1. Introduction
Chemoprophylaxis is a critical tool for many infectious diseases, and in COVID-19 it may have a particular benefit for vulnerable patients that do not maximally benefit from vaccination. Certain sectors of society either cannot or will not benefit from vaccines, and concerns around their longevity on the backdrop of new and future SARS-CoV-2 variants have been raised [
1]. Therefore, effective chemoprophylactic interventions represent a complimentary tool that can be deployed alongside national and international vaccination programmes [
2]. For other diseases and viruses such as malaria, tuberculosis and HIV, successful prophylactic countermeasures have been developed using small-molecule inhibitors of replication [
3,
4,
5]. The authors postulated that the topical administration of an inhibitor of SARS-CoV-2 entry via intranasal delivery to healthy individuals may have utility in preventing transmission. Transmembrane protease serine 2 (TMPRSS2) is a protease found abundantly on the surface of cells within the respiratory tract [
6] and is utilised by SARS-CoV-2 for spike (S) protein priming and activation, which enables virus entry into cells [
7]. TMPRSS2 activity is essential to the pathogenesis of coronaviruses [
8,
9], and therefore presents a putative opportunity as a drug target. The intranasal application of nafamostat has the benefit of direct delivery to SARS-CoV-2 target cells in the upper and lower respiratory tract. Furthermore, Intranasal delivery has the practical benefit of not requiring trained medical personnel or sterile conditions, meaning an intranasally delivered SARS-CoV-2 pre-exposure prophylactic could theoretically be self-administered by users as required.
Nafamostat mesylate (nafamostat) is a serine protease inhibitor used in the treatment of pancreatitis [
10], and has been demonstrated to bind and inhibit TMPRSS2 and block SARS-CoV-2 entry in vitro [
11]. Nafamostat is also hypothesised to have a secondary effect upon thrombotic complications in COVID-19, representing markers of severe disease that are linked to multi-organ failure and mortality [
12]. Nafamostat may inhibit platelet activation, resulting in the subsequent inhibition of neutrophil extracellular traps and thus the direct activation of the intrinsic pathway. When activated alongside other pathways during SARS-CoV-2 infection, it may result in a prothrombotic state [
12].
The current study sought to assess the potential efficacy of intranasal nafamostat in preventing the airborne transmission of SARS-CoV-2 from infected to uninfected Syrian Golden hamsters. The overarching aim was to provide preclinical data to support or refute the utility of nafamostat as a chemoprophylactic intervention for SARS-CoV-2.
2. Materials and Methods
2.1. Materials
Phosphate-buffered saline (PBS), foetal bovine serum (FBS) and 1% penicillin/streptomycin were purchased from Merck (Rahway, NJ, USA). High-glucose Dulbecco’s modified Eagle’s medium (DMEM) and Dulbecco’s PBS were purchased from GibcoTMC (Waltham, MA, USA). In addition, 10% neutral buffered formalin solution and 2.3% crystal violet solution were purchased from SIGMA (St. Louis, MO, USA), and 2% UltraPure LMP Agarose was purchased from Invitrogen (Waltham, MA, USA). Male Syrian Golden hamsters were purchased from Janvier Labs (Essex, UK). Further, 1 mL Amies Regular flocked swabs were purchased from Appleton Woods. Transmission cages were purchased from Techniplast UK Ltd. (Leicester, UK). The GoTaq® Probe 1-Step RT-qPCR System was purchased from Promega (Fitchburg, WI, USA). The SARS-CoV-2 (2019-nCoV) CDC qPCR Probe Assay and CDC RUO 2019-nCoV_N_Positive Control were purchased from IDT (Newark, NJ, USA). TRIzol reagent, GlycoBlueTM, PhasemakerTM tubes, Nanodrop and TURBO DNA-freeTM kits were purchased from Thermo Fisher (Waltham, MA, USA). A bead mill homogeniser was purchased from Fisher Scientific (Waltham, MA, USA). Precellys CKmix lysing tubes were purchased from Bertin Instruments. A Qtower3 Real-Time PCR Detector was purchased from Analytik Jena (Jena, Germany). For immunohistology, the rabbit anti-SARS-CoV nucleoprotein antibody was purchased from Rocklands (British CO, Canada), the peroxidase blocking buffer and the Envision + System HRP Rabbit as well as diaminobenzidine were purchased from Agilent DAKO (Carpinteria, CA, USA), and the Tissue-Tek Film for cover slipping was purchased from Sysmex (Hyogo, Japan).
