Animal Models for Henipavirus Research
Abstract
:1. Introduction
2. Henipavirus Infection in Humans
2.1. Hendra Virus
2.2. Nipah Virus
3. Animal Models of HNV Infection—Initial Studies
4. Mice
4.1. Immunocompetent Mice
4.2. Immunodeficient Mice
| Species/Genetic Background (Age) | Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| IFNAR-KO (3-week-old) | HeV (prototype) | 1 × 106 PFU | i.p. | 100% | Weight loss, aggressiveness, prostration, paralysis | [58] |
| IFNAR-KO (6-week-old) | ~80% | |||||
| IFNAR-KO (18-week-old) | 50% | |||||
| IFNAR-KO | 1 × 106 PFU | i.n. | None | None | ||
| NOD/SCID/γcnull | NiV-M | 1 × 105 TCID50 | intra-graft | None | None | [63] |
| 1 × 105 TCID50 | i.d. | |||||
| IFNAR-KO | NiV-M (UMMC1) | 1 × 106 PFU | i.p. | 100% (5/5) | Weight loss, aggressiveness, prostration, paralysis | [58] |
| 1 × 106 PFU | i.n | 60% (3/5) | ||||
| 1 × 105 PFU | i.c. | 100% (5/5) | ||||
| a rNiV-FlucNP | 8 × 104 PFU | i.n. | 50% (2/4) | Hunched posture | [64] | |
| 8 × 105 PFU | i.p. | 100% (4/4) | Hunched posture, lethargy, ataxia, seizure | |||
| C57BL/6 MyD88/MAVS-KO | NiV-M (UMMC1) | 1 × 106 PFU | i.p. | 66% (4/6) | Lordosis, prostration, paralysis | [61] |
| C57BL/6 IFNAR-KO | 1 × 106 PFU | 83% (5/6) | ||||
| C57BL/6 MyD88/TRIF/MAVS/STING-KO | NiV-M (UMMC1) | 1 × 106 PFU | i.p. | 100% (5/5) | Yes, not described | [62] |
| C57BL/6 MyD88/TRIF/MAVS-KO | 1 × 106 PFU | 40% (2/5) | ||||
| C57BL/6 IFNAR-KO | 1 × 106 PFU | 80% (4/5) | ||||
| C57BL/6 MyD88 KO | 1 × 106 PFU | None | None | |||
| C57BL/6 MyD88/TRIF-KO | 1 × 106 PFU | None | ||||
| IFNAR-KO (37–44-day-old) | NiV-M | 1 × 104 TCID50 | i.p. | 50% (4/8) | Clinical signs including weight loss b | [59] |
| 1 × 106 TCID50 | 63% (5/8) | |||||
| 1 × 107 TCID50 | 75% (6/8) |
5. Syrian Golden Hamster
6. Guinea Pig
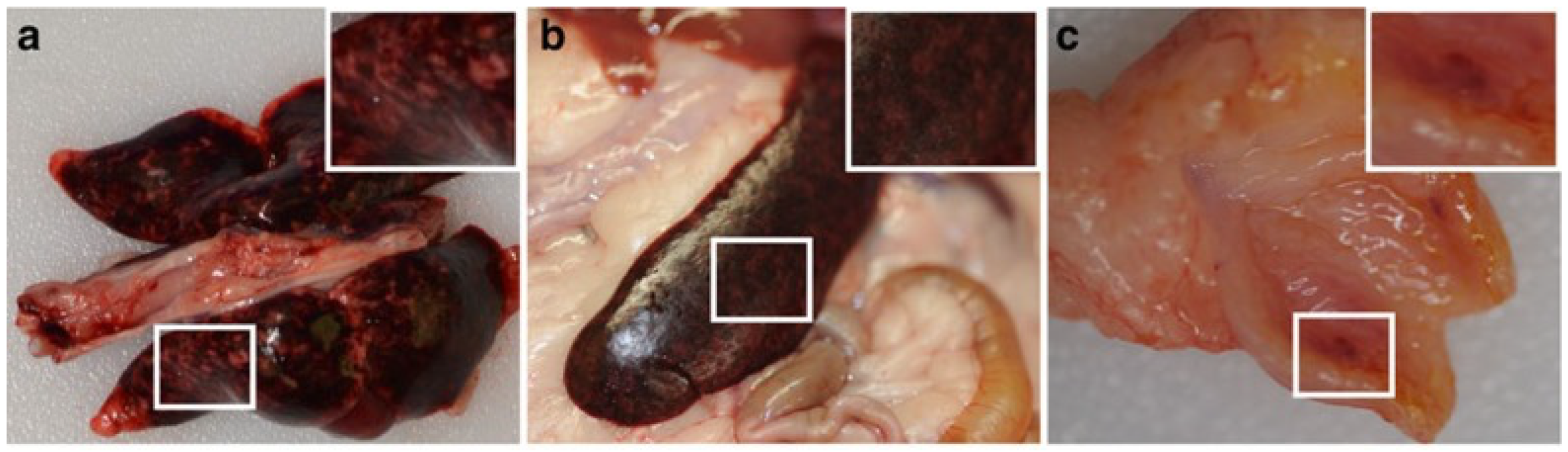
7. Ferret
8. Nonhuman Primates
8.1. African Green Monkey
8.2. Cynomolgus Macaque
8.3. Common Marmoset
8.4. Squirrel Monkey
9. Other Models of Note
9.1. Horses
9.2. Pigs
9.3. Dogs
9.4. Cat
10. Future Directions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Murray, K.; Selleck, P.; Hooper, P.; Hyatt, A.; Gould, A.; Gleeson, L.; Westbury, H.; Hiley, L.; Selvey, L.; Rodwell, B.; et al. A Morbillivirus That Caused Fatal Disease in Horses and Humans. Science 1995, 268, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Chua, K.B.; Goh, K.J.; Wong, K.T.; Kamarulzaman, A.; Tan, P.S.; Ksiazek, T.G.; Zaki, S.R.; Paul, G.; Lam, S.K.; Tan, C.T. Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. Lancet 1999, 354, 1257–1259. [Google Scholar] [CrossRef] [PubMed]
- Paton, N.I.; Leo, Y.S.; Zaki, S.R.; Auchus, A.P.; Lee, K.E.; Ling, A.E.; Chew, S.K.; Ang, B.; Rollin, P.E.; Umapathi, T.; et al. Outbreak of Nipah-virus infection among abattoir workers in Singapore. Lancet 1999, 354, 1253–1256. [Google Scholar] [CrossRef] [PubMed]
- Marsh, G.A.; De Jong, C.; Barr, J.A.; Tachedjian, M.; Smith, C.; Middleton, D.; Yu, M.; Todd, S.; Foord, A.J.; Haring, V.; et al. Cedar Virus: A Novel Henipavirus Isolated from Australian Bats. PLoS Pathog. 2012, 8, e1002836. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Yang, L.; Yang, F.; Ren, X.; Jiang, J.; Dong, J.; Sun, L.; Zhu, Y.; Zhou, H.; Jin, Q. Novel Henipa-like Virus, Mojiang Paramyxovirus, in Rats, China, 2012. Emerg. Infect. Dis. 2014, 20, 1064–1066. [Google Scholar] [CrossRef]
- Drexler, J.F.; Corman, V.M.; Müller, M.A.; Maganga, G.D.; Vallo, P.; Binger, T.; Gloza-Rausch, F.; Cottontail, V.M.; Rasche, A.; Yordanov, S.; et al. Bats host major mammalian paramyxoviruses. Nat. Commun. 2012, 3, 796. [Google Scholar] [CrossRef]
- Hayman, D.T.S.; Suu-Ire, R.; Breed, A.C.; McEachern, J.A.; Wang, L.; Wood, J.L.N.; Cunningham, A.A. Evidence of Henipavirus Infection in West African Fruit Bats. PLoS ONE 2008, 3, e2739. [Google Scholar] [CrossRef]
- Zhang, X.-A.; Li, H.; Jiang, F.-C.; Zhu, F.; Zhang, Y.-F.; Chen, J.-J.; Tan, C.-W.; Anderson, D.E.; Fan, H.; Dong, L.-Y.; et al. A Zoonotic Henipavirus in Febrile Patients in China. N. Engl. J. Med. 2022, 387, 470–472. [Google Scholar] [CrossRef]
- Halpin, K.; Young, P.L.; Field, H.E.; Mackenzie, J.S. Isolation of Hendra virus from pteropid bats: A natural reservoir of Hendra virus. J. Gen. Virol. 2000, 81, 1927–1932. [Google Scholar] [CrossRef]
- Anderson, D.E.; Islam, A.; Crameri, G.; Todd, S.; Islam, A.; Khan, S.U.; Foord, A.; Rahman, M.Z.; Mendenhall, I.H.; Luby, S.P.; et al. Isolation and Full-Genome Characterization of Nipah Viruses from Bats, Bangladesh. Emerg. Infect. Dis. 2019, 25, 166–170. [Google Scholar] [CrossRef]
- Chua, K.B.; Koh, C.L.; Hooi, P.S.; Wee, K.F.; Khong, J.H.; Chua, B.H.; Chan, Y.P.; Lim, M.E.; Lam, S.K. Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes Infect. 2002, 4, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.; Rogers, R.; Selvey, L.; Selleck, P.; Hyatt, A.; Gould, A.; Gleeson, L.; Hooper, P.; Westbury, H. A novel morbillivirus pneumonia of horses and its transmission to humans. Emerg. Infect. Dis. 1995, 1, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Selvey, L.A.; Wells, R.M.; McCormack, J.G.; Ansford, A.J.; Murray, K.; Rogers, R.J.; Lavercombe, P.S.; Selleck, P.; Sheridan, J.W. Infection of humans and horses by a newly described morbillivirus. Med. J. Aust. 1995, 162, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.J.; Douglas, I.C.; Baldock, F.C.; Glanville, R.J.; Seppanen, K.T.; Gleeson, L.J.; Selleck, P.N.; Dunn, K.J. Investigation of a second focus of equine morbillivirus infection in coastal Queensland. Aust. Vet. J. 1996, 74, 243–244. [Google Scholar] [CrossRef] [PubMed]
- Playford, E.G.; McCall, B.; Smith, G.; Slinko, V.; Allen, G.; Smith, I.; Moore, F.; Taylor, C.; Kung, Y.H.; Field, H. Human Hendra virus encephalitis associated with equine outbreak, Australia, 2008. Emerg. Infect. Dis. 2010, 16, 219–223. [Google Scholar] [CrossRef]
- Hanna, J.N.; McBride, W.J.; Brookes, D.L.; Shield, J.; Taylor, C.T.; Smith, I.L.; Craig, S.B.; Smith, G.A. Hendra virus infection in a veterinarian. Med. J. Aust. 2006, 185, 562–564. [Google Scholar] [CrossRef]
- Field, H.; Schaaf, K.; Kung, N.; Simon, C.; Waltisbuhl, D.; Hobert, H.; Moore, F.; Middleton, D.; Crook, A.; Smith, G.; et al. Hendra virus outbreak with novel clinical features, Australia. Emerg. Infect. Dis. 2010, 16, 338–340. [Google Scholar] [CrossRef]
- Eby, P.; Peel, A.J.; Hoegh, A.; Madden, W.; Giles, J.R.; Hudson, P.J.; Plowright, R.K. Pathogen spillover driven by rapid changes in bat ecology. Nature 2023, 613, 340–344. [Google Scholar] [CrossRef]
- Halpin, K.; Rota, P. A Review of Hendra Virus and Nipah Virus Infections in Man and Other Animals; Springer: Dordrecht, The Netherlands, 2015; pp. 997–1012. [Google Scholar]
- Wang, J.; Anderson, D.E.; Halpin, K.; Hong, X.; Chen, H.; Walker, S.; Valdeter, S.; Van Der Heide, B.; Neave, M.J.; Bingham, J.; et al. A new Hendra virus genotype found in Australian flying foxes. Virol. J. 2021, 18, 197. [Google Scholar] [CrossRef]
- Annand, E.J.; Horsburgh, B.A.; Xu, K.; Reid, P.A.; Poole, B.; De Kantzow, M.C.; Brown, N.; Tweedie, A.; Michie, M.; Grewar, J.D.; et al. Novel Hendra Virus Variant Detected by Sentinel Surveillance of Horses in Australia. Emerg. Infect. Dis. 2022, 28, 693–704. [Google Scholar] [CrossRef]
- Chua, K.B.; Bellini, W.J.; Rota, P.A.; Harcourt, B.H.; Tamin, A.; Lam, S.K.; Ksiazek, T.G.; Rollin, P.E.; Zaki, S.R.; Shieh, W.; et al. Nipah virus: A recently emergent deadly paramyxovirus. Science 2000, 288, 1432–1435. [Google Scholar] [CrossRef] [PubMed]
- Goh, K.J.; Tan, C.T.; Chew, N.K.; Tan, P.S.; Kamarulzaman, A.; Sarji, S.A.; Wong, K.T.; Abdullah, B.J.; Chua, K.B.; Lam, S.K. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N. Engl. J. Med. 2000, 342, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Parashar, U.D.; Sunn, L.M.; Ong, F.; Mounts, A.W.; Arif, M.T.; Ksiazek, T.G.; Kamaluddin, M.A.; Mustafa, A.N.; Kaur, H.; Ding, L.M.; et al. Case-Control Study of Risk Factors for Human Infection with a New Zoonotic Paramyxovirus, Nipah Virus, during a 1998–1999 Outbreak of Severe Encephalitis in Malaysia. J. Infect. Dis. 2000, 181, 1755–1759. [Google Scholar] [CrossRef]
- Sharma, V.; Kaushik, S.; Kumar, R.; Yadav, J.P.; Kaushik, S. Emerging trends of Nipah virus: A review. Rev. Med. Virol. 2019, 29, e2010. [Google Scholar] [CrossRef] [PubMed]
