Small Molecules Targeting 3C Protease Inhibit FMDV Replication and Exhibit Virucidal Effect in Cell-Based Assays
Abstract
:1. Introduction
2. Materials and Methods
2.1. Structure-Based Virtual Screening of NCI Compound Libraries
2.2. Cells and Viruses
2.3. Cytotoxicity Assay
2.4. Antiviral Activity
2.4.1. Post Entry Assay
2.4.2. Co-Treatment Assay
2.4.3. Pre-Treatment Assay
2.4.4. Attachment Assay
2.4.5. Penetration Assay
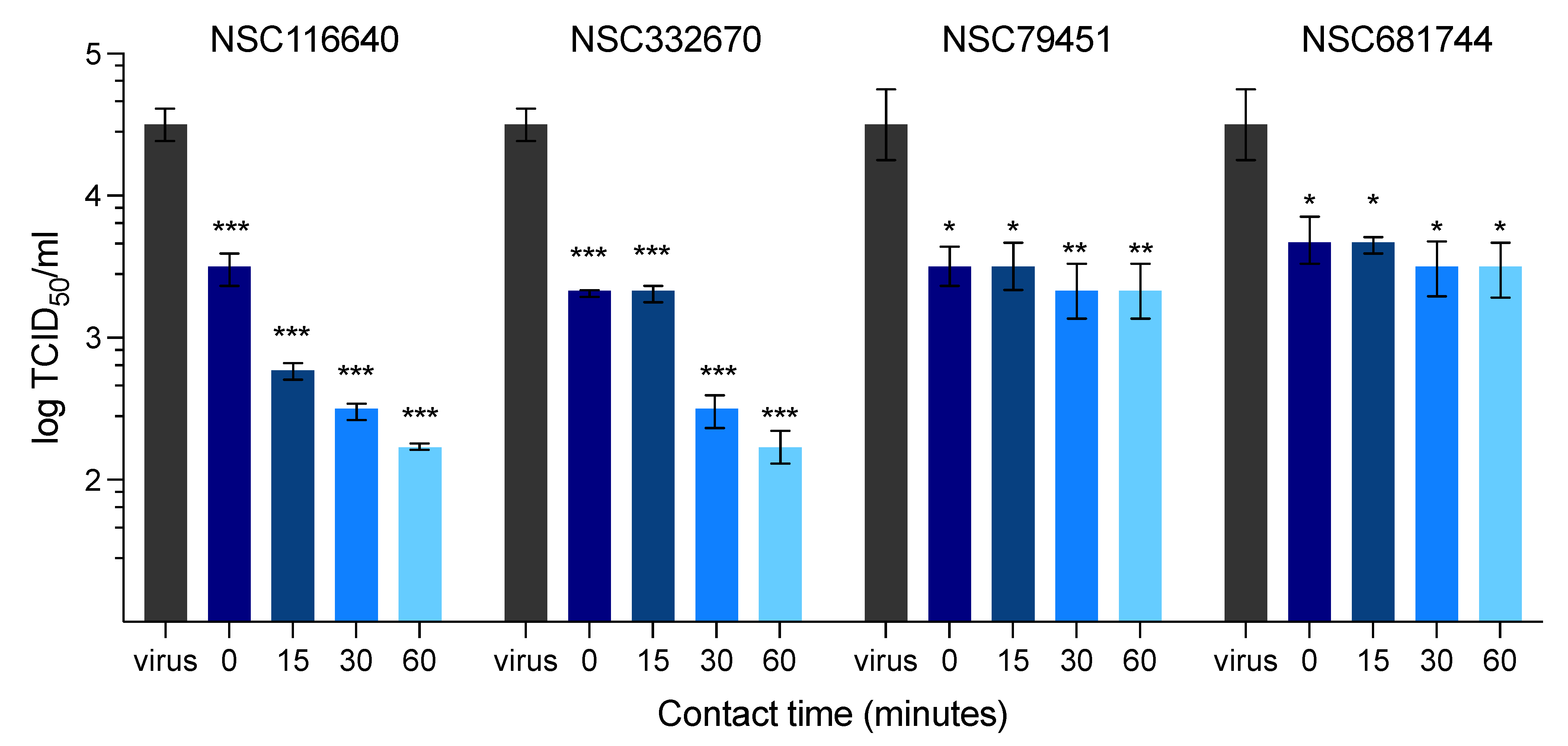
2.4.6. Virucidal Activity (Time Course Assays)
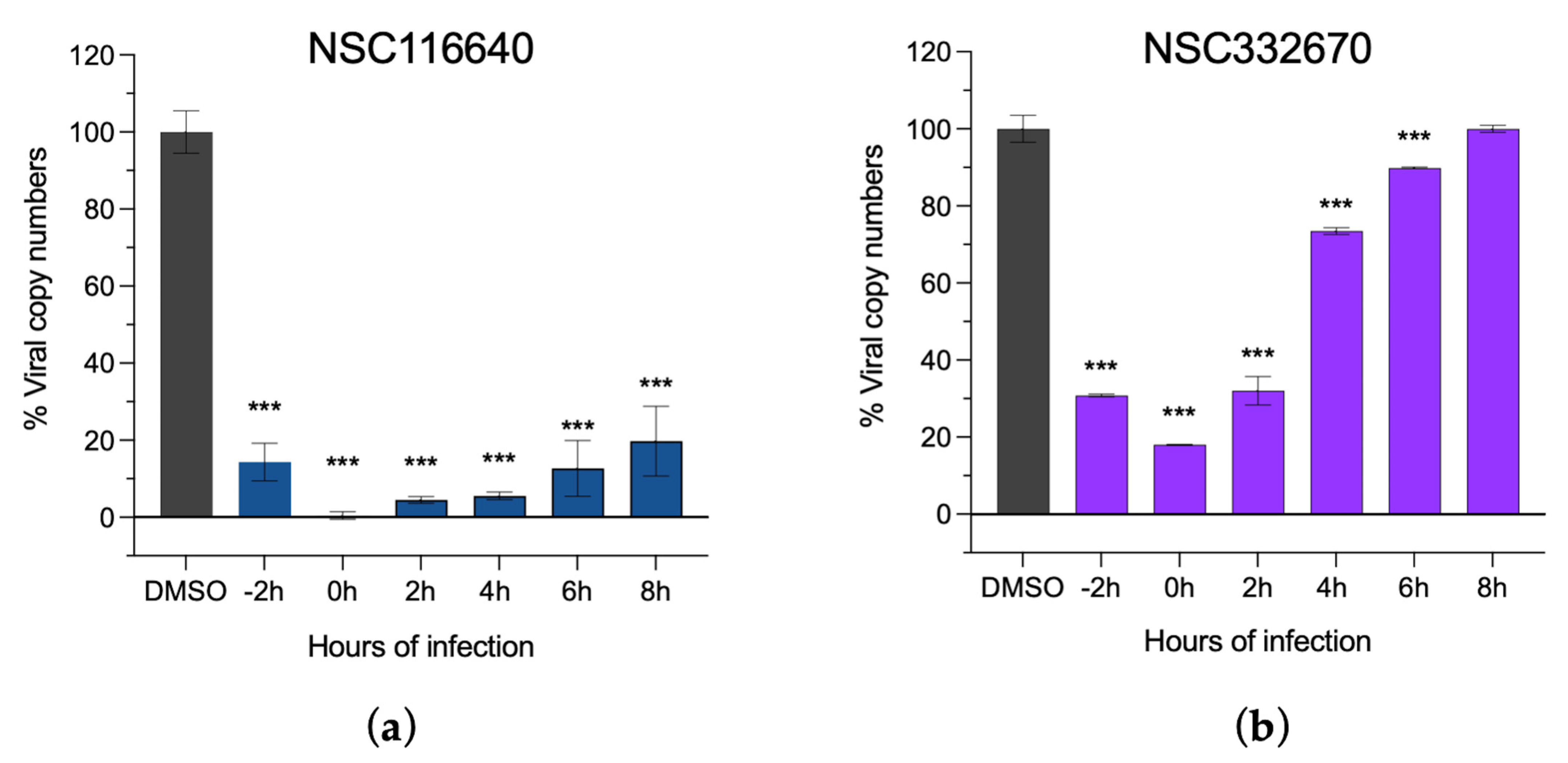
2.4.7. Time-of-Addition (ToA) Assay