2.2. Virus Isolates
A PANGO lineage B strain of SARS-CoV-2 (hCoV-2/human/Liverpool/REMRQ0001/2020) was used within this study. The virus was cultured from a nasopharyngeal swab collected from a patient in Liverpool in March 2020, and passaged in Vero-E6 cells. Direct RNA sequencing was previously performed and an in-house script was used to check for deletions in the mapped reads as described previously [
13]. The Illumina reads were mapped to the England/2/2020 genome using HISAT and the consensus genome was called using an in-house script based on the dominant nucleotide at each location on the genome. The sequence has been submitted to GenBank, accession number MW041156.
2.3. Animal Study Design
All work involving SARS-CoV-2 was performed under containment level 3 (CL3) by staff equipped with respirator airstream units with a filtered air supply. Prior to the start of the study, all risk assessments and standard operating procedures were approved by the University of Liverpool Biohazards Sub-Committee and the UK Health and Safety Executive.
All animal studies were conducted in accordance with UK Home Office Animals Scientific Procedures Act (ASPA, 1986). Additionally, all studies were approved by the local University of Liverpool Animal Welfare and Ethical Review Body and performed under UK Home Office Project License PP4715265.
A random block study design was selected for the animal study. Hamsters were randomly assigned into groups of four and acclimatised for 7 days prior to study initiation. Each cage of four animals was then randomly assigned to a treatment group. The hamster selected for virus inoculation, to be designated as the donor hamster, was random in each cage. All researchers completing the viral RNA quantification, plaque assays, and histology and immunohistology analysis were blinded to the sample identifiers and treatment groups during analysis, with a separate unblinded researcher interpretating the results and completing the statistical analysis.