- Ang, B.S.P.; Lim, T.C.C.; Wang, L. Nipah Virus Infection. J. Clin. Microbiol. 2018, 56. [Google Scholar] [CrossRef] [PubMed]
- Gómez Román, R.; Wang, L.F.; Lee, B.; Halpin, K.; de Wit, E.; Broder, C.C.; Rahman, M.; Kristiansen, P.; Saville, M. Nipah@20: Lessons Learned from Another Virus with Pandemic Potential. mSphere 2020, 5. [Google Scholar] [CrossRef]
- Soman Pillai, V.; Krishna, G.; Valiya Veettil, M. Nipah Virus: Past Outbreaks and Future Containment. Viruses 2020, 12, 465. [Google Scholar] [CrossRef]
- Harcourt, B.H.; Tamin, A.; Ksiazek, T.G.; Rollin, P.E.; Anderson, L.J.; Bellini, W.J.; Rota, P.A. Molecular characterization of Nipah virus, a newly emergent paramyxovirus. Virology 2000, 271, 334–349. [Google Scholar] [CrossRef]
- Harcourt, B.H.; Lowe, L.; Tamin, A.; Liu, X.; Bankamp, B.; Bowden, N.; Rollin, P.E.; Comer, J.A.; Ksiazek, T.G.; Hossain, M.J.; et al. Genetic characterization of Nipah virus, Bangladesh, 2004. Emerg. Infect. Dis. 2005, 11, 1594–1597. [Google Scholar] [CrossRef]
- Hossain, M.J.; Gurley, E.S.; Montgomery, J.M.; Bell, M.; Carroll, D.S.; Hsu, V.P.; Formenty, P.; Croisier, A.; Bertherat, E.; Faiz, M.A.; et al. Clinical presentation of nipah virus infection in Bangladesh. Clin. Infect. Dis. 2008, 46, 977–984. [Google Scholar] [CrossRef]
- Ching, P.K.; de los Reyes, V.C.; Sucaldito, M.N.; Tayag, E.; Columna-Vingno, A.B.; Malbas, F.F., Jr.; Bolo, G.C., Jr.; Sejvar, J.J.; Eagles, D.; Playford, G.; et al. Outbreak of henipavirus infection, Philippines, 2014. Emerg. Infect. Dis. 2015, 21, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Arunkumar, G.; Chandni, R.; Mourya, D.T.; Singh, S.K.; Sadanandan, R.; Sudan, P.; Bhargava, B. Outbreak Investigation of Nipah Virus Disease in Kerala, India, 2018. J. Infect. Dis. 2019, 219, 1867–1878. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Nipah Virus Infection—Bangladesh. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON442 (accessed on 3 August 2023).
- Gurley, E.S.; Montgomery, J.M.; Hossain, M.J.; Bell, M.; Azad, A.K.; Islam, M.R.; Molla, M.A.; Carroll, D.S.; Ksiazek, T.G.; Rota, P.A.; et al. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg. Infect. Dis. 2007, 13, 1031–1037. [Google Scholar] [CrossRef]
- Homaira, N.; Rahman, M.; Hossain, M.J.; Epstein, J.H.; Sultana, R.; Khan, M.S.; Podder, G.; Nahar, K.; Ahmed, B.; Gurley, E.S.; et al. Nipah virus outbreak with person-to-person transmission in a district of Bangladesh, 2007. Epidemiol. Infect. 2010, 138, 1630–1636. [Google Scholar] [CrossRef]
- Chong, V.; Hossain, M.; Chong, H. Differences in epidemiologic and clinical features of Nipah virus encephalitis between the Malaysian and Bangladesh outbreaks. Neurol. Asia 2008, 13, 23–26. [Google Scholar]
- Bonaparte, M.I.; Dimitrov, A.S.; Bossart, K.N.; Crameri, G.; Mungall, B.A.; Bishop, K.A.; Choudhry, V.; Dimitrov, D.S.; Wang, L.-F.; Eaton, B.T.; et al. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proc. Natl. Acad. Sci. USA 2005, 102, 10652–10657. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Broder, C.C.; Nikolov, D.B. Ephrin-B2 and ephrin-B3 as functional henipavirus receptors. Semin. Cell Dev. Biol. 2012, 23, 116–123. [Google Scholar] [CrossRef]
- Negrete, O.A.; Wolf, M.C.; Aguilar, H.C.; Enterlein, S.; Wang, W.; Mühlberger, E.; Su, S.V.; Bertolotti-Ciarlet, A.; Flick, R.; Lee, B. Two Key Residues in EphrinB3 Are Critical for Its Use as an Alternative Receptor for Nipah Virus. PLoS Pathog. 2006, 2, e7. [Google Scholar] [CrossRef]
- Lee, B. Envelope–Receptor Interactions in Nipah Virus Pathobiology. Ann. N. Y. Acad. Sci. 2007, 1102, 51–65. [Google Scholar] [CrossRef]
- Eaton, T.B.; Broder, C.C.; Wang, L.-F. Hendra and Nipah Viruses: Pathogenesis and Therapeutics. Curr. Mol. Med. 2005, 5, 805–816. [Google Scholar] [CrossRef]
- Wong, K.T.; Grosjean, I.; Brisson, C.; Blanquier, B.; Fevre-Montange, M.; Bernard, A.; Loth, P.; Georges-Courbot, M.-C.; Chevallier, M.; Akaoka, H.; et al. A Golden Hamster Model for Human Acute Nipah Virus Infection. Am. J. Pathol. 2003, 163, 2127–2137. [Google Scholar] [CrossRef] [PubMed]
- Geisbert, T.W.; Feldmann, H.; Broder, C.C. Animal challenge models of henipavirus infection and pathogenesis. Curr. Top. Microbiol. Immunol. 2012, 359, 153–177. [Google Scholar] [CrossRef] [PubMed]
- de Wit, E.; Munster, V.J. Animal models of disease shed light on Nipah virus pathogenesis and transmission. J. Pathol. 2015, 235, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.T.; Robertson, T.; Ong, B.B.; Chong, J.W.; Yaiw, K.C.; Wang, L.F.; Ansford, A.J.; Tannenberg, A. Human Hendra virus infection causes acute and relapsing encephalitis. Neuropathol. Appl. Neurobiol. 2009, 35, 296–305. [Google Scholar] [CrossRef]
- Wong, K.T.; Shieh, W.J.; Kumar, S.; Norain, K.; Abdullah, W.; Guarner, J.; Goldsmith, C.S.; Chua, K.B.; Lam, S.K.; Tan, C.T.; et al. Nipah virus infection: Pathology and pathogenesis of an emerging paramyxoviral zoonosis. Am. J. Pathol. 2002, 161, 2153–2167. [Google Scholar] [CrossRef]
- Ong, K.C.; Wong, K.T. Henipavirus Encephalitis: Recent Developments and Advances. Brain Pathol. 2015, 25, 605–613. [Google Scholar] [CrossRef]
- Maisner, A.; Neufeld, J.; Weingartl, H. Organ- and endotheliotropism of Nipah virus infections in vivo and in vitro. Thromb. Haemost. 2009, 102, 1014–1023. [Google Scholar] [CrossRef]
- Wong, K.T.; Ong, K.C. Pathology of acute henipavirus infection in humans and animals. Pathol. Res. Int. 2011, 2011, 567248. [Google Scholar] [CrossRef]
- Sejvar, J.J.; Hossain, J.; Saha, S.K.; Gurley, E.S.; Banu, S.; Hamadani, J.D.; Faiz, M.A.; Siddiqui, F.M.; Mohammad, Q.D.; Mollah, A.H.; et al. Long-term neurological and functional outcome in Nipah virus infection. Ann. Neurol. 2007, 62, 235–242. [Google Scholar] [CrossRef]
- Tan, C.T.; Goh, K.J.; Wong, K.T.; Sarji, S.A.; Chua, K.B.; Chew, N.K.; Murugasu, P.; Loh, Y.L.; Chong, H.T.; Tan, K.S.; et al. Relapsed and late-onset Nipah encephalitis. Ann. Neurol. 2002, 51, 703–708. [Google Scholar] [CrossRef]
- Chong, H.; Tan, C. Relapsed and late-onset Nipah encephalitis, a report of three cases. Neurol. J. Southeast. Asia 2003, 8, 109–112. [Google Scholar]
- Abdullah, S.; Chang, L.; Rahmat, K.; Goh, K.; Tan, C. Late-onset Nipah virus encephalitis 11 years after the initial outbreak: A case report. Neurol. Asia 2012, 17, 71–74. [Google Scholar]
- Westbury, H.; Hooper, P.; Selleck, P.; Murray, P. Equine morbillivirus pneumonia: Susceptibility of laboratory animals to the virus. Aust. Vet. J. 1995, 72, 278–279. [Google Scholar] [CrossRef] [PubMed]
- Dups, J.; Middleton, D.; Yamada, M.; Monaghan, P.; Long, F.; Robinson, R.; Marsh, G.A.; Wang, L.F. A new model for Hendra virus encephalitis in the mouse. PLoS ONE 2012, 7, e40308. [Google Scholar] [CrossRef] [PubMed]
- Dups, J.; Middleton, D.; Long, F.; Arkinstall, R.; Marsh, G.A.; Wang, L.-F. Subclinical infection without encephalitis in mice following intranasal exposure to Nipah virus-Malaysia and Nipah virus-Bangladesh. Virol. J. 2014, 11, 102. [Google Scholar] [CrossRef]
- Dhondt, K.P.; Mathieu, C.; Chalons, M.; Reynaud, J.M.; Vallve, A.; Raoul, H.; Horvat, B. Type I interferon signaling protects mice from lethal henipavirus infection. J. Infect. Dis. 2013, 207, 142–151. [Google Scholar] [CrossRef]
- Welch, S.R.; Spengler, J.R.; Genzer, S.C.; Coleman-McCray, J.D.; Harmon, J.R.; Sorvillo, T.E.; Scholte, F.E.M.; Rodriguez, S.E.; O’Neal, T.J.; Ritter, J.M.; et al. Single-dose mucosal replicon-particle vaccine protects against lethal Nipah virus infection up to 3 days after vaccination. Sci. Adv. 2023, 9, eadh4057. [Google Scholar] [CrossRef]
- Edwards, S.J.; Rowe, B.; Reid, T.; Tachedjian, M.; Caruso, S.; Blasdell, K.; Watanabe, S.; Bergfeld, J.; Marsh, G.A. Henipavirus-induced neuropathogenesis in mice. Virology 2023, 587, 109856. [Google Scholar] [CrossRef]
- Iampietro, M.; Aurine, N.; Dhondt, K.P.; Dumont, C.; Pelissier, R.; Spanier, J.; Vallve, A.; Raoul, H.; Kalinke, U.; Horvat, B. Control of Nipah Virus Infection in Mice by the Host Adaptors Mitochondrial Antiviral Signaling Protein (MAVS) and Myeloid Differentiation Primary Response 88 (MyD88). J. Infect. Dis. 2020, 221, S401–S406. [Google Scholar] [CrossRef]