2.5. Immunoperoxidase Monolayer Assay (IPMA)
2.6. Determination of FMDV Copy Number Using RT-qPCR
2.7. Intracellular Protease Assay
2.8. In Silico Molecular Interaction and Physicochemical Properties of Compounds
2.9. Statistical Analysis
(mean of the cell controlii − mean of the virus controlii)]
3. Results
3.1. Structure-Based Virtual Screening of Small Molecules Using AutoDock Vina
3.2. Antiviral Activity against FMDV Infection
3.3. Intracellular FMDV Protease Inhibition Assay
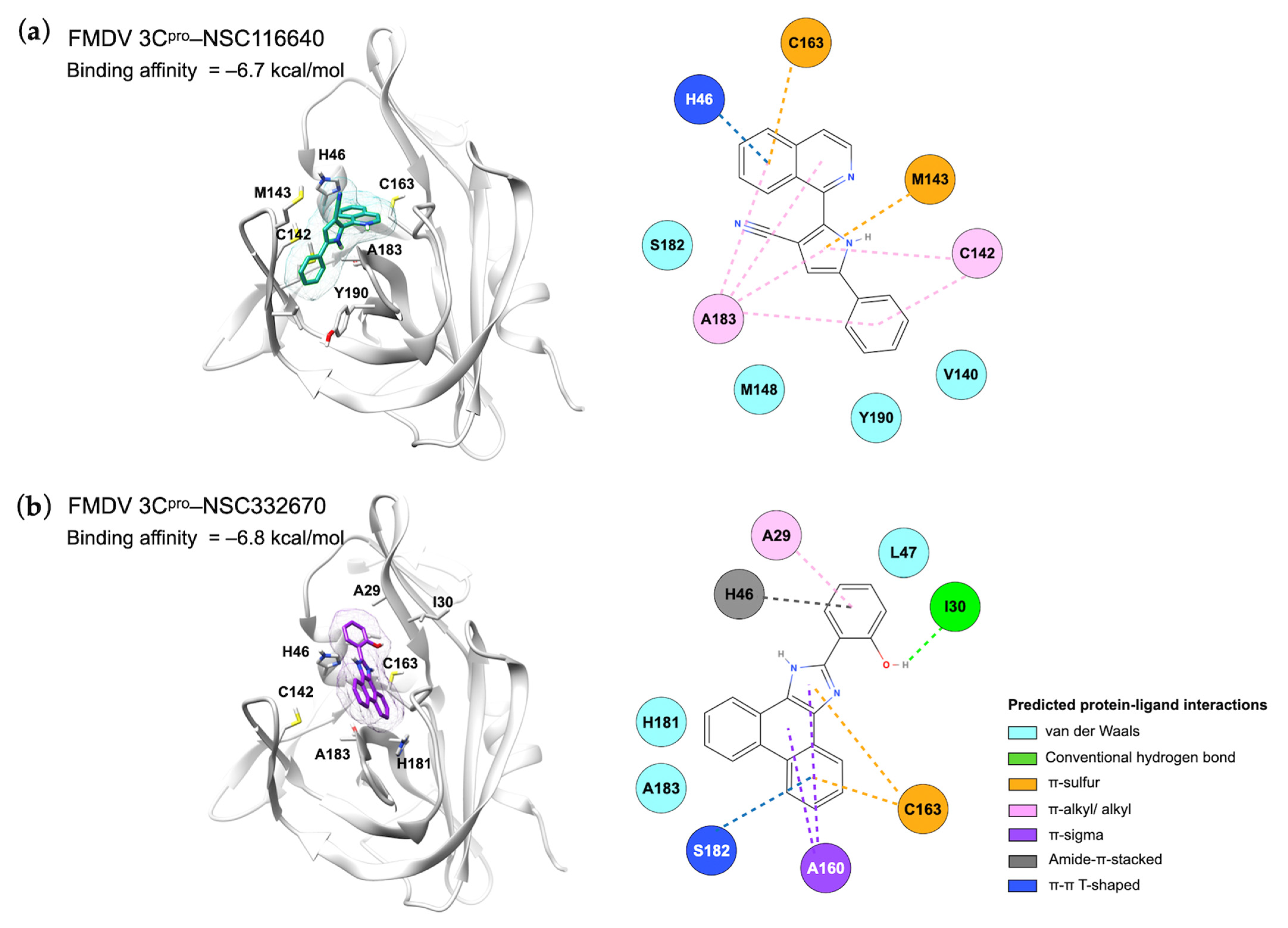
3.4. Protein–Ligand Interactions and Target Prediction of Candidate Compounds
