Single-Center Experience in Detecting Influenza Virus, RSV and SARS-CoV-2 at the Emergency Department
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Collection
2.2. Test Strategy
2.3. Immunologic Assays
2.4. RT-PCR
2.5. Data Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nguyen-Van-Tam, J.S.; O′Leary, M.; Martin, E.T.; Heijnen, E.; Callendret, B.; Fleischhackl, R.; Comeaux, C.; Tran, T.M.P.; Weber, K. Burden of respiratory syncytial virus infection in older and high-risk adults: A systematic review and meta-analysis of the evidence from developed countries. Eur. Respir. Rev. 2022, 31, 220105. [Google Scholar] [CrossRef] [PubMed]
- Burkert, F.R.; Lanser, L.; Bellmann-Weiler, R.; Weiss, G. Coronavirus Disease 2019: Clinics, Treatment, and Prevention. Front. Microbiol. 2021, 12, 761887. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, K.G. Clinical features of influenza. Semin. Respir. Infect. 1992, 7, 26–37. [Google Scholar] [PubMed]
- Uyeki, T.M.; Hui, D.S.; Zambon, M.; Wentworth, D.E.; Monto, A.S. Influenza. Lancet 2022, 400, 693–706. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.E.; Legge, K.L. Influenza A Virus Vaccination: Immunity, Protection, and Recent Advances Toward A Universal Vaccine. Vaccines 2020, 8, 434. [Google Scholar] [CrossRef]
- Bergeri, I.; Whelan, M.G.; Ware, H.; Subissi, L.; Nardone, A.; Lewis, H.C.; Li, Z.; Ma, X.; Valenciano, M.; Cheng, B.; et al. Global SARS-CoV-2 seroprevalence from January 2020 to April 2022: A systematic review and meta-analysis of standardized population-based studies. PLoS Med. 2022, 19, e1004107. [Google Scholar] [CrossRef]
- Koelle, K.; Martin, M.A.; Antia, R.; Lopman, B.; Dean, N.E. The changing epidemiology of SARS-CoV-2. Science 2022, 375, 1116–1121. [Google Scholar] [CrossRef]
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. The challenge of emerging and re-emerging infectious diseases. Nature 2004, 430, 242–249. [Google Scholar] [CrossRef]
- Kayode, A.J.; Banji-Onisile, F.O.; Olaniran, A.O.; Okoh, A.I. An Overview of the Pathogenesis, Transmission, Diagnosis, and Management of Endemic Human Coronaviruses: A Reflection on the Past and Present Episodes and Possible Future Outbreaks. Pathogens 2021, 10, 1108. [Google Scholar] [CrossRef]
- Corman, V.M.; Muth, D.; Niemeyer, D.; Drosten, C. Hosts and Sources of Endemic Human Coronaviruses. Adv. Virus Res. 2018, 100, 163–188. [Google Scholar] [CrossRef]
- Cohen, L.E.; Spiro, D.J.; Viboud, C. Projecting the SARS-CoV-2 transition from pandemicity to endemicity: Epidemiological and immunological considerations. PLoS Pathog. 2022, 18, e1010591. [Google Scholar] [CrossRef]
- Li, J.; Lai, S.; Gao, G.F.; Shi, W. The emergence, genomic diversity and global spread of SARS-CoV-2. Nature 2021, 600, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.S.; Liu, D.X. Similarities and Dissimilarities of COVID-19 and Other Coronavirus Diseases. Annu. Rev. Microbiol. 2021, 75, 19–47. [Google Scholar] [CrossRef] [PubMed]
- de Wit, E.; Van Doremalen, N.; Falzarano, D.; Munster, V.J. SARS and MERS: Recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016, 14, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Fineberg, H.V. Pandemic Preparedness and Response—Lessons from the H1N1 Influenza of 2009. N. Engl. J. Med. 2014, 370, 1335–1342. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.-M.; Wang, W.; Song, Z.-G.; Hu, Y.; Tao, Z.-W.; Tian, J.-H.; Pei, Y.-Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Iftekhar, E.N.; Priesemann, V.; Balling, R.; Bauer, S.; Beutels, P.; Valdez, A.C.; Cuschieri, S.; Czypionka, T.; Dumpis, U.; Glaab, E.; et al. A look into the future of the COVID-19 pandemic in Europe: An expert consultation. Lancet Reg. Health-Eur. 2021, 8, 100185. [Google Scholar] [CrossRef]
- Kevadiya, B.D.; Machhi, J.; Herskovitz, J.; Oleynikov, M.D.; Blomberg, W.R.; Bajwa, N.; Soni, D.; Das, S.; Hasan, M.; Patel, M.; et al. Diagnostics for SARS-CoV-2 infections. Nat. Mater. 2021, 20, 593–605. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Ahmad Farouk, I.; Lal, S.K. COVID-19: A Review on the Novel Coronavirus Disease Evolution, Transmission, Detection, Control and Prevention. Viruses 2021, 13, 202. [Google Scholar] [CrossRef] [PubMed]