Male Syrian Golden hamsters (80–100 g; Janvier Labs) were housed in individually ventilated cages with environmental enrichment under SPF barrier conditions and a 12 h light/dark cycle at 21 °C ± 2 °C. Free access to food and water was provided throughout the study. All animals were weighed and monitored daily throughout the experiment.
Assessment of Wuhan SARS-CoV-2 Airborne Transmission in Nafamostat-Treated Syrian Golden Hamsters
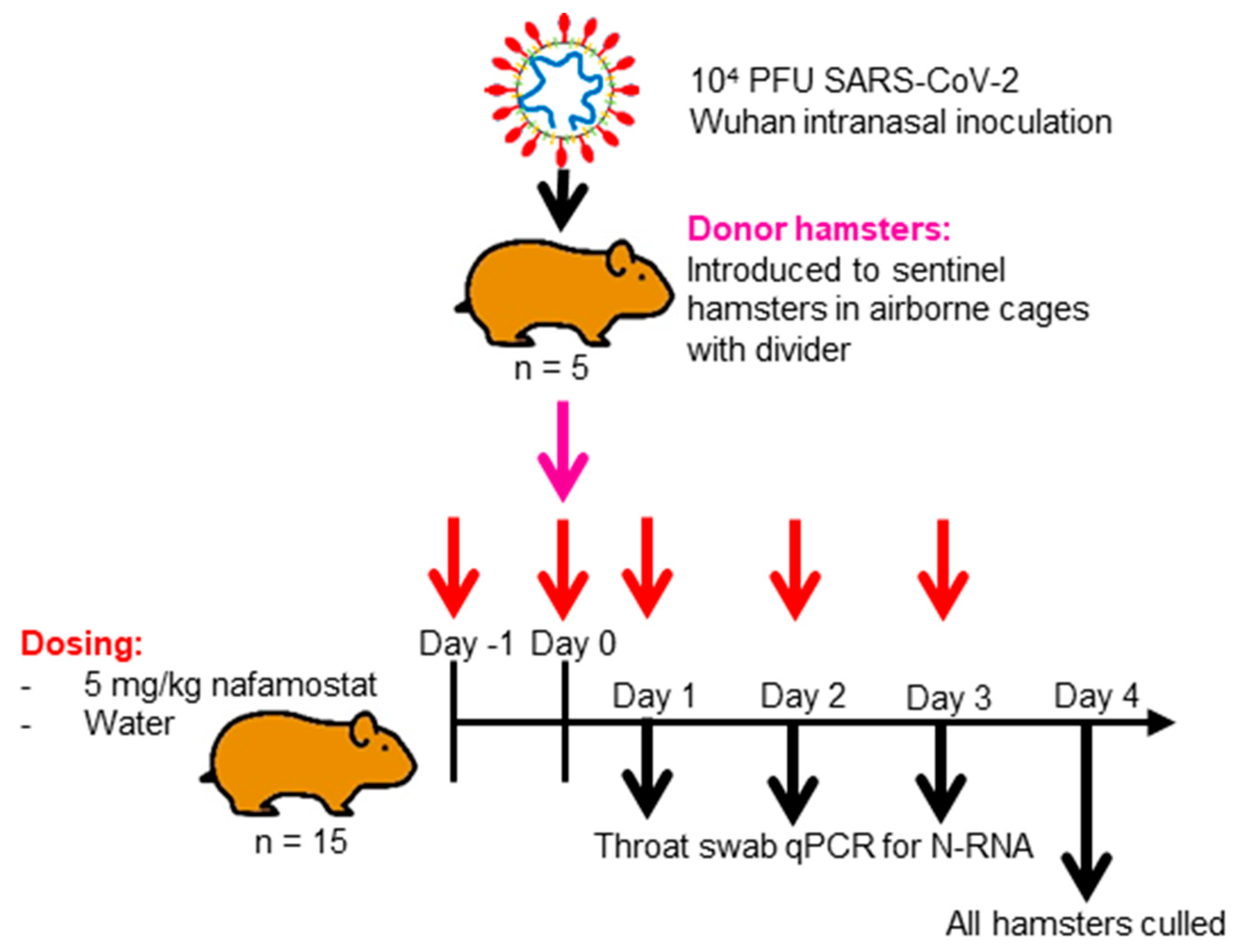
To assess the utility of nafamostat as a chemoprophylaxis against Wuhan SARS-CoV-2, as shown in
Figure 1, 15 naïve hamsters in each group were intranasally dosed with 50 µL of water (control) or 5 mg/kg nafamostat in water twice in 24 h prior to being cohoused with an infected hamster, and then were intranasally dosed twice daily for four days. These animals were known as the sentinel hamsters. Following 24 h cohabitation, an untreated hamster in each group was anaesthetised under 3% isoflurane and inoculated intranasally with 100 µL of 1 × 10
4 PFU of SARS-CoV-2 in PBS. These animals are henceforth referred to as the donor hamsters. Each study group consisted of 5 cages housing 3 treated hamsters and 1 donor hamster. The post-inoculation hamsters were housed in techniplast GR1800DIV cages with a plastic perforated divider that allowed airflow from one side to the other. In each treatment group, the donor hamster was cohoused within the same cage as the treated naïve hamsters, but was physically separated by the plastic perforated barrier to prevent contact transmission. Throat swabs were taken from all animals on days 1, 2, 3 and 4 post-inoculation of the donor hamster. The 15 naïve hamsters in each group continued their respective dosing for 4 days after donor inoculation (day 0) before the treatment was ended, and all hamsters were culled via a lethal intraperitoneal injection of pentobarbitone, which was followed by a cardiac puncture and immediate exsanguination from the heart. Samples from the right lung and nasal turbinates were then harvested and stored at −80 °C for the downstream PCR and plaque assay. Heads and left lungs were collected and fixed in 10% buffered formalin for histological analysis.