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- OIE. Infection With Foot and Mouth Disease Virus. 28th edition. In Terrestrial Animal Health Code; World Organisation for Animal Health (OIE): Paris, France, 2019; Volume 1, pp. 1–24. [Google Scholar]
- Belsham, G.J. Towards improvements in foot-and-mouth disease vaccine performance. Acta Vet. Scand. 2020, 62, 20. [Google Scholar] [CrossRef]
- King, A.M.Q.; Adams, M.J.; Carstens, E.B.; Lefkowitz, E.J. Order Picornavirales. In Virus Taxonomy; Elsevier: San Diego, CA, USA, 2012; pp. 835–839. [Google Scholar] [CrossRef]
- Zell, R. Picornaviridae—The ever-growing virus family. Arch. Virol. 2018, 163, 299–317. [Google Scholar] [CrossRef] [PubMed]
- Zell, R.; Delwart, E.; Gorbalenya, A.E.; Hovi, T.; King, A.M.Q.; Knowles, N.J.; Lindberg, A.M.; Pallansch, M.A.; Palmenberg, A.C.; Reuter, G.; et al. ICTV Virus Taxonomy Profile: Picornaviridae. J. Gen. Virol. 2017, 98, 2421–2422. [Google Scholar] [CrossRef]
- The Food and Agriculture Organization (FAO). Food-and-Mouth Disease, April–June 2021, Quarterly Report. FAST Reports: Foot-and-Mouth and Similar Transboundary Animal Diseases. 2021. Available online: http://www.fao.org/3/cb5998en/cb5998en.pdf (accessed on 21 January 2023).