- Buchta, C.; Müller, M.M.; Griesmacher, A. The importance of external quality assessment data in evaluating SARS-CoV-2 virus genome detection assays. Lancet Microbe 2022, 3, e168. [Google Scholar] [CrossRef] [PubMed]
- Dinnes, J.; Deeks, J.J.; Berhane, S.; Taylor, M.; Adriano, A.; Davenport, C.; Dittrich, S.; Emperador, D.; Takwoingi, Y.; Cunningham, J.; et al. Rapid, point-of-care antigen and Molecular-Based tests for diagnosis of SARS-CoV-2 infection. Cochrane Database Syst. Rev. 2021, 3, CD013705. [Google Scholar] [CrossRef]
- Brümmer, L.E.; Katzenschlager, S.; McGrath, S.; Schmitz, S.; Gaeddert, M.; Erdmann, C.; Bota, M.; Grilli, M.; Larmann, J.; Weigand, M.A.; et al. Accuracy of rapid point-of-care antigen-based diagnostics for SARS-CoV-2: An updated systematic review and meta-analysis with meta-regression analyzing influencing factors. PLoS Med. 2022, 19, e1004011. [Google Scholar] [CrossRef]
- Corman, V.M.; Haage, V.C.; Bleicker, T.; Schmidt, M.L.; Mühlemann, B.; Zuchowski, M.; Jo, W.K.; Tscheak, P.; Möncke-Buchner, E.; Müller, M.A.; et al. Comparison of seven commercial SARS-CoV-2 rapid point-of-care antigen tests: A single-centre laboratory evaluation study. Lancet Microbe 2021, 2, e311–e319. [Google Scholar] [CrossRef]
- Bellmann-Weiler, R.; Beikircher, B.; Kurz, K.; Theurl, I.; Weiss, G. Accuracy of bedside antigen tests in the diagnosis of new influenza A/H1N1v infection. Clin. Microbiol. Infect. 2011, 17, 235–237. [Google Scholar] [CrossRef]
- Lanser, L.; Bellmann-Weiler, R.; Öttl, K.-W.; Huber, L.; Griesmacher, A.; Theurl, I.; Weiss, G. Evaluating the clinical utility and sensitivity of SARS-CoV-2 antigen testing in relation to RT-PCR Ct values. Infection 2020, 49, 555–557. [Google Scholar] [CrossRef]
- Self, W.H.; McNaughton, C.D.; Grijalva, C.G.; Zhu, Y.; Chappell, J.D.; Williams, J.V.; Talbot, H.K.; Shay, D.K.; Griffin, M.R. Diagnostic performance of the BinaxNow Influenza A&B rapid antigen test in ED patients. Am. J. Emerg. Med. 2012, 30, 1955–1961. [Google Scholar] [CrossRef]
- Dugas, A.F.; Valsamakis, A.; Atreya, M.; Thind, K.; Manchego, P.A.; Faisal, A.; Gaydos, C.A.; Rothman, R. Clinical diagnosis of influenza in the ED. Am. J. Emerg. Med. 2015, 33, 770–775. [Google Scholar] [CrossRef] [Green Version]
- Monto, A.S.; Gravenstein, S.; Elliott, M.; Colopy, M.; Schweinle, J. Clinical Signs and Symptoms Predicting Influenza Infection. Arch. Intern. Med. 2000, 160, 3243–3247. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Song, J.-U.; Kim, Y.H. Diagnostic Accuracy of the Quidel Sofia Rapid Influenza Fluorescent Immunoassay in Patients with Influenza-like Illness: A Systematic Review and Meta-analysis. Tuberc. Respir. Dis. 2021, 84, 226–236. [Google Scholar] [CrossRef]
- Isles, N.; Badman, S.G.; Ballard, S.; Zhang, B.; Howden, B.P.; Guy, R.; Williamson, D.A. Analytical sensitivity and specificity of the Cepheid Xpert Xpress SARS-CoV-2/Flu/RSV assay. Pathology 2021, 54, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.; Zubrzycki, A.; Henry, M.; Ranadheera, C.; Corbett, C.; Meyers, A.F.; Sandstrom, P.A.; Becker, M.G. Clinical Evaluation of the GeneXpert® Xpert® Xpress SARS-CoV-2/Flu/RSV Combination Test. J. Clin. Virol. Plus 2021, 1, 100014. [Google Scholar] [CrossRef] [PubMed]
- Uhteg, K.; Jarrett, J.; Richards, M.; Howard, C.; Morehead, E.; Geahr, M.; Gluck, L.; Hanlon, A.; Ellis, B.; Kaur, H.; et al. Comparing the analytical performance of three SARS-CoV-2 molecular diagnostic assays. J. Clin. Virol. 2020, 127, 104384. [Google Scholar] [CrossRef] [PubMed]
- Visseaux, B.; Le Hingrat, Q.; Collin, G.; Ferré, V.; Storto, A.; Ichou, H.; Bouzid, D.; Poey, N.; de Montmollin, E.; Descamps, D.; et al. Evaluation of the RealStar® SARS-CoV-2 RT-PCR kit RUO performances and limit of detection. J. Clin. Virol. 2020, 129, 104520. [Google Scholar] [CrossRef] [PubMed]
- Research, V.C.f.E. Chronologie zur Corona-Krise in Österreich. Austrian Corona Panel Proj Teil 1–7. Available online: https://viecer.univie.ac.at/coronapanel/austrian-corona-panel-data/method-report/ (accessed on 21 December 2022).
- Steindl, D. Distance Learning während der COVID-19 Pandemie. Diploma thesis published in May 2022, 8–10. Available online: https://epub.jku.at/obvulihs/content/titleinfo/7833609/full.pdf (accessed on 26 December 2022).