- Iampietro, M.; Dumont, C.; Mathieu, C.; Spanier, J.; Robert, J.; Charpenay, A.; Dupichaud, S.; Dhondt, K.P.; Aurine, N.; Pelissier, R.; et al. Activation of cGAS/STING pathway upon paramyxovirus infection. iScience 2021, 24, 102519. [Google Scholar] [CrossRef]
- Valbuena, G.; Halliday, H.; Borisevich, V.; Goez, Y.; Rockx, B. A Human Lung Xenograft Mouse Model of Nipah Virus Infection. PLoS Pathog. 2014, 10, e1004063. [Google Scholar] [CrossRef] [PubMed]
- Yun, T.; Park, A.; Hill, T.E.; Pernet, O.; Beaty, S.M.; Juelich, T.L.; Smith, J.K.; Zhang, L.; Wang, Y.E.; Vigant, F.; et al. Efficient Reverse Genetics Reveals Genetic Determinants of Budding and Fusogenic Differences between Nipah and Hendra Viruses and Enables Real-Time Monitoring of Viral Spread in Small Animal Models of Henipavirus Infection. J. Virol. 2015, 89, 1242–1253. [Google Scholar] [CrossRef] [PubMed]
- Guillaume, V.; Wong, K.T.; Looi, R.Y.; Georges-Courbot, M.C.; Barrot, L.; Buckland, R.; Wild, T.F.; Horvat, B. Acute Hendra virus infection: Analysis of the pathogenesis and passive antibody protection in the hamster model. Virology 2009, 387, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Dawes, B.E.; Kalveram, B.; Ikegami, T.; Juelich, T.; Smith, J.K.; Zhang, L.; Park, A.; Lee, B.; Komeno, T.; Furuta, Y.; et al. Favipiravir (T-705) protects against Nipah virus infection in the hamster model. Sci. Rep. 2018, 8, 7604. [Google Scholar] [CrossRef]
- Georges-Courbot, M.C.; Contamin, H.; Faure, C.; Loth, P.; Baize, S.; Leyssen, P.; Neyts, J.; Deubel, V. Poly(I)-Poly(C12U) but Not Ribavirin Prevents Death in a Hamster Model of Nipah Virus Infection. Antimicrob. Agents Chemother. 2006, 50, 1768–1772. [Google Scholar] [CrossRef]
- Freiberg, A.N.; Worthy, M.N.; Lee, B.; Holbrook, M.R. Combined chloroquine and ribavirin treatment does not prevent death in a hamster model of Nipah and Hendra virus infection. J. Gen. Virol. 2010, 91, 765–772. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Lambe, T.; Sebastian, S.; Bushmaker, T.; Fischer, R.; Feldmann, F.; Haddock, E.; Letko, M.; Avanzato, V.A.; Rissanen, I.; et al. A single-dose ChAdOx1-vectored vaccine provides complete protection against Nipah Bangladesh and Malaysia in Syrian golden hamsters. PLoS Neglected Trop. Dis. 2019, 13, e0007462. [Google Scholar] [CrossRef]
- Walpita, P.; Cong, Y.; Jahrling, P.B.; Rojas, O.; Postnikova, E.; Yu, S.; Johns, L.; Holbrook, M.R. A VLP-based vaccine provides complete protection against Nipah virus challenge following multiple-dose or single-dose vaccination schedules in a hamster model. NPJ Vaccines 2017, 2, 21. [Google Scholar] [CrossRef]
- Lo, M.K.; Spengler, J.R.; Welch, S.R.; Harmon, J.R.; Coleman-McCray, J.D.; Scholte, F.E.M.; Shrivastava-Ranjan, P.; Montgomery, J.M.; Nichol, S.T.; Weissman, D.; et al. Evaluation of a Single-Dose Nucleoside-Modified Messenger RNA Vaccine Encoding Hendra Virus-Soluble Glycoprotein Against Lethal Nipah virus Challenge in Syrian Hamsters. J. Infect. Dis. 2019, 221, S493–S498. [Google Scholar] [CrossRef]
- Monath, T.P.; Nichols, R.; Tussey, L.; Scappaticci, K.; Pullano, T.G.; Whiteman, M.D.; Vasilakis, N.; Rossi, S.L.; Campos, R.K.; Azar, S.R.; et al. Recombinant vesicular stomatitis vaccine against Nipah virus has a favorable safety profile: Model for assessment of live vaccines with neurotropic potential. PLoS Pathog. 2022, 18, e1010658. [Google Scholar] [CrossRef]
- Guillaume, V.; Contamin, H.; Loth, P.; Grosjean, I.; Courbot, M.C.G.; Deubel, V.; Buckland, R.; Wild, T.F. Antibody Prophylaxis and Therapy against Nipah Virus Infection in Hamsters. J. Virol. 2006, 80, 1972–1978. [Google Scholar] [CrossRef] [PubMed]
- Guillaume, V.; Contamin, H.; Loth, P.; Georges-Courbot, M.C.; Lefeuvre, A.; Marianneau, P.; Chua, K.B.; Lam, S.K.; Buckland, R.; Deubel, V.; et al. Nipah virus: Vaccination and passive protection studies in a hamster model. J. Virol. 2004, 78, 834–840. [Google Scholar] [CrossRef]
- Lo, M.K.; Bird, B.H.; Chattopadhyay, A.; Drew, C.P.; Martin, B.E.; Coleman, J.D.; Rose, J.K.; Nichol, S.T.; Spiropoulou, C.F. Single-dose replication-defective VSV-based Nipah virus vaccines provide protection from lethal challenge in Syrian hamsters. Antivir. Res. 2014, 101, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Yoneda, M.; Georges-Courbot, M.C.; Ikeda, F.; Ishii, M.; Nagata, N.; Jacquot, F.; Raoul, H.; Sato, H.; Kai, C. Recombinant measles virus vaccine expressing the Nipah virus glycoprotein protects against lethal Nipah virus challenge. PLoS ONE 2013, 8, e58414. [Google Scholar] [CrossRef] [PubMed]
- De Wit, E.; Bushmaker, T.; Scott, D.; Feldmann, H.; Munster, V.J. Nipah Virus Transmission in a Hamster Model. PLoS Neglected Trop. Dis. 2011, 5, e1432. [Google Scholar] [CrossRef]
- Rockx, B.; Brining, D.; Kramer, J.; Callison, J.; Ebihara, H.; Mansfield, K.; Feldmann, H. Clinical outcome of henipavirus infection in hamsters is determined by the route and dose of infection. J. Virol. 2011, 85, 7658–7671. [Google Scholar] [CrossRef]
- DeBuysscher, B.L.; de Wit, E.; Munster, V.J.; Scott, D.; Feldmann, H.; Prescott, J. Comparison of the Pathogenicity of Nipah Virus Isolates from Bangladesh and Malaysia in the Syrian Hamster. PLoS Neglected Trop. Dis. 2013, 7, e2024. [Google Scholar] [CrossRef]
- Escaffre, O.; Hill, T.; Ikegami, T.; Juelich, T.L.; Smith, J.K.; Zhang, L.; Perez, D.E.; Atkins, C.; Park, A.; Lawrence, W.S.; et al. Experimental Infection of Syrian Hamsters With Aerosolized Nipah Virus. J. Infect. Dis. 2018, 218, 1602–1610. [Google Scholar] [CrossRef]
- Ploquin, A.; Szécsi, J.; Mathieu, C.; Guillaume, V.; Barateau, V.; Ong, K.C.; Wong, K.T.; Cosset, F.-L.; Horvat, B.; Salvetti, A. Protection Against Henipavirus Infection by Use of Recombinant Adeno-Associated Virus–Vector Vaccines. J. Infect. Dis. 2012, 207, 469–478. [Google Scholar] [CrossRef]
- Yoneda, M.; Guillaume, V.; Sato, H.; Fujita, K.; Georges-Courbot, M.-C.; Ikeda, F.; Omi, M.; Muto-Terao, Y.; Wild, T.F.; Kai, C. The Nonstructural Proteins of Nipah Virus Play a Key Role in Pathogenicity in Experimentally Infected Animals. PLoS ONE 2010, 5, e12709. [Google Scholar] [CrossRef]
- Findlay-Wilson, S.; Flett, L.; Salguero, F.J.; Ruedas-Torres, I.; Fotheringham, S.; Easterbrook, L.; Graham, V.; Dowall, S. Establishment of a Nipah Virus Disease Model in Hamsters, including a Comparison of Intranasal and Intraperitoneal Routes of Challenge. Pathogens 2023, 12, 976. [Google Scholar] [CrossRef]
- Mathieu, C.; Guillaume, V.; Volchkova, V.A.; Pohl, C.; Jacquot, F.; Looi, R.Y.; Wong, K.T.; Legras-Lachuer, C.; Volchkov, V.E.; Lachuer, J.; et al. Nonstructural Nipah Virus C Protein Regulates both the Early Host Proinflammatory Response and Viral Virulence. J. Virol. 2012, 86, 10766–10775. [Google Scholar] [CrossRef] [PubMed]
- De Wit, E.; Prescott, J.; Falzarano, D.; Bushmaker, T.; Scott, D.; Feldmann, H.; Munster, V.J. Foodborne Transmission of Nipah Virus in Syrian Hamsters. PLoS Pathog. 2014, 10, e1004001. [Google Scholar] [CrossRef] [PubMed]
- Hooper, P.T.; Westbury, H.A.; Russell, G.M. The Lesions of Experimental Equine Morbillivirus Disease in Cats and Guinea Pigs. Vet. Pathol. 1997, 34, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Williamson, M.M.; Hooper, P.T.; Selleck, P.W.; Westbury, H.A.; Slocombe, R.F. A guinea-pig model of Hendra virus encephalitis. J. Comp. Pathol. 2001, 124, 273–279. [Google Scholar] [CrossRef]
- Williamson, M.M.; Hooper, P.T.; Selleck, P.W.; Westbury, H.A.; Slocombe, R.F. Experimental hendra virus infection in pregnant guinea-pigs and fruit Bats (Pteropus poliocephalus). J. Comp. Pathol. 2000, 122, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Embury-Hyatt, C.; Weingartl, H.M. Experimental inoculation study indicates swine as a potential host for Hendra virus. Vet. Res. 2010, 41, 33. [Google Scholar] [CrossRef] [PubMed]
- Middleton, D.J.; Morrissy, C.J.; van der Heide, B.M.; Russell, G.M.; Braun, M.A.; Westbury, H.A.; Halpin, K.; Daniels, P.W. Experimental Nipah virus infection in pteropid bats (Pteropus poliocephalus). J. Comp. Pathol. 2007, 136, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Torres-Velez, F.J.; Shieh, W.-J.; Rollin, P.E.; Morken, T.; Brown, C.; Ksiazek, T.G.; Zaki, S.R. Histopathologic and Immunohistochemical Characterization of Nipah Virus Infection in the Guinea Pig. Vet. Pathol. 2008, 45, 576–585. [Google Scholar] [CrossRef]
