Organization. Chikungunya Fact Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/chikungunya (accessed on 5 November 2021).
- Centers for Disease Control Areas at Risk for Chikungunya|Chikungunya Virus|CDC. Available online: https://www.cdc.gov/chikungunya/geo/index.html (accessed on 21 May 2022).
- European Centre for Disease Prevention and Control Chikungunya Worldwide Overview. Available online: https://www.ecdc.europa.eu/en/chikungunya-monthly (accessed on 7 June 2022).
- Puntasecca, C.J.; King, C.H.; LaBeaud, A.D. Measuring the Global Burden of Chikungunya and Zika Viruses: A Systematic Review. PLoS Negl. Trop. Dis. 2021, 15, e0009055. [Google Scholar] [CrossRef]
- Bettis, A.A.; Jackson, M.L.; Yoon, I.-K.; Breugelmans, J.G.; Goios, A.; Gubler, D.J.; Powers, A.M. The Global Epidemiology of Chikungunya from 1999 to 2020: A Systematic Literature Review to Inform the Development and Introduction of Vaccines. PLoS Negl. Trop. Dis. 2022, 16, e0010069. [Google Scholar] [CrossRef]
- Volk, S.M.; Chen, R.; Tsetsarkin, K.A.; Adams, A.P.; Garcia, T.I.; Sall, A.A.; Nasar, F.; Schuh, A.J.; Holmes, E.C.; Higgs, S.; et al. Genome-Scale Phylogenetic Analyses of Chikungunya Virus Reveal Independent Emergences of Recent Epidemics and Various Evolutionary Rates. J. Virol. 2010, 84, 6497–6504. [Google Scholar] [CrossRef]
- Weaver, S.C.; Forrester, N.L. Chikungunya: Evolutionary History and Recent Epidemic Spread. Antivir. Res. 2015, 120, 32–39. [Google Scholar] [CrossRef]
- Vu, D.M.; Jungkind, D. Angelle Desiree LaBeaud Chikungunya Virus. Clin. Lab. Med. 2017, 37, 371–382. [Google Scholar] [CrossRef]
- Lumsden, W.H. An Epidemic of Virus Disease in Southern Province, Tanganyika Territory, in 1952-53. II. General Description and Epidemiology. Trans. R. Soc. Trop. Med. Hyg. 1955, 49, 33–57. [Google Scholar] [CrossRef]
- Wahid, B.; Ali, A.; Rafique, S.; Idrees, M. Global Expansion of Chikungunya Virus: Mapping the 64-Year History. Int. J. Infect. Dis. 2017, 58, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Angelini, R.; Finarelli, A.C.; Angelini, P.; Po, C.; Petropulacos, K.; Silvi, G.; Macini, P.; Fortuna, C.; Venturi, G.; Magurano, F.; et al. Chikungunya in North-Eastern Italy: A Summing up of the Outbreak. Eurosurveillance 2007, 12, 3313. [Google Scholar] [CrossRef] [PubMed]
- Grandadam, M.; Caro, V.; Plumet, S.; Thiberge, J.-M.; Souarès, Y.; Failloux, A.-B.; Tolou, H.J.; Budelot, M.; Cosserat, D.; Leparc-Goffart, I.; et al. Chikungunya Virus, Southeastern France. Emerg. Infect. Dis. 2011, 17, 910–913. [Google Scholar] [CrossRef] [PubMed]
- Bustos Carrillo, F.; Collado, D.; Sanchez, N.; Ojeda, S.; Lopez Mercado, B.; Burger-Calderon, R.; Gresh, L.; Gordon, A.; Balmaseda, A.; Kuan, G.; et al. Epidemiological Evidence for Lineage-Specific Differences in the Risk of Inapparent Chikungunya Virus Infection. J. Virol. 2019, 93, e01622-18. [Google Scholar] [CrossRef]
- de Castro, A.P.C.R.; Lima, R.A.; Nascimento, J.d.S. Chikungunya: Vision of the Pain Clinician. Rev. Dor 2016, 17, 299–302. [Google Scholar] [CrossRef]
- Goupil, B.A.; Mores, C.N. A Review of Chikungunya Virus-Induced Arthralgia: Clinical Manifestations, Therapeutics, and Pathogenesis. Open Rheumatol. J. 2016, 10, 129–140. [Google Scholar] [CrossRef]
- Centers for Disease Control Chikungunya: Information for Healthcare Providers 2014. Available online: https://www.cdc.gov/chikungunya/pdfs/CHIKV_Clinicians.pdf (accessed on 30 May 2022).
