Extensive Survey and Analysis of Factors Associated with Presence of Antibodies to Orthoebolaviruses in Bats from West and Central Africa
Abstract
:1. Introduction
2. Materials and Methods
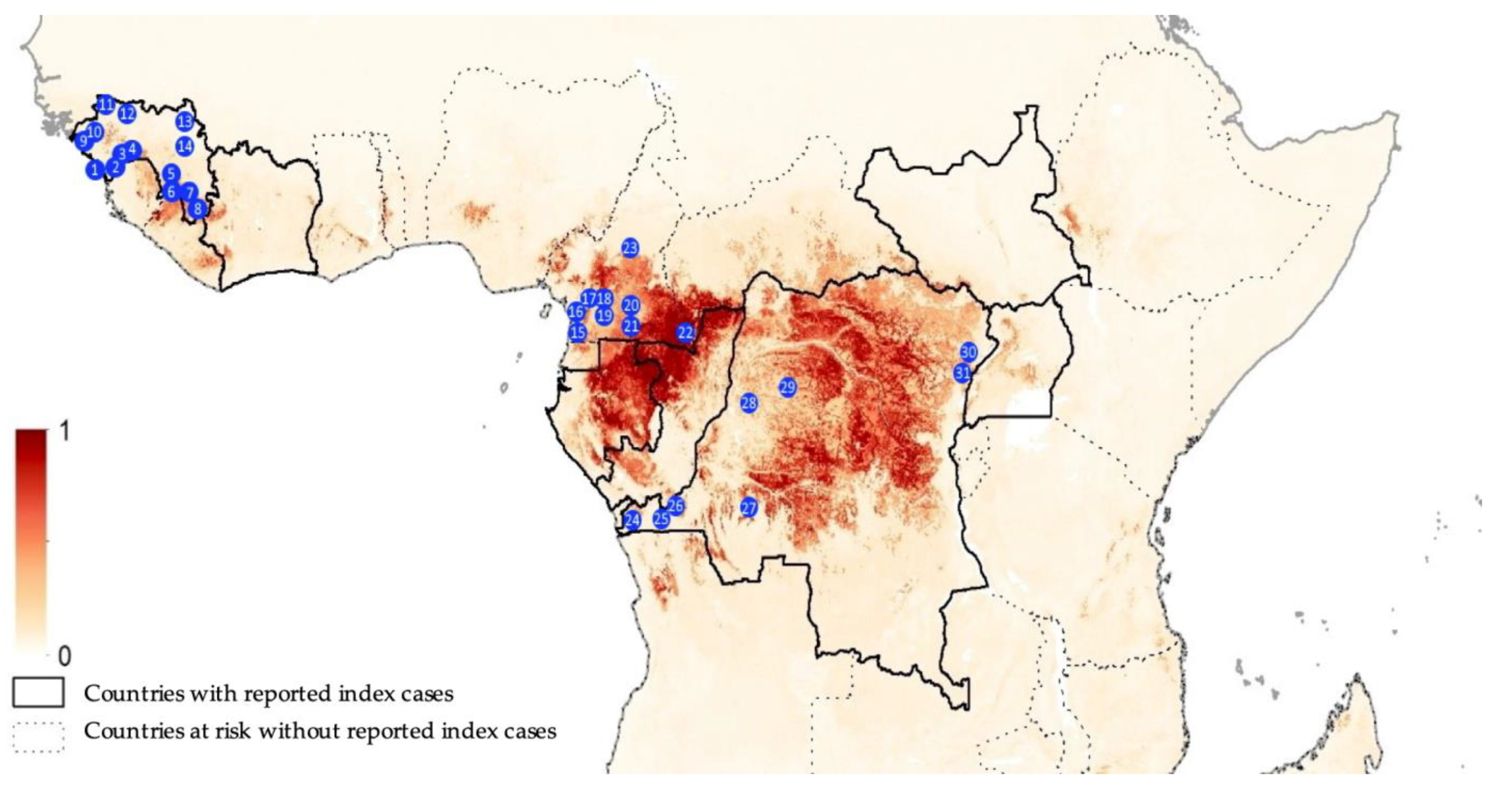
2.1. Collection Sites
2.2. Screening for Orthoebolavirus Antibodies
2.3. Molecular Confirmation of Bat Species
2.4. Statistical Analysis to Study Factors Associated with Seropositivity
3. Results
3.1. Bat Species and Sample Sites
3.2. Antibodies against Different Orthoebolavirus Antigens
3.3. Factors Associated with Antibodies to Orthoebolaviruses
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- CDC. History of Ebola Virus Disease (EVD) Outbreaks. Available online: https://www.cdc.gov/vhf/ebola/history/chronology.html (accessed on 31 July 2023).
