Features of SARS-CoV-2 Replication in Various Types of Reptilian and Fish Cell Cultures
Abstract
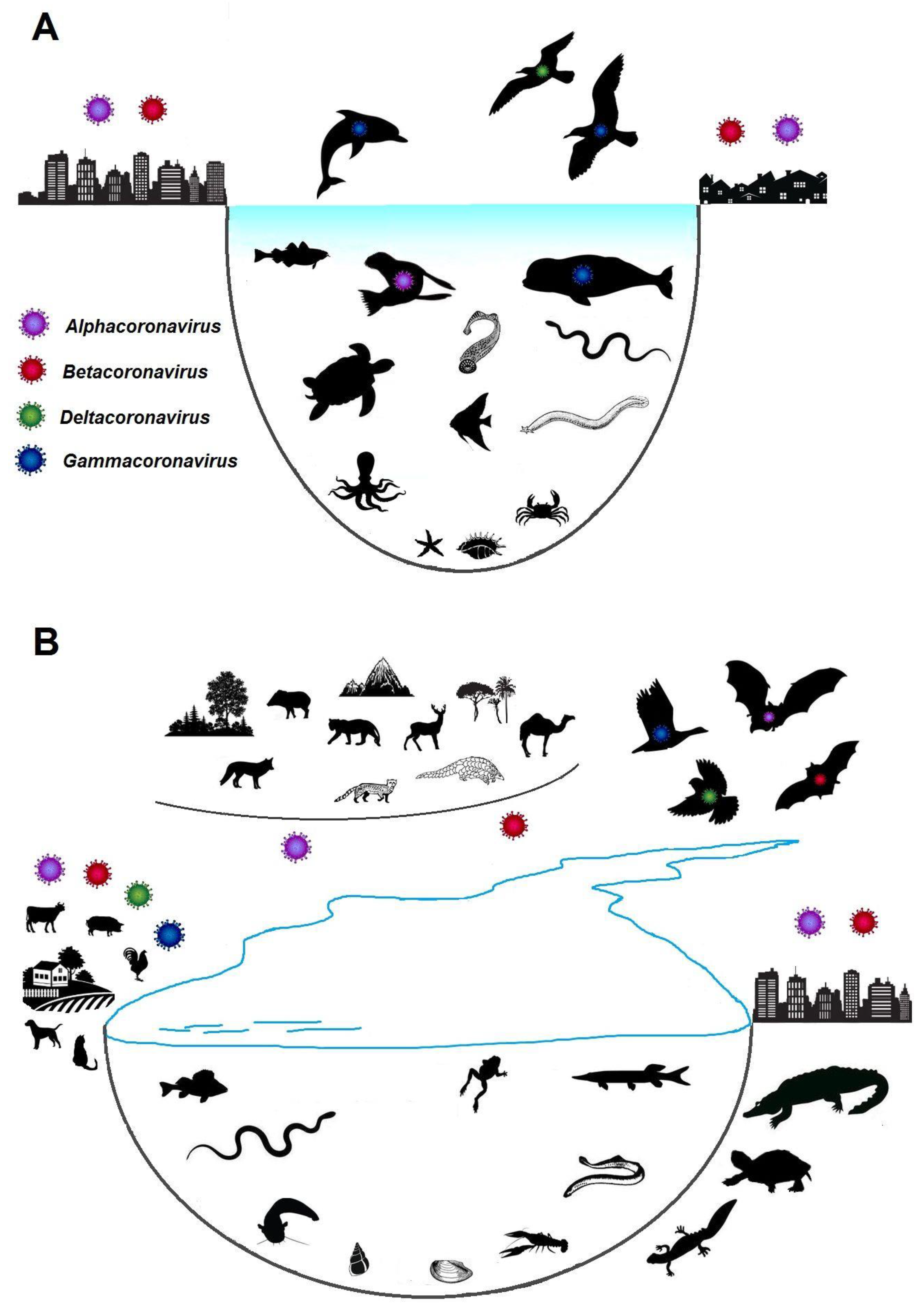
:1. Introduction
2. Materials and Methods
2.1. Virus
2.2. Cell Cultures
2.3. Infection
2.4. Study of SARS-CoV-2 Infection in Cell Cultures
3. Results
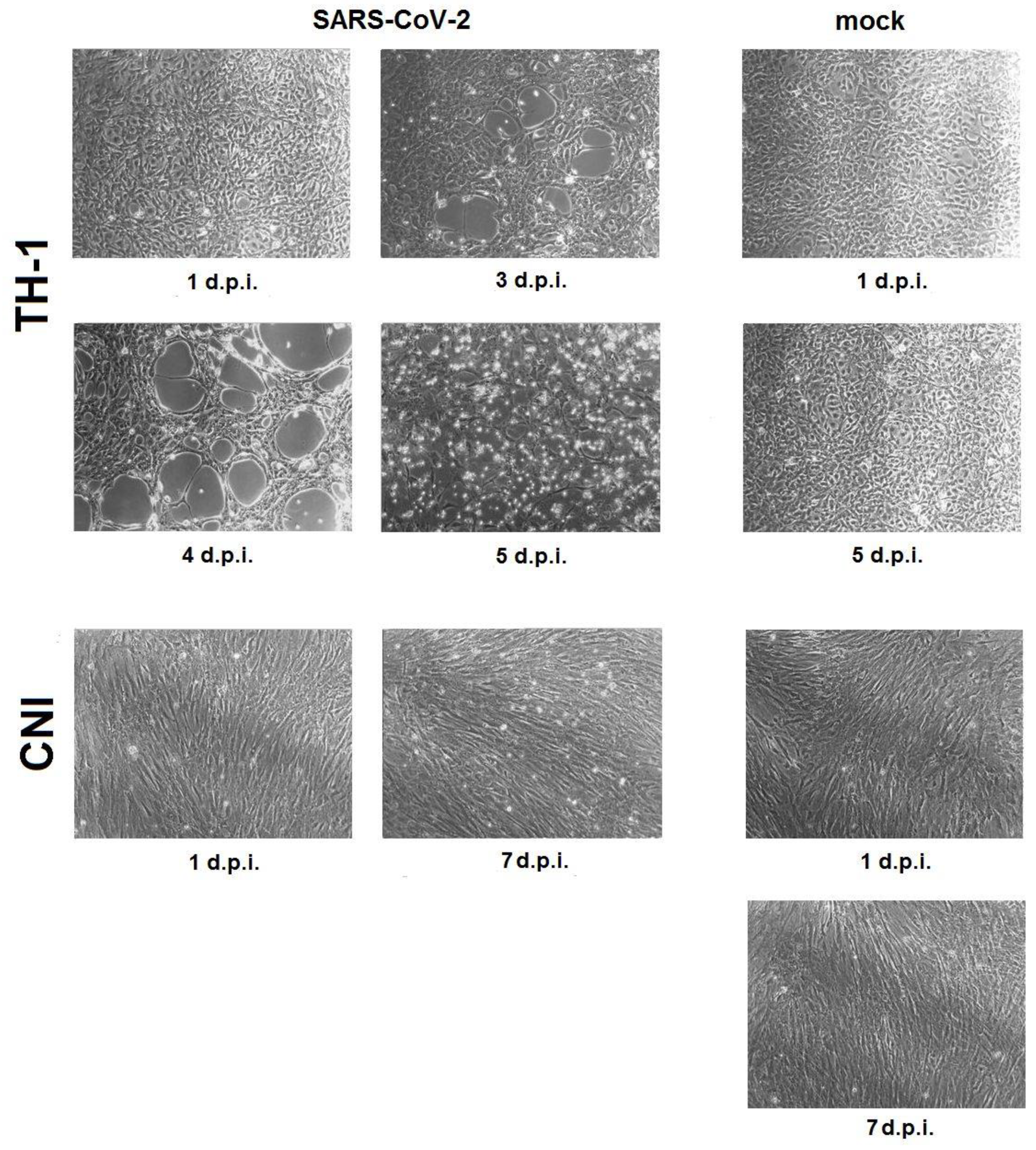
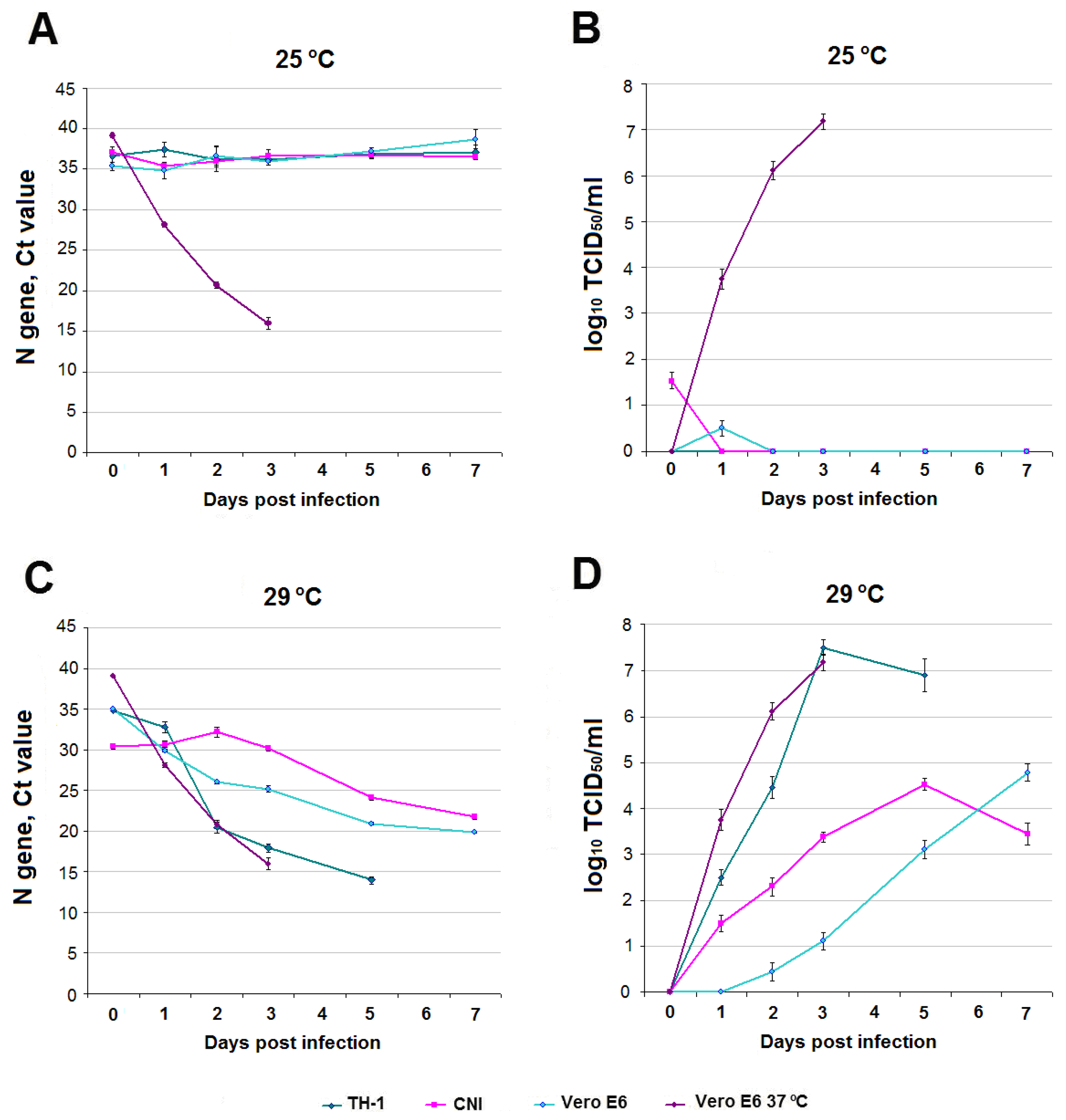
3.1. SARS-CoV-2 Infection in Reptile Cell Cultures
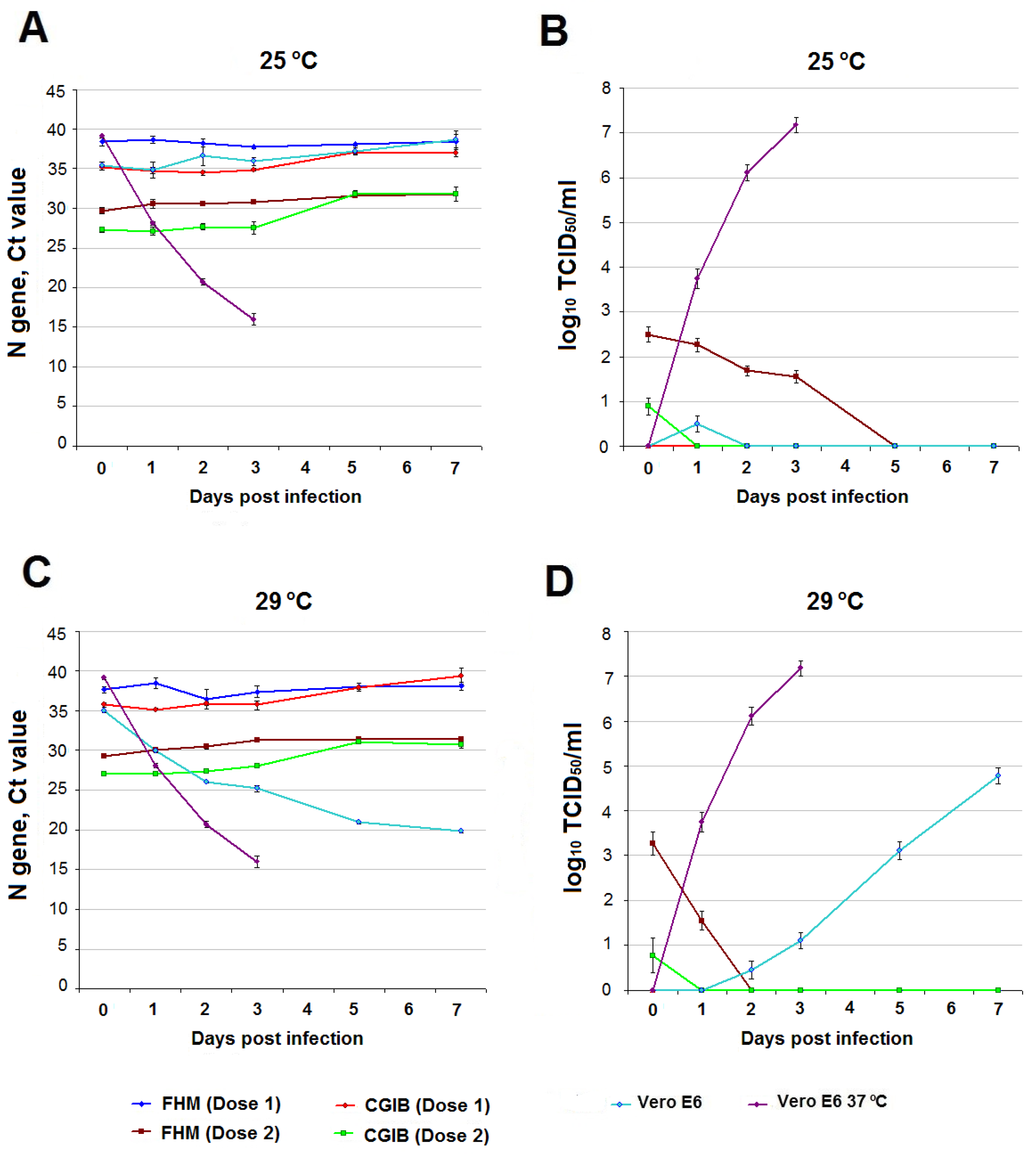
3.2. SARS-CoV-2 Infection in Fish Cell Cultures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ji, W.; Wang, W.; Zhao, X.; Zai, J.; Li, X. Cross-species Transmission of the Newly Identified Coronavirus 2019-nCoV. J. Med. Virol. 2020, 92, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.R.; Cao, Q.D.; Hong, Z.S.; Tan, Y.Y.; Chen, S.D.; Jin, H.J.; Tan, K.S.; Wang, D.Y.; Yan, Y. The Origin, Transmission and Clinical Therapies on Coronavirus Disease 2019 (COVID-19) Outbreak—An Update on the Status. Mil. Med. Res. 2020, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Nie, J.; Li, Q.; Zhang, L.; Cao, Y.; Zhang, Y.; Li, T.; Wu, J.; Liu, S.; Zhang, M.; Zhao, C.; et al. Functional Comparison of SARS-CoV-2 with Closely Related Pangolin and Bat Coronaviruses. Cell Discov. 2021, 7, 21. [Google Scholar] [CrossRef]
- Liu, W.J.; Liu, P.; Lei, W.; Jia, Z.; He, X.; Shi, W.; Tan, Y.; Zou, S.; Wong, G.; Wang, J.; et al. Surveillance of SARS-CoV-2 at the Huanan Seafood Market. Nature 2023. [Google Scholar] [CrossRef]
- Canuti, M.; Bianchi, S.; Kolbl, O.; Pond, S.L.K.; Kumar, S.; Gori, M.; Fappani, C.; Colzani, D.; Borghi, E.; Zuccotti, G.; et al. Waiting for the Truth: Is Reluctance in Accepting an Early Origin Hypothesis for SARS-CoV-2 Delaying our Understanding of Viral Emergence? BMJ Glob. Health 2022, 7, e008386. [Google Scholar] [CrossRef] [PubMed]