- Paton, D.J.; Di Nardo, A.; Knowles, N.J.; Wadsworth, J.; Pituco, E.M.; Cosivi, O.; Rivera, A.M.; Kassimi, L.B.; Brocchi, E.; de Clercq, K.; et al. The history of foot-and-mouth disease virus serotype C: The first known extinct serotype? Virus Evol. 2021, 7, veab009. [Google Scholar] [CrossRef]
- OIE. Application for official recognition by the OIE of free status for Foot and Mouth Disease. In Terrestrial Animal Health Code; World Organisaton of Animal Health (OIE): Paris, France, 2022; Chapter 1.11.; pp. 60–84. [Google Scholar]
- Goris, N.; Vandenbussche, F.; De Clercq, K. Potential of antiviral therapy and prophylaxis for controlling RNA viral infections of livestock. Antiviral Res. 2008, 78, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Sun, S.Q.; Guo, H.C. Biological function of Foot-and-mouth disease virus non-structural proteins and non-coding elements. Virol. J. 2016, 13, 107. [Google Scholar] [CrossRef]
- Yi, J.; Peng, J.; Yang, W.; Zhu, G.; Ren, J.; Li, D.; Zheng, H. Picornavirus 3C—A protease ensuring virus replication and subverting host responses. J. Cell Sci. 2021, 134, jcs253237. [Google Scholar] [CrossRef] [PubMed]
- Birtley, J.R.; Knox, S.R.; Jaulent, A.M.; Brick, P.; Leatherbarrow, R.J.; Curry, S. Crystal structure of foot-and-mouth disease virus 3C protease: New insights into catalytic mechanism and cleavage specificity. J. Biol. Chem. 2005, 280, 11520–11527. [Google Scholar] [CrossRef] [PubMed]
- Dragovich, P.S.; Prins, T.J.; Zhou, R.; Johnson, T.O.; Hua, Y.; Luu, H.T.; Sakata, S.K.; Brown, E.L.; Maldonado, F.C.; Tuntland, T.; et al. Structure-based design, synthesis, and biological evaluation of irreversible human rhinovirus 3C protease inhibitors. 8. Pharmacological optimization of orally bioavailable 2-pyridone-containing peptidomimetics. J. Med. Chem. 2003, 46, 4572–4585. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, L.; Crump, C.; Hayden, F. In vitro activity of pleconaril and AG7088 against selected serotypes and clinical isolates of human rhinoviruses1. Antiviral Res. 2000, 47, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Hayden, F.G.; Turner, R.B.; Gwaltney, J.M.; Chi-Burris, K.; Gersten, M.; Hsyu, P.; Patick, A.K.; Smith, G.J.; Zalman, L.S. Phase II, randomized, double-blind, placebo-controlled studies of ruprintrivir nasal spray 2-percent suspension for prevention and treatment of experimentally induced rhinovirus colds in healthy volunteers. Antimicrob. Agents Chemother. 2003, 47, 3907–3916. [Google Scholar] [CrossRef]
- Binford, S.L.; Weady, P.T.; Maldonado, F.; Brothers, M.A.; Matthews, D.A.; Patick, A.K. In vitro resistance study of rupintrivir, a novel inhibitor of human rhinovirus 3C protease. Antimicrob. Agents Chemother. 2007, 51, 4366–4373. [Google Scholar] [CrossRef] [PubMed]
- Furuta, Y.; Takahashi, K.; Shiraki, K.; Sakamoto, K.; Smee, D.F.; Barnard, D.L.; Gowen, B.B.; Julander, J.G.; Morrey, J.D. T-705 (favipiravir) and related compounds: Novel broad-spectrum inhibitors of RNA viral infections. Antiviral Res. 2009, 82, 95–102. [Google Scholar] [CrossRef]
- Sakamoto, K.; Ohashi, S.; Reiko, Y.; Kazumi, T.; Furuta, Y. The inhibition of FMD virus excretion from the infected pigs by an antiviral agent, T-1105. In FAO Report of the Research Group of the Standing Technical Committee of European Commission for the control of Foot-and-Mouth Disease, Appendix 64; FAO: Paphos, Cyprus, 2006; pp. 418–424. [Google Scholar]