- Biedenkopf, N.; Bukreyev, A.; Chandran, K.; Di Paola, N.; Formenty, P.B.H.; Griffiths, A.; Hume, A.J.; Mühlberger, E.; Netesov, S.V.; Palacios, G.; et al. Renaming of genera Ebolavirus and Marburgvirus to Orthoebolavirus and Orthomarburgvirus, respectively, and introduction of binomial species names within family Filoviridae. Arch. Virol. 2023, 168, 220. [Google Scholar] [CrossRef] [PubMed]
- Keita, A.K.; Koundouno, F.R.; Faye, M.; Düx, A.; Hinzmann, J.; Diallo, H.; Ayouba, A.; Le Marcis, F.; Soropogui, B.; Ifono, K.; et al. Resurgence of Ebola virus in 2021 in Guinea suggests a new paradigm for outbreaks. Nature 2021, 597, 539–543. [Google Scholar] [CrossRef] [PubMed]
- Mbala-Kingebeni, P.; Pratt, C.; Mutafali-Ruffin, M.; Pauthner, M.G.; Bile, F.; Nkuba-Ndaye, A.; Black, A.; Kinganda-Lusamaki, E.; Faye, M.; Aziza, A.; et al. Ebola Virus Transmission Initiated by Relapse of Systemic Ebola Virus Disease. N. Engl. J. Med. 2021, 384, 1240–1247. [Google Scholar] [CrossRef] [PubMed]
- Pourrut, X.; Délicat, A.; Rollin, P.E.; Ksiazek, T.G.; Gonzalez, J.-P.; Leroy, E.M. Spatial and Temporal Patterns of Zaire Ebolavirus Antibody Prevalence in the Possible Reservoir Bat Species. J. Infect. Dis. 2007, 196, S176–S183. [Google Scholar] [CrossRef]
- Pourrut, X.; Souris, M.; Towner, J.S.; Rollin, P.E.; Nichol, S.T.; Gonzalez, J.-P.; Leroy, E. Large Serological Survey Showing Cocirculation of Ebola and Marburg Viruses in Gabonese Bat Populations; and a High Seroprevalence of Both Viruses in Rousettus aegyptiacus. BMC Infect. Dis. 2009, 9, 159. [Google Scholar] [CrossRef]
- Hayman, D.T.S.; Yu, M.; Crameri, G.; Wang, L.-F.; Suu-Ire, R.; Wood, J.L.N.; Cunningham, A.A. Ebola Virus Antibodies in Fruit Bats; Ghana; West Africa. Emerg. Infect. Dis. 2012, 18, 1207–1209. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Miyamoto, H.; Nakayama, E.; Yoshida, R.; Nakamura, I.; Sawa, H.; Ishii, A.; Thomas, Y.; Nakagawa, E.; Matsuno, K.; et al. Seroepidemiological Prevalence of Multiple Species of Filoviruses in Fruit Bats (Eidolon helvum) Migrating in Africa. J. Infect. Dis. 2015, 212 (Suppl. 2), S101–S108. [Google Scholar] [CrossRef]
- De Nys, H.M.; Kingebeni, P.M.; Keita, A.K.; Butel, C.; Thaurignac, G.; Villabona-Arenas, C.J.; Lemarcis, T.; Geraerts, M.; Vidal, N.; Esteban, A.; et al. Survey of Ebola Viruses in Frugivorous and Insectivorous Bats in Guinea; Cameroon; and the Democratic Republic of the Congo; 2015–2017. Emerg. Infect. Dis. 2018, 24, 2228–2240. [Google Scholar] [CrossRef]
- Seifert, S.N.; Fischer, R.J.; Kuisma, E.; Badzi Nkoua, C.; Bounga, G.; Akongo, M.J.; Schulz, J.E.; Escudero-Pérez, B.; Akoundzie, B.J.; Ampiri, V.R.B.; et al. Zaire ebolavirus surveillance near the Bikoro region of the Democratic Republic of the Congo during the 2018 outbreak reveals presence of seropositive bats. PLoS Negl. Trop. Dis. 2022, 16, e0010504. [Google Scholar] [CrossRef]
- Leroy, E.M.; Kumulungui, B.; Pourrut, X.; Rouquet, P.; Hassanin, A.; Yaba, P.; Délicat, A.; Paweska, J.T.; Gonzalez, J.-P.; Swanepoel, R. Fruit bats as reservoirs of Ebola virus. Nature 2005, 438, 575–576. [Google Scholar] [CrossRef]
- Leroy, E.M.; Rouquet, P.; Formenty, P.; Souquière, S.; Kilbourne, A.; Froment, J.M.; Bermejo, M.; Smit, S.; Karesh, W.; Swanepoel, R.; et al. Multiple Ebola virus transmission events and rapid decline of central African wildlife. Science 2004, 303, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Rouquet, P.; Froment, J.M.; Bermejo, M.; Kilbourn, A.; Karesh, W.; Reed, P.; Kumulungui, B.; Yaba, P.; Délicat, A.; Rollin, P.E.; et al. Wild animal mortality monitoring and human Ebola outbreaks; Gabon and Republic of Congo; 2001–2003. Emerg. Infect. Dis. 2005, 11, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Bermejo, M.; Rodríguez-Teijeiro, J.D.; Illera, G.; Barroso, A.; Vilà, C.; Walsh, P.D. Ebola outbreak killed 5000 gorillas. Science 2006, 314, 1564. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Pourrut, X.; Albariño, C.G.; Nkogue, C.N.; Bird, B.H.; Grard, G.; Ksiazek, T.G.; Gonzalez, J.-P.; Nichol, S.T.; Leroy, E.M. Marburg Virus Infection Detected in a Common African Bat. PLoS ONE 2007, 2, e764. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Amman, B.R.; Sealy, T.K.; Carroll, S.A.R.; Comer, J.A.; Kemp, A.; Swanepoel, R.; Paddock, C.D.; Balinandi, S.; Khristova, M.L.; et al. Isolation of Genetically Diverse Marburg Viruses from Egyptian Fruit Bats. PLoS Pathog. 2009, 5, e1000536. [Google Scholar] [CrossRef]