- Bossart, K.N.; Zhu, Z.; Middleton, D.; Klippel, J.; Crameri, G.; Bingham, J.; McEachern, J.A.; Green, D.; Hancock, T.J.; Chan, Y.-P. A neutralizing human monoclonal antibody protects against lethal disease in a new ferret model of acute nipah virus infection. PLoS Pathog. 2009, 5, e1000642. [Google Scholar] [CrossRef]
- Pallister, J.; Middleton, D.; Wang, L.-F.; Klein, R.; Haining, J.; Robinson, R.; Yamada, M.; White, J.; Payne, J.; Feng, Y.-R. A recombinant Hendra virus G glycoprotein-based subunit vaccine protects ferrets from lethal Hendra virus challenge. Vaccine 2011, 29, 5623–5630. [Google Scholar] [CrossRef] [PubMed]
- Pallister, J.A.; Klein, R.; Arkinstall, R.; Haining, J.; Long, F.; White, J.R.; Payne, J.; Feng, Y.-R.; Wang, L.-F.; Broder, C.C. Vaccination of ferrets with a recombinant G glycoprotein subunit vaccine provides protection against Nipah virus disease for over 12 months. Virol. J. 2013, 10, 237. [Google Scholar] [CrossRef] [PubMed]
- Leon, A.J.; Borisevich, V.; Boroumand, N.; Seymour, R.; Nusbaum, R.; Escaffre, O.; Xu, L.; Kelvin, D.J.; Rockx, B. Host gene expression profiles in ferrets infected with genetically distinct henipavirus strains. PLoS Neglected Trop. Dis. 2018, 12, e0006343. [Google Scholar] [CrossRef] [PubMed]
- Mire, C.E.; Chan, Y.-P.; Borisevich, V.; Cross, R.W.; Yan, L.; Agans, K.N.; Dang, H.V.; Veesler, D.; Fenton, K.A.; Geisbert, T.W.; et al. A Cross-Reactive Humanized Monoclonal Antibody Targeting Fusion Glycoprotein Function Protects Ferrets Against Lethal Nipah Virus and Hendra Virus Infection. J. Infect. Dis. 2020, 221, S471–S479. [Google Scholar] [CrossRef] [PubMed]
- Clayton, B.A.; Middleton, D.; Arkinstall, R.; Frazer, L.; Wang, L.-F.; Marsh, G.A. The Nature of Exposure Drives Transmission of Nipah Viruses from Malaysia and Bangladesh in Ferrets. PLoS Neglected Trop. Dis. 2016, 10, e0004775. [Google Scholar] [CrossRef] [PubMed]
- Clayton, B.A.; Middleton, D.; Bergfeld, J.; Haining, J.; Arkinstall, R.; Wang, L.; Marsh, G.A. Transmission Routes for Nipah Virus from Malaysia and Bangladesh. Emerg. Infect. Dis. 2012, 18, 1983–1993. [Google Scholar] [CrossRef]
- Pallister, J.; Middleton, D.; Crameri, G.; Yamada, M.; Klein, R.; Hancock, T.J.; Foord, A.; Shiell, B.; Michalski, W.; Broder, C.C.; et al. Chloroquine Administration Does Not Prevent Nipah Virus Infection and Disease in Ferrets. J. Virol. 2009, 83, 11979–11982. [Google Scholar] [CrossRef]
- Satterfield, B.A.; Borisevich, V.; Foster, S.L.; Rodriguez, S.E.; Cross, R.W.; Fenton, K.A.; Agans, K.N.; Basler, C.F.; Geisbert, T.W.; Mire, C.E. Antagonism of STAT1 by Nipah virus P gene products modulates disease course but not lethal outcome in the ferret model. Sci. Rep. 2019, 9, 16710. [Google Scholar] [CrossRef]
- Satterfield, B.A.; Cross, R.W.; Fenton, K.A.; Agans, K.N.; Basler, C.F.; Geisbert, T.W.; Mire, C.E. The immunomodulating V and W proteins of Nipah virus determine disease course. Nat. Commun. 2015, 6, 7483. [Google Scholar] [CrossRef]
- Satterfield, B.A.; Cross, R.W.; Fenton, K.A.; Borisevich, V.; Agans, K.N.; Deer, D.J.; Graber, J.; Basler, C.F.; Geisbert, T.W.; Mire, C.E. Nipah Virus C and W Proteins Contribute to Respiratory Disease in Ferrets. J. Virol. 2016, 90, 6326–6343. [Google Scholar] [CrossRef]
- Geisbert, T.W.; Daddario-DiCaprio, K.M.; Hickey, A.C.; Smith, M.A.; Chan, Y.P.; Wang, L.F.; Mattapallil, J.J.; Geisbert, J.B.; Bossart, K.N.; Broder, C.C. Development of an acute and highly pathogenic nonhuman primate model of Nipah virus infection. PLoS ONE 2010, 5, e10690. [Google Scholar] [CrossRef] [PubMed]
- Rockx, B.; Bossart, K.N.; Feldmann, F.; Geisbert, J.B.; Hickey, A.C.; Brining, D.; Callison, J.; Safronetz, D.; Marzi, A.; Kercher, L.; et al. A novel model of lethal Hendra virus infection in African green monkeys and the effectiveness of ribavirin treatment. J. Virol. 2010, 84, 9831–9839. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.N.; Woolsey, C.; Geisbert, J.B.; Agans, K.N.; Borisevich, V.; Deer, D.J.; Mire, C.E.; Cross, R.W.; Fenton, K.A.; Broder, C.C.; et al. Resistance of Cynomolgus Monkeys to Nipah and Hendra Virus Disease Is Associated with Cell-Mediated and Humoral Immunity. J. Infect. Dis. 2020, 221, S436–S447. [Google Scholar] [CrossRef] [PubMed]
- Stevens, C.S.; Lowry, J.; Juelich, T.; Atkins, C.; Johnson, K.; Smith, J.K.; Panis, M.; Ikegami, T.; tenOever, B.; Freiberg, A.N.; et al. Nipah Virus Bangladesh Infection Elicits Organ-Specific Innate and Inflammatory Responses in the Marmoset Model. J. Infect. Dis. 2023, 228, 604–614. [Google Scholar] [CrossRef] [PubMed]
- Woolsey, C.; Borisevich, V.; Fears, A.C.; Agans, K.N.; Deer, D.J.; Prasad, A.N.; O’Toole, R.; Foster, S.L.; Dobias, N.S.; Geisbert, J.B.; et al. Recombinant vesicular stomatitis virus-vectored vaccine induces long-lasting immunity against Nipah virus disease. J. Clin. Investig. 2023, 133, e164946. [Google Scholar] [CrossRef]
- Bossart, K.N.; Geisbert, T.W.; Feldmann, H.; Zhu, Z.; Feldmann, F.; Geisbert, J.B.; Yan, L.; Feng, Y.R.; Brining, D.; Scott, D.; et al. A neutralizing human monoclonal antibody protects african green monkeys from hendra virus challenge. Sci. Transl. Med. 2011, 3, 105ra103. [Google Scholar] [CrossRef]
- Mire, C.E.; Geisbert, J.B.; Agans, K.N.; Feng, Y.R.; Fenton, K.A.; Bossart, K.N.; Yan, L.; Chan, Y.P.; Broder, C.C.; Geisbert, T.W. A recombinant Hendra virus G glycoprotein subunit vaccine protects nonhuman primates against Hendra virus challenge. J. Virol. 2014, 88, 4624–4631. [Google Scholar] [CrossRef]
- Prasad, A.N.; Agans, K.N.; Sivasubramani, S.K.; Geisbert, J.B.; Borisevich, V.; Mire, C.E.; Lawrence, W.S.; Fenton, K.A.; Geisbert, T.W. A Lethal Aerosol Exposure Model of Nipah Virus Strain Bangladesh in African Green Monkeys. J. Infect. Dis. 2020, 221, S431–S435. [Google Scholar] [CrossRef]
- Lara, A.; Cong, Y.; Jahrling, P.B.; Mednikov, M.; Postnikova, E.; Yu, S.; Munster, V.; Holbrook, M.R. Peripheral immune response in the African green monkey model following Nipah-Malaysia virus exposure by intermediate-size particle aerosol. PLoS Negl. Trop. Dis. 2019, 13, e0007454. [Google Scholar] [CrossRef]
- Hammoud, D.A.; Lentz, M.R.; Lara, A.; Bohannon, J.K.; Feuerstein, I.; Huzella, L.; Jahrling, P.B.; Lackemeyer, M.; Laux, J.; Rojas, O.; et al. Aerosol exposure to intermediate size Nipah virus particles induces neurological disease in African green monkeys. PLoS Neglected Trop. Dis. 2018, 12, e0006978. [Google Scholar] [CrossRef]
- Cline, C.; Bell, T.M.; Facemire, P.; Zeng, X.; Briese, T.; Lipkin, W.I.; Shamblin, J.D.; Esham, H.L.; Donnelly, G.C.; Johnson, J.C.; et al. Detailed analysis of the pathologic hallmarks of Nipah virus (Malaysia) disease in the African green monkey infected by the intratracheal route. PLoS ONE 2022, 17, e0263834. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.C.; Briese, T.; Bell, T.M.; Pratt, W.D.; Shamblin, J.D.; Esham, H.L.; Donnelly, G.C.; Johnson, J.C.; Hensley, L.E.; Lipkin, W.I.; et al. Detailed Analysis of the African Green Monkey Model of Nipah Virus Disease. PLoS ONE 2015, 10, e0117817. [Google Scholar] [CrossRef] [PubMed]
- Cong, Y.; Lentz, M.R.; Lara, A.; Alexander, I.; Bartos, C.; Bohannon, J.K.; Hammoud, D.; Huzella, L.; Jahrling, P.B.; Janosko, K.; et al. Loss in lung volume and changes in the immune response demonstrate disease progression in African green monkeys infected by small-particle aerosol and intratracheal exposure to Nipah virus. PLoS Neglected Trop. Dis. 2017, 11, e0005532. [Google Scholar] [CrossRef]
- Mire, C.E.; Satterfield, B.A.; Geisbert, J.B.; Agans, K.N.; Borisevich, V.; Yan, L.; Chan, Y.P.; Cross, R.W.; Fenton, K.A.; Broder, C.C.; et al. Pathogenic Differences between Nipah Virus Bangladesh and Malaysia Strains in Primates: Implications for Antibody Therapy. Sci. Rep. 2016, 6, 30916. [Google Scholar] [CrossRef]
- Bossart, K.N.; Rockx, B.; Feldmann, F.; Brining, D.; Scott, D.; LaCasse, R.; Geisbert, J.B.; Feng, Y.-R.; Chan, Y.-P.; Hickey, A.C.; et al. A Hendra Virus G Glycoprotein Subunit Vaccine Protects African Green Monkeys from Nipah Virus Challenge. Sci. Transl. Med. 2012, 4, 146ra107. [Google Scholar] [CrossRef] [PubMed]