- Voskarides, K. SARS-CoV-2: Tracing the Origin, Tracking the Evolution. BMC Med. Genom. 2022, 15, 62. [Google Scholar] [CrossRef] [PubMed]
- Qiu, X.; Liu, Y.; Sha, A. SARS-CoV-2 and Natural Infection in Animals. J. Med. Virol. 2023, 95, e28147. [Google Scholar] [CrossRef]
- Cui, X.; Wang, Y.; Zhai, J.; Xue, M.; Zheng, C.; Yu, L. Future Trajectory of SARS-CoV-2: Constant Spillover Back and Forth between Humans and Animals. Virus Res. 2023, 328, 199075. [Google Scholar] [CrossRef]
- World Organisation for Animal Health. SARS-CoV-2 in Animals—Situation Report 22. Available online: https://www.woah.org/app/uploads/2023/07/sars-cov-2-situation-report-22.pdf (accessed on 5 November 2023).
- Yen, H.L.; Sit, T.H.C.; Brackman, C.J.; Chuk, S.S.Y.; Gu, H.; Tam, K.W.S.; Law, P.Y.T.; Leung, G.M.; Peiris, M.; Poon, L.L.M. Transmission of SARS-CoV-2 Delta Variant (AY.127) from Pet Hamsters to Humans, Leading to Onward Human-to-Human Transmission: A Case Study. Lancet 2022, 399, 1070–1078. [Google Scholar] [CrossRef]
- Oude Munnink, B.B.; Sikkema, R.S.; Nieuwenhuijse, D.F.; Molenaar, R.J.; Munger, E.; Molenkamp, R.; van der Spek, A.; Tolsma, P.; Rietveld, A.; Brouwer, M.; et al. Transmission of SARS-CoV-2 on Mink Farms between Humans and Mink and Back to Humans. Science 2021, 371, 172–177. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, L.; Deng, Q.; Zhang, G.; Wu, K.; Ni, L.; Yang, Y.; Liu, B.; Wang, W.; Wei, C.; et al. The Presence of SARS-CoV-2 RNA in the Feces of COVID-19 Patients. J. Med. Virol. 2020, 92, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Liu, J.; Xu, W.; Luo, Q.; Chen, D.; Lei, Z.; Huang, Z.; Li, X.; Deng, K.; Lin, B.; et al. SARS-CoV-2 Can be Detected in Urine, Blood, Anal Swabs, and Oropharyngeal Swabs Specimens. J. Med. Virol. 2020, 92, 1676–1680. [Google Scholar] [CrossRef] [PubMed]