- Sales, G.M.P.G.; Barbosa, I.C.P.; Canejo Neta, L.M.S.; de Melo, P.L.; Leitão, R.d.A.; Melo, H.M.d.A. Treatment of Chikungunya Chronic Arthritis: A Systematic Review. Rev. Assoc. Med. Bras. 2018, 64, 63–70. [Google Scholar] [CrossRef]
- Guaraldo, L.; Wakimoto, M.D.; Ferreira, H.; Bressan, C.; Calvet, G.A.; Pinheiro, G.C.; Siqueira, A.M.; Brasil, P. Treatment of Chikungunya Musculoskeletal Disorders: A Systematic Review. Expert Rev. Anti-Infect. Ther. 2018, 16, 333–344. [Google Scholar] [CrossRef]
- Hayman, B.; Pagliusi, S. Emerging Vaccine Manufacturers Are Innovating for the next Decade. Vaccine X 2020, 5, 100066. [Google Scholar] [CrossRef]
- Wressnigg, N.; Hochreiter, R.; Zoihsl, O.; Fritzer, A.; Bézay, N.; Klingler, A.; Lingnau, K.; Schneider, M.; Lundberg, U.; Meinke, A.; et al. Single-Shot Live-Attenuated Chikungunya Vaccine in Healthy Adults: A Phase 1, Randomised Controlled Trial. Lancet Infect. Dis. 2020, 20, 1193–1203. [Google Scholar] [CrossRef]
- Schrauf, S.; Tschismarov, R.; Tauber, E.; Ramsauer, K. Current Efforts in the Development of Vaccines for the Prevention of Zika and Chikungunya Virus Infections. Front. Immunol. 2020, 11, 592. [Google Scholar] [CrossRef] [PubMed]
- Petitdemange, C.; Wauquier, N.; Vieillard, V. Control of Immunopathology during Chikungunya Virus Infection. J. Allergy Clin. Immunol. 2015, 135, 846–855. [Google Scholar] [CrossRef] [PubMed]
- Sourisseau, M.; Schilte, C.; Casartelli, N.; Trouillet, C.; Guivel-Benhassine, F.; Rudnicka, D.; Sol-Foulon, N.; Roux, K.L.; Prevost, M.-C.; Fsihi, H.; et al. Characterization of Reemerging Chikungunya Virus. PLoS Pathog. 2007, 3, e89. [Google Scholar] [CrossRef]
- Lum, F.-M.; Ng, L.F.P. Cellular and Molecular Mechanisms of Chikungunya Pathogenesis. Antivir. Res. 2015, 120, 165–174. [Google Scholar] [CrossRef]
- Signorile, A.; Sgaramella, G.; Bellomo, F.; De Rasmo, D. Prohibitins: A Critical Role in Mitochondrial Functions and Implication in Diseases. Cells 2019, 8, 71. [Google Scholar] [CrossRef]
- Wintachai, P.; Wikan, N.; Kuadkitkan, A.; Jaimipuk, T.; Ubol, S.; Pulmanausahakul, R.; Auewarakul, P.; Kasinrerk, W.; Weng, W.-Y.; Panyasrivanit, M.; et al. Identification of Prohibitin as a Chikungunya Virus Receptor Protein. J. Med. Virol. 2012, 84, 1757–1770. [Google Scholar] [CrossRef]
- Schnierle, B.S. Cellular Attachment and Entry Factors for Chikungunya Virus. Viruses 2019, 11, 1078. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Kim, A.S.; Fox, J.M.; Nair, S.; Basore, K.; Klimstra, W.B.; Rimkunas, R.; Fong, R.H.; Lin, H.; Poddar, S.; et al. Mxra8 Is a Receptor for Multiple Arthritogenic Alphaviruses. Nature 2018, 557, 570–574. [Google Scholar] [CrossRef] [PubMed]
- De Caluwé, L.; Coppens, S.; Vereecken, K.; Daled, S.; Dhaenens, M.; Van Ostade, X.; Deforce, D.; Ariën, K.K.; Bartholomeeusen, K. The CD147 Protein Complex Is Involved in Entry of Chikungunya Virus and Related Alphaviruses in Human Cells. Front. Microbiol. 2021, 12, 352. [Google Scholar] [CrossRef]
- Moller-Tank, S.; Kondratowicz, A.S.; Davey, R.A.; Rennert, P.D.; Maury, W. Role of the Phosphatidylserine Receptor TIM-1 in Enveloped-Virus Entry. J. Virol. 2013, 87, 8327–8341. [Google Scholar] [CrossRef]
- Prado Acosta, M.; Geoghegan, E.M.; Lepenies, B.; Ruzal, S.; Kielian, M.; Martinez, M.G. Surface (S) Layer Proteins of Lactobacillus Acidophilus Block Virus Infection via DC-SIGN Interaction. Front. Microbiol. 2019, 10, 810. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.A.; Dermody, T.S. Chikungunya Virus: Epidemiology, Replication, Disease Mechanisms, and Prospective Intervention Strategies. J. Clin. Investig. 2017, 127, 737–749. [Google Scholar] [CrossRef] [PubMed]
- Inglis, F.M.; Lee, K.M.; Chiu, K.B.; Purcell, O.M.; Didier, P.J.; Russell-Lodrigues, K.; Weaver, S.C.; Roy, C.J.; MacLean, A.G. Neuropathogenesis of Chikungunya Infection: Astrogliosis and Innate Immune Activation. J. Neurovirol. 2016, 22, 140–148. [Google Scholar] [CrossRef]
- Bender, A.T.; Tzvetkov, E.; Pereira, A.; Wu, Y.; Kasar, S.; Przetak, M.M.; Vlach, J.; Niewold, T.B.; Jensen, M.A.; Okitsu, S.L. TLR7 and TLR8 Differentially Activate the IRF and NF-ΚB Pathways in Specific Cell Types to Promote Inflammation. ImmunoHorizons 2020, 4, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Wauquier, N.; Becquart, P.; Nkoghe, D.; Padilla, C.; Ndjoyi-Mbiguino, A.; Leroy, E.M. The Acute Phase of Chikungunya Virus Infection in Humans Is Associated with Strong Innate Immunity and T CD8 Cell Activation. J. Infect. Dis. 2011, 204, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Ng, L.F.P.; Chow, A.; Sun, Y.-J.; Kwek, D.J.C.; Lim, P.-L.; Dimatatac, F.; Ng, L.-C.; Ooi, E.-E.; Choo, K.-H.; Her, Z.; et al. IL-1beta, IL-6, and RANTES as Biomarkers of Chikungunya Severity. PLoS ONE 2009, 4, e4261. [Google Scholar] [CrossRef]