- Amman, B.R.; Nyakarahuka, L.; McElroy, A.K.; Dodd, K.A.; Sealy, T.K.; Schuh, A.J.; Shoemaker, T.R.; Balinandi, S.; Atimnedi, P.; Kaboyo, W.; et al. Marburgvirus Resurgence in Kitaka Mine Bat Population after Extermination Attempts; Uganda. Emerg. Infect. Dis. 2014, 20, 1761–1764. [Google Scholar] [CrossRef]
- Amman, B.R.; Bird, B.H.; Bakarr, I.A.; Bangura, J.; Schuh, A.J.; Johnny, J.; Sealy, T.K.; Conteh, I.; Koroma, A.H.; Foday, I.; et al. Isolation of Angola-like Marburg Virus from Egyptian Rousette Bats from West Africa. Nat. Commun. 2020, 11, 510. [Google Scholar] [CrossRef]
- Makenov, M.T.; Boumbaly, S.; Tolno, F.R.; Sacko, N.; N’Fatoma, L.T.; Mansare, O.; Kolie, B.; Stukolova, O.A.; Morozkin, E.S.; Kholodilov, I.S.; et al. Marburg virus in Egyptian Rousettus bats in Guinea: Investigation of Marburg virus outbreak origin in 2021. PLoS Negl. Trop. Dis. 2023, 17, e0011279. [Google Scholar] [CrossRef]
- Goldstein, T.; Anthony, S.J.; Gbakima, A.; Bird, B.H.; Bangura, J.; Tremeau-Bravard, A.; Belaganahalli, M.N.; Wells, H.L.; Dhanota, J.K.; Liang, E.; et al. The Discovery of Bombali Virus Adds Further Support for Bats as Hosts of Ebolaviruses. Nat. Microbiol. 2018, 3, 1084–1089. [Google Scholar] [CrossRef]
- Forbes, K.M.; Al, K.M.F.E.; Jääskeläinen, A.J.; Abdurahman, S.; Ogola, J.; Masika, M.M.; Kivistö, I.; Alburkat, H.; Plyusnin, I.; Levanov, L.; et al. Bombali Ebola Virus in Mops condylurus Bat; Kenya. Emerg. Infect. Dis. 2019, 25, 955. [Google Scholar] [CrossRef]
- Karan, L.S.; Makenov, M.T.; Korneev, M.G.; Sacko, N.; Boumbaly, S.; Yakovlev, S.A.; Kourouma, K.; Bayandin, R.B.; Gladysheva, A.V.; Shipovalov, A.V.; et al. Bombali Virus in Mops condylurus Bats; Guinea. Emerg. Infect. Dis. 2019, 25, 1774. [Google Scholar] [CrossRef] [PubMed]
- Negredo, A.; Palacios, G.; Vázquez-Morón, S.; González, F.; Dopazo, H.; Molero, F.; Juste, J.; Quetglas, J.; Savji, N.; Martínez, M.D.L.C.; et al. Discovery of an Ebolavirus-Like Filovirus in Europe. PLoS Pathog. 2011, 7, e1002304. [Google Scholar] [CrossRef] [PubMed]
- Jayme, S.I.; Field, H.E.; de Jong, C.; Olival, K.J.; Marsh, G.; Tagtag, A.M.; Hughes, T.; Bucad, A.C.; Barr, J.; Azul, R.R.; et al. Molecular evidence of Ebola Reston virus infection in Philippine bats. Virol. J. 2015, 12, 107. [Google Scholar] [CrossRef]
- Yang, X.-L.; Zhang, Y.-Z.; Jiang, R.-D.; Guo, H.; Zhang, W.; Li, B.; Wang, N.; Wang, L.; Waruhiu, C.; Zhou, J.-H.; et al. Genetically Diverse Filoviruses in Rousettus and Eonycteris spp. Bats; China; 2009 and 2015. Emerg. Infect. Dis. 2017, 23, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Kemenesi, G.; Kurucz, K.; Dallos, B.; Zana, B.; Földes, F.; Boldogh, S.; Görföl, T.; Carroll, M.W.; Jakab, F. Re-emergence of Lloviu virus in Miniopterus schreibersii bats; Hungary; 2016. Emerg. Microbes Infect. 2018, 7, 1–4. [Google Scholar] [CrossRef]
- Hayman, D.T. Bats as Viral Reservoirs. Annu. Rev. Virol. 2016, 3, 77–99. [Google Scholar] [CrossRef]
- Gloza-Rausch, F.; Ipsen, A.; Seebens, A.; Göttsche, M.; Panning, M.; Drexler, J.F.; Petersen, N.; Annan, A.; Grywna, K.; Müller, M.; et al. Detection and Prevalence Patterns of Group I Coronaviruses in Bats; Northern Germany. Emerg. Infect. Dis. 2008, 14, 626–631. [Google Scholar] [CrossRef]
- Plowright, R.K.; Field, H.E.; Smith, C.; Divljan, A.; Palmer, C.; Tabor, G.; Daszak, P.; Foley, J.E. Reproduction and nutritional stress are risk factors for Hendra virus infection in little red flying foxes (Pteropus scapulatus). Proc. R. Soc. B Biol. Sci. 2008, 275, 861–869. [Google Scholar] [CrossRef]
