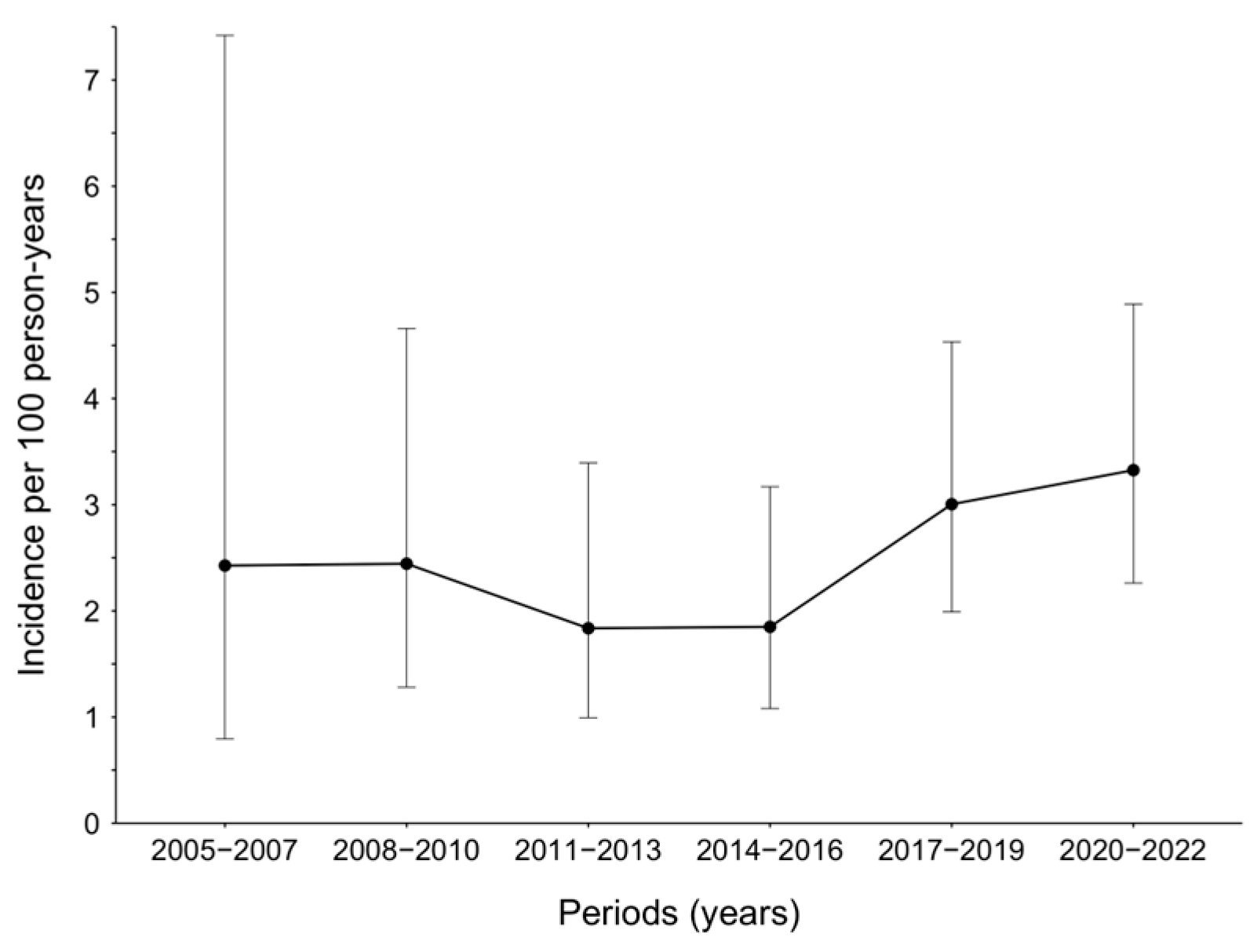
Temporal Trends in Syphilis Incidence among Men with HIV in Busan, Korea, 2005–2022: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Definition
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tao, Y.T.; Gao, T.Y.; Li, H.Y.; Ma, Y.T.; Li, H.J.; Xian-Yu, C.Y.; Deng, N.J.; Zhang, C. Global, regional, and national trends of syphilis from 1990 to 2019: The 2019 global burden of disease study. BMC Public Health 2023, 23, 754. [Google Scholar] [CrossRef]
- Hook, E.W., 3rd. Syphilis. Lancet 2017, 389, 1550–1557. [Google Scholar] [CrossRef]
- Chen, T.; Wan, B.; Wang, M.; Lin, S.; Wu, Y.; Huang, J. Evaluating the global, regional, and national impact of syphilis: Results from the global burden of disease study 2019. Sci. Rep. 2023, 13, 11386. [Google Scholar] [CrossRef]
- Borg, S.A.; Tenneti, N.; Lee, A.; Drewett, G.P.; Ivan, M.; Giles, M.L. The Reemergence of Syphilis Among Females of Reproductive Age and Congenital Syphilis in Victoria, Australia, 2010 to 2020: A Public Health Priority. Sex. Transm. Dis. 2023, 50, 479–484. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Sur-Veillance 2020; Department of Health and Human Services: Atlanta, GA, USA, 2021.