- Theerawatanasirikul, S.; Thangthamniyom, N.; Kuo, C.-J.; Semkum, P.; Phecharat, N.; Chankeeree, P.; Lekcharoensuk, P. Natural phytochemicals, luteolin and isoginkgetin, inhibit 3C protease and infection of FMDV, in silico and in vitro. Viruses 2021, 13, 2118. [Google Scholar] [CrossRef]
- Theerawatanasirikul, S.; Lekcharoensuk, P. Virtual screening of natural compounds targeting proteases of coronaviruses and picornaviruses. In Methods in Pharmacology and Toxicology; Roy, K., Ed.; Springer: New York, NY, USA, 2021; pp. 661–681. [Google Scholar]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera—A visualization system for exploratory research and analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef]
- O’Boyle, N.M.; Banck, M.; James, C.A.; Morley, C.; Vandermeersch, T.; Hutchison, G.R. Open Babel: An open chemical toolbox. J. Cheminform. 2011, 3, 33. [Google Scholar] [CrossRef] [PubMed]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 2009, 31, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Dallakyan, S.; Olson, A.J. Small-molecule library screening by docking with PyRx. Chem. Biol. Methods Protoc. 2015, 1263, 243–250. [Google Scholar]
- Theerawatanasirikul, S.; Lueangaramkul, V.; Thangthamniyom, N.; Chankeeree, P.; Semkum, P.; Lekcharoensuk, P. Andrographolide and deoxyandrographolide inhibit protease and IFN-antagonist activities of foot-and-mouth disease virus 3Cpro. Animals 2022, 12, 1995. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A Simple Method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Lekcharoensuk, P.; Wiriyarat, W.; Petcharat, N.; Lekcharoensuk, C.; Auewarakul, P.; Richt, J.A. Cloned cDNA of A/swine/Iowa/15/1930 internal genes as a candidate backbone for reverse genetics vaccine against influenza A viruses. Vaccine 2012, 30, 1453–1459. [Google Scholar] [CrossRef] [PubMed]
- Semkum, P.; Kaewborisuth, C.; Thangthamniyom, N.; Theerawatanasirikul, S.; Lekcharoensuk, C.; Hansoongnern, P.; Ramasoota, P.; Lekcharoensuk, P. A novel plasmid DNA-based foot and mouth disease virus minigenome for intracytoplasmic mRNA production. Viruses 2021, 13, 1047. [Google Scholar] [CrossRef] [PubMed]
- Van Der Linden, L.; Ulferts, R.; Nabuurs, S.B.; Kusov, Y.; Liu, H.; George, S.; Lacroix, C.; Goris, N.; Lefebvre, D.; Lanke, K.H.W.; et al. Application of a cell-based protease assay for testing inhibitors of picornavirus 3C proteases. Antiviral Res. 2014, 103, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Sariya, L.; Thangthumniyom, N.; Wajjwalku, W.; Chumsing, W.; Ramasoota, P.; Lekcharoensuk, P. Expression of foot and mouth disease virus nonstructural polyprotein 3ABC with inactive 3Cpro in Escherichia coli. Protein Expr. Purif. 2011, 80, 17–21. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef]
- Sander, T.; Freyss, J.; von Korff, M.; Rufener, C. DataWarrior: An open-source program for chemistry aware data visualization and analysis. J. Chem. Inf. Model. 2015, 55, 460–473. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissTargetPrediction: Updated data and new features for efficient prediction of protein targets of small molecules. Nucleic Acids Res. 2019, 47, W357–W364. [Google Scholar] [CrossRef]