- Dietrich, M.; Wilkinson, D.A.; Benlali, A.; Lagadec, E.; Ramasindrazana, B.; Dellagi, K.; Tortosa, P. Leptospira and paramyxovirus infection dynamics in a bat maternity enlightens pathogen maintenance in wildlife. Environ. Microbiol. 2015, 17, 4280–4289. [Google Scholar] [CrossRef]
- Montecino-Latorre, D.; Goldstein, T.; Gilardi, K.; Wolking, D.; Van Wormer, E.; Kazwala, R.; Ssebide, B.; Nziza, J.; Sijali, Z.; Cranfield, M.; et al. Reproduction of East-African bats may guide risk mitigation for coronavirus spillover. One Health Outlook 2020, 2, 2. [Google Scholar] [CrossRef]
- Meta Djomsi, D.; Lacroix, A.; Soumah, A.K.; Kinganda Lusamaki, E.; Mesdour, A.; Raulino, R.; Esteban, A.; Ndong Bass, I.; Mba Djonzo, F.A.; Goumou, S.; et al. Coronaviruses Are Abundant and Genetically Diverse in West and Central African Bats; including Viruses Closely Related to Human Coronaviruses. Viruses 2023, 15, 337. [Google Scholar] [CrossRef]
- Amman, B.R.; Carroll, S.A.; Reed, Z.D.; Sealy, T.K.; Balinandi, S.; Swanepoel, R.; Kemp, A.; Erickson, B.R.; Comer, J.A.; Campbell, S.; et al. Seasonal Pulses of Marburg Virus Circulation in Juvenile Rousettus aegyptiacus Bats Coincide with Periods of Increased Risk of Human Infection. PLoS Pathog. 2012, 8, e1002877. [Google Scholar] [CrossRef]
- Djomsi, D.M.; Mba Djonzo, F.A.; Ndong Bass, I.; Champagne, M.; Lacroix, A.; Thaurignac, G.; Esteban, A.; De Nys, H.; Bourgarel, M.; Akoachere, J.F.; et al. Dynamics of Antibodies to Ebolaviruses in an Eidolon helvum Bat Colony in Cameroon. Viruses 2022, 14, 560. [Google Scholar] [CrossRef]
- Pigott, D.M.; Millear, A.I.; Earl, L.; Morozoff, C.; Han, B.A.; Shearer, F.M.; Weiss, D.J.; Brady, O.J.; Kraemer, M.U.; Moyes, C.L.; et al. Updates to the zoonotic niche map of Ebola virus disease in Africa. Elife 2016, 5, e16412. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, A.; Mbala Kingebeni, P.; Ndimbo Kumugo, S.P.; Lempu, G.; Butel, C.; Serrano, L.; Vidal, N.; Thaurignac, G.; Esteban, A.; Mukadi Bamuleka, D.; et al. Investigating the Circulation of Ebola Viruses in Bats during the Ebola Virus Disease Outbreaks in the Equateur and North Kivu Provinces of the Democratic Republic of Congo from 2018. Pathogens 2021, 10, 557. [Google Scholar] [CrossRef] [PubMed]
- Ayouba, A.; Touré, A.; Butel, C.; Keita, A.K.; Binetruy, F.; Sow, M.S.; Foulongne, V.; Delaporte, E.; Peeters, M. Development of a Sensitive and Specific Serological Assay Based on Luminex Technology for Detection of Antibodies to Zaire Ebola Virus. J. Clin. Microbiol. 2017, 55, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Irwin, D.M.; Kocher, T.D.; Wilson, A.C. Evolution of the Cytochrome b Gene of Mammals. J. Mol. Evol. 1991, 32, 128–144. [Google Scholar] [CrossRef]
- Van der Kuyl, A.C.; Kuiken, C.L.; Dekker, J.T.; Goudsmit, J. Phylogeny of African monkeys based upon mitochondrial 12S rRNA sequences. J. Mol. Evol. 1995, 40, 173–180. [Google Scholar] [CrossRef]
- Trifinopoulos, J.; Nguyen, L.T.; von Haeseler, A.; Minh, B.Q. W-IQ-TREE: A fast online phylogenetic tool for maximum likelihood analysis. Nucleic Acids Res. 2016, 44, W232–W235. [Google Scholar] [CrossRef]
- Nesi, N.; Nakouné, E.; Cruaud, C.; Hassanin, A. DNA Barcoding of African Fruit Bats (Mammalia; Pteropodidae). The Mitochondrial Genome Does Not Provide a Reliable Discrimination between Epomophorus gambianus and Micropteropus pusillus. C. R. Biol. 2011, 334, 544–555. [Google Scholar] [CrossRef]
- Diallo, M.S.K.; Ayouba, A.; Keita, A.K.; Thaurignac, G.; Sow, M.S.; Kpamou, C.; Barry, T.A.; Msellati, P.; Etard, J.F.; Peeters, M.; et al. Temporal evolution of the humoral antibody response after Ebola virus disease in Guinea: A 60-month observational prospective cohort study. Lancet Microbe 2021, 2, e676–e684. [Google Scholar] [CrossRef] [PubMed]