- Tanabe, I.S.B.; Tanabe, E.L.L.; Santos, E.C.; Martins, W.V.; Araújo, I.M.T.C.; Cavalcante, M.C.A.; Lima, A.R.V.; Câmara, N.O.S.; Anderson, L.; Yunusov, D.; et al. Cellular and Molecular Immune Response to Chikungunya Virus Infection. Front. Cell. Infect. Microbiol. 2018, 8, 345. [Google Scholar] [CrossRef]
- Galatas, B.; Ly, S.; Duong, V.; Baisley, K.; Nguon, K.; Chan, S.; Huy, R.; Ly, S.; Sorn, S.; Som, L.; et al. Long-Lasting Immune Protection and Other Epidemiological Findings after Chikungunya Emergence in a Cambodian Rural Community, April 2012. PLoS Negl. Trop. Dis. 2016, 10, e0004281. [Google Scholar] [CrossRef]
- Cerny, T.; Schwarz, M.; Schwarz, U.; Lemant, J.; Gérardin, P.; Keller, E. The Range of Neurological Complications in Chikungunya Fever. Neurocrit. Care 2017, 27, 447–457. [Google Scholar] [CrossRef]
- Hopkins, H.K.; Traverse, E.M.; Barr, K.L. Chikungunya Encephalitis: An Inconsistently Reported Headache and Cause of Death in Patients with Pre-Existing Conditions. Curr. Trop. Med. Rep. 2022, 291, 1–19. [Google Scholar] [CrossRef]
- Brito Ferreira, M.L.; Militão de Albuquerque, M.d.F.P.; de Brito, C.A.A.; de Oliveira França, R.F.; Porto Moreira, Á.J.; de Morais Machado, M.Í.; da Paz Melo, R.; Medialdea-Carrera, R.; Dornelas Mesquita, S.; Lopes Santos, M.; et al. Neurological Disease in Adults with Zika and Chikungunya Virus Infection in Northeast Brazil: A Prospective Observational Study. Lancet Neurol. 2020, 19, 826–839. [Google Scholar] [CrossRef]
- Anand, K.S.; Agrawal, A.K.; Garg, J.; Dhamija, R.K.; Mahajan, R.K. Spectrum of Neurological Complications in Chikungunya Fever: Experience at a Tertiary Care Centre and Review of Literature. Trop. Doct. 2019, 49, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.; Gerardin, P.; de Brito, C.A.A.; Soares, C.N.; Ferreira, M.L.B.; Solomon, T. The Neurological Complications of Chikungunya Virus: A Systematic Review. Rev. Med. Virol. 2018, 28, e1978. [Google Scholar] [CrossRef] [PubMed]
- Carrera, J.-P.; Cucunubá, Z.M.; Neira, K.; Lambert, B.; Pittí, Y.; Liscano, J.; Garzón, J.L.; Beltran, D.; Collado-Mariscal, L.; Saenz, L.; et al. Endemic and Epidemic Human Alphavirus Infections in Eastern Panama: An Analysis of Population-Based Cross-Sectional Surveys. Am. J. Trop. Med. Hyg. 2020, 103, 2429–2437. [Google Scholar] [CrossRef]
- Guerrero-Arguero, I.; Tellez-Freitas, C.M.; Scott Weber, K.; Berges, B.K.; Robinson, R.A.; Pickett, B.E. Alphaviruses: Host Pathogenesis, Immune Response, and Vaccine & Treatment Updates. Microbiol. Soc. 2021, 102, 001644. [Google Scholar] [CrossRef]
- Economopoulou, A.; Dominguez, M.; Helynck, B.; Sissoko, D.; Wichmann, O.; Quenel, P.; Germonneau, P.; Quatresous, I. Atypical Chikungunya Virus Infections: Clinical Manifestations, Mortality and Risk Factors for Severe Disease during the 2005–2006 Outbreak on Réunion. Epidemiol. Infect. 2009, 137, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Tandale, B.V.; Sathe, P.S.; Arankalle, V.A.; Wadia, R.S.; Kulkarni, R.; Shah, S.V.; Shah, S.K.; Sheth, J.K.; Sudeep, A.B.; Tripathy, A.S.; et al. Systemic Involvements and Fatalities during Chikungunya Epidemic in India, 2006. J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol. 2009, 46, 145–149. [Google Scholar] [CrossRef] [PubMed]
- van Aalst, M.; Nelen, C.M.; Goorhuis, A.; Stijnis, C.; Grobusch, M.P. Long-Term Sequelae of Chikungunya Virus Disease: A Systematic Review. Travel Med. Infect. Dis. 2017, 15, 8–22. [Google Scholar] [CrossRef]
- Palha, N.; Guivel-Benhassine, F.; Briolat, V.; Lutfalla, G.; Sourisseau, M.; Ellett, F.; Wang, C.-H.; Lieschke, G.J.; Herbomel, P.; Schwartz, O.; et al. Real-Time Whole-Body Visualization of Chikungunya Virus Infection and Host Interferon Response in Zebrafish. PLoS Pathog. 2013, 9, e1003619. [Google Scholar] [CrossRef]
- Passoni, G.; Langevin, C.; Palha, N.; Mounce, B.C.; Briolat, V.; Affaticati, P.; De Job, E.; Joly, J.-S.; Vignuzzi, M.; Saleh, M.-C.; et al. Imaging of Viral Neuroinvasion in the Zebrafish Reveals That Sindbis and Chikungunya Viruses Favour Different Entry Routes. Dis. Model. Mech. 2017, 10, 847–857. [Google Scholar] [CrossRef]
- Kashyap, R.S.; Morey, S.; Bhullar, S.; Baheti, N.; Chandak, N.; Purohit, H.; Taori, G.; Daginawala, H. Determination of Toll-like Receptor-Induced Cytokine Profiles in the Blood and Cerebrospinal Fluid of Chikungunya Patients. Neuroimmunomodulation 2014, 21, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.J.; Ashkar, A.A. The Dual Nature of Type I and Type II Interferons. Front. Immunol. 2018, 9, 2061. [Google Scholar] [CrossRef]