- Barra, G.B.; Rita, T.H.S.; Mesquita, P.G.; Jácomo, R.H.; Nery, L.F.A. Overcoming Supply Shortage for SARS-CoV-2 Detection by RT-qPCR. Genes 2021, 12, 90. [Google Scholar] [CrossRef]
- Esbin, M.N.; Whitney, O.N.; Chong, S.; Maurer, A.; Darzacq, X.; Tjian, R. Overcoming the bottleneck to widespread testing: A rapid review of nucleic acid testing approaches for COVID-19 detection. RNA 2020, 26, 771–783. [Google Scholar] [CrossRef]
- Michel, J.; Neumann, M.; Krause, E.; Rinner, T.; Muzeniek, T.; Grossegesse, M.; Hille, G.; Schwarz, F.; Puyskens, A.; Förster, S.; et al. Resource-efficient internally controlled in-house real-time PCR detection of SARS-CoV-2. Virol. J. 2021, 18, 110. [Google Scholar] [CrossRef]
- Nairz, M.; Bellmann-Weiler, R.; Ladstätter, M.; Schüllner, F.; Zimmermann, M.; Koller, A.-M.; Blunder, S.; Naschberger, H.; Klotz, W.; Herold, M.; et al. Overcoming limitations in the availability of swabs systems used for SARS-CoV-2 laboratory diagnostics. Sci. Rep. 2021, 11, 2261. [Google Scholar] [CrossRef]
- Zambon, M.; Hays, J.; Webster, A.; Newman, R.; Keene, O. Diagnosis of Influenza in the Community. Arch. Intern. Med. 2001, 161, 2116–2122. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Pan, Y.; Li, G.; Xu, W.; Zhang, L.; Yuan, S.; Xia, Y.; Lu, P.; Zhang, J. Distinguishing between COVID-19 and influenza during the early stages by measurement of peripheral blood parameters. J. Med. Virol. 2021, 93, 1029–1037. [Google Scholar] [CrossRef]
- Sieber, P.; Flury, D.; Güsewell, S.; Albrich, W.C.; Boggian, K.; Gardiol, C.; Schlegel, M.; Sieber, R.; Vernazza, P.; Kohler, P. Characteristics of patients with Coronavirus Disease 2019 (COVID-19) and seasonal influenza at time of hospital admission: A single center comparative study. BMC Infect. Dis. 2021, 21, 271. [Google Scholar] [CrossRef]
- Zhang, J.; Ding, D.; Huang, X.; Zhang, J.; Chen, D.; Fu, P.; Shi, Y.; Xu, W.; Tao, Z. Differentiation of COVID-19 from seasonal influenza: A multicenter comparative study: A multicenter comparative study. J. Med. Virol. 2021, 93, 1512–1519. [Google Scholar] [CrossRef] [PubMed]
- Havasi, A.; Visan, S.; Cainap, C.; Cainap, S.S.; Mihaila, A.A.; Pop, L.-A. Influenza A, Influenza B, and SARS-CoV-2 Similarities and Differences—A Focus on Diagnosis. Front. Microbiol. 2022, 13, 908525. [Google Scholar] [CrossRef]
- Burkert, F.R.; Lanser, L.; Pizzini, A.; Bellmann-Weiler, R.; Weiss, G. Markers of Infection-Mediated Cardiac Damage in Influenza and COVID-19. Pathogens 2022, 11, 1191. [Google Scholar] [CrossRef]
- Papachristou, E.; Rokka, C.; Sotiriadou, T.; Maneka, L.; Vassilakis, A.; Sapounas, S.; Paraskevis, D.; Jahaj, E.; Kotanidou, A.; Lagiou, P.; et al. Low circulation of respiratory syncytial and influenza viruses during autumn-winter 2021 in the industrial workplace and long-term healthcare facilities in Athens, Greece. Front. Med. 2023, 9, 1025147. [Google Scholar] [CrossRef]
- García-García, E.; Rodríguez-Pérez, M.; García, S.M.; Montes, R.F.; Castañón, C.S.; Bello, M.C.A.; Dehli, C.R.; Pérez-Méndez, C.; Álvarez, M.A.A.; Calle-Miguel, L. Change on the Circulation of Respiratory Viruses and Pediatric Healthcare Utilization during the COVID-19 Pandemic in Asturias, Northern Spain. Children 2022, 9, 1464. [Google Scholar] [CrossRef]
- Razanajatovo, N.H.; Randriambolamanantsoa, T.H.; Rabarison, J.H.; Randrianasolo, L.; Ankasitrahana, M.F.; Ratsimbazafy, A.; Raherinandrasana, A.H.; Razafimanjato, H.; Raharinosy, V.; Andriamandimby, S.F.; et al. Epidemiological Patterns of Seasonal Respiratory Viruses during the COVID-19 Pandemic in Madagascar, March 2020–May 2022. Viruses 2022, 15, 12. [Google Scholar] [CrossRef]
- Fonville, J.M.; Wilks, S.H.; James, S.L.; Fox, A.; Ventresca, M.; Aban, M.; Xue, L.; Jones, T.C.; Le, N.M.H.; Pham, Q.T.; et al. Antibody landscapes after influenza virus infection or vaccination. Science 2014, 346, 996–1000. [Google Scholar] [CrossRef] [Green Version]
- Gostic, K.M.; Ambrose, M.; Worobey, M.; Lloyd-Smith, J.O. Potent protection against H5N1 and H7N9 influenza via childhood hemagglutinin imprinting. Science 2016, 354, 722–726. [Google Scholar] [CrossRef] [PubMed]
- Möst, J.; Redlberger-Fritz, M.; Weiss, G. Multiple Influenza Virus Infections in 4 Consecutive Epidemiological Seasons: A Retrospective Study in Children and Adolescents. Open Forum Infect. Dis. 2019, 6, ofz195. [Google Scholar] [CrossRef] [PubMed]
- Steponavičienė, A.; Burokienė, S.; Ivaškevičienė, I.; Stacevičienė, I.; Vaičiūnienė, D.; Jankauskienė, A. Influenza and Respiratory Syncytial Virus Infections in Pediatric Patients during the COVID-19 Pandemic: A Single-Center Experience. Children 2023, 10, 126. [Google Scholar] [CrossRef] [PubMed]
- Trifonova, I.; Christova, I.; Madzharova, I.; Angelova, S.; Voleva, S.; Yordanova, R.; Tcherveniakova, T.; Krumova, S.; Korsun, N. Clinical significance and role of coinfections with respiratory pathogens among individuals with confirmed severe acute respiratory syndrome coronavirus-2 infection. Front. Public Health 2022, 10, 959319. [Google Scholar] [CrossRef] [PubMed]
- Virologie Wien. Available online: www.virologie.meduniwien.ac.at/wissenschaft-forschung/virus-epidemiologie/influenza-projekt-diagnostisches-influenzanetzwerk-oesterreich-dinoe/vorhergehende-saisonen/saison-20202021/ (accessed on 29 December 2022).