- Schuh, A.J.; Amman, B.R.; Sealy, T.S.; Flietstra, T.D.; Guito, J.C.; Nichol, S.T.; Towner, J.S. Comparative analysis of serologic cross-reactivity using convalescent sera from filovirus-experimentally infected fruit bats. Sci. Rep. 2019, 9, 6707. [Google Scholar] [CrossRef] [PubMed]
- Penas, J.A.; Miranda, M.E.; De Los Reyes, V.C.; Sucaldito, M.N.L.; Magpantay, R.L. Risk assessment of Ebola Reston virus in humans in the Philippines. West. Pac. Surveill. Response J. 2019, 10, 1–8. [Google Scholar] [CrossRef]
- Bodmer, B.S.; Breithaupt, A.; Heung, M.; Brunetti, J.E.; Henkel, C.; Müller-Guhl, J.; Rodríguez, E.; Wendt, L.; Winter, S.L.; Vallbracht, M.; et al. In vivo characterization of the novel ebolavirus Bombali virus suggests a low pathogenic potential for humans. Emerg Microbes Infect. 2023, 12, 2164216. [Google Scholar] [CrossRef]
- Laing, E.D.; Mendenhall, I.H.; Linster, M.; Low, D.H.W.; Chen, Y.; Yan, L.; Sterling, S.L.; Borthwick, S.; Neves, E.S.; Lim, J.S.L.; et al. Serologic, Evidence of Fruit Bat Exposure to Filoviruses; Singapore; 2011–2016. Emerg. Infect. Dis. 2018, 24, 122. [Google Scholar] [CrossRef] [PubMed]
- Dovih, P.; Laing, E.D.; Chen, Y.; Low, D.H.W.; Ansil, B.R.; Yang, X.; Shi, Z.; Broder, C.C.; Smith, G.J.D.; Linster, M.; et al. Filovirus-reactive antibodies in humans and bats in Northeast India imply zoonotic spillover. PLoS Negl. Trop. Dis. 2019, 13, e0007733. [Google Scholar] [CrossRef] [PubMed]
- Brook, C.E.; Ranaivoson, H.C.; Broder, C.C.; Cunningham, A.A.; Héraud, J.M.; Peel, A.J.; Gibson, L.; Wood, J.L.N.; Metcalf, C.J.; Dobson, A.P. Disentangling serology to elucidate henipa- and filovirus transmission in Madagascar fruit bats. J. Anim. Ecol. 2019, 88, 1001–1016. [Google Scholar] [CrossRef]
- Schulz, J.E.; Seifert, S.N.; Thompson, J.T.; Avanzato, V.; Sterling, S.L.; Yan, L.; Letko, M.C.; Matson, M.J.; Fischer, R.J.; Tremeau-Bravard, A.; et al. Serological Evidence for Henipa-like and Filo-like Viruses in Trinidad Bats. J. Infect. Dis. 2020, 221 (Suppl. 4), S375–S382. [Google Scholar] [CrossRef]
- Barr, J.; Boyd, V.; Todd, S.; Smith, I.; Prada, D.; O’Dea, M.; Jackson, B.; Pearce, L.; Adams, T.E.; Vanderduys, E.; et al. Detection of filovirus-reactive antibodies in Australian bat species. J. Gen. Virol. 2022, 103, 001785. [Google Scholar] [CrossRef]
- Cappelle, J.; Furey, N.; Hoem, T.; Ou, T.P.; Lim, T.; Hul, V.; Heng, O.; Chevalier, V.; Dusart, P.; Duong, V. Longitudinal monitoring in Cambodia suggests higher circulation of alpha and betacoronaviruses in juvenile and immature bats of three species. Sci. Rep. 2021, 11, 24145. [Google Scholar] [CrossRef]
- Hayman, D.T.S. Biannual birth pulses allow filoviruses to persist in bat populations. Proc. R. Soc. B Biol. Sci. 2015, 282, 20142591. [Google Scholar] [CrossRef] [PubMed]
- Reed Hranac, C.; Marshall, J.C.; Monadjem, A.; Hayman, D.T.S. Predicting Ebola virus disease risk and the role of African bat birthing. Epidemics 2019, 29, 100366. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.E.; Schuh, A.J.; Amman, B.R.; Sealy, T.K.; Zaki, S.R.; Nichol, S.T.; Towner, J.S. Experimental Inoculation of Egyptian Rousette Bats (Rousettus aegyptiacus) with Viruses of the Ebolavirus and Marburgvirus Genera. Viruses 2015, 7, 3420–3442. [Google Scholar] [CrossRef] [PubMed]
- Science, this Bat Species May Be the Source of the Ebola Epidemic That Killed more than 11,000 People in West Africa. Available online: https://www.science.org/content/article/bat-species-may-be-source-ebola-epidemic-killed-more-11000-people-west-africa (accessed on 31 July 2023).
- Bokelmann, M.; Vogel, U.; Debeljak, F.; Düx, A.; Riesle-Sbarbaro, S.; Lander, A.; Wahlbrink, A.; Kromarek, N.; Neil, S.; Couacy-Hymann, E.; et al. Tolerance and Persistence of Ebola Virus in Primary Cells from Mops condylurus; a Potential Ebola Virus Reservoir. Viruses 2021, 13, 2186. [Google Scholar] [CrossRef] [PubMed]
- Hermida Lorenzo, R.J.; Cadar, D.; Koundouno, F.R.; Juste, J.; Bialonski, A.; Baum, H.; García-Mudarra, J.L.; Hakamaki, H.; Bencsik, A.; Nelson, E.V.; et al. Metagenomic Snapshots of Viral Components in Guinean Bats. Microorganisms 2021, 9, 599. [Google Scholar] [CrossRef]