- Priya, R.; Patro, I.K.; Parida, M.M. TLR3 Mediated Innate Immune Response in Mice Brain Following Infection with Chikungunya Virus. Virus Res. 2014, 189, 194–205. [Google Scholar] [CrossRef]
- Blackburn, D.; Sargsyan, S.; Monk, P.N.; Shaw, P.J. Astrocyte Function and Role in Motor Neuron Disease: A Future Therapeutic Target? Glia 2009, 57, 1251–1264. [Google Scholar] [CrossRef] [PubMed]
- Abraham, R.; Mudaliar, P.; Padmanabhan, A.; Sreekumar, E. Induction of Cytopathogenicity in Human Glioblastoma Cells by Chikungunya Virus. PLoS ONE 2013, 8, e75854. [Google Scholar] [CrossRef] [PubMed]
- Yang, I.; Han, S.J.; Kaur, G.; Crane, C.; Parsa, A.T. The Role of Microglia in Central Nervous System Immunity and Glioma Immunology. J. Clin. Neurosci. 2010, 17, 6–10. [Google Scholar] [CrossRef]
- Labadie, K.; Larcher, T.; Joubert, C.; Mannioui, A.; Delache, B.; Brochard, P.; Guigand, L.; Dubreil, L.; Lebon, P.; Verrier, B.; et al. Chikungunya Disease in Nonhuman Primates Involves Long-Term Viral Persistence in Macrophages. J. Clin. Investig. 2010, 120, 894–906. [Google Scholar] [CrossRef]
- Qadri, S.W.; Kumar, N.; Santhoshkumar, R.; Desai, A.; Ravi, V.; Venkataswamy, M.M. Infection of Human Microglial Cell Line CHME-3 to Study Neuropathogenesis of Chikungunya Virus. J. Neurovirol. 2022; Online ahead of print. [Google Scholar] [CrossRef]
- Abere, B.; Wikan, N.; Ubol, S.; Auewarakul, P.; Paemanee, A.; Kittisenachai, S.; Roytrakul, S.; Smith, D.R. Proteomic Analysis of Chikungunya Virus Infected Microgial Cells. PLoS ONE 2012, 7, e34800. [Google Scholar] [CrossRef]
- Traverse, E.M.; Hopkins, H.K.; Vaidhyanathan, V.; Barr, K.L. Cardiomyopathy and Death Following Chikungunya Infection: An Increasingly Common Outcome. Trop. Med. Infect. Dis. 2021, 6, 108. [Google Scholar] [CrossRef]
- Alvarez, M.F.; Bolívar-Mejía, A.; Rodriguez-Morales, A.J.; Ramirez-Vallejo, E. Cardiovascular Involvement and Manifestations of Systemic Chikungunya Virus Infection: A Systematic Review. F1000Research 2017, 6, 390. [Google Scholar] [CrossRef] [PubMed]
- London, B. Immune Modulation of Cardiac Arrhythmias. Circ. Res. 2017, 121, 11–12. [Google Scholar] [CrossRef] [PubMed]
- Schultz, J.C.; Hilliard, A.A.; Cooper, L.T.; Rihal, C.S. Diagnosis and Treatment of Viral Myocarditis. Mayo Clin. Proc. 2009, 84, 1001–1009. [Google Scholar] [CrossRef]
- Mann, D.L. The Emerging Role of Innate Immunity in the Heart and Vascular System: For Whom the Cell Tolls. Circ. Res. 2011, 108, 1133–1145. [Google Scholar] [CrossRef] [PubMed]
- Kearney, M.; Cotton, J.; Richardson, P.; Shah, A. Viral Myocarditis and Dilated Cardiomyopathy: Mechanisms, Manifestations, and Management. Postgrad. Med. J. 2001, 77, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Mason, J.W. Myocarditis and Dilated Cardiomyopathy|Cardiovascular Research|Oxford Academic. Available online: https://academic.oup.com/cardiovascres/article/60/1/5/322628 (accessed on 30 January 2021).
- Human Protein Atlas Tissue Expression of PHB-Primary Data—The Human Protein Atlas. Available online: https://www.proteinatlas.org/ENSG00000167085-PHB/tissue/primary+data (accessed on 9 June 2021).
- Human Protein Atlas Tissue Expression of BSG-Summary—The Human Protein Atlas. Available online: https://www.proteinatlas.org/ENSG00000172270-BSG/tissue (accessed on 10 October 2021).
- The Human Protein Atlas Tissue Expression of MXRA8-Primary Data—The Human Protein Atlas. Available online: https://www.proteinatlas.org/ENSG00000162576-MXRA8/tissue/primary+data (accessed on 9 June 2021).
- Mallilankaraman, K.; Shedlock, D.J.; Bao, H.; Kawalekar, O.U.; Fagone, P.; Ramanathan, A.A.; Ferraro, B.; Stabenow, J.; Vijayachari, P.; Sundaram, S.G.; et al. A DNA Vaccine against Chikungunya Virus Is Protective in Mice and Induces Neutralizing Antibodies in Mice and Nonhuman Primates. PLoS Negl. Trop. Dis. 2011, 5, e928. [Google Scholar] [CrossRef] [PubMed]
- Ngwe Tun, M.M.; Muthugala, R.; Kyaw Kyaw, A.; Shimada, S.; Morita, K.; Hayasaka, D. Pathogenetic Potential Relating to Metabolic Activity in a Mouse Model of Infection with the Chikungunya Virus East/Central/South African Genotype. Viruses 2020, 12, 169. [Google Scholar] [CrossRef]
- Sharp, T.M.; Keating, M.K.; Shieh, W.-J.; Bhatnager, J. Clinical Characteristics, Histopathology, and Tissue Immunolocalization of Chikungunya Virus Antigen in Fatal Cases|Clinical Infectious Diseases|Oxford Academic. Available online: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa837/5866622 (accessed on 31 January 2021).