- ECDC. Available online: www.ecdc.europa.eu/enpublications-data/inlfuenza-virus-characterisation-summary-europe-may-2021 (accessed on 21 December 2022).
- Amman, F.; Markt, R.; Endler, L.; Hupfauf, S.; Agerer, B.; Schedl, A.; Richter, L.; Zechmeister, M.; Bicher, M.; Heiler, G.; et al. Viral variant-resolved wastewater surveillance of SARS-CoV-2 at national scale. Nat. Biotechnol. 2022, 40, 1814–1822. [Google Scholar] [CrossRef]
- Thannesberger, J.; Edermayr, A.; Karimi, A.; Mueller, M.; Karnthaler, U.; Gauss, R.; Penz, D.; Ferlitsch, A.; Steininger, C. Evolution of SARS-CoV-2 Key Mutations in Vienna Detected by Large Scale Screening Program. Viruses 2021, 13, 2014. [Google Scholar] [CrossRef]
- Redlberger-Fritz, M.; Kundi, M.; Popow-Kraupp, T. Detailed Report on 2014/15 Influenza Virus Characteristics, and Estimates on Influenza Virus Vaccine Effectiveness from Austria’s Sentinel Physician Surveillance Network. PLoS ONE 2016, 11, e0149916. [Google Scholar] [CrossRef]
- Schubert, L.; Steininger, J.; Lötsch, F.; Herdina, A.N.; Redlberger-Fritz, M.; Tobudic, S.; Kundi, M.; Strassl, R.; Steininger, C. Surveillance of respiratory syncytial virus infections in adults, Austria, 2017 to 2019. Sci. Rep. 2021, 11, 8939. [Google Scholar] [CrossRef]
- Melidou, A.; Pereyaslov, D.; Hungnes, O.; Prosenc, K.; Alm, E.; Adlhoch, C.; Fielding, J.; Sneiderman, M.; Martinuka, O.; Celentano, L.P.; et al. Virological surveillance of influenza viruses in the WHO European Region in 2019/20—Impact of the COVID-19 pandemic. Eurosurveillance 2020, 25, 2001822. [Google Scholar] [CrossRef]
- Billah, A.; Miah, M.; Khan, N. Reproductive number of coronavirus: A systematic review and meta-analysis based on global level evidence. PLoS ONE 2020, 15, e0242128. [Google Scholar] [CrossRef]
- Burki, T.K. Lifting of COVID-19 restrictions in the UK and the Delta variant. Lancet Respir. Med. 2021, 9, e85. [Google Scholar] [CrossRef] [PubMed]
- Coburn, B.J.; Wagner, B.G.; Blower, S. Modeling influenza epidemics and pandemics: Insights into the future of swine flu (H1N1). BMC Med. 2009, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Rocklöv, J. The effective reproductive number of the Omicron variant of SARS-CoV-2 is several times relative to Delta. J. Travel Med. 2022, 29, taac037. [Google Scholar] [CrossRef] [PubMed]
- Read, J.M.; Bridgen, J.R.E.; Cummings, D.A.T.; Ho, A.; Jewell, C.P. Novel coronavirus 2019-nCoV (COVID-19): Early estimation of epidemiological parameters and epidemic size estimates. Philos. Trans. R. Soc. B Biol. Sci. 2021, 376, 20200265. [Google Scholar] [CrossRef]
- Tang, B.; Bragazzi, N.L.; Li, Q.; Tang, S.; Xiao, Y.; Wu, J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect. Dis. Model. 2020, 5, 248–255. [Google Scholar] [CrossRef]
- Zhao, S.; Lin, Q.; Ran, J.; Musa, S.S.; Yang, G.; Wang, W.; Lou, Y.; Gao, D.; Yang, L.; He, D.; et al. The basic reproduction number of novel coronavirus (2019-nCoV) estimation based on exponential growth in the early outbreak in China from 2019 to 2020: A reply to Dhungana. Int. J. Infect. Dis. 2020, 94, 148–150. [Google Scholar] [CrossRef]
- Adam, D.C.; Wu, P.; Wong, J.Y.; Lau, E.H.Y.; Tsang, T.K.; Cauchemez, S.; Leung, G.M.; Cowling, B.J. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat. Med. 2020, 26, 1714–1719. [Google Scholar] [CrossRef]
- Brugger, J.; Althaus, C.L. Transmission of and susceptibility to seasonal influenza in Switzerland from 2003 to 2015. Epidemics 2020, 30, 100373. [Google Scholar] [CrossRef]