- Swanepoel, R.; Leman, P.A.; Burt, F.J.; Zachariades, N.A.; Braack, L.E.; Ksiazek, T.G.; Rollin, P.E.; Zaki, S.R.; Peters, C.J. Experimental inoculation of plants and animals with Ebola virus. Emerg. Infect. Dis. 1996, 2, 321–325. [Google Scholar] [CrossRef]
- Peel, A.J.; Wood, J.L.N.; Baker, K.S.; Breed, A.C.; de Carvalho, A.; Fernández-Loras, A.; Gabrieli, H.S.; Gembu, G.-C.; Kakengi, V.A.; Kaliba, P.M.; et al. How Does Africa’s Most Hunted Bat Vary Across the Continent? Population Traits of the Straw-Coloured Fruit Bat (Eidolon helvum) and Its Interactions with Humans. Acta Chiropterol. 2017, 19, 77–92. [Google Scholar] [CrossRef]
- Kamins, A.; Restif, O.; Ntiamoa-Baidu, Y.; Suu-Ire, R.; Hayman, D.; Cunningham, A.; Wood, J.; Rowcliffe, M. Uncovering the fruit bat bushmeat commodity chain and the true extent of fruit bat hunting in Ghana; West Africa. Biol. Conserv. 2011, 144, 3000–3008. [Google Scholar] [CrossRef]
- Baudel, H.; De Nys, H.; Ngole, E.M.; Peeters, M.; Desclaux, A. Understanding Ebola virus and other zoonotic transmission risks through human–bat contacts: Exploratory study on knowledge; attitudes and practices in Southern Cameroon. Zoonoses Public Health 2019, 66, 288–295. [Google Scholar] [CrossRef]
- Frick, W.F.; Kingston, T.; Flanders, J. A review of the major threats and challenges to global bat conservation. Ann. N. Y. Acad. Sci. 2020, 1469, 5–25. [Google Scholar] [CrossRef]
- Euren, J.; Bangura, J.; Gbakima, A.; Sinah, M.; Yonda, S.; Lange, C.E.; McIver, D.J.; LeBreton, M.; Wolking, D.; Grigorescu Monagin, C.; et al. Human Interactions with Bat Populations in Bombali; Sierra Leone. EcoHealth 2020, 17, 292–301. [Google Scholar] [CrossRef] [PubMed]





| Guinea | Cameroon | DRC | Total | ||
|---|---|---|---|---|---|
| Frugivorous bats | |||||
| Pteropodidae | |||||
| Eidolon helvum | 178 | 1020 | 454 | 1652 | |
| Epomophorus sp. a | 406 | 19 | 189 | 614 | |
| Epomops sp. b | 21 | 846 | 209 | 1076 | |
| Hypsignathus monstrosus | 18 | 542 | 12 | 572 | |
| Lissonycteris angolensis | 35 | 96 | 55 | 186 | |
| Micropteropus pusillus | 21 | 32 | 203 | 256 | |
| Myonycteris torquata | 1 | 294 | 102 | 397 | |
| Rousettus aegyptiacus | 551 | 584 | 5 | 1140 | |
| Other frugivorous species c | 3 | 44 | 32 | 79 | |
| Subtotal | 1234 | 3477 | 1261 | 5972 | |
| Insectivorous bats | |||||
| Molossidae | |||||
| Chaerephon/Mops d | 1039 | 368 | 21 | 1428 | |
| Hipposideridae | |||||
| Hipposideros sp. d | 435 | 925 | 231 | 1591 | |
| Miniopteridae | |||||
| Miniopterus sp. d | 46 | 9 | 209 | 264 | |
| Nycteridae | |||||
| Nycteris sp. d | 79 | 7 | 2 | 88 | |
| Rhinolophidae | |||||
| Rhinolophus sp. d | 74 | 71 | 9 | 154 | |
| Other insectivorous species e | 37 | 29 | 31 | 97 | |
| Subtotal | 1710 | 1409 | 503 | 3622 | |
| Total | 2944 | 4886 | 1764 | 9594 | |
| Genus/Species | N Tested | NP EBOV | GP EBOV-k | GP-EBOV-m | VP-EBOV | NP SUDV | GP SUDV | VP SUDV | GP BDBV | VP BDBV | GP RESTV | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Frugivorous bats | ||||||||||||
| Pteropodidae | ||||||||||||
| Eidolon helvum | 1652 | 20–61 (1.2–3.7) | 130–552 (7.9–33.4) | 99–298 (6–18) | 5–38 (0.3–2.3) | 18–45 (1.1–2.7) | 125–722 (7.6–43.7) | 32–96 (1.9–5.8) | 63–460 (3.8–27.8) | 0–3 (0–0.2) | 9–6 (0.5–0.4) | 233–795 (14.1–48.1) |
| Epomophorus sp. a | 614 | 1–6 (0.2–1) | 2–25 (0.3–4.1) | 2–14 (0.3–2.3) | 1–2 (0.2–0.3) | 1–3 (0.2–0.5) | 2–49 (0.3–8) | 6–13 (1–2.1) | 3–25 (0.5–4.1) | 0–0 (0–0) | 0–0 (0–0) | 18–74 (2.9–12.1) |
| Epomops sp. b | 1076 | 5–7 (0.5–0.7) | 1–7 (0.1–0.7) | 2–4 (0.2–0.4) | 4–14 (0.4–1.3) | 7–8 (0.7–0.7) | 0–21 (0–2) | 6–12 (0.6–1.1) | 1–8 (0.1–0.7) | 1–3 (0.1–0.3) | 1–0 (0.1–0) | 24–62 (2.2–5.8) |
| Hypsignathus monstrosus | 572 | 2–7 (0.3–1.2) | 13–91 (2.3–15.9) | 27–65 (4.7–11.4) | 5–10 (0.9–1.7) | 7–15 (1.2–2.6) | 24–145 (4.2–25.3) | 3–12 (0.5–2.1) | 20–95 (3.5–16.6) | 4–6 (0.7–1) | 32–19 (5.6–3.3) | 71–175 (12.4–30.6) |