- Zhang, H.-L.; Dong, H.-L.; Zhang, Y.-N.; Xu, L.-L.; Deng, C.-L.; Li, X.-F.; Li, X.-D.; Ye, H.-Q.; Yuan, Z.-M.; Qin, C.-F.; et al. Visualization of Chikungunya Virus Infection in Vitro and in Vivo. Emerg. Microbes Infect. 2019, 8, 1574–1583. [Google Scholar] [CrossRef]
- Cojan-Minzat, B.O.; Zlibut, A.; Agoston-Coldea, L. Non-Ischemic Dilated Cardiomyopathy and Cardiac Fibrosis. Heart Fail. Rev. 2020, 26, 1081–1101. [Google Scholar] [CrossRef]
- Schultheiss, H.-P.; Fairweather, D.; Caforio, A.L.P.; Escher, F.; Hershberger, R.E.; Lipshultz, S.E.; Liu, P.P.; Matsumori, A.; Mazzanti, A.; McMurray, J.; et al. Dilated Cardiomyopathy. Nat. Rev. Dis. Primer 2019, 5. [Google Scholar] [CrossRef]
- Her, Z.; Teng, T.-S.; Tan, J.J.; Teo, T.-H.; Kam, Y.-W.; Lum, F.-M.; Lee, W.W.; Gabriel, C.; Melchiotti, R.; Andiappan, A.K.; et al. Loss of TLR3 Aggravates CHIKV Replication and Pathology Due to an Altered Virus-Specific Neutralizing Antibody Response. EMBO Mol. Med. 2015, 7, 24–41. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.R.; Leopoldo, C.G.; Castro, J.S.; Rodríguez, L.; Saravia, V.; Arvelaez, J.; Ríos-Fabra, A.; Longhi, M.A.; Marcano, M. Chikungunya Fever: Atypical and Lethal Cases in the Western Hemisphere: A Venezuelan Experience. IDCases 2015, 2, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Amin, P.; Silva, G.S.; Hidalgo, J.; Jiménez, J.I.S.; Karnad, D.R.; Richards, G.A. Chikungunya: Report from the Task Force on Tropical Diseases by the World Federation of Societies of Intensive and Critical Care Medicine. J. Crit. Care 2018, 46, 110–114. [Google Scholar] [CrossRef]
- Oliveira, R.d.M.A.B.; Barreto, F.K.d.A.; Maia, A.M.P.C.; Gomes, I.P.; Simião, A.R.; Barbosa, R.B.; Rodrigues, A.S.R.; Lopes, K.W.; Araújo, F.M.d.C.; do Vale, R.L.S.; et al. Maternal and Infant Death after Probable Vertical Transmission of Chikungunya Virus in Brazil–Case Report. BMC Infect. Dis. 2018, 18, 333. [Google Scholar] [CrossRef] [PubMed]
- Bonifay, T.; Prince, C.; Neyra, C.; Demar, M.; Rousset, D.; Kallel, H.; Nacher, M.; Djossou, F.; Epelboin, L. Atypical and Severe Manifestations of Chikungunya Virus Infection in French Guiana: A Hospital-Based Study. PLoS ONE 2018, 13, e0207406. [Google Scholar] [CrossRef] [PubMed]
- Cerbino-Neto, J.; Mesquita, E.C.; Amancio, R.T.; Brasil, P.E.A.A. Do Events Preceding Death among Chikungunya Virus Infected Patients: A Systematic Review. Available online: https://www.scielo.br/scielo.php?pid=S0037-86822020000100201&script=sci_arttext (accessed on 31 January 2021).
- Calvo, E.P.; Archila, E.D.; López, L.; Castellanos, J.E. Rediscovering the Chikungunya Virus. Biomed. Rev. Inst. Nac. Salud 2021, 41, 353–373. [Google Scholar] [CrossRef]
- Benjamanukul, S.; Chansaenroj, J.; Chirathaworn, C.; Poovorawan, Y. Atypical Skin Manifestation in Severe Acute Chikungunya Infection in a Pregnant Woman: A Case Report. J. Med. Case Rep. 2022, 16, 5. [Google Scholar] [CrossRef]
- Singh, A. Acute Respiratory Distress Syndrome: An Unusual Presentation of Chikungunya Fever Viral Infection. J. Glob. Infect. Dis. 2017, 9, 33–34. [Google Scholar] [CrossRef]
- The ARDS Definition Task Force. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Fan, E.; Brodie, D.; Slutsky, A.S. Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment. JAMA 2018, 319, 698–710. [Google Scholar] [CrossRef]
- Moldoveanu, B.; Otmishi, P.; Jani, P.; Walker, J.; Sarmiento, X.; Guardiola, J.; Saad, M.; Yu, J. Inflammatory Mechanisms in the Lung. J. Inflamm. Res. 2009, 2, 1–11. [Google Scholar]
- Vellere, I.; Lagi, F.; Spinicci, M.; Mantella, A.; Mantengoli, E.; Corti, G.; Colao, M.G.; Gobbi, F.; Rossolini, G.M.; Bartoloni, A.; et al. Arbo-Score: A Rapid Score for Early Identification of Patients with Imported Arbovirosis Caused by Dengue, Chikungunya and Zika Virus. Microorganisms 2020, 8, 1731. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.H.; Cruz-Lopez, F.; Vargas Torres, D.; Perez-Padilla, J.; Lorenzi, O.D.; Rivera, A.; Staples, J.E.; Lugo, E.; Munoz-Jordan, J.; Fischer, M.; et al. Risk Factors for Hospitalization of Patients with Chikungunya Virus Infection at Sentinel Hospitals in Puerto Rico. PLoS Negl. Trop. Dis. 2019, 13, e0007084. [Google Scholar] [CrossRef]
- Rouse, B.T.; Sehrawat, S. Immunity and Immunopathology to Viruses: What Decides the Outcome? Nat. Rev. Immunol. 2010, 10, 514–526. [Google Scholar] [CrossRef] [PubMed]