- Chen, P.Z.; Koopmans, M.; Fisman, D.N.; Gu, F.X. Understanding why superspreading drives the COVID-19 pandemic but not the H1N1 pandemic. Lancet Infect. Dis. 2021, 21, 1203–1204. [Google Scholar] [CrossRef]
- Endo, A.; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group; Abbott, S.; Kucharski, A.J.; Funk, S. Estimating the overdispersion in COVID-19 transmission using outbreak sizes outside China. Wellcome Open Res. 2020, 5, 67. [Google Scholar] [CrossRef]
- Popa, A.; Genger, J.-W.; Nicholson, M.D.; Penz, T.; Schmid, D.; Aberle, S.W.; Agerer, B.; Lercher, A.; Endler, L.; Colaço, H.; et al. Genomic epidemiology of superspreading events in Austria reveals mutational dynamics and transmission properties of SARS-CoV-2. Sci. Transl. Med. 2020, 12, eabe2555. [Google Scholar] [CrossRef] [PubMed]
- Sneppen, K.; Nielsen, B.F.; Taylor, R.J.; Simonsen, L. Overdispersion in COVID-19 increases the effectiveness of limiting nonrepetitive contacts for transmission control. Proc. Natl. Acad. Sci. USA 2021, 118, e2016623118. [Google Scholar] [CrossRef]
- Wong, F.; Collins, J.J. Evidence that coronavirus superspreading is fat-tailed. Proc. Natl. Acad. Sci. USA 2020, 117, 29416–29418. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.C.; Biele, G.; Mühlemann, B.; Veith, T.; Schneider, J.; Beheim-Schwarzbach, J.; Bleicker, T.; Tesch, J.; Schmidt, M.L.; Sander, L.E.; et al. Estimating infectiousness throughout SARS-CoV-2 infection course. Science 2021, 373, eabi5273. [Google Scholar] [CrossRef] [PubMed]
- Avanzato, V.A.; Matson, M.J.; Seifert, S.N.; Pryce, R.; Williamson, B.N.; Anzick, S.L.; Barbian, K.; Judson, S.D.; Fischer, E.R.; Martens, C.; et al. Case Study: Prolonged Infectious SARS-CoV-2 Shedding from an Asymptomatic Immunocompromised Individual with Cancer. Cell 2020, 183, 1901–1912.e9. [Google Scholar] [CrossRef]
- Chen, X.; Zhu, B.; Hong, W.; Zeng, J.; He, X.; Chen, J.; Zheng, H.; Qiu, S.; Deng, Y.; Chan, J.C.; et al. Associations of clinical characteristics and treatment regimens with the duration of viral RNA shedding in patients with COVID-19. Int. J. Infect. Dis. 2020, 98, 252–260. [Google Scholar] [CrossRef]
- Dzien, A.; Dzien-Bischinger, C.; Lechleitner, M.; Winner, H.; Weiss, G. Will the COVID-19 pandemic slow down in the Northern hemisphere by the onset of summer? An epidemiological hypothesis. Infection 2020, 48, 627–629. [Google Scholar] [CrossRef]
- Gale, P. Thermodynamic equilibrium dose-response models for MERS-CoV infection reveal a potential protective role of human lung mucus but not for SARS-CoV-2. Microb. Risk Anal. 2020, 16, 100140. [Google Scholar] [CrossRef]
- Karimzadeh, S.; Bhopal, R.; Tien, H.N. Review of infective dose, routes of transmission and outcome of COVID-19 caused by the SARS-CoV-2: Comparison with other respiratory viruses–CORRIGENDUM. Epidemiol. Infect. 2021, 149, e116. [Google Scholar] [CrossRef]
- Miller, S.L.; Nazaroff, W.W.; Jimenez, J.L.; Boerstra, A.; Buonanno, G.; Dancer, S.J.; Kurnitski, J.; Marr, L.C.; Morawska, L.; Noakes, C. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air 2020, 31, 314–323. [Google Scholar] [CrossRef]
- Prentiss, M.; Chu, A.; Berggren, K.K. Finding the infectious dose for COVID-19 by applying an airborne-transmission model to superspreader events. PLoS ONE 2022, 17, e0265816. [Google Scholar] [CrossRef]