2.4. Quantification of Viral RNA via qPCR
A section of the dissected right lung lobe and nasal turbinate material was homogenised twice in 1 mL of TRIzol reagent (Thermo Fisher, Waltham, MA, USA) using a bead mill homogeniser (Fisher Scientific, Waltham, MA, USA) and Precellys CKmix lysing tubes (Bertin Instruments, Montigny-le-Bretonneux, France) at 3.5 m per second for 30 s. The resulting lysate was centrifuged at 12,000× g for 5 min at 4 °C. Throat swab media (260 µL) was added to 750 µL of the TRIzol LS reagent (Thermo Fisher). The clear supernatants were transferred to PhasemakerTM tubes (Thermo Fisher) and processed as per the manufacturer’s instructions to separate total RNA from the phenol-chloroform layer. Subsequently, the recovered RNA was precipitated using GlycoBlueTM according to the manufacturer’s instructions (Thermo Fisher), and was washed and solubilised in RNAse-free water. The RNA was quantified and quality assessed using a Nanodrop (Thermo Fisher). Samples were diluted to 200 ng/mL in 60 µL of RNAse-free water. The resulting RNA samples were DNAse treated using the TURBO DNA-freeTM kit according to the manufacturer’s instructions (Thermo Fisher). The DNAse-treated RNA was stored at −80 °C prior to downstream analysis.
The viral RNA derived from hamster lung, nasal turbinate and throat swabs was quantified using a protocol adapted from the CDC 2019-Novel Coronavirus (2019-nCoV) Real-Time PCR Diagnostic Panel [
14] using the GoTaq
® Probe 1-Step RT-qPCR System (Promega, Fitchburg, WI, USA). For quantification of SARS-CoV-2 using the nCoV assay, the N1 primer/probe mix from the SARS-CoV-2 (2019-nCoV) CDC qPCR Probe Assay (IDT) was selected. A standard curve was prepared (200,000—2 copies/reaction) via a 10-fold serial dilution of the CDC RUO 2019-nCoV_N_Positive Control (IDT). DNAse-treated RNA at 200 ng/mL or dH
2O was added to the appropriate wells, producing final reaction volumes of 20 µL. The prepared plates were run using a Qtower
3 Real-Time PCR Detector (Analytik Jena). The thermal cycling conditions for the qRT-PCR reactions were: 1 cycle of 45 °C for 15 min and 1 cycle of 95 °C for 2 min, followed by 40 cycles of 95 °C for 3 s and 55 °C for 30 s.
The quantification of 18S RNA utilised previously described primers and probe sequences [
15], which were used at 300 nM and 200 nM, respectively (IDT), using the GoTaq
® Probe 1-Step RT-qPCR System (Promega, Fitchburg, WI, USA). Methods for the generation of the 18S standards have been outlined previously [
16]. The PCR product was serially diluted to produce a standard curve in the range of 5 × 10
8, or 5 copies/reaction, via a 10-fold serial dilution. DNAse-treated RNA at 200 ng/mL or dH
2O was added to the appropriate wells, producing final reaction volumes of 20 µL. The prepared plates were run using a qTOWER
3 Real-Time PCR Detector (Analytik Jena, Jena, Germany). The thermal cycling conditions for the qRT-PCR reactions were: 1 cycle of 45 °C for 15 min and 1 cycle of 95 °C for 2 min, followed by 40 cycles of 95 °C for 3 s and 55 °C for 30 s. N-RNA data were normalised to 18S data for subsequent quantitation. The limit of detection (LOD) for the assay was defined as an N-RNA value of ≤2 copies/reaction and a PCR Ct value cut off of ≥32 cycles. These were selected based on previously published data which demonstrated that PCR Ct values between 17 and 32 represent culturable virus amounts, and are assumed to be infectious [
17,
18].
2.5. Plaque Assay
A section of the dissected right lung lobe was homogenised in Precellys® tubes in 1 mL of Dulbecco’s PBS (GibcoTM, Waltham, MA, USA). Samples were homogenised twice using a bead mill homogeniser (Fisher Scientific) at 3.5 m per second (m/s) for 30 s. Samples were then stored at −80 °C for downstream analysis in plaque assays.