- Mueller, S.N.; Rouse, B.T. Immune Responses to Viruses. Clin. Immunol. 2008, 421–431. [Google Scholar] [CrossRef]
- Rai, K.R.; Shrestha, P.; Yang, B.; Chen, Y.; Liu, S.; Maarouf, M.; Chen, J.-L. Acute Infection of Viral Pathogens and Their Innate Immune Escape. Front. Microbiol. 2021, 12, 672026. [Google Scholar] [CrossRef]
- Foresto, R.D.; Santos, D.W.d.C.L.; Hazin, M.A.A.; Leyton, A.T.Z.; Tenório, N.C.; Viana, L.A.; Cristelli, M.P.; Silva, H.T.; Pestana, J.O.M. Chikungunya in a Kidney Transplant Recipient: A Case Report. J. Bras. Nefrol. 2019, 41, 575–579. [Google Scholar] [CrossRef]
- Mercado, M.; Acosta-Reyes, J.; Parra, E.; Guzmán, L.; Beltrán, M.; Gasque, P.; Mejía-García, C.; Viasus, D. Renal Involvement in Fatal Cases of Chikungunya Virus Infection. J. Clin. Virol. 2018, 103, 16–18. [Google Scholar] [CrossRef]
- Perti, T.; Lucero-Obusan, C.A.; Schirmer, P.L.; Winters, M.A.; Holodniy, M. Chikungunya Fever Cases Identified in the Veterans Health Administration System, 2014. PLoS Negl. Trop. Dis. 2016, 10, e0004630. [Google Scholar] [CrossRef]
- da Silva Junior, G.B.; Pinto, J.R.; Mota, R.M.S.; Pires Neto, R.d.J.; Daher, E.D.F. Impact of Chronic Kidney Disease on Chikungunya Virus Infection Clinical Manifestations and Outcome: Highlights during an Outbreak in Northeastern Brazil. Am. J. Trop. Med. Hyg. 2018, 99, 1327–1330. [Google Scholar] [CrossRef]
- Gupta, N.; Mittal, A.; Kutty, S.V.; Kumar, A.; Wig, N. Technical and Alarm Signs for Referral in Adult Patients with Acute Febrile Illness: A Study from a Tertiary Care Hospital in North India. J. Fam. Med. Prim. Care 2018, 7, 832–835. [Google Scholar] [CrossRef]
- Pinto, J.R.; da Silva Junior, G.B.; Mota, R.M.S.; Martins, P.; Santos, A.K.T.; de Moura, D.C.N.; Pires Neto, R.d.J.; Daher, E.D.F. Clinical Profile and Factors Associated with Hospitalization during a Chikungunya Epidemic in Ceará, Brazil. Rev. Soc. Bras. Med. Trop. 2019, 52, e20190167. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control Key Facts|Overview|Transplant Safety|CDC. Available online: https://www.cdc.gov/transplantsafety/overview/key-facts.html (accessed on 8 August 2022).
- Moura-Neto, J.A.; Braga Silva, C.A.; Moura, A.F.; Rocco Suassuna, J.H. Emergent Arboviruses and Renal Transplantation: A Global Challenge. Kidney Int. Rep. 2019, 4, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Moura-Neto, J.A.; de Souza Moura, A.F.; Souza, E.; de Carvalho Henriques, J.L.; Arruda, M.B.; Pessoa, L.S.; Boullosa, L.T.; da Costa Ferreira Junior, O.; Rocco Suassuna, J.H. Successful Live Kidney Transplantation after Chikungunya Disease in the Donor. Kidney Int. Rep. 2017, 2, 1250–1253. [Google Scholar] [CrossRef] [PubMed]
- Ensor, C.R.; Trofe-Clark, J.; Gabardi, S.; McDevitt-Potter, L.M.; Shullo, M.A. Generic Maintenance Immunosuppression in Solid Organ Transplant Recipients. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2011, 31, 1111–1129. [Google Scholar] [CrossRef]
- Pierrotti, L.C.; Lopes, M.I.B.F.; do Nascimento, A.P.; Caiaffa-Filho, H.; Lemos, F.B.C.; Reusing, J.O.; Sejas, O.N.E.; David-Neto, E.; Azevedo, L.S. Chikungunya in Kidney Transplant Recipients: A Series of Cases. Int. J. Infect. Dis. 2017, 64, 96–99. [Google Scholar] [CrossRef]
- Amaral, J.K.; Sutaria, R.; Schoen, R.T. Treatment of Chronic Chikungunya Arthritis with Methotrexate: A Systematic Review. Arthritis Care Res. 2018, 70, 1501–1508. [Google Scholar] [CrossRef]
- Bandyopadhyay, D.; Ghosh, S.K. Mucocutaneous Features of Chikungunya Fever: A Study from an Outbreak in West Bengal, India. Int. J. Dermatol. 2008, 47, 1148–1152. [Google Scholar] [CrossRef]
- Prashant, S.; Kumar, A.S.; Basheeruddin, D.D.M.; Chowdhary, T.N.; Madhu, B. Cutaneous Manifestations in Patients Suspected of Chikungunya Disease. Indian J. Dermatol. 2009, 54, 128–131. [Google Scholar] [CrossRef]
- Riyaz, N.; Riyaz, A.; Rahima; Abdul Latheef, E.N.; Anitha, P.M.; Aravindan, K.P.; Nair, A.S.; Shameera, P. Cutaneous Manifestations of Chikungunya during a Recent Epidemic in Calicut, North Kerala, South India. Indian J. Dermatol. Venereol. Leprol. 2010, 76, 671–676. [Google Scholar] [CrossRef]