- Foster, S.L.; Woolsey, C.; Borisevich, V.; Agans, K.N.; Prasad, A.N.; Deer, D.J.; Geisbert, J.B.; Dobias, N.S.; Fenton, K.A.; Cross, R.W.; et al. A recombinant VSV-vectored vaccine rapidly protects nonhuman primates against lethal Nipah virus disease. Proc. Natl. Acad. Sci. USA 2022, 119, e2200065119. [Google Scholar] [CrossRef] [PubMed]
- de Wit, E.; Feldmann, F.; Cronin, J.; Goldin, K.; Mercado-Hernandez, R.; Williamson, B.N.; Meade-White, K.; Okumura, A.; Callison, J.; Weatherman, S.; et al. Distinct VSV-based Nipah virus vaccines expressing either glycoprotein G or fusion protein F provide homologous and heterologous protection in a nonhuman primate model. eBioMedicine 2023, 87, 104405. [Google Scholar] [CrossRef] [PubMed]
- Geisbert, J.B.; Borisevich, V.; Prasad, A.N.; Agans, K.N.; Foster, S.L.; Deer, D.J.; Cross, R.W.; Mire, C.E.; Geisbert, T.W.; Fenton, K.A. An Intranasal Exposure Model of Lethal Nipah Virus Infection in African Green Monkeys. J. Infect. Dis. 2020, 221, S414–S418. [Google Scholar] [CrossRef]
- Lo, M.K.; Feldmann, F.; Gary, J.M.; Jordan, R.; Bannister, R.; Cronin, J.; Patel, N.R.; Klena, J.D.; Nichol, S.T.; Cihlar, T.; et al. Remdesivir (GS-5734) protects African green monkeys from Nipah virus challenge. Sci. Transl. Med. 2019, 11, eaau9242. [Google Scholar] [CrossRef]
- Mire, C.E.; Geisbert, J.B.; Agans, K.N.; Versteeg, K.M.; Deer, D.J.; Satterfield, B.A.; Fenton, K.A.; Geisbert, T.W. Use of Single-Injection Recombinant Vesicular Stomatitis Virus Vaccine to Protect Nonhuman Primates Against Lethal Nipah Virus Disease. Emerg. Infect. Dis. 2019, 25, 1144–1152. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Avanzato, V.A.; Goldin, K.; Feldmann, F.; Schulz, J.E.; Haddock, E.; Okumura, A.; Lovaglio, J.; Hanley, P.W.; Cordova, K.; et al. ChAdOx1 NiV vaccination protects against lethal Nipah Bangladesh virus infection in African green monkeys. NPJ Vaccines 2022, 7, 171. [Google Scholar] [CrossRef] [PubMed]
- Marianneau, P.; Guillaume, V.; Wong, K.T.; Badmanathan, M.; Looi, R.Y.; Murri, S.; Loth, P.; Tordo, N.; Wild, T.F.; Horvat, B.; et al. Experimental Infection of Squirrel Monkeys with Nipah Virus. Emerg. Infect. Dis. J. 2010, 16, 507. [Google Scholar] [CrossRef] [PubMed]
- Mungall, B.A.; Middleton, D.; Crameri, G.; Bingham, J.; Halpin, K.; Russell, G.; Green, D.; McEachern, J.; Pritchard, L.I.; Eaton, B.T.; et al. Feline model of acute nipah virus infection and protection with a soluble glycoprotein-based subunit vaccine. J. Virol. 2006, 80, 12293–12302. [Google Scholar] [CrossRef] [PubMed]
- Hooper, P.T.; Ketterer, P.J.; Hyatt, A.D.; Russell, G.M. Lesions of Experimental Equine Morbillivirus Pneumonia in Horses. Vet. Pathol. 1997, 34, 312–322. [Google Scholar] [CrossRef] [PubMed]
- Marsh, G.; Haining, J.; Hancock, T.; Robinson, R.; Foord, A.; Barr, J.; Riddell, S.; Heine, H.; White, J.; Crameri, G.; et al. Experimental Infection of Horses with Hendra Virus/Australia/Horse/2008/Redlands. Emerg. Infect. Dis. 2011, 17, 2232–2238. [Google Scholar] [CrossRef]
- Halpin, K.; Graham, K.; Durr, P.A. Sero-Monitoring of Horses Demonstrates the Equivac® HeV Hendra Virus Vaccine to Be Highly Effective in Inducing Neutralising Antibody Titres. Vaccines 2021, 9, 731. [Google Scholar] [CrossRef]
- Chua, K.B. Nipah virus outbreak in Malaysia. J. Clin. Virol. 2003, 26, 265–275. [Google Scholar] [CrossRef]
- Middleton, D.J.; Westbury, H.A.; Morrissy, C.J.; van der Heide, B.M.; Russell, G.M.; Braun, M.A.; Hyatt, A.D. Experimental Nipah Virus Infection in Pigs and Cats. J. Comp. Pathol. 2002, 126, 124–136. [Google Scholar] [CrossRef]
- Weingartl, H.M.; Berhane, Y.; Caswell, J.L.; Loosmore, S.; Audonnet, J.-C.; Roth, J.A.; Czub, M. Recombinant Nipah Virus Vaccines Protect Pigs against Challenge. J. Virol. 2006, 80, 7929–7938. [Google Scholar] [CrossRef]
- Pickering, B.S.; Hardham, J.M.; Smith, G.; Weingartl, E.T.; Dominowski, P.J.; Foss, D.L.; Mwangi, D.; Broder, C.C.; Roth, J.A.; Weingartl, H.M. Protection against henipaviruses in swine requires both, cell-mediated and humoral immune response. Vaccine 2016, 34, 4777–4786. [Google Scholar] [CrossRef]
- Pedrera, M.; Macchi, F.; McLean, R.K.; Franceschi, V.; Thakur, N.; Russo, L.; Medfai, L.; Todd, S.; Tchilian, E.Z.; Audonnet, J.-C.; et al. Bovine Herpesvirus-4-Vectored Delivery of Nipah Virus Glycoproteins Enhances T Cell Immunogenicity in Pigs. Vaccines 2020, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Berhane, Y.; Weingartl, H.M.; Lopez, J.; Neufeld, J.; Czub, S.; Embury-Hyatt, C.; Goolia, M.; Copps, J.; Czub, M. Bacterial Infections in Pigs Experimentally Infected with Nipah Virus. Transbound. Emerg. Dis. 2008, 55, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Stachowiak, B.; Weingartl, H.M. Nipah Virus Infects Specific Subsets of Porcine Peripheral Blood Mononuclear Cells. PLoS ONE 2012, 7, e30855. [Google Scholar] [CrossRef] [PubMed]
- Weingartl, H.; Czub, S.; Copps, J.; Berhane, Y.; Middleton, D.; Marszal, P.; Gren, J.; Smith, G.; Ganske, S.; Manning, L.; et al. Invasion of the Central Nervous System in a Porcine Host by Nipah Virus. J. Virol. 2005, 79, 7528–7534. [Google Scholar] [CrossRef] [PubMed]
- Kasloff, S.B.; Leung, A.; Pickering, B.S.; Smith, G.; Moffat, E.; Collignon, B.; Embury-Hyatt, C.; Kobasa, D.; Weingartl, H.M. Pathogenicity of Nipah henipavirus Bangladesh in a swine host. Sci. Rep. 2019, 9, 5230. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, P.D.; Gabor, M.; Poe, I.; Neale, K.; Chaffey, K.; Finlaison, D.S.; Gu, X.; Hick, P.M.; Read, A.J.; Wright, T.; et al. Hendra Virus Infection in Dog, Australia, 2013. Emerg. Infect. Dis. 2015, 21, 2182–2185. [Google Scholar] [CrossRef]
- Middleton, D.; Riddell, S.; Klein, R.; Arkinstall, R.; Haining, J.; Frazer, L.; Mottley, C.; Evans, R.; Johnson, D.; Pallister, J. Experimental Hendra virus infection of dogs: Virus replication, shedding and potential for transmission. Aust. Vet. J. 2017, 95, 10–18. [Google Scholar] [CrossRef]
- Field, H.; Young, P.; Yob, J.M.; Mills, J.; Hall, L.; Mackenzie, J. The natural history of Hendra and Nipah viruses. Microbes Infect. 2001, 3, 307–314. [Google Scholar] [CrossRef]
- Mills, J.N.; Alim, A.N.M.; Bunning, M.L.; Lee, O.B.; Wagoner, K.D.; Amman, B.R.; Stockton, P.C.; Ksiazek, T.G. Nipah Virus Infection in Dogs, Malaysia, 1999. Emerg. Infect. Dis. 2009, 15, 950–952. [Google Scholar] [CrossRef]
- Hooper, P.; Zaki, S.; Daniels, P.; Middleton, D. Comparative pathology of the diseases caused by Hendra and Nipah viruses. Microbes Infect. 2001, 3, 315–322. [Google Scholar] [CrossRef]
- Westbury, H.; Hooper, P.; Brouwer, S.; Selleck, P. Susceptibility of cats to equine morbillivirus. Aust. Vet. J. 1996, 74, 132–134. [Google Scholar] [CrossRef] [PubMed]
- Williamson, M.; Hooper, P.; Selleck, P.; Gleeson, L.; Daniels, P.; Westbury, H.; Murray, P. Transmission studies of Hendra virus (equine morbilli-virus) in fruit bats, horses and cats. Aust. Vet. J. 1998, 76, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Mungall, B.A.; Middleton, D.; Crameri, G.; Halpin, K.; Bingham, J.; Eaton, B.T.; Broder, C.C. Vertical Transmission and Fetal Replication of Nipah Virus in an Experimentally Infected Cat. J. Infect. Dis. 2007, 196, 812–816. [Google Scholar] [CrossRef] [PubMed]


| Species (Age) | Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| C57BL/6 (aged) | HeV (Redlands/Horse/2008) | 5 × 104 TCID50 | i.n. | 100% (5/5) | Depression, ataxia, hypersensitivity, tremors | [56] |
| BALB/c (aged) | 60% (3/5) | |||||
| C57BL/6 (juvenile) | s.c. | None | None | |||
| BALB/c (juvenile) | ||||||
| C57BL/6 (aged) | NiV-B (human/2004/Rajbari, R1) | 5 × 104 TCID50 | i.n. | None | None | [57] |
| C57BL/6 (juvenile) | ||||||
| BALB/c (aged) | ||||||
| BALB/c (juvenile) | ||||||
| C57BL/6 (aged) | NiV-M (Malaysia/human/99) | 5 × 104 TCID50 | i.n. | None | None | |
| C57BL/6 (juvenile) | ||||||
| BALB/c (aged) | ||||||
| BALB/c (juvenile) | ||||||
| Unknown | HeV (prototype) | 5 × 103 TCID50 | s.c. | None | None | [55] |
| Swiss (juvenile) | HeV (prototype) | 6 × 105 PFU | i.n. | None | None | [43] |
| 1 × 107 PFU | i.p. | |||||
| C57BL/6 | NiV-M (UMMC1) | 1 × 106 PFU | i.p. | None | None | [58] |
| 1 × 105 PFU | i.c. | 100% (5/5) | Weight loss, aggressiveness, prostration, paralysis | [58] | ||
| Suckling Mice (2–3-day-old) | NiV-M | 1 × 100 TCID50 | i.c. | 15% (9–13) a | Clinical signs including weight loss b | [59] |