- Amirian, E.S. Potential Fecal Transmission of SARS-CoV-2: Current Evidence and Implications for Public Health. Int. J. Infect Dis. 2020, 95, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Han, B.; Wang, J. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission. Gastroenterology 2020, 158, 1518–1519. [Google Scholar] [CrossRef] [PubMed]
- Lodder, W.; de Roda Husman, A.M. SARS-CoV-2 in Wastewater: Potential Health Risk, but also Data Source. Lancet Gastroenterol. Hepatol. 2020, 5, 533–534. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Hu, J.; Hou, Y.; Tao, Z.; Chen, Z.; Chen, K. Pit Latrines may be a Potential Risk in Rural China and Low-income Countries when Dealing with COVID-19. Sci. Total Environ. 2021, 761, 143283. [Google Scholar] [CrossRef] [PubMed]
- Xiao, F.; Sun, J.; Xu, Y.; Li, F.; Huang, X.; Li, H.; Zhao, J.; Huang, J.; Zhao, J. Infectious SARS-CoV-2 in Feces of Patient with Severe COVID-19. Emerg. Infect Dis. 2020, 26, 1920–1922. [Google Scholar] [CrossRef]
- Dergham, J.; Delerce, J.; Bedotto, M.; La Scola, B.; Moal, V. Isolation of Viable SARS-CoV-2 Virus from Feces of an Immunocompromised Patient Suggesting a Possible Fecal Mode of Transmission. J. Clin. Med 2021, 10, 2696. [Google Scholar] [CrossRef]
- Sun, J.; Zhu, A.; Li, H.; Zheng, K.; Zhuang, Z.; Chen, Z.; Shi, Y.; Zhang, Z.; Chen, S.B.; Liu, X.; et al. Isolation of Infectious SARS-CoV-2 from Urine of a COVID-19 Patient. Emerg. Microbes Infect. 2020, 9, 991–993. [Google Scholar] [CrossRef]
- Jeong, H.W.; Kim, S.M.; Kim, H.S.; Kim, Y.I.; Kim, J.H.; Cho, J.Y.; Kim, S.H.; Kang, H.; Kim, S.G.; Park, S.J.; et al. Viable SARS-CoV-2 in Various Specimens from COVID-19 Patients. Clin. Microbiol. Infect. 2020, 26, 1520–1524. [Google Scholar] [CrossRef]