- Zhang, J.-H.; Chung, T.D.Y.; Oldenburg, K.R. A Simple statistical parameter for use in evaluation and validation of high throughput screening assays. SLAS Discov. 1999, 4, 67–73. [Google Scholar] [CrossRef]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Deliv. Rev. 1997, 23, 3–25. [Google Scholar] [CrossRef]
- Mendez, D.; Gaulton, A.; Bento, A.P.; Chambers, J.; De Veij, M.; Félix, E.; Magariños, M.P.; Mosquera, J.F.; Mutowo, P.; Nowotka, M.; et al. ChEMBL: Towards direct deposition of bioassay data. Nucleic Acids Res. 2019, 47, D930–D940. [Google Scholar] [CrossRef]
- Francisco-Velilla, R.; Embarc-Buh, A.; Abellan, S.; Martinez-Salas, E. Picornavirus translation strategies. FEBS Open Bio. 2022, 12, 1125–1141. [Google Scholar] [CrossRef] [PubMed]
- Zunszain, P.A.; Knox, S.R.; Sweeney, T.R.; Yang, J.; Roqué-Rosell, N.; Belsham, G.J.; Leatherbarrow, R.J.; Curry, S. insights into cleavage specificity from the crystal structure of foot-and-mouth disease virus 3C protease complexed with a peptide substrate. J. Mol. Biol. 2010, 395, 375–389. [Google Scholar] [CrossRef]
- Curry, S.; Roqué-Rosell, N.; Sweeney, T.R.; Zunszain, P.A.; Leatherbarrow, R.J. Structural analysis of foot-and-mouth disease virus 3C protease: A viable target for antiviral drugs? Biochem. Soc. Trans. 2007, 35, 594–598. [Google Scholar] [CrossRef]
- Belsham, G.J.; McInerney, G.M.; Ross-Smith, N. Foot-and-mouth disease virus 3C protease induces cleavage of translation initiation factors eIF4A and eIF4G within infected cells. J. Virol. 2000, 74, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, P.; Schafer, E.A.; Rieder, E. The nuclear protein Sam68 is cleaved by the FMDV 3C protease redistributing Sam68 to the cytoplasm during FMDV infection of host cells. Virology 2012, 425, 40–52. [Google Scholar] [CrossRef]
- Sweeney, T.R.; Roqué-Rosell, N.; Birtley, J.R.; Leatherbarrow, R.J.; Curry, S. Structural and mutagenic analysis of foot-and-mouth disease virus 3C protease reveals the role of the β-ribbon in proteolysis. J. Virol. 2007, 81, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Ekanayaka, P.; Shin, S.H.; Weeratunga, P.; Lee, H.; Kim, T.-H.; Chathuranga, K.; Subasinghe, A.; Park, J.-H.; Lee, J.-S. Foot-and-Mouth Disease Virus 3C Protease Antagonizes Interferon Signaling and C142T Substitution Attenuates the FMD Virus. Front. Microbiol. 2021, 12, 737031. [Google Scholar] [CrossRef]
- Yaacoub, K.; Guillaudeux, T.; Daniellou, R.; Lafite, P.; Aci-Seche, S.; Bonnet, P. Selective C-Flip Inhibitors as Anticancer Agents. Patent US 20190282563, 19 September 2019. [Google Scholar]
- Li, X.; Zhang, Z.; Wang, Z.; Gutiérrez-Castrellón, P.; Shi, H. Cell deaths: Involvement in the pathogenesis and intervention therapy of COVID-19. Signal Transduct. Target. Ther. 2022, 7, 186. [Google Scholar] [CrossRef]
- Mongkol, W.; Arunyawat, U.; Surat, W.; Kubera, A. Active compounds against Anopheles minimus carboxypeptidase b for malaria transmission-blocking strategy. J. Med. Entomol. 2015, 52, 1322–1332. [Google Scholar] [CrossRef] [PubMed]