| 1 × 101 TCID50 | 66% (9–13) a | |||||
| 1 × 102 TCID50 | 100% (9–13) a | |||||
| 1 × 103 TCID50 | 100% (9–13) a | |||||
| 1 × 104 TCID50 | 100% (9–13) a | |||||
| 1 × 105 TCID50 | 100% (9–13) a | |||||
| 1 × 106 TCID50 | 100% (9–13) a | |||||
| BALB/c (13-week-old) | NiV-B (human/2004/Rajbari, R1) | 5 × 104 TCID50 | i.n. | None | None | [60] |
| rNiV-WT | None | |||||
| rNiV-FHeV | None | |||||
| rNiV-GHeV | None | |||||
| rNiV-MHeV | None | |||||
| HeV (Redlands/Horse/2008) | 5 × 104 TCID50 | i.n. | None | None | ||
| rHeV-WT | 40% (2/5) | Depression (2/5), increased respiration (2/5), hypersensitivity to stimuli (2/5), piloerection (1/5), hunched posture (1/5) | ||||
| rHeV-FNiV | None | None | ||||
| rHeV-GNiV | None | |||||
| rHeV-MNiV | None |
| Age | Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| 8–10-week-old | NiV-M | 1 × 104 TCID50 | i.p. | 80% (4/5) | Weight loss | [68] |
| HeV (prototype) | 1 × 104 TCID50 | i.p. | 100% (5/5) | Head tilt, weight loss, hypothermia, | ||
| 7-week-old | HeV (prototype) | 1 × 105 PFU | i.p. | 100% (6/6) | Paralysis, trembling limbs, breathing difficulties, serosanguinous nasal discharge | [65] |
| 1 × 104 PFU | 100% (6/6) | |||||
| 1 × 103 PFU | 100% (6/6) | |||||
| 1 × 102 PFU | 83% (5/6) | |||||
| 1 × 101 PFU | 67% (4/6) | |||||
| 1 × 100 PFU | None | None | ||||
| 11-week-old | 1.2 × 103 PFU | 80% (4/5) | Paralysis, trembling limbs, breathing difficulties, serosanguinous nasal discharge | |||
| 7-week-old | 1.2 × 103 PFU | 100% (5/5) | ||||
| 11-week-old | 1.2 × 104 PFU | 100% (5/5) | ||||
| 7-week-old | 1.2 × 104 PFU | 100% (5/5) | ||||
| 2-month-old | NiV-M | 6 × 105 PFU | i.n. | 100% (2/2) | Ataxia, imbalance | [43] |
| 1 × 107 PFU | i.p. | 100% (2/2) | ||||
| 7–14-week-old | 1 × 104 PFU | i.p. | 100% (6/6) | Tremors, limb paralysis | ||
| 1 × 103 PFU | 83% (5/6) | |||||
| 1 × 102 PFU | 67% (4/6) | |||||
| 1 × 101 PFU | None (0/6) | |||||
| 1 × 100 PFU | None (0/6) | |||||
| 7–14-week-old | 1 × 106 PFU | i.n. | 83% (5/6) | Imbalance, limb paralysis, lethargy, muscle twitching, breathing difficulties | ||
| 1 × 105 PFU | 83% (5/6) | |||||
| 1 × 104 PFU | 50% (3/6) | |||||
| 1 × 103 PFU | 50% (3/6) | |||||
| 1 × 102 PFU | None (0/6) | |||||
| 1 × 101 PFU | None (0/6) | |||||
| ~10-week-old a | NiV-M | 6.84 × 104 TCID50 | i.p. | 100% (10/10) | Severe clinical signs of disease, not described | [71] |
| ~10-week-old | NiV-M | 1 × 105 TCID50 | i.p. | 100% (3/3) | Neurological signs, respiratory distress | [75] |
| 8-week-old | NiV (unknown) | 2 × 103 TCID50 | i.p. | 90% (9/10) | Not described | [76] |
| Unknown | NiV-M b | 1 × 103 PFU | i.p. | 100% (unknown) | Not described | [74] |
| 6–8-week-old | NiV-M | 1 × 107 TCID50 | i.n. | 100% (14/14) c | Severe signs of disease, respiratory distress | [77] |
| 1 × 105 TCID50 | 67% (4/6) | Weight loss | ||||
| 1 × 103 TCID50 | 33% (2/6) | Weight loss, neurological signs | ||||
| 6-week-old | NiV-M | 1 × 105 TCID50 | i.n. | 100% (5/5) | Weight loss, severe acute respiratory distress | [78] |
| 1 × 102 TCID50 | 100% (5/5) | Weight loss, neurological signs (complete paralysis, seizure, muscle fasciculations) | ||||
| HeV (prototype) | 1 × 105 TCID50 | i.n. | 100% (5/5) | Weight loss, severe acute respiratory distress (labored breathing, serosanguineous oronasal exudates) | ||
| 1 × 102 TCID50 | 100% (5/5) | Weight loss, respiratory disease, neurological signs (complete paralysis, seizure, muscle fasciculations) | ||||
| 5–6-week-old | NiV-M | 1 × 105 TCID50 | i.p. | 100% (5/5) | Respiratory distress (labored breathing, hunched posture), neurological signs (one animal) | [79] |
| 1 × 104 TCID50 | 100% (5/5) | Respiratory distress (labored breathing, hunched posture) | ||||
| 1 × 103 TCID50 | 100% (5/5) | Neurological signs (imbalance, partial paralysis, seizure) | ||||
| 1 × 102 TCID50 | 60% (3/5) | Neurological signs (imbalance, partial paralysis, seizure) | ||||
| 1 × 101 TCID50 | None (0/5) | Neurological signs | ||||
| 1 × 100 TCID50 | None (0/5) | |||||
| 5–6-week-old | NiV-B | 1 × 105 TCID50 | i.p. | 80% (4/5) | Respiratory or neurological, both respiratory and neurological (one animal) | |
| 1 × 104 TCID50 | 80% (4/5) | Respiratory or neurological, both respiratory and neurological (one animal) | ||||
| 1 × 103 TCID50 | 60% (5/5) | Neurological signs | ||||
| 1 × 102 TCID50 | None (0/5) | |||||
| 1 × 101 TCID50 | 40% (2/5) | |||||
| 1 × 100 TCID50 | None (0/5) | |||||
| 5–6-week-old | NiV-M | 1 × 105 TCID50 | i.n. | 100% (5/5) | Not described | |
| 5–6-week-old | NiV-B | 1 × 105 TCID50 | 100% (5/5) | |||
| 4–5-week-old | NiV-M | 1 × 105 PFU | aerosol | 100% (5/5) | Weight loss, scruffy coat (3/5), Respiratory and neurological signs (2/5) | [80] |
| 2 × 104 TCID50 | 60% (3/5) | Neurological signs (3/5), Respiratory and neurological signs (2/5) | ||||
| 8 × 102 TCID50 | 80% (4/5) | Neurological signs (3/5), Respiratory and neurological signs (2/5) | ||||
| 2.5 × 102 TCID50 | 80% (4/5) | Neurological signs (3/5), Respiratory and neurological signs (2/5) | ||||
| 4–5-week-old | rNiV-FlucNP | 2 × 105 PFU | aerosol | 100% (5/5) | Weight loss, scruffy coat, labored breathing (4/5), Respiratory and neurological symptoms (1/5) | |
| 8.5 × 104 TCID50 | 100% (5/5) | Respiratory and neurological signs (4/5), weight loss | ||||
| 9.5 × 103 TCID50 | 100% (5/5) | Respiratory and neurological signs (4/5), weight loss, weight loss (1/5), respiratory only (1/5) | ||||
| 2.5 × 102 TCID50 | 60% (3/5) | Respiratory and neurological signs (2/5), weight loss, respiratory only (1/5) | ||||
| 6.6 × 101 TCID50 | 60% (3/5) | Respiratory and neurological signs (2/5), weight loss, respiratory only (1/5) | ||||
| Unknown | NiV-M (UMMC1) d | 1 × 104 PFU | i.p. | 100% (6/6) | Weight loss, dyspnea, tremor, paralysis | [81] |
| Unknown | HeV (prototype) d | 1 × 104 PFU | 100% (6/6) | Weight loss, dyspnea, tremor, paralysis | ||
| 8-week-old | rNiV(W-) e | 1 × 105 PFU | i.p. | 83% (5/6) | Neurological signs | [82] |
| 1 × 104 PFU | 83% (5/6) | |||||
| 1 × 103 PFU | 66% (4/6) | |||||
| 1 × 101 PFU | 50% (3/6) | |||||
| 1 × 100 PFU | 16% (1/6) | |||||
| 6–11-week-old | NiV-M | 1 × 105 TCID50 | i.n. | 100% (10/10) | Respiratory signs (dyspnea, wasp waist), ataxia (2/10) | [83] |
| 1 × 104 TCID50 | 100% (4/4) | Dyspnea (1/4), ataxia (2/4) | ||||
| NiV-M | 1 × 103 TCID50 | i.p. | 100% (8/8) | Neurological signs, ataxia (2/8), respiratory signs (2/8). | ||
| 1 × 102 TCID50 | 75% (3/4) | Neurological signs | ||||
| 8-week-old | NiV-M (UMMC1) | 1 × 102 PFU | i.p. | 100% Unknown f | Not described | [84] |
| 1 × 103 PFU | 100% Unknown f | |||||
| NiVΔC1 g | 1 × 102 PFU | i.p. | ~30–40% Unknown f | Not described | ||
| 1 × 103 PFU | ~80–90% Unknown f | |||||
| NiVΔC2 g | 1 × 102 PFU | i.p. | ~60% Unknown f | Not described | ||
| 1 × 103 PFU | ~70% Unknown f | |||||
| 5–7- week-old | NiV-M | 1 × 106 TCID50 | i.n. | 76% (~35/46) h | Clinical signs including weight loss i | [59] |
| 1 × 105 TCID50 | 50% Unknown | |||||
| 1 × 103 TCID50 | 12% Unknown | |||||
| 1 × 104 TCID50 | i.p. | 100% Unknown |
| Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|
| HeV (prototype) | 5 × 103 TCID50 | s.c. | 80% (4/5) | Respiratory distress, inappetence | [55] |
| 5 × 104 TCID50 | s.c. | 75% (9/12) | Weakness, lethargy, head tilt, depression, abortion (1/12) | [88] | |
| 3.4 × 106 PFU | i.n. | 33% (2/6) | Depression, inappetence, inactivity, weight loss, nasal hemorrhage (1/6) | [89] | |
| NiV-M | 6 × 105 PFU | i.n. | None | None | [43] |
| 1 × 107 PFU | i.p. | None | Transient fever and weight loss | ||
| 5 × 104 TCID50 | i.p. | 38% (3/8) | Ruffled fur, ataxia (1/8) | [90] | |
| 6 × 104 PFU | i.p. | 92% (24/26) | Severe clinical disease (features not described) | [91] |
| Virus (Isolate) | Dose | Route | Treatment | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| NiV-M (EUKK 19817) | 5 × 104 TCID50 | o.n. | N/A | 100% (2/2) | Severe depression, orthopnea, expiratory dyspnea, serous nasal discharge, cough, subcutaneous edema of the head | [92] |
| 5 × 103 TCID50 | 100% (2/2) | Severe depression, orthopnea, cutaneous ecchymoses, vomiting, hypothermia | ||||
| 5 × 102 TCID50 | 50% (1/2) | Obtundation, tremor, and hind limb paralysis | ||||
| 5 × 101 TCID50 | None (0/2) | None | ||||