- Yezli, S.; Otter, J.A. Minimum Infective Dose of the Major Human Respiratory and Enteric Viruses Transmitted Through Food and the Environment. Food Environ. Virol. 2011, 3, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Cusi, M.G.; Terrosi, C.; Kleines, M.; Schildgen, O. RSV and HMPV seroprevalence in Tuscany (Italy) and North-Rhine Westfalia (Germany) in the winter season 2009/2010. Influ. Other Respir. Viruses 2011, 5, 380–381. [Google Scholar] [CrossRef]
- Griffiths, C.; Drews, S.J.; Marchant, D.J. Respiratory Syncytial Virus: Infection, Detection, and New Options for Prevention and Treatment. Clin. Microbiol. Rev. 2017, 30, 277–319. [Google Scholar] [CrossRef] [PubMed]
- Blümel, B.; Schweiger, B.; Dehnert, M.; Buda, S.; Reuss, A.; Czogiel, I.; Kamtsiuris, P.; Schlaud, M.; Poethko-Müller, C.; Thamm, M.; et al. Age-related prevalence of cross-reactive antibodies against influenza A(H3N2) variant virus, Germany, 2003 to 2010. Eurosurveillance 2015, 20, 21206–21224. [Google Scholar] [CrossRef]
- Hoffmann, K.; Paget, J.; Wojczewski, S.; Katic, M.; Maier, M.; Soldo, D. Influenza vaccination prevalence and demographic factors of patients and GPs in primary care in Austria and Croatia: A cross-sectional comparative study in the framework of the APRES project. Eur. J. Public Health 2016, 26, 395–401. [Google Scholar] [CrossRef]
- Šubelj, V.; Prosenc, K.; Sočan, M. Seroprevalence study of antibodies against influenza A(H1N1) 2009 virus after the second pandemic wave in Slovenia. Wien. Klin. Wochenschr. 2012, 124, 177–180. [Google Scholar] [CrossRef]
- Anderson, E.M.; Goodwin, E.C.; Verma, A.; Arevalo, C.P.; Bolton, M.J.; Weirick, M.E.; Gouma, S.; McAllister, C.M.; Christensen, S.R.; Weaver, J.; et al. Seasonal human coronavirus antibodies are boosted upon SARS-CoV-2 infection but not associated with protection. Cell 2021, 184, 1858–1864. [Google Scholar] [CrossRef]
- Loos, C.; Atyeo, C.; Fischinger, S.; Burke, J.; Slein, M.D.; Streeck, H.; Lauffenburger, D.; Ryan, E.T.; Charles, R.C.; Alter, G. Evolution of Early SARS-CoV-2 and Cross-Coronavirus Immunity. Msphere 2020, 5, e00622-20. [Google Scholar] [CrossRef]
- Breyer, M.-K.; Breyer-Kohansal, R.; Hartl, S.; Kundi, M.; Weseslindtner, L.; Stiasny, K.; Puchhammer-Stöckl, E.; Schrott, A.; Födinger, M.; Binder, M.; et al. Low SARS-CoV-2 seroprevalence in the Austrian capital after an early governmental lockdown. Sci. Rep. 2021, 11, 10158. [Google Scholar] [CrossRef]
- Nunhofer, V.; Weidner, L.; Hoeggerl, A.D.; Zimmermann, G.; Badstuber, N.; Grabmer, C.; Jungbauer, C.; Lindlbauer, N.; Held, N.; Pascariuc, M.; et al. Persistence of Naturally Acquired and Functional SARS-CoV-2 Antibodies in Blood Donors One Year after Infection. Viruses 2022, 14, 637. [Google Scholar] [CrossRef] [PubMed]
- Seekircher, L.; Siller, A.; Astl, M.; Tschiderer, L.; Wachter, G.A.; Pfeifer, B.; Huber, A.; Gaber, M.; Schennach, H.; Willeit, P. Seroprevalence of Anti-SARS-CoV-2 IgG Antibodies in Tyrol, Austria: Updated Analysis Involving 22,607 Blood Donors Covering the Period October 2021 to April 2022. Viruses 2022, 14, 1877. [Google Scholar] [CrossRef] [PubMed]
- Siller, A.; Wachter, G.A.; Neururer, S.; Pfeifer, B.; Astl, M.; Borena, W.; Kimpel, J.; Elmer, S.; Spöck, F.; Vales, A.; et al. Prevalence of SARS-CoV-2 antibodies in healthy blood donors from the state of Tyrol, Austria, in summer 2020. Wien. Klin. Wochenschr. 2021, 133, 1272–1280. [Google Scholar] [CrossRef] [PubMed]
- Weidner, L.; Nunhofer, V.; Jungbauer, C.; Hoeggerl, A.D.; Grüner, L.; Grabmer, C.; Zimmermann, G.; Rohde, E.; Laner-Plamberger, S. Seroprevalence of anti-SARS-CoV-2 total antibody is higher in younger Austrian blood donors. Infection 2021, 49, 1187–1194. [Google Scholar] [CrossRef]