- Nelson, R. Congenital syphilis increases in the USA. Lancet Microbe 2022, 3, e171. [Google Scholar] [CrossRef]
- Takahashi, T.; Arima, Y.; Yamagishi, T.; Nishiki, S.; Kanai, M.; Ishikane, M.; Matsui, T.; Sunagawa, T.; Ohnishi, M.; Oishi, K. Rapid Increase in Reports of Syphilis Associated with Men Who Have Sex With Women and Women Who Have Sex With Men, Japan, 2012 to 2016. Sex. Transm. Dis. 2018, 45, 139–143. [Google Scholar] [CrossRef]
- Htet, K.Z.; Lindrose, A.R.; O’Connell, S.; Marsh, J.; Kissinger, P. The burden of chlamydia, gonorrhea, and syphilis in older adults in the United States: A systematic review. Int. J. STD AIDS 2023, 34, 288–298. [Google Scholar] [CrossRef]
- Wang, C.; Zhao, P.; Xiong, M.; Tucker, J.D.; Ong, J.J.; Hall, B.J.; Sami, M.; Zheng, H.; Yang, B. New Syphilis Cases in Older Adults, 2004–2019: An Analysis of Surveillance Data From South China. Front. Med. 2021, 8, 781759. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. National Overview of STDs; Division of STD Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2021.
- Ghaznavi, C.; Tanoue, Y.; Kawashima, T.; Eguchi, A.; Yoneoka, D.; Sakamoto, H.; Ueda, P.; Ishikane, M.; Ando, N.; Miyazato, Y.; et al. Recent changes in the reporting of STIs in Japan during the COVID-19 pandemic. Sex. Transm. Infect. 2023, 99, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Ukai, T.; Kakimoto, K.; Kawahata, T.; Miyama, T.; Iritani, N.; Motomura, K. Resurgence of syphilis in 2022 amongst heterosexual men and women in Osaka, Japan. Clin. Microbiol. Infect. 2023, 29, 396–397. [Google Scholar] [CrossRef] [PubMed]
- Naito, T.; Mori, H.; Fujibayashi, K.; Fukushima, S.; Yuda, M.; Fukui, N.; Suzuki, M.; Goto-Hirano, K.; Kuwatsuru, R. Syphilis in people living with HIV does not account for the syphilis resurgence in Japan. J. Infect. Chemother. 2022, 28, 1494–1500. [Google Scholar] [CrossRef] [PubMed]
- Erbelding, E.; Rompalo, A. Changing Epidemiology of Syphilis and Its Persistent Relationship with HIV. Curr. Infect. Dis. Rep. 2004, 6, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Lynn, W.A.; Lightman, S. Syphilis and HIV: A dangerous combination. Lancet Infect. Dis. 2004, 4, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Bissessor, M.; Fairley, C.K.; Leslie, D.; Howley, K.; Chen, M.Y. Frequent screening for syphilis as part of HIV monitoring increases the detection of early asymptomatic syphilis among HIV-positive homosexual men. J. Acquir. Immune Defic. Syndr. 2010, 55, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Branger, J.; van der Meer, J.T.; van Ketel, R.J.; Jurriaans, S.; Prins, J.M. High incidence of asymptomatic syphilis in HIV-infected MSM justifies routine screening. Sex. Transm Dis. 2009, 36, 84–85. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.P.F.; Callander, D.; Fairley, C.K.; Zhang, L.; Donovan, B.; Guy, R.; Lewis, D.A.; Hellard, M.; Read, P.; Ward, A.; et al. Increased Syphilis Testing of Men Who Have Sex With Men: Greater Detection of Asymptomatic Early Syphilis and Relative Reduction in Secondary Syphilis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2017, 65, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Cohen, C.E.; Winston, A.; Asboe, D.; Boag, F.; Mandalia, S.; Azadian, B.; Hawkins, D.A. Increasing detection of asymptomatic syphilis in HIV patients. Sex. Transm. Infect. 2005, 81, 217–219. [Google Scholar] [CrossRef] [PubMed]