- Kapitzky, L.; Beltrao, P.; Berens, T.J.; Gassner, N.; Zhou, C.; Wüster, A.; Wu, J.; Babu, M.M.; Elledge, S.J.; Toczyski, D.; et al. Cross-species chemogenomic profiling reveals evolutionarily conserved drug mode of action. Mol. Syst. Biol. 2010, 6, 451. [Google Scholar] [CrossRef]
- Daina, A.; Zoete, V. A BOILED-Egg to predict gastrointestinal absorption and brain penetration of small molecules. ChemMedChem 2016, 11, 1117–1121. [Google Scholar] [CrossRef] [PubMed]


| NCI ID and IUPAC Name | Structure | Molecular Weight (g/mol) | H-Bond Donor Count | H-Bond Acceptor Count | Rotatable Bond Count | Log-P | TSPA (Å) |
|---|---|---|---|---|---|---|---|
| NSC116640 2-isoquinolin-1-yl-5-phenyl-1H-pyrrole-3-carbonitrile (Binding affinity = −6.7 kcal/mol) | 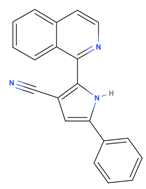 | 295.34 | 1 | 2 | 2 | 4.769 | 52.47 |
| NSC332670 2-isoquinolin-1-yl-5-phenyl-1H-pyrrole-3-carbonitrile (Binding affinity = −6.7 kcal/mol) |  | 310.35 | 2 | 2 | 1 | 5.242 | 48.91 |
| NSC79451 2-Hydroxy-N-(2-methyl-5-nitrophenyl)-3-nitrobenzamide (Binding affinity = −6.6 kcal/mol) |  | 317.25 | 2 | 6 | 5 | 2.769 | 140.97 |
| NSC681744 N-[6-[benzoyl-[cyano(phenyl)methyl]amino]hexyl]-N-[cyano(phenyl)methyl]benzamide (Binding affinity = −6.7 kcal/mol) |  | 554.68 | 0 | 4 | 15 | 7.361 | 88.2 |
| NSC64672 8-[(2E)-2-[(4-hydroxy-3-methoxyphenyl)methylidene]hydrazinyl]-1,3-dimethyl-7H-purine-2,6-dione (Binding affinity = −6.7 kcal/mol) | 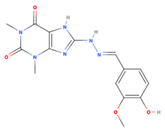 | 334.33 | 3 | 9 | 4 | 0.12 | 126.53 |
| NSC119805 2-[(E)-[(E)-[(E)-3-(2-nitrophenyl)prop-2-enylidene]hydrazinylidene] methyl]phenol (Binding affinity = −6.7 kcal/mol) |  | 295.29 | 1 | 5 | 5 | 3.419 | 88.09 |
| NSC331757 N-[5-(diethylamino)pentan-2-yl]-9,10-dioxoanthracene-2-carboxamide;hydrochloride (Binding affinity = −6.8 kcal/mol) |  | 428.96 | 1 | 4 | 9 | 4.124 | 66.48 |
| Reference values (Lipinski’s rule [35]) | <500 | <5 | <10 | <10 | <5 | <140 |
| Compounds | CC50 (µM) 1 | EC50 (µM) 2 | ||
|---|---|---|---|---|
| Post Entry | Co-Treatment | Pre-Treatment | ||
| NSC116640 | 210.70 ± 0.17 | 2.88 ± 0.17 | 5.74 ± 0.23 | 7.27 ± 0.86 |
| NSC332670 | 65.82 ± 0.06 | 5.92 ± 0.20 | 2.04 ± 0.02 | 7.18 ± 0.98 |
| NSC79451 | 32.79 ± 0.3 | I | 1.56 ± 0.03 | I |
| NSC681744 | 124.00 ± 0.5 | I | 4.83 ± 0.08 | I |
| NSC64672 | 130.09 ± 2.30 | I | I | I |
| NSC119805 | 82.45 ± 0.40 | I | I | I |
| NSC331757 | 62.78 ± 0.87 | I | I | I |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theerawatanasirikul, S.; Lueangaramkul, V.; Pantanam, A.; Mana, N.; Semkum, P.; Lekcharoensuk, P. Small Molecules Targeting 3C Protease Inhibit FMDV Replication and Exhibit Virucidal Effect in Cell-Based Assays. Viruses 2023, 15, 1887. https://doi.org/10.3390/v15091887
Theerawatanasirikul S, Lueangaramkul V, Pantanam A, Mana N, Semkum P, Lekcharoensuk P. Small Molecules Targeting 3C Protease Inhibit FMDV Replication and Exhibit Virucidal Effect in Cell-Based Assays. Viruses. 2023; 15(9):1887. https://doi.org/10.3390/v15091887
Chicago/Turabian StyleTheerawatanasirikul, Sirin, Varanya Lueangaramkul, Achiraya Pantanam, Natjira Mana, Ploypailin Semkum, and Porntippa Lekcharoensuk. 2023. "Small Molecules Targeting 3C Protease Inhibit FMDV Replication and Exhibit Virucidal Effect in Cell-Based Assays" Viruses 15, no. 9: 1887. https://doi.org/10.3390/v15091887