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Primers 2018, 4, 3. [Google Scholar] [CrossRef]
- Tschiderer, L.; Seekircher, L.; Richter, L.; von Laer, D.; Lass-Flörl, C.; Forer, L.; Schönherr, S.; Krammer, F.; Embacher-Aichhorn, S.; Tilg, H.; et al. Ultra-rapid rollout vaccination with BNT162b2 to reduce SARS-CoV-2 infections in the general population. Iscience 2022, 25, 105380. [Google Scholar] [CrossRef]
- Bhavnani, D.; James, E.R.; Johnson, K.E.; Beaudenon-Huibregtse, S.; Chang, P.; Rathouz, P.J.; Weldon, M.; Matouschek, A.; Young, A.E. SARS-CoV-2 viral load is associated with risk of transmission to household and community contacts. BMC Infect. Dis. 2022, 22, 672. [Google Scholar] [CrossRef]
- Granados, A.; Peci, A.; McGeer, A.; Gubbay, J.B. Influenza and rhinovirus viral load and disease severity in upper respiratory tract infections. J. Clin. Virol. 2017, 86, 14–19. [Google Scholar] [CrossRef]
- Hijano, D.R.; De Cardenas, J.B.; Maron, G.; Garner, C.D.; Ferrolino, J.A.; Dallas, R.H.; Gu, Z.; Hayden, R.T. Clinical correlation of influenza and respiratory syncytial virus load measured by digital PCR. PLoS ONE 2019, 14, e0220908. [Google Scholar] [CrossRef]
- Jacot, D.; Greub, G.; Jaton, K.; Opota, O. Viral load of SARS-CoV-2 across patients and compared to other respiratory viruses. Microbes Infect. 2020, 22, 617–621. [Google Scholar] [CrossRef]
- Lee, N.; Chan, P.K.S.; Hui, D.; Rainer, T.; Wong, E.; Choi, K.; Lui, C.Y.G.; Wong, B.C.K.; Wong, R.Y.K.; Lam, W.; et al. Viral Loads and Duration of Viral Shedding in Adult Patients Hospitalized with Influenza. J. Infect. Dis. 2009, 200, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Salto-Alejandre, S.; Berastegui-Cabrera, J.; Camacho-Martínez, P.; Infante-Domínguez, C.; Carretero-Ledesma, M.; Crespo-Rivas, J.C.; Márquez, E.; Lomas, J.M.; Bueno, C.; Amaya, R.; et al. SARS-CoV-2 viral load in nasopharyngeal swabs is not an independent predictor of unfavorable outcome. Sci. Rep. 2021, 11, 12931. [Google Scholar] [CrossRef]
- Heo, M.; Jeong, J.H.; Ju, S.; Lee, S.J.; Jeong, Y.Y.; Lee, J.D.; Yoo, J.-W. Comparison of Clinical Features and Outcomes between SARS-CoV-2 and Non-SARS-CoV-2 Respiratory Viruses Associated Acute Respiratory Distress Syndrome: Retrospective Analysis. J. Clin. Med. 2022, 11, 2246. [Google Scholar] [CrossRef]
- Montesinos, I.L.; Arrieta-Aldea, I.; Dicastillo, A.; Zuccarino, F.; Sorli, L.; Guerri-Fernández, R.; Arnau-Barrés, I.; Montero, M.M.; Siverio-Parès, A.; Durán, X.; et al. Comparison of Hospitalized Coronavirus Disease 2019 and Influenza Patients Requiring Supplemental Oxygen in a Cohort Study: Clinical Impact and Resource Consumption. Clin. Infect. Dis. 2022, 75, 2225–2238. [Google Scholar] [CrossRef]
- Groves, H.E.; Piché-Renaud, P.-P.; Peci, A.; Farrar, D.S.; Buckrell, S.; Bancej, C.; Sevenhuysen, C.; Campigotto, A.; Gubbay, J.B.; Morris, S.K. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: A population-based study. Lancet Reg. Health-Am. 2021, 1, 100015. [Google Scholar] [CrossRef] [PubMed]
- Sahanic, S.; Löffler-Ragg, J.; Tymoszuk, P.; Hilbe, R.; Demetz, E.; Masanetz, R.K.; Theurl, M.; Holfeld, J.; Gollmann-Tepeköylü, C.; Tzankov, A.; et al. The Role of Innate Immunity and Bioactive Lipid Mediators in COVID-19 and Influenza. Front. Physiol. 2021, 12, 688946. [Google Scholar] [CrossRef] [PubMed]