| Lissonycteris angolensis | 186 | 0–4 (0–2.2) | 5–31 (2.7–16.7) | 9–21 (4.8–11.3) | 0–4 (0–2.2) | 2–4 (1.1–2.2) | 3–27 (1.6–14.5) | 2–4 (1.1–2.2) | 11–32 (5.9–17.2) | 0–0 (0–0) | 2–0 (1.1–0) | 17–51 (9.1–27.4) |
| Micropteropus pusillus | 256 | 2–2 (0.8–0.8) | 2–13 (0.8–5.1) | 1–7 (0.4–2.7) | 0–0 (0–0) | 2–4 (0.8–1.6) | 1–16 (0.4–6.3) | 2–5 (0.8–2) | 1–7 (0.4–2.7) | 0–0 (0–0) | 0–0 (0–0) | 8–29 (3.1–11.3) |
| Myonycteris torquata | 397 | 0–1 (0–0.3) | 4–20 (1–5) | 2–12 (0.5–3) | 0–5 (0–1.3) | 3–7 (0.8–1.8) | 1–29 (0.3–7.3) | 3–7 (0.8–1.8) | 1–16 (0.3–4) | 1–1 (0.3–0.3) | 0–0 (0–0) | 12–52 (3–13.1) |
| Rousettus aegyptiacus | 1140 | 14–54 (1.2–4.7) | 36–189 (3.2–16.6) | 36–93 (3.2–8.2) | 32–90 (2.8–7.9) | 43–71 (3.8–6.2) | 32–261 (2.8–22.9) | 41–92 (3.6–8.1) | 31–162 (2.7–14.2) | 9–18 (0.8–1.6) | 20–10 (1.8–0.9) | 160–405 (14–35.5) |
| Other frugivorous species c | 79 | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–1.3) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–1.3) |
| Subtotal | 5972 | 44–142 (0.7–2.4) | 193–928 (3.2–15.5) | 178–514 (3–8.6) | 47–163 (0.8–2.7) | 83–158 (1.4–2.6) | 188–1270 (3.1–21.3) | 95–241 (1.6–4) | 131–805 (2.2–13.5) | 15–31 (0.3–0.5) | 64–35 (1.1–0.6) | 543–1644 (9.1–27.5) |
| Insectivorous bats | ||||||||||||
| Molossidae | ||||||||||||
| Chaerephon/Mops d | 1428 | 4–15 (0.3–1.1) | 9–70 (0.6–4.9) | 7–32 (0.5–2.2) | 3–9 (0.2–0.6) | 1–6 (0.1–0.4) | 1–54 (0.1–3.8) | 5–12 (0.4–0.8) | 7–51 (0.5–3.6) | 1–1 (0.1–0.1) | 10–2 (0.7–0.1) | 26–107 (1.8–7.5) |
| Hipposideridae | ||||||||||||
| Hipposideros sp. d | 1591 | 0–0 (0–0) | 1–7 (0.1–0.4) | 0–3 (0–0.2) | 1–2 (0.1–0.1) | 3–7 (0.2–0.4) | 0–8 (0–0.5) | 2–3 (0.1–0.2) | 0–7 (0–0.4) | 0–0 (0–0) | 1–0 (0.1–0) | 6–21 (0.4–1.3) |
| Miniopteridae | ||||||||||||
| Miniopterus sp. d | 264 | 1–1 (0.4–0.4) | 1–11 (0.4–4.2) | 1–5 (0.4–1.9) | 6–11 (2.3–4.2) | 1–4 (0.4–1.5) | 0–7 (0–2.7) | 3–7 (1.1–2.7) | 1–9 (0.4–3.4) | 0–1 (0–0.4) | 3–1 (1.1–0.4) | 12–32 (4.5–12.1) |
| Nycteridae | ||||||||||||
| Nycteris sp. d | 88 | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–1.1) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 1–1 (1.1–1.1) |
| Rhinolophidae | ||||||||||||
| Rhinolophus sp. d | 154 | 0–1 (0–0.6) | 0–0 (0–0) | 0–0 (0–0) | 1–1 (0.6–0.6) | 0–0 (0–0) | 0–0 (0–0) | 2–3 (1.3–1.9) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 2–4 (1.3–2.6) |
| Other insectivorous species e | 97 | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–1) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–1) |
| Subtotal | 3622 | 5–17 (0.1–0.5) | 11–88 (0.3–2.4) | 8–41 (0.2–1.1) | 11–24 (0.3–0.7) | 5–17 (0.1–0.5) | 1–69 (0–1.9) | 12–25 (0.3–0.7) | 8–67 (0.2–1.8) | 1–2 (0–0.1) | 14–3 (0.4–0.1) | 47–166 (1.3–4.6) |
| Total | 9594 | 49–159 (0.5–1.7) | 204–1016 (2.1–10.6) | 186–555 (1.9–5.8) | 58–187 (0.6–1.9) | 88–175 (0.9–1.8) | 189–1339 (2–14) | 107–266 (1.1–2.8) | 139–872 (1.4–9.1) | 16–33 (0.2–0.3) | 78–38 (0.8–0.4) | 590–1810 (6.1–18.9) |
| Genus/Species | N Tested | NP + GP EBOV | NP + VP EBOV | GP + VP EBOV | NP + GP + VP EBOV | Total EBOV * | NP + GP SUDV | NP + VP SUDV | GP + VP SUDV | NP + GP + VP SUDV | Total SUDV* | GP + VP BDBV | Total ** |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Frugivorous bats | |||||||||||||
| Pteropodidae | |||||||||||||
| Eidolon helvum | 1652 | 3–28 (0.2–1.7) | 1–2 (0.1–0.1) | 0–18 (0–1.1) | 0–6 (0–0.4) | 4–54 (0.2–3.3) | 1–22 (0.1–1.3) | 0–0 (0–0) | 9–72 (0.5–4.4) | 0–3 (0–0.2) | 10–97 (0.6–5.9) | 0–2 (0–0.1) | 13–128 (0.8–7.7) |
| Epomophorus sp. a | 614 | 0–1 (0–0.2) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–0.2) | 0–2 (0–0.3) | 0–0 (0–0) | 0–2 (0–0.3) | 0–0 (0–0.2) | 0–4 (0–0.7) | 0–0 (0–0.1) | 0–5 (0–0.8) |
| Epomops sp. b | 1076 | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–0.1) | 0–0 (0–0) | 0–1 (0–0.1) | 0–0 (0–0) | 2–2 (0.2–0.2) | 0–0 (0–0) | 0–0 (0–0.2) | 2–2 (0.2–0.2) | 0–0 (0–0.1) | 2–3 (0.2–0.3) |