| 5 × 103 TCID50 | PBS (IV) | 100% (2/2) | Weight loss, fever, depression, reduced play activity, subcutaneous edema of the head, cutaneous hemorrhages, inappetence (1/2), diarrhea (1/2), blood in the mouth (1/2) | |||
| mAb a (IV) | 66% (2/3) | Fever, depression, weight loss, reduced play activity, inappetence, diarrhea, crusting nasal discharge, hind limb paralysis (1/2), generalized tremor (1/3) | ||||
| HeV (Redlands 2008) | 5 × 104 TCID50 | o.n. | N/A | 100% (2/2) | Fever, depression, decreased grooming, generalized tremors | [93] |
| 5 × 103 TCID50 | 100% (2/2) | |||||
| 5 × 102 TCID50 | 100% (2/2) | |||||
| 5 × 101 TCID50 | 100% (2/2) | |||||
| 5 × 103 TCID50 | HeVsG 100 μg b | None (0/2) | None | |||
| HeVsG 20 μg b | None (0/2) | |||||
| HeVsG 4 μg b | 50% (1/2) | Reduced play activity, weakness, tremor | ||||
| CpG Adjuvant c | 100% (2/2) | Reduced play activity, fever, hind limb paralysis | ||||
| NiV-B (human/2004/Rajbari, R1) | 5 × 103 TCID50 | unknown | HeVsG 100 μg b,d | None (1/1) | None | [94] |
| HeVsG 20 μg b,d | None (2/2) | |||||
| HeVsG 4 μg b,d | None (1/1) | |||||
| HeVsG 100 μg b,e | None (1/1) | |||||
| HeVsG 20 μg b,e | None (1/1) | |||||
| HeVsG 4 μg b,e | None (2/2) | |||||
| CpG Adjuvant c | 100% (2/2) | Fever | ||||
| CpG Adjuvant c | 100% (2/2) | Fever, reduced playfulness | ||||
| NiV-M (patient isolate 1998 Malaysia outbreak) | 1 × 105 TCID50 | i.n. | N/A | 100% (4/4) | Labored breathing, fever, mild paralysis, generalized tremors, subcutaneous edema of head and neck, lack of grooming, hunched posture, ataxia, continuous licking, imbalance, myoclonus, head tilt, hind-limb paralysis, seizures | [95] |
| 1 × 103 TCID50 | 100% (4/4) | |||||
| 1 × 102 TCID50 | 100% (4/4) | |||||
| 1 × 101 TCID50 | 25% (1/4) | |||||
| NiV-B (2004 patient isolate) | 1 × 105 TCID50 | i.n. | N/A | 100% (4/4) | ||
| 1 × 103 TCID50 | 100% (4/4) | |||||
| 1 × 102 TCID50 | 75% (3/4) | |||||
| 1 × 101 TCID50 | 25% (1/4) | |||||
| HeV (prototype) | 1 × 105 TCID50 | i.n. | N/A | 100% (4/4) | ||
| 1 × 103 TCID50 | 100% (4/4) | |||||
| 1 × 102 TCID50 | 100% (4/4) | |||||
| 1 × 101 TCID50 | 75% (3/4) | |||||
| NiV-M (isolate 1999011924) | 5 × 103 PFU | i.n. | N/A | 100% (1/1) | Fever, facial edema, nasal and ocular discharge, sneezing, depression, loss of appetite, labored breathing, head and neck myoclonus | [96] |
| mAb f | None (0/3) | Fever (1/3) | ||||
| mAb g | None (0/3) | Fever (1/3), minor facial and ear twitching (1/3) | ||||
| HeV (prototype) | 5 × 103 PFU | i.n. | N/A | 100% (1/1) | Fever, nasal and ocular discharge, sneezing, loss of appetite, depression, facial edema, labored breathing | |
| mAb g | None (0/3) | Mild fever | ||||
| NiV-B (human/2004/Rajbari, R1) | 5 × 103 PFU | o.n. | N/A | 100% (4/4) | Fever, ataxia, agitation, facial edema, disorientation, tachypnea/dyspnea | [97] |
| contact h | 100% (4/4) | |||||
| NiV-M (Malaysia/Human/99) | 5 × 103 PFU | o.n. | N/A | 100% (4/4) | ||
| contact h | 100% (4/4) | |||||
| NiV-B (human/2004/Rajbari, R1) | 5 × 103 TCID50 | o.n. | N/A | 100% (8/8) | Hunched posture, agitation, sneezing, weight loss, licking, dehydration, vomiting, myoclonus of forelimbs, hindlimbs, flank, or tail, nasal discharge, facial edema, oral mucosa hemorrhage, ataxia, ventral neck edema, paralysis | [98] |
| NiV-M (Malaysia/Human/99) | 5 × 103 TCID50 | o.n. | N/A | 100% (6/6) i | Severe ataxia, facial and hind limb tremors, head tilt, torticollis, sneezing, nasal discharge, facial edema, hemorrhage of rectal mucosa, dyspnea, hemorrhage from nose and mouth, spastic paralysis of right forelimb, myoclonus of right trunk, extensive cutaneous petechial hemorrhage, hind limb paralysis, hunched posture, muscular fasciculation over flank, weight loss, recumbency | |
| NiV-M (EUKK 19817) | 5 × 103 TCID50 | o.n. | Vehicle control j | 100% (2/2) | Fever, depression, hind-limb paralysis, myoclonus, urinary incontinence, subcutaneous edema of neck and throat, cutaneous petechial hemorrhage, serosanguinous oral secretions | [99] |
| Antiviral k | 100% (3/3) | |||||
| Antiviral l | 100% (3/3) | |||||
| rNiVM-wt | 5 × 103 PFU | i.n. | N/A | 100% (5/5) | Fever, respiratory distress, lethargy, inappetence, depression, ocular, oral, and nasal discharge, ataxia, severe hypothermia, myoclonus, weight loss, hindlimb paresis, rales, hyperglycemia | [100] |
| rNiVM-PY166E | 5 × 103 PFU | i.n. | N/A | 100% (5/5) | Fever, depression, lethargy, inappetence, oral and nasal discharge, seizure, weight loss, aggressiveness, hyperglycemia, ataxia, hindlimb paresis | |
| rNiVM-PD116–135 | 5 × 103 PFU | i.n. | N/A | 100% (5/5) | Fever, depression, lethargy, inappetence, sneezing, myoclonus, facial tremor, nasal discharge, weight loss, hindlimb paresis, quadriparesis, hypothermia, seizure | |
| rNiVM-wt | 5 × 103 PFU | i.n. | N/A | 100% (5/5) | Depression, lethargy, inappetence, ocular and nasal discharge, myoclonus, ataxia, weight loss, sneezing, obtundation, nasal and oral frothing, facial edema, tremor | [101] |
| rNiVM-WKO | 5 × 103 PFU | i.n. | N/A | 100% (5/5) | Depression, lethargy, dehydration, sneezing, rales, nasal and oral frothing, severe ataxia, seizure, hypothermia, inappetence, hypersalivation, tremors, ocular and nasal discharge, obtundation | |
| rNiVM-VKO | 5 × 103 PFU | i.n. | N/A | None (0/5) | Lethargy, nasal discharge, depression, tremors, mild ataxia | |
| rNiVM-wt | 5 × 103 PFU | i.n. | N/A | 100% (5/5) | Depression, lethargy, inappetence, ocular and nasal discharge, ataxia, hindlimb myoclonus, tremors, nasal and oral frothing, facial edema, rales, hypothermia, sneezing, weight loss, obtundation | [102] |
| rNiVM-CKO | 5 × 103 PFU | i.n. | N/A | 100% (5/5) | Depression, lethargy, sneezing, ataxia, hypothermia, inappetence, myoclonus, rales, ocular and nasal discharge, weight loss | |
| rNiVM- CKOWKO | 5 × 103 PFU | i.n. | N/A | 60% (3/5) | Depression, lethargy, sneezing, nasal discharge, rales, hindlimb myoclonus and paralysis, severe tremors, seizures, weight loss, facial myoclonus, dilated pupils, facial edema, obtundation, severe hypothermia, visual deficit, aggressiveness |
| Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|
| HeV (prototype) | 4 × 105 TCID50 | i.t. | 100% (4/4) | Fever, severe respiratory distress (increased breathing rate, open mouth breathing), interstitial pneumonia (radiology) | [108] |
| 5 × 105 PFU | 100% (4/4) | Fever, depression, lethargy, inappetence, labored breathing, hind limb paralysis (1/4), dehydration | [109] | ||
| 4 × 105 TCID50 | 100% (3/3) | Nasal discharge, labored breathing | [104] | ||
| HeV (prototype) | 4 × 105 TCID50 | i.t. | 100% (9/9) a | Nasal discharge, labored breathing, seizure (1/9), muscle fasciculations (5/9) | |
| NiV-M | 1.3 × 106 PFU | i.t., oral | 100% (1/1) | Depression, lethargy, fever, inappetence, severe dyspnea, labored breathing | [103] |
| 7.0 × 103 PFU | None (0/1) | Depression, lethargy, fever, inappetence, severe dyspnea, labored breathing, nausea, lymphadenopathy, ecchymotic rash at the venipuncture site, muscle twitches, behavioral changes | |||
| 8.1 × 104 PFU | 100% (1/1) | Depression, lethargy, fever, inappetence, severe dyspnea, labored breathing, nausea, pleural effusions (X-ray) | |||
| 6.5 × 104 PFU | i.t. | 100% (1/1) | Depression, lethargy, fever, inappetence, labored breathing, pleural effusions (X-ray) | ||
| 5.9 × 104 PFU | 100% (1/1) | Depression, lethargy, inappetence, labored breathing, X-ray showed pleural effusions | |||
| 2.3 × 104 PFU | 100% (1/1) | Depression, lethargy, fever, inappetence, labored breathing, loss of balance, pleural effusions (X-ray) | |||
| 7.0 × 103 PFU | 100% (1/1) | Depression, lethargy, inappetence, labored breathing, pleural effusions (X-ray) | |||
| 2.5 × 103 PFU | 100% (1/1) | Depression, lethargy, inappetence, labored breathing, pleural effusions (X-ray) | |||
| NiV-B (isolate 200401066) | 8.81 × 102 PFU | aerosol | 100% (1/1) | Anorexia | [110] |
| 1.33 × 103 PFU | 100% (1/1) | Depression, lethargy, recumbency, anorexia, severe dyspnea, hypothermia | |||
| 9.95 × 103 PFU | 100% (1/1) | Depression, lethargy, anorexia, fever, severe dyspnea, pulmonary consolidation (X-ray) | |||
| 1.31 × 104 PFU | 100% (1/1) | Anorexia, mild dyspnea | |||