- Sobsey, M.D. Absence of Virological and Epidemiological Evidence that SARS-CoV-2 Poses COVID-19 Risks from Environmental Fecal Waste, Wastewater and Water Exposures. J. Water Health 2022, 20, 126–138. [Google Scholar] [CrossRef]
- Amahmid, O.; El Guamri, Y.; Rakibi, Y.; Ouizat, S.; Yazidi, M.; Razoki, B.; Kaid Rassou, K.; Asmama, S.; Bouhoum, K.; Belghyti, D. Occurrence of SARS-CoV-2 in Excreta, Sewage, and Environment: Epidemiological Significance and Potential Risks. Int. J. Environ. Health Res. 2021, 23, 1686–1706. [Google Scholar] [CrossRef] [PubMed]
- Parida, V.K.; Saidulu, D.; Bhatnagar, A.; Gupta, A.K.; Afzal, M.S. A Critical Assessment of SARS-CoV-2 in Aqueous Environment: Existence, Detection, Survival, Wastewater-based Surveillance, Inactivation Methods, and Effective Management of COVID-19. Chemosphere 2023, 327, 138503. [Google Scholar] [CrossRef] [PubMed]
- Albert, S.; Ruiz, A.; Peman, J.; Salavert, M.; Domingo-Calap, P. Lack of Evidence for Infectious SARS-CoV-2 in Feces and Sewage. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 2665–2667. [Google Scholar] [CrossRef] [PubMed]
- Joshi, M.; Mohandas, S.; Prasad, S.; Shinde, M.; Chavan, N.; Yadav, P.D.; Lavania, M. Lack of Evidence of Viability and Infectivity of SARS-CoV-2 in the Fecal Specimens of COVID-19 Patients. Front Public Health 2022, 10, 1030249. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.M.; Kim, H.M.; Lee, E.J.; Jo, H.J.; Yoon, Y.; Lee, N.J.; Son, J.; Lee, Y.J.; Kim, M.S.; Lee, Y.P.; et al. Detection and Isolation of SARS-CoV-2 in Serum, Urine, and Stool Specimens of COVID-19 Patients from the Republic of Korea. Osong Public Health Res. Perspect. 2020, 11, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Westhaus, S.; Weber, F.A.; Schiwy, S.; Linnemann, V.; Brinkmann, M.; Widera, M.; Greve, C.; Janke, A.; Hollert, H.; Wintgens, T.; et al. Detection of SARS-CoV-2 in Raw and Treated Wastewater in Germany—Suitability for COVID-19 Surveillance and Potential Transmission Risks. Sci. Total Environ. 2021, 751, 141750. [Google Scholar] [CrossRef] [PubMed]