Vero-E6 cells (passages 11 to 16) were maintained in high-glucose DMEM (GibcoTM) that was supplemented with 10% FBS and 1% penicillin/streptomycin at 37 °C and 5% CO2. Vero-E6 cells at an 80–90% confluency where seeded at 3 × 105 cells/well in 24-well plates and incubated overnight at 37 °C and 5% CO2. Once 100% confluency of the cells was confirmed in each well, the plates were transferred to CL3, and the plaque assay was completed.
A serial dilution of homogenised tissue samples was prepared in maintenance media (high-glucose DMEM, 2% FBS) in the range of 1–10−7 of the virus titre within the sample.
Then, 100 µL of the serially diluted tissue samples were added to each well of the Vero-E6 cell 24-well plate in duplicate and incubated for one hour at 37 °C and 5% CO2. Next, 500 µL of freshly prepared overlay (maintenance media and 2% UltraPure LMP Agarose (Invitrogen), 4:1) was added to each well and cells were incubated for 72 h at 37 °C and 5% CO2. After the incubation period, cells were fixed with 10% neutral buffered formalin solution (SIGMA) for 30 min and stained with 2.3% crystal violet solution (SIGMA).
In order to determine the plaque-forming units per mL (PFU/mL), the number of formed plaques per well were counted manually and the following formula applied:
where d = the dilution factor, and V = the volume of diluted virus added to the well (mL).
2.6. Histological and Immunohistological Analyses
From all animals the left lung and head were fixed in 10% buffered formalin for 48 h and then stored in 70% ethanol until further processing. Two longitudinal sections were prepared from the lung and were routinely embedded in paraffin wax. Cross sections of the nose, taken using a diamond saw (Exakt 300; Exakt), were prepared in approximately 1.5 mm thick slices (tip of the nose to the level of the olfactory bulb). Sections were gently decalcified in RDF (Biosystems, Foster City, CA, USA) for 10 days at room temperature (RT) and on a shaker, and then were embedded in paraffin wax. Consecutive sections (3–5 µm) were prepared and stained with haematoxylin eosin (HE) for histological examination or subjected to immunohistological staining to detect the SARS-CoV-2 antigen (performed in an autostainer; Agilent DAKO, Carpinteria, CA, USA), using the horseradish peroxidase (HRP) method and rabbit anti-SARS-CoV nucleocapsid protein (Rockland) as previously described [
19]. Briefly, sections were deparaffinised and rehydrated with graded alcohol. Antigen retrieval was achieved via 20 min incubation in citrate buffer (pH 6.0) at 98 °C in a pressure cooker. This was followed by incubation with the primary antibody (diluted 1:3000 in dilution buffer; Agilent Dako) overnight at 4 °C, a 10 min incubation in RT with peroxidase blocking buffer (Agilent Dako) and a 30 min incubation in RT with the Envision + System HRP Rabbit (Agilent Dako, CA, USA). The reaction was visualised with diaminobenzidine (DAB; Dako) for 10 min in RT. After counterstaining with haematoxylin for 2 s, sections were dehydrated and placed on a coverslip with Tissue-Tek Film (Sysmex).
2.7. Statistical Analysis
Prior to the study, a power calculation was conducted for a two-sided unpaired t-test to determine the number of experimental units per study group required to complete a comparison of the lung viral RNA values, which quantified for the water-treated control group and the nafamostat-treated group a power of 0.8 and a significance level of 0.05. A minimum effect size was determined as a 2-fold difference in lung viral RNA, with a standard deviation of 0.38 derived from previous comparable studies conducted in house. An n number of 4 per group was calculated. The power calculation was completed using the NC3Rs Experimental Design Assistant. All sentinel hamsters where housed 3 per cage with a single donor hamster, with a total of five cages per group (15 sentinels and 5 donor hamsters per group total).
A 2-way mixed-effect ANOVA with a Bonferroni correction to correct for multiple comparisons was applied to compare the percentage weight change or viral RNA quantified in the throat swabs by qPCR between the water-treated control and the nafamostat-treated group over the time course of the study. An unpaired t-test was used to compare the differences in the viral RNA load between the water-treated control group and the nafamostat-treated group’s throat swabs, and their lung and nasal turbinate samples. A p-value of ≤0.05 was taken as statistically significant. All statistical analyses were completed using GraphPad Prism version 8.3.0.