- Leung, N.H.L.; Chu, D.K.W.; Shiu, E.Y.C.; Chan, K.-H.; McDevitt, J.J.; Hau, B.J.P.; Yen, H.-L.; Li, Y.; Ip, D.K.M.; Peiris, J.S.M.; et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020, 26, 676–680. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-P.; Dorigatti, I.; Tsui, K.-L.; Xie, M.; Ling, M.-H.; Yuan, H.-Y. Impact of early phase COVID-19 precautionary behaviors on seasonal influenza in Hong Kong: A time-series modeling approach. Front. Public Health 2022, 10, 992697. [Google Scholar] [CrossRef]
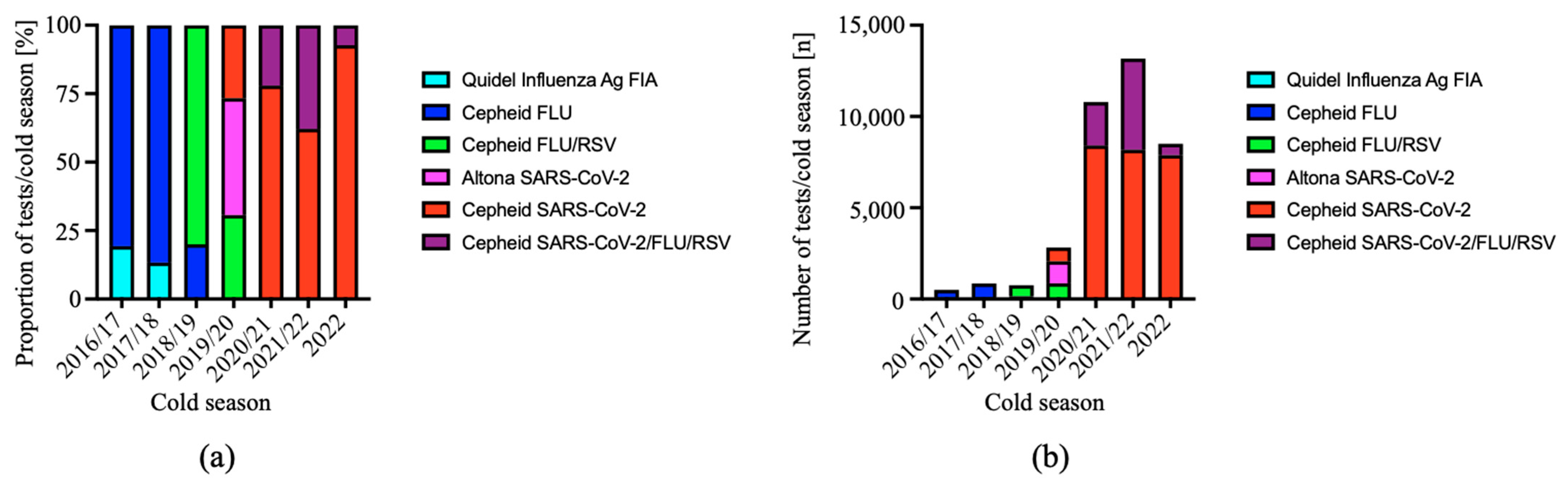






| Name | Method | Format | Virus | Start (CW) | Stop (CW) | Application |
|---|---|---|---|---|---|---|
| Quidel® Sofia® Influenza | Ag test | FIA | Influenza A + B | 05/2016 | 08/2019 | Seasonal |
| Cepheid® FLU | RT-PCR | Cartridge | Influenza A + B | 30/2016 | 02/2019 | Seasonal |
| Cepheid® FLU/RSV | RT-PCR | Cartridge | Influenza A + B + RSV | 01/2019 | Ongoing | Seasonal |
| Altona® SARS-CoV-2 | RT-PCR | 96-well plate | SARS-CoV-2 | 11/2020 | 15/2020 | Temporary |
| Cepheid® SARS-CoV-2 | RT-PCR | Cartridge | SARS-CoV-2 | 16/2020 | Ongoing | Perennial |
| Cepheid® SARS-CoV-2 /FLU/RSV | RT-PCR | Cartridge | Influenza A + B + RSV + SARS-CoV-2 | 51/2020 | Ongoing | Perennial |
| Containment Measure | Start (Date) | Stop (Date) |
|---|---|---|
| First restrictions of international flights | 03/10/2020 | 03/24/2020 |
| First restriction of international railway traffic | 03/11/2020 | 06/02/2020 |
| Cancellation of public events | 03/11/2020 | 05/10/2020 |
| Closure of universities | 03/16/2020 | 05/01/2022 |
| Closure of non-essential shops | 03/16/2020 | 05/01/2020 |
| Restrictions of movement | 03/16/2020 | 05/01/2020 |
| Closure of gastronomy | 03/17/2020 | 05/15/2020 |
| Closure of schools | 03/18/2020 | 05/17/2020 |
| Quarantine of all local communities in Tyrol | 03/18/2020 | 04/07/2020 |
| Face masks in supermarkets and pharmacies | 03/30/2020 | 06/08/2020 |
| Face masks in public means of transport | 04/14/2020 | 01/25/2021 |
| Face masks in non-essential shops | 05/06/2020 | 06/08/2020 |
| FFP2 masks in public indoor places | 01/25/2021 | 07/01/2021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nairz, M.; Todorovic, T.; Gehrer, C.M.; Grubwieser, P.; Burkert, F.; Zimmermann, M.; Trattnig, K.; Klotz, W.; Theurl, I.; Bellmann-Weiler, R.; et al. Single-Center Experience in Detecting Influenza Virus, RSV and SARS-CoV-2 at the Emergency Department. Viruses 2023, 15, 470. https://doi.org/10.3390/v15020470
Nairz M, Todorovic T, Gehrer CM, Grubwieser P, Burkert F, Zimmermann M, Trattnig K, Klotz W, Theurl I, Bellmann-Weiler R, et al. Single-Center Experience in Detecting Influenza Virus, RSV and SARS-CoV-2 at the Emergency Department. Viruses. 2023; 15(2):470. https://doi.org/10.3390/v15020470
Chicago/Turabian StyleNairz, Manfred, Theodora Todorovic, Clemens M. Gehrer, Philipp Grubwieser, Francesco Burkert, Martina Zimmermann, Kristina Trattnig, Werner Klotz, Igor Theurl, Rosa Bellmann-Weiler, and et al. 2023. "Single-Center Experience in Detecting Influenza Virus, RSV and SARS-CoV-2 at the Emergency Department" Viruses 15, no. 2: 470. https://doi.org/10.3390/v15020470
APA StyleNairz, M., Todorovic, T., Gehrer, C. M., Grubwieser, P., Burkert, F., Zimmermann, M., Trattnig, K., Klotz, W., Theurl, I., Bellmann-Weiler, R., & Weiss, G. (2023). Single-Center Experience in Detecting Influenza Virus, RSV and SARS-CoV-2 at the Emergency Department. Viruses, 15(2), 470. https://doi.org/10.3390/v15020470