- Polo, D.; Lois, M.; Fernández-Núñez, M.T.; Romalde, J.L. Detection of SARS-CoV-2 RNA in Bivalve Mollusks and Marine Sediments. Sci. Total Environ. 2021, 786, 147534. [Google Scholar] [CrossRef]
- Le Guernic, A.; Palos Ladeiro, M.; Boudaud, N.; Do Nascimento, J.; Gantzer, C.; Inglard, J.C.; Mouchel, J.M.; Pochet, C.; Moulin, L.; Rocher, V.; et al. First Evidence of SARS-CoV-2 Genome Detection in Zebra Mussel (Dreissena polymorpha). J. Environ. Manag. 2022, 301, 113866. [Google Scholar] [CrossRef]
- Mancusi, A.; Capuano, F.; Girardi, S.; Di Maro, O.; Suffredini, E.; Di Concilio, D.; Vassallo, L.; Cuomo, M.C.; Tafuro, M.; Signorelli, D.; et al. Detection of SARS-CoV-2 RNA in Bivalve Mollusks by Droplet Digital RT-PCR (dd RT-PCR). Int. J. Environ. Res. Public Health 2022, 19, 943. [Google Scholar] [CrossRef]
- Menachery, V.D.; Dinnon, K.H., 3rd; Yount, B.L., Jr.; McAnarney, E.T.; Gralinski, L.E.; Hale, A.; Graham, R.L.; Scobey, T.; Anthony, S.J. Trypsin Treatment Unlocks Barrier for Zoonotic Bat Coronavirus Infection. J. Virol. 2020, 94, e01774-19. [Google Scholar] [CrossRef] [PubMed]
- Aguilo-Gisbert, J.; Padilla-Blanco, M.; Lizana, V.; Maiques, E.; Munoz-Baquero, M.; Chillida-Martinez, E.; Cardells, J.; Rubio-Guerri, C. First Description of SARS-CoV-2 Infection in Two Feral American Mink (Neovison vison) Caught in the Wild. Animals 2021, 11, 1422. [Google Scholar] [CrossRef] [PubMed]
- Confirmation of COVID-19 in Otters at an Aquarium in Georgia. Available online: https://www.aphis.usda.gov/aphis/newsroom/stakeholder-info/sa_by_date/sa-2021/sa-04/covid-georgia-otters (accessed on 8 November 2023).