4. Discussion
This study sought to determine the suitability of intranasally delivered nafamostat for use as a chemoprophylaxis against SARS-CoV-2 in an airborne transmission model in Syrian Golden hamsters, where donor and sentinel hamsters received a separate food and water supply and were physically separated by a plastic perforated barrier. The intranasal infection of Syrian Golden hamsters with SARS-CoV-2 has previously been demonstrated to result in viral titres and pathological changes similar to those seen in human patients [
22]. Importantly for the current study, the TMPRSS2-mediated priming of the SARS-CoV-2 S protein was found to be largely similar in hamsters and humans [
23], highlighting the similarity between the host response in hamsters and humans and supporting the use of this model for TMPRSS2-targeted therapeutics. However, it should be noted that as a rodent, the hamster is an obligate nasal breather [
24] and has abbreviated bronchioles, which may result in the faster therapeutic clearance in the alveolar of hamsters compared to humans [
25]. The importance of this for the translatability of the results in humans is uncertain, but may suggest a potential limitation for the use of this species to characterise intranasally delivered chemoprophylactic interventions. It is not anticipated that obligate nasal breathing would lower the efficacy of intranasally administered nafamostat; however, it may increase virus acquisition in the lungs of hamsters.
The intranasal dosing of test therapeutics enables direct drug delivery to a primary site of respiratory virus infection, which may be particularly useful for chemoprophylaxis. However, it has so far been unclear whether nafamostat delivered via this route would be sufficient to meaningfully alter the course of SARS-CoV-2 if given in a therapy model. A single-dose pretreatment of Ad5-
hACE2-transduced mice and K18-
hACE2 mice with 3 mg/kg of nafamostat intranasally delivered prior to inoculation with SARS-CoV-2 significantly reduced the viral titres over the study time course [
26]. Furthermore, a study of 420 µg/mL of nafamostat suspended within a novel lipid formulation and administered intranasally to hamsters, which was immediately followed by inoculation with SARS-CoV-2, showed a transient but significant reduction in the viral load within the nasal cavity compared to controls [
27]. Unfortunately, a histopathological assessment of the animals was not undertaken. Also, it is not possible to ascertain whether the limited benefit was a result of the formulation itself, since unformulated nafamostat was not used as a control [
27]. However, studies with a primary lung epithelium cell model demonstrated the low cytotoxicity of the lipid formulation up to 6 µg/mL of nafamostat, with evidence of SARS-CoV-2 inhibition at this dose [
28]. Given that the systemic half-life of nafamostat after intravenous delivery is only 8 min [
29], the protection reported in the present study, with twice daily administration, bodes extremely well for nafamostat reaching its target when intranasally administered. Nafamostat is not currently approved for oral or inhalational administration in human patients, so the development of a specific formulation may be needed if this approach is to be tested in humans.
Lung and nasal turbinate samples were collected at study termination in order to determine the presence or absence of the virus, as well as to analyse the pathological changes in hamsters when given nafamostat as a chemoprophylaxis compared to the donor hamsters or water-treated control group. Widespread SARS-CoV-2 infection in all donor hamsters was confirmed through the quantification of viral RNA, semi-quantitative live virus calculation via plaque assay, and immunohistological staining for the viral antigen. Similarly, all water-treated sentinel animals in four cages were found to be infected, with both nose and lungs harbouring the virus, confirming successful airborne transmission. Interestingly, transmission was less successful in cage #1, where only one sentinel hamster carried the virus in the nose and lungs; in one, only a nasal infection was confirmed, and the third tested negative throughout. It is possible that the donor animal in this cage only shed the virus intermittently or at lower levels [
30]. Also, overall, viral RNA levels and the extent of viral antigen expression were lower than in the donor animals. As shown in
Figure 3 and
Figure 4, the lung, nasal turbinate and swab sample viral RNA at days 3 and 4 in the donor hamsters was comparable to that in the water-treated control group. These high viral loads at the study endpoint indicate a recent infection, which could be the result of airborne transmission between the sentinel hamsters, but could also have been transmitted from the sentinel hamsters back to the donor hamster.