- Seetharam, K.A.; Sridevi, K.; Vidyasagar, P. Cutaneous Manifestations of Chikungunya Fever. Indian Pediatr. 2012, 49, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Vasani, R.; Kanhere, S.; Chaudhari, K.; Phadke, V.; Mukherjee, P.; Gupta, S.; Kasliwal, C.; Poojary, S. Congenital Chikungunya—A Cause of Neonatal Hyperpigmentation. Pediatr. Dermatol. 2016, 33, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Domínguez, N.; Achach-Asaf, J.A.; Basso-García, L.M.; Quiñones-Pacheco, Y.B.; Gómez-Carro, S. Septic shock secondary to non-congenital chikungunya fever in a young infant: A clinical case. Rev. Chil. Pediatr. 2016, 87, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Sharma, M.K.; Jain, S.K.; Yadav, S.K.; Singhal, A.K. Cutaneous Manifestations of Chikungunya Fever: Observations from an Outbreak at a Tertiary Care Hospital in Southeast Rajasthan, India. Indian Dermatol. Online J. 2017, 8, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Garg, T.; Sanke, S.; Ahmed, R.; Chander, R.; Basu, S. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis-like Cutaneous Presentation of Chikungunya Fever: A Case Series. Pediatr. Dermatol. 2018, 35, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Sangmala, S.; Eksomtramage, T.; Aiempanakit, K.; Chiratikarnwong, K.; Auepemkiate, S. Lobular Panniculitis Associated with Chikungunya Fever: A Case Report. IDCases 2018, 14, e00462. [Google Scholar] [CrossRef]
- Di Maio Ferreira, F.C.P.A.; da Silva, A.S.V.; Bispo de Filippis, A.M.; Brasil, P. Late Identification of Chikungunya Virus in the Central Nervous System of a 2-Month-Old Infant: Persistence of Maternal-Neonatal Infection? J. Pediatr. Infect. Dis. Soc. 2019, 8, 374–377. [Google Scholar] [CrossRef]
- Barr, K.L.; Vaidhyanathan, V. Chikungunya in Infants and Children: Is Pathogenesis Increasing? Viruses 2019, 11, 294. [Google Scholar] [CrossRef]
- Gavotto, A.; Muanza, B.; Delion, F.; Dusacre, J.-A.; Amedro, P. Chikungunya Disease among Infants in French West Indies during the 2014 Outbreak. Arch. Pédiatrie 2019, 26, 259–262. [Google Scholar] [CrossRef]
- Bothra, A.; Maheswari, A.; Singh, M.; Pawar, M.; Jodhani, K. Cutaneous Manifestations of Viral Outbreaks. Australas. J. Dermatol. 2021, 62, 27–36. [Google Scholar] [CrossRef]
- Kaleem, S.; Ghafoor, R.; Khan, S. Mucocutaneous Manifestations of Chikungunya Fever, an Experience of Tertiary Care Hospital. JPMA J. Pak. Med. Assoc. 2021, 71, 619–623. [Google Scholar] [CrossRef]
- Inamadar, A.C.; Palit, A.; Sampagavi, V.V.; Raghunath, S.; Deshmukh, N.S. Cutaneous Manifestations of Chikungunya Fever: Observations Made during a Recent Outbreak in South India. Int. J. Dermatol. 2008, 47, 154–159. [Google Scholar] [CrossRef]
- Pakran, J.; George, M.; Riyaz, N.; Arakkal, R.; George, S.; Rajan, U.; Khader, A.; Thomas, S.; Abdurahman, R.; Sasidharanpillai, S.; et al. Purpuric Macules with Vesiculobullous Lesions: A Novel Manifestation of Chikungunya. Int. J. Dermatol. 2011, 50, 61–69. [Google Scholar] [CrossRef]
- Panwar, H.; Joshi, D.; Goel, G.; Asati, D.; Majumdar, K.; Kapoor, N. Diagnostic Utility and Pitfalls of Tzanck Smear Cytology in Diagnosis of Various Cutaneous Lesions. J. Cytol. 2017, 34, 179–182. [Google Scholar] [CrossRef]
- Wichit, S.; Hamel, R.; Zanzoni, A.; Diop, F.; Cribier, A.; Talignani, L.; Diack, A.; Ferraris, P.; Liegeois, F.; Urbach, S.; et al. SAMHD1 Enhances Chikungunya and Zika Virus Replication in Human Skin Fibroblasts. Int. J. Mol. Sci. 2019, 20, 1695. [Google Scholar] [CrossRef]
- Ahmed, T.; Asaduzzaman, S.A.I.; Tanvir, R.; Nahar, Z.; Tasnim, N.; Saha, C.; Noor, R. Pathogenesis of the Chikungunya virus and the host immunity response. Life Res. 2021, 4, 10. [Google Scholar] [CrossRef]
- Agarwal, A.; Joshi, G.; Nagar, D.P.; Sharma, A.K.; Sukumaran, D.; Pant, S.C.; Parida, M.M.; Dash, P.K. Mosquito Saliva Induced Cutaneous Events Augment Chikungunya Virus Replication and Disease Progression. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2016, 40, 126–135. [Google Scholar] [CrossRef]
- Cox, J.; Mota, J.; Sukupolvi-Petty, S.; Diamond, M.S.; Rico-Hesse, R. Mosquito Bite Delivery of Dengue Virus Enhances Immunogenicity and Pathogenesis in Humanized Mice. J. Virol. 2012, 86, 7637–7649. [Google Scholar] [CrossRef]
- Berger, A. Th1 and Th2 Responses: What Are They? BMJ 2000, 321, 424. [Google Scholar] [CrossRef]
- Matusali, G.; Colavita, F.; Bordi, L.; Lalle, E.; Ippolito, G.; Capobianchi, M.R.; Castilletti, C. Tropism of the Chikungunya Virus. Viruses 2019, 11, 175. [Google Scholar] [CrossRef]