- Padilla-Blanco, M.; Aguiló-Gisbert, J.; Rubio, V.; Lizana, V.; Chillida-Martínez, E.; Cardells, J.; Maiques, E.; Rubio-Guerri, C. The Finding of the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2) in a Wild Eurasian River Otter (Lutra lutra) Highlights the Need for Viral Surveillance in Wild Mustelids. Front. Veter. Sci. 2022, 9, 826991. [Google Scholar] [CrossRef] [PubMed]
- Melo, F.L.; Bezerra, B.; Luna, F.O.; Barragan, N.A.; Arcoverde, R.M.; Umeed, R.; Lucchini, K.; Attademo, F.L. Coronavirus (SARS-CoV-2) in Antillean manatees (Trichechus Manatusmanatus). Res. Sq. 2022, 1–9. [Google Scholar] [CrossRef]
- Vercammen, F.; Cay, B.; Gryseels, S.; Balmelle, N.; Joffrin, L.; Van Hoorde, K.; Verhaegen, B.; Mathijs, E.; Van Vredendaal, R.; Dharmadhikari, T.; et al. SARS-CoV-2 Infection in Captive Hippos (Hippopotamus amphibius), Belgium. Animals 2023, 13, 316. [Google Scholar] [CrossRef] [PubMed]
- Bui, V.N.; Dao, T.D.; Tran, L.H.; Vu, T.T.; Nguyen, T.H.; Nguyen, G.H.; Tran, K.V.D.; Nguyen, H.X.; Bui, A.N.; Unger, F.; et al. SARS-CoV-2 Infection in a Hippopotamus, Hanoi, Vietnam. Emerg. Infect Dis. 2023, 29, 658–661. [Google Scholar] [CrossRef] [PubMed]
- Neovison Vison (American Mink). Available online: https://www.iucnredlist.org/fr/species/41661/45214988 (accessed on 8 November 2023).
- Lutra Lutra (Eurasian Otter). Available online: https://www.iucnredlist.org/fr/species/12419/218069689 (accessed on 8 November 2023).
- Wurtz, N.; Penant, G.; Jardot, P.; Duclos, N.; La Scola, B. Culture of SARS-CoV-2 in a Panel of Laboratory cell lines, Permissivity, and Differences in Growth Profile. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 477–484. [Google Scholar] [CrossRef]
- Xie, S.Z.; Liu, M.Q.; Jiang, R.D.; Lin, H.F.; Zhang, W.; Li, B.; Su, J.; Ke, F.; Zhang, Q.Y.; Shi, Z.L.; et al. Fish ACE2 is not Susceptible to SARS-CoV-2. Virol. Sin. 2022, 37, 142–144. [Google Scholar] [CrossRef]
- Laghi, V.; Rezelj, V.; Boucontet, L.; Fretaud, M.; Da Costa, B.; Boudinot, P.; Salinas, I.; Lutfalla, G.; Vignuzzi, M.; Levraud, J.P. Exploring Zebrafish Larvae as a COVID-19 Model: Probable Abortive SARS-CoV-2 Replication in the Swim Bladder. Front. Cell. Infect. Microbiol. 2022, 12, 790851. [Google Scholar] [CrossRef]
- Shelemba, A.A.; Kazachkova, E.A.; Kononova, Y.V.; Kazachinskaya, E.I.; Rukavishnikov, M.Y.; Kuvshinova, I.N.; Voevoda, M.I.; Shestopalov, A.M.; Chepurnov, A.A. Cell and Organism Technologies for Assessment of the SARS-CoV-2 Infectivity in Fluid Environment. Bull. Exp. Biol. Med. 2022, 173, 519–522. [Google Scholar] [CrossRef]
- Happi, A.N.; Ayinla, A.O.; Ogunsanya, O.A.; Sijuwola, A.E.; Saibu, F.M.; Akano, K.; George, U.E.; Sopeju, A.E.; Rabinowitz, P.M.; Ojo, K.K.; et al. Detection of SARS-CoV-2 in Terrestrial Animals in Southern Nigeria: Potential Cases of Reverse Zoonosis. Viruses 2023, 15, 1187. [Google Scholar] [CrossRef] [PubMed]
- Chepurnov, A.A.; Kazachinskaya, E.I.; Kazachkova, E.A.; Sharshov, K.A.; Kononova, Y.V.; Shelemba, A.A.; Alekseev, A.Y.; Gulyaeva, M.A.; Voevoda, M.I.; Shestopalov, A.M. Development of a Purified Viral Preparation for Studies of COVID-19 (SARS-CoV-2) Biology. Bull. Exp. Biol. Med. 2021, 172, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Zhukhovitsky, V.; Shevlyagina, N.; Zubasheva, M.; Russu, L.; Gushchin, V.; Meerovich, G.; Strakhovskaya, M. Infectivity and Morphology of Bovine Coronavirus Inactivated In Vitro by Cationic Photosensitizers. Viruses 2022, 14, 1053. [Google Scholar] [CrossRef] [PubMed]
- Romanenko, S.A.; Prokopov, D.Y.; Proskuryakova, A.A.; Davletshina, G.I.; Tupikin, A.E.; Kasai, F.; Ferguson-Smith, M.A.; Trifonov, V.A. The Cytogenetic Map of the Nile Crocodile (Crocodylus niloticus, Crocodylidae, Reptilia) with Fluorescence In Situ Localization of Major Repetitive DNAs. Int. J. Mol. Sci. 2022, 23, 13063. [Google Scholar] [CrossRef] [PubMed]