| NiV-M | ~64 × 101 PFU b | aerosol | 100% (3/3) | Weight loss, cough, lethargy, inappetence, pulmonary consolidation (CT scan), neutrophilia (2/6), anemia (2/6), monocytosis (2/6), lymphopenia (3/6), hypoalbuminemia, increased globulin, increased respiratory rate only on day of euthanasia | [111,112] |
| ~7 × 102 PFU b | 66% (2/3) | ||||
| NiV-M | 2.41 × 105 PFU | aerosol | 100% (4/4) | Decreased activity, labored breathing, increased respiratory rates, unresponsiveness, fever, continuous head twitch (1/4) | [113] |
| NiV-M | 2.5 × 104 PFU | i.t. | 50% (2/4) | Decreased responsiveness, tachypnea, fever, tachycardia, tachypnea (3/4), hypotension (2/4), hypothermia (2/4), tremors (1/4), bloody oronasal exudate (1/4), lymphadenopathy, weight loss (1/4) | [114] |
| NiV-M | 1.3 × 104 PFU | i.t. | 100% (3/3) | Lethargy, cough, breathing difficulty, inappetence | [115] |
| 4.03 × 104 PFU | aerosol | 100% (3/3) | |||
| NiV-M (isolate 199902916) | 5 × 105 PFU | i.t./i.n. | 50% (2/4) | Depression, lethargy (3/4), fever, inappetence, dyspnea, lymphopenia, thrombocytopenia, hypoalbuminemia, nasal exudate (3/4), tremors (2/4) | [116] |
| NiV-B (isolate 200401066) | 5 × 105 PFU | i.t./i.n. | 100% (4/4) | Fever (2/4), depression, inappetence, severe dyspnea, lymphopenia, thrombocytopenia, hypoalbuminemia, labored breathing (3/4), nasal exudate (2/4), with epistaxis (1/4), tremors (1/4) | |
| 100% (2/2) c | Fever, depression, lethargy, inappetence, severe dyspnea, labored breathing, nasal exudate with epistaxis (1/2) | ||||
| NiV-B (isolate 200401066) | 5 × 105 PFU | i.t./i.n. | 100% (6/6) | Aggressiveness, pulmonary edema (3/6), abdominal (3/6) or open mouth breathing (2/6), lethargy (4/6), depression (1/6), dyspnea (1/6), anorexia (3/6), recumbency (3/6), bradypnea (2/6), nasal exudate (1/6), hypothermia (1/6) | [105] |
| NiV-M (isolate 199902916) | 5 × 105 PFU | i.t./i.n. | 50% (1/2) | Depression, abdominal breathing, anorexia (1/2), lethargy (1/2), recumbency (1/2), nasal exudates, pulmonary consolidation (x-ray, 1/2), tremors (1/2) | |
| HeV-prototype (isolate 9409-30-1800) | 5 × 105 PFU | i.t./i.n. | 80% (4/5) | Anorexia (2/5), abdominal breathing (2/5), severe bradypnea (1/5), lethargy (1/5), dyspnea (1/5), mild tachypnea (1/5), pulmonary edema (1/5), depression (1/5) | |
| NiV-M | 1 × 105 TCID50 | i.t. | 100% (1/1) d | Anorexia, depression, decreased activity, hunched posture, increase in respiratory rate, acute respiratory distress, decrease in platelet count | [117] |
| NiV-B (isolate 200401066) | 5 × 105 PFU | i.t./i.n. | 100% (6/6) e | Increased respiration rates, tachypnea, dyspnea, depression | [118] |
| NiV (unknown isolate/strain) | 1 × 108 TCID50 | i.n./oral | None (0/1) | Weight loss, severe illness | [76] |
| 1 × 106 TCID50 | None (0/1) | ||||
| 1 × 108 TCID50 | i.p. | 100% (1/1) | Weight loss, severe depression, anorexia, decreased activity | ||
| 1 × 106 TCID50 | 100% (1/1) | ||||
| NiV-M (isolate 199901924) | 1 × 105 TCID50 | i.t./i.n. | 100% (2/2) e | Clinical signs not described | [119] |
| NiV-B (isolate 200401066) | 1 × 105 TCID50 | i.t./i.n. | 100% (2/2) e | Clinical signs not described |
| Species | Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| Cynomolgus Macaque | NiV-B (isolate 200401066) | 5 × 105 PFU | i.t./i.n. | None (0/3) | Pulmonary edema, abdominal breathing, fever (2/3), lymphadenitis (1/3) | [105] |
| NiV-M (isolate 199902916) | None (0/3) | None | ||||
| HeV (prototype) | None (0/2) | Agitation (1/2), increased aggressiveness (1/2), abdominal breathing (1/2) | ||||
| Common Marmoset | NiV-B (isolate 200401066) | 6.33 × 104 PFU | i.t./i.n. | 100% (4/4) | Hyperventilation (4/4), anorexia (3/4), lethargy (2/4), open mouth breathing (1/4), hunched posture (1/4), hindlimb tremors (1/4) | [106] |
| Squirrel Monkey | NiV-M (UMMC1) | 1 × 103 PFU | i.v. | 100% (2/2) | Uncoordinated motor movements, prostration, coma | [124] |
| 1 × 107 PFU | 50% (1/2) | Uncoordinated motor movements, prostration, coma, anorexia, depression | ||||
| 1 × 103 PFU | i.n. | None (0/0) | Anorexia, seizure | |||
| 1 × 107 PFU | None (0/0) | Anorexia, seizure, ocular edema |
| Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|
| HeV (prototype) | N/A a | i.v./i.n. | 100% (2/2) | Fever, weakness, labored breathing, agitation | [126] |
| 2 × 107 TCID50 | i.v./i.n. aerosol | 100% (2/2) | Mild temperature increase, labored breathing, depression | ||
| HeV (Australia/Horse/2008/Redlands) | 2 × 106 TCID50 | o.n. | 100% (3/3) | Increased heart rate, depression, anorexia, serous nasal discharge, dyspnea, agitation, irritability, panting respiration | [127] |
| Species (Age) | Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| Landrace | HeV (prototype) | 6.6 × 107 PFU | o.n. | 100% (2/2) | Fever, inappetence, severe depression, respiratory distress, recumbency | [89] |
| Gottingen Minipigs | HeV (prototype) | 2.0 × 107 PFU | i.n. | N/A a (0/5) | Fever (1/5), mild depression, cough, respiratory distress, transient neurological signs | |
| Landrace (7–8-week-old) | NiV-M b | 2.5 × 105 PFU | i.n. | N/A a (0/4) | Fever, lethargy, labored breathing (1/4), cough (1/4), unwilling to stand (1/4) | [131] |
| Landrace (9-week-old) c | NiV-M b | 5 × 105 PFU | i.n. | None (0/2) | Mild temperature increase | [132] |
| Landrace (9-week-old) c | HeV (prototype) | 5 × 105 PFU | i.n. | None (0/1) | Mild temperature increase | |
| Landrace (4-week-old) | NiV-M (human isolate) | 2.5 × 105 PFU | o.n. | 16% (1/6) | Transient temperature increase, exudative epidermitis (1/6), mild to severe depression (3/6), shivering, unwilling to stand (3/6), inappetence, shiver, hunched posture (2/4), cough (2/6), increased respiratory rate | [134] |
| Landrace (4–6-week-old) | NiV-M b | 2.5 × 105 PFU | i.n. | 31% (5/16) | Not described | [135] |
| Conventional (6-week-old) | NiV-M | 5 × 103 TCID50 | s.c. | 66% (2/3) | Loss of consciousness, lateral recumbency, ataxia, unwillingness to stand, muscle fasciculations, nasal discharge, shivering, persistent cough upon stimulation, mild increase in temperature | [130] |
| oral | None (0/3) | No signs attributed to NiV infection | ||||
| Landrace (4-week-old) | NiV-M (human isolate) | 2.5 × 105 PFU | o.n. + ocular | 18% (2/11) d | Wide stance, difficulty standing, unsteady balance, restless, lethargy, unwilling to walk, sawhorse stance, depression, severe shivering, seizure | [136] |
| Landrace (5–6-week-old) | rNiV-B e | 2.5 × 105 PFU | o.n. | None (0/10) | None | [137] |
| Species (Age) | Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| Unknown | HeV (prototype) | 5 × 103 TCID50 | s.c. | None (0/2) | None | [55] |
| Beagle (5–8-month-old) | HeV (Australia/Horse/2008/Redlands) | 2 × 106 TCID50 | o.n. | None (0/6) | Mild inappetence, mild conjunctivitis, tonsillar hyperplasia, transient mild temperature increase | [139] |
| Species (Age) | Virus (Isolate) | Dose | Route | % Lethality | Clinical Disease | Reference |
|---|---|---|---|---|---|---|
| Domestic shorthair cat (12–24-month-old) | NiV-M | 5 × 103 TCID50 | s.c. | 100% (2/2) | Fever, increased respiratory rate, inappetence, depression | [125] |
| 5 × 102 TCID50 | 100% (4/4) | |||||
| Domestic shorthair cat | NiV-M | 5 × 103 TCID50 | o.n. | 50% (1/2) | Fever, depression, increased respiratory rates, vomiting, decreased grooming, dyspnea, open mouth breathing | [130] |
| Unknown | HeV (prototype) | 5 × 103 TCID50 | s.c. | 100% (2/2) | Inappetence, increased respiratory rate | [55] |
| Unknown | HeV (prototype) | 5 × 104 TCID50 | o.r. | 100% (2/2) | Open mouth breathing, dyspnea | [144] |
| Unknown (8-month-old) | HeV (prototype) | 1 × 103.6 TCID50 | o.r. | 100% (2/2) | Depression, fever, increased respiratory rate | [143] |
| i.n. | 100% (2/2) | |||||
| s.c. | 100% (2/2) | |||||
| N/A | Contact a | 50% (1/2) | ||||
| Unknown | HeV (prototype) | 5 × 103 TCID50 | s.c. | 100% (2/2) | Not described | [86] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pigeaud, D.D.; Geisbert, T.W.; Woolsey, C. Animal Models for Henipavirus Research. Viruses 2023, 15, 1980. https://doi.org/10.3390/v15101980
Pigeaud DD, Geisbert TW, Woolsey C. Animal Models for Henipavirus Research. Viruses. 2023; 15(10):1980. https://doi.org/10.3390/v15101980
Chicago/Turabian StylePigeaud, Declan D., Thomas W. Geisbert, and Courtney Woolsey. 2023. "Animal Models for Henipavirus Research" Viruses 15, no. 10: 1980. https://doi.org/10.3390/v15101980