- Jung, O.E.; Mi, J.Y.; Jeongok, C.; Insik, K. Sexually Transmitted Infections (STIs) Surveillance in the Republic of Korea, 2014–2018. Public Health Wkly. Rep. 2019, 13, 924–933. [Google Scholar]
- Ahn, J.Y.; Boettiger, D.; Kiertiburanakul, S.; Merati, T.P.; Huy, B.V.; Wong, W.W.; Ditangco, R.; Lee, M.P.; Oka, S.; Durier, N.; et al. Incidence of syphilis seroconversion among HIV-infected persons in Asia: Results from the TREAT Asia HIV Observational Database. J. Int. AIDS Soc. 2016, 19, 20965. [Google Scholar] [CrossRef]
- Lee, E.; Kim, J.; Bang, J.H.; Lee, J.Y.; Cho, S.I. Association of HIV-syphilis coinfection with optimal antiretroviral adherence: A nation-wide claims study. AIDS Care 2020, 32, 651–655. [Google Scholar] [CrossRef]
- Park, W.B.; Jang, H.C.; Kim, S.H.; Kim, H.B.; Kim, N.J.; Oh, M.D.; Choe, K.W. Effect of highly active antiretroviral therapy on incidence of early syphilis in HIV-infected patients. Sex. Transm. Dis. 2008, 35, 304–306. [Google Scholar] [CrossRef]
- Kenyon, C.; Lynen, L.; Florence, E.; Caluwaerts, S.; Vandenbruaene, M.; Apers, L.; Soentjens, P.; Van Esbroeck, M.; Bottieau, E. Syphilis reinfections pose problems for syphilis diagnosis in Antwerp, Belgium—1992 to 2012. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. = Eur. Commun. Dis. Bull. 2014, 19, 20958. [Google Scholar] [CrossRef]
- Nishijima, T.; Teruya, K.; Shibata, S.; Yanagawa, Y.; Kobayashi, T.; Mizushima, D.; Aoki, T.; Kinai, E.; Yazaki, H.; Tsukada, K.; et al. Incidence and Risk Factors for Incident Syphilis among HIV-1-Infected Men Who Have Sex with Men in a Large Urban HIV Clinic in Tokyo, 2008–2015. PLoS ONE 2016, 11, e0168642. [Google Scholar] [CrossRef] [PubMed]
- Novak, R.M.; Ghanem, A.; Hart, R.; Ward, D.; Armon, C.; Buchacz, K.; HIV Outpatient Study Investigators. Risk Factors and Incidence of Syphilis in Human Immunodeficiency Virus (HIV)-Infected Persons: The HIV Outpatient Study, 1999–2015. Clin. Infect. Dis. 2018, 67, 1750–1759. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Case definitions for infectious conditions under public health surveillance. MMWR Recomm. Rep. 1997, 46, 1–55. [Google Scholar]
- Lee, S.O.; Lee, J.E.; Lee, S.; Lee, S.H.; Kang, J.S. Prevalence and patterns of illicit drug use in people with human immunodeficiency virus infection in Korea. PLoS ONE 2021, 16, e0249361. [Google Scholar] [CrossRef]
- Thurnheer, M.C.; Weber, R.; Toutous-Trellu, L.; Cavassini, M.; Elzi, L.; Schmid, P.; Bernasconi, E.; Christen, A.B.; Zwahlen, M.; Furrer, H. Occurrence, risk factors, diagnosis and treatment of syphilis in the prospective observational Swiss HIV Cohort Study. Aids 2010, 24, 1907–1916. [Google Scholar] [CrossRef] [PubMed]
- Korea Disease Control and Prevention Agency. HIV/AIDS Notifications in the Republic of Korea 2021; Public Health Weekly Report; Korea Disease Control and Prevention Agency: Cheongju, Republic of Korea, 2022.