- Gravell, M.; Malsberger, R.G. A Permanent Cell Line from the Fathead Minnow (Pimephales promelas). Ann. N. Y. Acad. Sci. 1965, 126, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Solis, J.; Mora, E.C. Viral Susceptibility Range of the Fathead Minnow (Pimephales promelas) Poikilothermic Cell Line. Appl. Microbiol. 1970, 19, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Clark, H.F.; Karzon, D.T. Acquired Tolerance to Elevated Temperatures in a Poikilothermic Cell Line (Terrapene Heart, TH-1). Exp. Cell Res. 1967, 48, 269–275. [Google Scholar] [CrossRef]
- Xu, J.; Liu, M.; Niu, X.; Hanson, J.; Jung, K.; Ru, P.; Tu, H.; Jones, D.M.; Vlasova, A.N.; Saif, L.J.; et al. The Cold-Adapted, Temperature-Sensitive SARS-CoV-2 Strain TS11 Is Attenuated in Syrian Hamsters and a Candidate Attenuated Vaccine. Viruses 2022, 15, 95. [Google Scholar] [CrossRef]
- Current ICTV Taxonomy Release. Available online: https://ictv.global/taxonomy (accessed on 8 November 2023).
- Bukhari, K.; Mulley, G.; Gulyaeva, A.A.; Zhao, L.; Shu, G.; Jiang, J.; Neuman, B.W. Description and Initial Characterization of Metatranscriptomic Nidovirus-like Genomes from the Proposed New Family Abyssoviridae, and from a Sister Group to the Coronavirinae, the Proposed Genus Alphaletovirus. Virology 2018, 524, 160–171. [Google Scholar] [CrossRef]
- Mordecai, G.J.; Miller, K.M.; Di Cicco, E.; Schulze, A.D.; Kaukinen, K.H.; Ming, T.J.; Li, S.; Tabata, A.; Teffer, A.; Patterson, D.A.; et al. Endangered Wild Salmon Infected by Newly Discovered Viruses. eLife 2019, 8, e47615. [Google Scholar] [CrossRef]
- Miller, A.K.; Mifsud, J.O.C.; Costa, V.A.; Grimwood, R.M.; Kitson, J.; Baker, C.; Brosnahan, C.L.; Pande, A.; Holmes, E.C.; Gemmell, N.J.; et al. Slippery when Wet: Cross-species Transmission of Divergent Coronaviruses in Bony and Jawless Fish and the Evolutionary History of the Coronaviridae. Virus Evol. 2021, 7, veab050. [Google Scholar] [CrossRef] [PubMed]
- Mordecai, G.J.; Hewson, I. Coronaviruses in the Sea. Front. Microbiol. 2020, 11, 1795. [Google Scholar] [CrossRef] [PubMed]
- Bestion, E.; Halfon, P.; Mezouar, S.; Mège, J.L. Cell and Animal Models for SARS-CoV-2 Research. Viruses 2022, 14, 1507. [Google Scholar] [CrossRef] [PubMed]
- Farber, I.; Kruger, J.; Rocha, C.; Armando, F.; von Kockritz-Blickwede, M.; Pohlmann, S.; Braun, A.; Baumgartner, W.; Runft, S.; Kruger, N. Investigations on SARS-CoV-2 Susceptibility of Domestic and Wild Animals Using Primary Cell Culture Models Derived from the Upper and Lower Respiratory Tract. Viruses 2022, 14, 828. [Google Scholar] [CrossRef] [PubMed]
- Al-Benna, S. Gene Expression of Angiotensin-Converting Enzyme 2 Receptor in Skin and the Implications for COVID-19. Adv. Skin. Wound Care 2021, 34, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Zhang, M.; Chang, T.L. ACE2-Independent Alternative Receptors for SARS-CoV-2. Viruses 2022, 14, 2535. [Google Scholar] [CrossRef] [PubMed]
- V’kovski, P.; Gultom, M.; Kelly, J.N.; Steiner, S.; Russeil, J.; Mangeat, B.; Cora, E.; Pezoldt, J.; Holwerda, M.; Kratzel, A.; et al. Disparate Temperature-dependent Virus-Host Dynamics for SARS-CoV-2 and SARS-CoV in the Human Respiratory Epithelium. PLoS Biol. 2021, 19, e3001158. [Google Scholar] [CrossRef] [PubMed]
- Stauft, C.B.; Sangare, K.; Wang, T.T. Differences in New Variant of Concern Replication at Physiological Temperatures In Vitro. J. Infect. Dis. 2023, 227, 202–205. [Google Scholar] [CrossRef]
- Clark, H.F.; Karzon, D.T. Terrapene heart (TH-1), a Continuous Cell Line from the Heart of the Box Turtle Terrapene carolina. Exp. Cell Res. 1967, 48, 263–268. [Google Scholar] [CrossRef]
- Terrapene carolina (Eastern Box Turtle). Available online: https://www.iucnredlist.org/fr/species/21641/97428179#habitat-ecology (accessed on 8 November 2023).