| Hypsignathus monstrosus | 572 | 1–4 (0.2–0.7) | 0–0 (0–0) | 0–2 (0–0.3) | 0–0 (0–0) | 1–6 (0.2–1) | 0–8 (0–1.4) | 0–0 (0–0) | 0–6 (0–1) | 0–0 (0–0.2) | 0–14 (0–2.4) | 0–0 (0–0.1) | 1–20 (0.2–3.5) |
| Lissonycteris angolensis | 186 | 0–2 (0–1.1) | 0–0 (0–0) | 0–1 (0–0.5) | 0–0 (0–0) | 0–3 (0–1.6) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–0.5) | 0–0 (0–0) | 0–1 (0–0.5) | 0–0 (0–0.1) | 0–4 (0–2.2) |
| Micropteropus pusillus | 256 | 0–0 (0–0) | 0–0 (0–0) | 0– (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–0.4) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0.2) | 0–1 (0–0.4) | 0–0 (0–0.1) | 0–1 (0–0.4) |
| Myonycteris torquata | 397 | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–0.3) | 0–0 (0–0) | 0–1 (0–0.3) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0.2) | 0–0 (0–0) | 0–0 (0–0.1) | 0–1 (0–0.3) |
| Rousettus aegyptiacus | 1140 | 1–13 (0.1–1.1) | 2–5 (0.2–0.4) | 6–30 (0.5–2.6) | 0–14 (0–1.2) | 9–62 (0.8–5.4) | 2–16 (0.2–1.4) | 5–11 (0.4–1) | 6–28 (0.5–2.5) | 1–14 (0.1–1.2) | 14–69 (1.2–6.1) | 0–9 (0–0.8) | 20–103 (1.8–9) |
| Other frugivorous species c | 79 | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) |
| Subtotal | 5972 | 5–48 (0.1–0.8) | 3–7 (0.1–0.1) | 6–53 (0.1–0.9) | 0–20 (0–0.3) | 14–128 (0.2–2.1) | 3–49 (0.1–0.8) | 7–13 (0.1–0.2) | 15–109 (0.3–1.8) | 1–17 (0–0.3) | 26–188 (0.4–3.1) | 0–11 (0–0.2) | 36–265 (0.6–4.4) |
| Insectivorous bats | |||||||||||||
| Molossidae | |||||||||||||
| Chaerephon/Mops d | 1428 | 1–4 (0.1–0.3) | 2–1 (0.1–0.1) | 1–2 (0.1–0.1) | 0–1 (0–0.1) | 4–8 (0.3–0.6) | 0–2 (0–0.1) | 0–0 (0–0) | 0–3 (0–0.2) | 0–0 (0–0) | 0–5 (0–0.4) | 0–0 (0–0) | 4–12 (0.3–0.8) |
| Hipposideridae | |||||||||||||
| Hipposideros sp. d | 1591 | 0–0 (0–0) | 0–0 (0–0) | 1–1 (0.1–0.1) | 0–0 (0–0) | 1–1 (0.1–0.1) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–1 (0–0.1) | 0–1 (0–0.1) | 0–0 (0–0) | 1–1 (0.1–0.1) |
| Miniopteridae | |||||||||||||
| Miniopterus sp. d | 264 | 0–0 (0–0) | 1–1 (0.4–0.4) | 0–1 (0–0.4) | 0–0 (0–0) | 1–2 (0.4–0.8) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 1–3 (0.4–1.1) |
| Nycteridae | |||||||||||||
| Nycteris sp. d | 88 | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) |
| Rhinolophidae | |||||||||||||
| Rhinolophus sp. d | 154 | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) |
| Other insectivorous species e | 97 | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) | 0–0 (0–0) |
| Subtotal | 3622 | 1–4 (0–0.1) | 3–2 (0.1–0.1) | 2–4 (0.1–0.1) | 0–1 (0–0) | 6–11 (0.2–0.3) | 0–2 (0–0.1) | 0–0 (0–0) | 0–3 (0–0.1) | 0–1 (0–0) | 0–6 (0–0.2) | 0–0 (0–0) | 6–16 (0.2–0.4) |
| Total | 9594 | 6–52 (0.1–0.5) | 6–9 (0.1–0.1) | 8–57 (0.1–0.6) | 0–21 (0–0.2) | 20–139 (0.2–1.4) | 3–51 (0–0.5) | 7–13 (0.1–0.1) | 15–112 (0.2–1.2) | 1–18 (0–0.2) | 26–194 (0.3–2) | 0–11 (0–0.1) | 46–281 (0.5–2.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peeters, M.; Champagne, M.; Ndong Bass, I.; Goumou, S.; Ndimbo Kumugo, S.-P.; Lacroix, A.; Esteban, A.; Meta Djomsi, D.; Soumah, A.K.; Mbala Kingebeni, P.; et al. Extensive Survey and Analysis of Factors Associated with Presence of Antibodies to Orthoebolaviruses in Bats from West and Central Africa. Viruses 2023, 15, 1927. https://doi.org/10.3390/v15091927
Peeters M, Champagne M, Ndong Bass I, Goumou S, Ndimbo Kumugo S-P, Lacroix A, Esteban A, Meta Djomsi D, Soumah AK, Mbala Kingebeni P, et al. Extensive Survey and Analysis of Factors Associated with Presence of Antibodies to Orthoebolaviruses in Bats from West and Central Africa. Viruses. 2023; 15(9):1927. https://doi.org/10.3390/v15091927
Chicago/Turabian StylePeeters, Martine, Maëliss Champagne, Innocent Ndong Bass, Souana Goumou, Simon-Pierre Ndimbo Kumugo, Audrey Lacroix, Amandine Esteban, Dowbiss Meta Djomsi, Abdoul Karim Soumah, Placide Mbala Kingebeni, and et al. 2023. "Extensive Survey and Analysis of Factors Associated with Presence of Antibodies to Orthoebolaviruses in Bats from West and Central Africa" Viruses 15, no. 9: 1927. https://doi.org/10.3390/v15091927