- Lee, J.A.; Kim, Y.; Choi, J.Y. Impact of the COVID-19 Pandemic on HIV Services in Korea: Results from a Cross-Sectional Online Survey. Infect. Chemother. 2021, 53, 741–752. [Google Scholar] [CrossRef]
- Choi, J.K.; Lee, S.J.; Yoo, J.H. History of Syphilis and Gonorrhea in Korea. Infect Chemother. 2019, 51, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Yumi Seo, G.L. Syphilis Notification Systems in Korea over the Last 20 Years. Urogenit. Tract. Infect. 2021, 16, 16–23. [Google Scholar]
- Ang, L.; Wong, C.S.; Ng, O.T.; Leo, Y.S. Incidence of syphilis among HIV-infected men in Singapore, 2006–2017: Temporal trends and associated risk factors. Sex. Transm. Infect. 2020, 96, 293–299. [Google Scholar] [CrossRef]
- Burchell, A.N.; Allen, V.G.; Gardner, S.L.; Moravan, V.; Tan, D.H.; Grewal, R.; Raboud, J.; Bayoumi, A.M.; Kaul, R.; Mazzulli, T.; et al. High incidence of diagnosis with syphilis co-infection among men who have sex with men in an HIV cohort in Ontario, Canada. BMC Infect. Dis. 2015, 15, 356. [Google Scholar] [CrossRef] [PubMed]
- Park, I.U.; Fakile, Y.F.; Chow, J.M.; Gustafson, K.J.; Jost, H.; Schapiro, J.M.; Novak-Weekley, S.; Tran, A.; Nomura, J.H.; Chen, V.; et al. Performance of Treponemal Tests for the Diagnosis of Syphilis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2019, 68, 913–918. [Google Scholar] [CrossRef] [PubMed]
- Romanowski, B.; Sutherland, R.; Fick, G.H.; Mooney, D.; Love, E.J. Serologic response to treatment of infectious syphilis. Ann. Intern. Med. 1991, 114, 1005–1009. [Google Scholar] [CrossRef] [PubMed]
- Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Available online: https://https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/whats-new (accessed on 12 December 2023).
- Workowski, K.A.; Bachmann, L.H.; Chan, P.A.; Johnston, C.M.; Muzny, C.A.; Park, I.; Reno, H.; Zenilman, J.M.; Bolan, G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm. Rep. 2021, 70, 1–187. [Google Scholar] [CrossRef]
- Cantor, A.G.; Pappas, M.; Daeges, M.; Nelson, H.D. Screening for Syphilis: Updated Evidence Report and wSystematic Review for the US Preventive Services Task Force. JAMA 2016, 315, 2328–2337. [Google Scholar] [CrossRef]


| Characteristics | All Patients (n = 499) | Patients with Incident Syphilis (n = 82) | Patients without Incident Syphilis (n = 417) | p-Value |
|---|---|---|---|---|
| Median age at baseline, years [IQR] | 41 [31–51] | 34 [24–43.3] | 42 [32–52] | <0.001 |
| Ethnicity | 0.491 | |||
| Korean | 486 (97.4) | 81 (98.8) | 405 (97.1) | |
| Non-Korean | 13 (2.6) | 1 (1.2) | 12 (2.9) | |
| Marriage | 0.002 | |||
| Unmarried | 308 (61.7) | 64 (78.0) | 244 (58.5) | |
| Married previously | 185 (37.1) | 18 (22.0) | 167 (40.1) | |
| Unknown | 6 (1.2) | 0 (0) | 6 (1.4) | |
| Sexual behavior | <0.001 | |||
| Non-MSM | 191 (38.3) | 16 (19.5) | 175 (42.0) | |
| MSM | 290 (58.1) | 65 (79.3) | 225 (54.0) | |
| Unknown | 18 (3.6) | 1 (1.2) | 17 (4.1) | |
| Median CD4 cell counts, /µL [IQR] | 262 [100–417] | 302 [150.5–380] | 261 [92–422] | 0.495 |
| Anti-retroviral therapy | 0.393 | |||
| Naïve | 426 (85.4) | 73 (89.0) | 353 (84.7) | |
| Experienced | 73 (14.6) | 9 (11.0) | 64 (15.3) | |
| Treponemal test positive at baseline | 172 (34.5) | 41 (50.0) | 131 (31.5) | 0.002 |
| Incaceration, ever | 30 (6.0) | 8 (9.8) | 22 (5.3) | 0.128 |
| Illicit drug use, ever | 32 (6.4) | 8 (9.8) | 24 (5.8) | 0.213 |
| Injection drug use, ever | 14 (2.8) | 3 (3.7) | 11 (2.6) | 0.712 |