- Rodríguez-Morales, A.J.; Cardona-Ospina, J.A.; Fernanda Urbano-Garzón, S.; Sebastian Hurtado-Zapata, J. Prevalence of Post-Chikungunya Infection Chronic Inflammatory Arthritis: A Systematic Review and Meta-Analysis. Arthritis Care Res. 2016, 68, 1849–1858. [Google Scholar] [CrossRef] [PubMed]
- Amaral, J.K.; Bilsborrow, J.B.; Schoen, R.T. Chronic Chikungunya Arthritis and Rheumatoid Arthritis: What They Have in Common. Am. J. Med. 2020, 133, e91–e97. [Google Scholar] [CrossRef]
- Mostafavi, H.; Tharmarajah, K.; Vider, J.; West, N.P.; Freitas, J.R.; Cameron, B.; Foster, P.S.; Hueston, L.P.; Lloyd, A.R.; Mahalingam, S.; et al. Interleukin-17 Contributes to Ross River Virus-Induced Arthritis and Myositis. PLoS Pathog. 2022, 18, e1010185. [Google Scholar] [CrossRef]
- Powers, A.M.; Brault, A.C.; Tesh, R.B.; Weaver, S.C. Re-Emergence of Chikungunya and O’nyong-Nyong Viruses: Evidence for Distinct Geographical Lineages and Distant Evolutionary Relationships. J. Gen. Virol. 2000, 81, 471–479. [Google Scholar] [CrossRef]
- Chaaitanya, I.K.; Muruganandam, N.; Sundaram, S.G.; Kawalekar, O.; Sugunan, A.P.; Manimunda, S.P.; Ghosal, S.R.; Muthumani, K.; Vijayachari, P. Role of Proinflammatory Cytokines and Chemokines in Chronic Arthropathy in CHIKV Infection. Viral Immunol. 2011, 24, 265–271. [Google Scholar] [CrossRef]
- Danillo Lucas Alves, E.; da Benedito Antonio Lopes, F. Characterization of the Immune Response Following in Vitro Mayaro and Chikungunya Viruses (Alphavirus, Togaviridae) Infection of Mononuclear Cells. Virus Res. 2018, 256, 166–173. [Google Scholar] [CrossRef]
- Teo, T.-H.; Lum, F.-M.; Claser, C.; Lulla, V.; Lulla, A.; Merits, A.; Rénia, L.; Ng, L.F.P. A Pathogenic Role for CD4+ T Cells during Chikungunya Virus Infection in Mice. J. Immunol. 2013, 190, 259–269. [Google Scholar] [CrossRef]
- Ruan, Q.; Kameswaran, V.; Zhang, Y.; Zheng, S.; Sun, J.; Wang, J.; DeVirgiliis, J.; Liou, H.-C.; Beg, A.A.; Chen, Y.H. The Th17 Immune Response Is Controlled by the Rel–RORγ–RORγT Transcriptional Axis. J. Exp. Med. 2011, 208, 2321–2333. [Google Scholar] [CrossRef]
- Tesmer, L.A.; Lundy, S.K.; Sarkar, S.; Fox, D.A. Th17 Cells in Human Disease. Immunol. Rev. 2008, 223, 87–113. [Google Scholar] [CrossRef]
- Amaral, J.K.; Taylor, P.C.; Teixeira, M.M.; Morrison, T.E.; Schoen, R.T. The Clinical Features, Pathogenesis and Methotrexate Therapy of Chronic Chikungunya Arthritis. Viruses 2019, 11, 289. [Google Scholar] [CrossRef]
- Bedoui, Y.; Giry, C.; Jaffar-Bandjee, M.-C.; Selambarom, J.; Guiraud, P.; Gasque, P. Immunomodulatory Drug Methotrexate Used to Treat Patients with Chronic Inflammatory Rheumatisms Post-Chikungunya Does Not Impair the Synovial Antiviral and Bone Repair Responses. PLoS Negl. Trop. Dis. 2018, 12, e0006634. [Google Scholar] [CrossRef] [PubMed]
- Pathak, H.; Mohan, M.C.; Ravindran, V. Chikungunya Arthritis. Clin. Med. 2019, 19, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Rezza, G.; Weaver, S.C. Chikungunya as a Paradigm for Emerging Viral Diseases: Evaluating Disease Impact and Hurdles to Vaccine Development. PLoS Negl. Trop. Dis. 2019, 13, e0006919. [Google Scholar] [CrossRef] [PubMed]
- Gasque, P.; Couderc, T.; Lecuit, M.; Roques, P.; Ng, L.F.P. Chikungunya Virus Pathogenesis and Immunity. Vector Borne Zoonotic Dis. 2015, 15, 241–249. [Google Scholar] [CrossRef]
- de Lima Cavalcanti, T.Y.V.; Pereira, M.R.; de Paula, S.O.; Franca, R.F.d.O. A Review on Chikungunya Virus Epidemiology, Pathogenesis and Current Vaccine Development. Viruses 2022, 14, 969. [Google Scholar] [CrossRef]
- Leta, S.; Beyene, T.J.; De Clercq, E.M.; Amenu, K.; Kraemer, M.U.G.; Revie, C.W. Global Risk Mapping for Major Diseases Transmitted by Aedes Aegypti and Aedes Albopictus. Int. J. Infect. Dis. 2018, 67, 25–35. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Traverse, E.M.; Millsapps, E.M.; Underwood, E.C.; Hopkins, H.K.; Young, M.; Barr, K.L. Chikungunya Immunopathology as It Presents in Different Organ Systems. Viruses 2022, 14, 1786. https://doi.org/10.3390/v14081786
Traverse EM, Millsapps EM, Underwood EC, Hopkins HK, Young M, Barr KL. Chikungunya Immunopathology as It Presents in Different Organ Systems. Viruses. 2022; 14(8):1786. https://doi.org/10.3390/v14081786
Chicago/Turabian StyleTraverse, Elizabeth M., Erin M. Millsapps, Emma C. Underwood, Hannah K. Hopkins, Makenzie Young, and Kelli L. Barr. 2022. "Chikungunya Immunopathology as It Presents in Different Organ Systems" Viruses 14, no. 8: 1786. https://doi.org/10.3390/v14081786