With the nafamostat treatment, two thirds of the sentinel animals tested negative by all approaches at 4 dpi, and there was generally no viral antigen detected. However, several of these animals showed focal type II pneumocyte/bronchiolar epithelial cell hyperplasia, which is consistent with regenerative attempts after infection, as it can be seen as early as 3 days post infection in the hamster model of COVID-19 [
20,
21].
Some discrepancies were observed between the results of the different approaches to detect and quantify infection. In the case of a very limited and focal rather than diffuse infection, this may in part be attributed to the sampling protocol where the left lung was processed for histology and immunohistology, and the right lung was subjected to the quantitative PCR and plaque assay. A further limitation of the present study is that intranasally nafamostat-dosed animals not cohoused with a donor hamster were not included in the study, meaning that determining if intranasal dosing alone induces histological changes in the nasal mucosa and lung is beyond the scope of this study. In three hamsters in the water-treated control group and five hamsters in the nafamostat-treated group, a N-gene PCR value below the LOD for the assay was observed alongside a positive plaque assay result. Variation in virus detection between the different analyses may be caused by the LOD cut off applied to the viral N-gene RNA quantification via PCR. For the PCR assay, an LOD was defined as an N-RNA value of ≤2 copies/reaction and the PCR Ct value cut off was 32 cycles. This LOD was determined given that PCR Ct values between 17 and 32 have been demonstrated previously to represent culturable virus amounts, which are assumed to be infectious [
17,
18]. The inclusion of this Ct cut off as part of the LOD may exclude quantifiable values of viral N-RNA lower than 2 copies/reaction. Consideration must also be given to the plaque assay being semi-quantitative and to its ability to exclusively highlight the presence of live virus within the lung samples. Despite these limitations, collectively these methods enable a comprehensive evaluation of the chemoprophylactic effect of intranasally administered nafamostat, which must be holistically assessed.
Of note, when using the plaque assay data, the transmission rate of SARS-CoV-2 from the donor hamsters to the water-treated control hamsters and to the nafamostat-treated hamsters was found to be 80% and 33%, respectively. A previous study which used surgical mask material to separate a donor hamster from untreated hamsters recorded a reduction in transmissibility from 60% in the no surgical mask partition group to 12.5% in the surgical mask partitioned group, which was culled at day 4 after cohousing [
31]. This comparable reduction in transmissibility between the nafamostat treatment and mask wearing is of interest. In a real-world situation, mask wearing could be combined with the administration of an intranasal chemoprophylaxis, but additional studies would be needed to ascertain the benefits of such an approach. Mask use and chemoprophylaxis both have a role to play in SARS-CoV-2 disease prevention in people who are at risk of complications from disease acquisition. The development of a self-administered aerosol of nafamostat may afford additional discretion for the user and would enable protection for people with a low tolerance for wearing masks over extended periods of time.
The primary mechanism of action of nafamostat is thought to be the inhibition of the TMPRSS2 serine protease, which plays an important role in cell entry. This is important because some data have suggested differences in the importance of TMPRSS2 for the entry of different SARS-CoV-2 lineages and sub-lineages [
32,
33,
34]. Accordingly, future clinical trials and deployment may need to consider the relative importance of TMPRSS2 for variants predominantly circulating at the time of intervention. Further studies would be beneficial to assess the pharmacokinetics of intranasally delivered nafamostat in respiratory secretions and whether the efficacy of nafamostat can be boosted through delivery with an aerosol. Overall, clear differences in the response to cohousing with the donor hamsters was observed between the water-treated control group and the nafamostat-treated hamsters (see
Supplementary Table S1) in terms of viral RNA quantification, live virus calculation, and the histological and immunohistological findings. Taken collectively, these data demonstrate that 5 mg/kg of twice daily intranasally administered nafamostat can exert a chemoprophylactic effect in healthy hamsters.