| HBV surface antigen, positive | 29 (5.8) | 3 (3.7) | 26 (6.2) | 0.449 |
| HCV antibody, positive | 16 (3.2) | 1 (1.2) | 15 (3.6) | 0.333 |
| Calendar period of baseline visit | 0.289 | |||
| 2005–2007 | 98 (19.6) | 15 (18.3) | 83 (19.9) | |
| 2008–2010 | 96 (19.2) | 15 (18.3) | 81 (19.4) | |
| 2011–2013 | 100 (20.0) | 21(25.6) | 79 (18.9) | |
| 2014–2015 | 78 (15.6) | 16 (19.5) | 62 (14.9) | |
| 2016–2019 | 80 (16.0) | 12 (14.6) | 68 (16.3) | |
| 2020–2022 | 47 (9.4) | 3 (3.7) | 44 (10.6) | |
| Median testing rates per year [IQR] | 2.2 [1.6–2.8] | 2.9 [1.7–4.28] | 2.2 [1.6–2.7] | 0.043 |
| Median follow-up periods, years [IQR] | 5.08 [1.97–9.93] | 3.03 [1.01–6.9] | 5.76 [2.35–11.13] | <0.001 |
| Variables | Incidences per 100 PY | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| Crude HR (95% CI) | p-Value | Adjusted HR (95% CI) | p-Value | ||
| Age at enrollment, years | |||||
| >50 | 0.98 | Reference | |||
| 30–50 | 2.21 | 2.3 (1.08–4.92) | 0.032 | 2.35 (0.99–5.58) | 0.052 |
| ≤30 | 5.69 | 5.41 (2.5–11.71) | <0.001 | 6.27 (2.38–16.56) | <0.001 |
| Ethnicity (non-Korean vs. Korean) | 6.14 vs. 2.53 | 1.62 (0.22–11.92) | 0.633 | ||
| Marriage (unmarried vs. previously married) | 3.57 vs. 1.28 | 2.63 (1.56–4.44) | <0.001 | 1.07 (0.57–2.03) | 0.825 |
| Sexual behavior (MSM vs. non-MSM) | 3.4 vs. 1.27 | 2.63 (1.52–4.55) | <0.001 | 2.36 (1.34–4.16) | 0.003 |
| CD4 cell counts at baseline, /µL | |||||
| ≤200 | 1.97 | Reference | |||
| 201–500 | 3.06 | 1.52 (0.94–2.47) | 0.091 | 1.24 (0.76–2.03) | 0.398 |
| >500 | 2.84 | 1.39 (0.74–2.61) | 0.301 | 0.99 (0.51–1.91) | 0.964 |
| ART (experienced vs. naïve) | 2.54 vs. 2.55 | 0.94 (0.47–1.89) | 0.860 | ||
| Treponemal test at baseline (positive vs. negative) | 3.85 vs. 1.9 | 1.96 (1.27–3.02) | 0.002 | 2.33 (1.48–3.67) | <0.001 |
| Incarceration (ever vs. never) | 4.97 vs. 2.42 | 2.02 (0.97–4.19) | 0.059 | 2.62 (1.21–5.67) | 0.015 |
| Illicit drug use (ever vs. never) | 3.11 vs. 2.50 | 1.26 (0.61–2.62) | 0.530 | ||
| Injection drug use (ever vs. never) | 3.33 vs. 2.52 | 1.27 (0.40–4.02) | 0.684 | ||
| HBV surface antigen (positive vs. negative) | 1.51 vs. 2.61 | 0.58 (0.18–1.83) | 0.351 | ||
| HCV antibody (positive vs. negative) | 1.26 vs. 2.58 | 0.46 (0.06–3.29) | 0.437 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.H.; Lee, J.E.; Lee, S.O.; Lee, S.; Ko, W.S.; Kim, H.-H.; Shin, K.-H.; Kang, J.S.; Son, H. Temporal Trends in Syphilis Incidence among Men with HIV in Busan, Korea, 2005–2022: A Retrospective Cohort Study. Viruses 2024, 16, 265. https://doi.org/10.3390/v16020265
Lee SH, Lee JE, Lee SO, Lee S, Ko WS, Kim H-H, Shin K-H, Kang JS, Son H. Temporal Trends in Syphilis Incidence among Men with HIV in Busan, Korea, 2005–2022: A Retrospective Cohort Study. Viruses. 2024; 16(2):265. https://doi.org/10.3390/v16020265
Chicago/Turabian StyleLee, Sun Hee, Jeong Eun Lee, Soon Ok Lee, Shinwon Lee, Woo Seog Ko, Hyung-Hoi Kim, Kyung-Hwa Shin, Jin Suk Kang, and Hyunjin Son. 2024. "Temporal Trends in Syphilis Incidence among Men with HIV in Busan, Korea, 2005–2022: A Retrospective Cohort Study" Viruses 16, no. 2: 265. https://doi.org/10.3390/v16020265
APA StyleLee, S. H., Lee, J. E., Lee, S. O., Lee, S., Ko, W. S., Kim, H.-H., Shin, K.-H., Kang, J. S., & Son, H. (2024). Temporal Trends in Syphilis Incidence among Men with HIV in Busan, Korea, 2005–2022: A Retrospective Cohort Study. Viruses, 16(2), 265. https://doi.org/10.3390/v16020265