- Rottier, P.J.; Spaan, W.J.; Horzinek, M.C.; van der Zeijst, B.A. Translation of Three Mouse Hepatitis Virus Strain A59 Subgenomic RNAs in Xenopus laevis Oocytes. J. Virol. 1981, 38, 20–26. [Google Scholar] [CrossRef]
- de Oliveira, L.C.; Torres-Franco, A.F.; Lopes, B.C.; Santos, B.S.Á.D.S.; Costa, E.A.; Costa, M.S.; Reis, M.T.P.; Melo, M.C.; Polizzi, R.B.; Teixeira, M.M.; et al. Viability of SARS-CoV-2 in River Water and Wastewater at Different Temperatures and Solids Content. Water Res. 2021, 195, 117002. [Google Scholar] [CrossRef]
- Sherchan, S.; Thakali, O.; Ikner, L.A.; Gerba, C.P. Survival of SARS-CoV-2 in wastewater. Sci. Total Environ. 2023, 882, 163049. [Google Scholar] [CrossRef]
- UN News. WHO Chief Declares End to COVID-19 as a Global Health Emergency. Available online: https://news.un.org/en/story/2023/05/1136367 (accessed on 8 November 2023).
| Name of Culture, Organ (Tissue) Origin | Type of Culture | Composition of Growth Medium | Cultivation Conditions | Collection |
|---|---|---|---|---|
| Vero E6 African green monkey (Chlorocebus sabaeus), kidney | continuous, epithelial-like | MEM with L-glutamine, 10% FBS (Fetal Bovine Serum), gentamicin 5 μL/mL | 5% CO2, 37 °C | State Research Center of Virology and Biotechnology «VECTOR», Rospotrebnadzor |
| TH-1 eastern box turtle (Terrapene carolina), heart | continuous, epithelial-like | DMEM with L-glutamine, 10% FBS, gentamicin 5 μL/mL | 24 °C | National Research Center for Epidemiology and Microbiology named after Honorary Academician N F Gamaleya of the Ministry of Health of the Russian Federation |
| FHM fathead minnow (Pimephales promelas), caudal peduncle | continuous, epithelial-like | DMEM with L-glutamine, 10% FBS, gentamicin 5 μL/mL | 24 °C | National Research Center for Epidemiology and Microbiology named after Honorary Academician N F Gamaleya of the Ministry of Health of the Russian Federation |
| CNI Nile crocodile (Crocodylus niloticus), embryo | primary fibroblasts, 4th passage | Alpha MEM with L-glutamine, 15 FBS, gentamicin 5 μL/mL | 5% CO2, 30 °C | Cryobank of Cell Culture, Core Facilities Centre, IMCB, SB RAS |
| CGIB Silver carp (Carassius gibelio), swim bladder | diploid fibroblasts, 22th passage | Alpha MEM with L-glutamine, 15% FBS, gentamicin 5 μL/mL | 5% CO2, 28 °C | Cryobank of Cell Culture, Core Facilities Centre, IMCB, SB RAS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kononova, Y.; Adamenko, L.; Kazachkova, E.; Solomatina, M.; Romanenko, S.; Proskuryakova, A.; Utkin, Y.; Gulyaeva, M.; Spirina, A.; Kazachinskaia, E.; et al. Features of SARS-CoV-2 Replication in Various Types of Reptilian and Fish Cell Cultures. Viruses 2023, 15, 2350. https://doi.org/10.3390/v15122350
Kononova Y, Adamenko L, Kazachkova E, Solomatina M, Romanenko S, Proskuryakova A, Utkin Y, Gulyaeva M, Spirina A, Kazachinskaia E, et al. Features of SARS-CoV-2 Replication in Various Types of Reptilian and Fish Cell Cultures. Viruses. 2023; 15(12):2350. https://doi.org/10.3390/v15122350
Chicago/Turabian StyleKononova, Yulia, Lyubov Adamenko, Evgeniya Kazachkova, Mariya Solomatina, Svetlana Romanenko, Anastasia Proskuryakova, Yaroslav Utkin, Marina Gulyaeva, Anastasia Spirina, Elena Kazachinskaia, and et al. 2023. "Features of SARS-CoV-2 Replication in Various Types of Reptilian and Fish Cell Cultures" Viruses 15, no. 12: 2350. https://doi.org/10.3390/v15122350
APA StyleKononova, Y., Adamenko, L., Kazachkova, E., Solomatina, M., Romanenko, S., Proskuryakova, A., Utkin, Y., Gulyaeva, M., Spirina, A., Kazachinskaia, E., Palyanova, N., Mishchenko, O., Chepurnov, A., & Shestopalov, A. (2023). Features of SARS-CoV-2 Replication in Various Types of Reptilian and Fish Cell Cultures. Viruses, 15(12), 2350. https://doi.org/10.3390/v15122350






