Application of MPBT Assay for Multiplex Determination of Infectious Titers and for Selection of the Optimal Formulation for the Trivalent Novel Oral Poliovirus Vaccine
Abstract
1. Introduction
2. Materials and Methods
2.1. nOPV Samples and HEp-2C Cells
2.2. Virus Titration by CCID50 Assay
2.3. Multiplex PCR-Based Titration (MPBT) Assay
2.4. Formulation Preparation
2.5. Freeze/Thaw Samples Preparation
3. Results
3.1. Evaluation and Optimization of MPBT Assay for Titration of Trivalent nOPV (tnOPV)
3.2. Evaluation of the MPBT Assay’s Ability to Differentiate 0.5 Log10 Difference between Titers Using Half Plate
3.3. MPBT Assay Evaluation for Titer Determination of Untreated and Treated 35% Sucrose Formulated tnOPV Drug Product
3.4. MPBT Assay Analysis of Untreated, Treated and Freeze–Thawed tnOPV Drug Products Formulated with Different Excipients
4. Discussion
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Liu, B. Universal PCR Primers Are Critical for Direct Sequencing-Based Enterovirus Genotyping. J. Clin. Microbiol. 2017, 55, 339–340. [Google Scholar] [CrossRef] [PubMed]
- Tapparel, C.; Siegrist, F.; Petty, T.J.; Kaiser, L. Picornavirus and enterovirus diversity with associated human diseases. Infect. Genet. Evol. 2013, 14, 282–293. [Google Scholar] [CrossRef]
- WHO. Global Eradication of Wild Poliovirus Type 2 Declared; Declaration Further Milestone for Globally-Coordinated Vaccineswitch in 2016 [cited 2015 Sep 20]; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- WHO. Two Out of Three Wild Poliovirus Strains Eradicated; Globaleradication of Wild Poliovirus Type 3 Declared on World Polio Day 2019; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Laassri, M.; Lottenbach, K.; Belshe, R.; Rennels, M.; Plotkin, S.; Chumakov, K. Analysis of reversions in the 5′-untranslated region of attenuated poliovirus after sequential administration of inactivated and oral poliovirus vaccines. J. Infect. Dis. 2006, 193, 1344–1349. [Google Scholar] [CrossRef] [PubMed]
- Yakovenko, M.L.; Korotkova, E.A.; Ivanova, O.E.; Eremeeva, T.P.; Samoilovich, E.; Uhova, I.; Gavrilin, G.V.; Agol, V.I. Evolution of the Sabin vaccine into pathogenic derivatives without appreciable changes in antigenic properties: need for improvement of current poliovirus surveillance. J. Virol. 2009, 83, 3402–3406. [Google Scholar] [CrossRef] [PubMed]
- WHO. Detection of Circulating Vaccine Derived Polio Virus 2 (cVDPV2) in Environmental Samples—The United Kingdom of Great Britain and Northern Ireland and the United States of America; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Konopka-Anstadt, J.L.; Campagnoli, R.; Vincent, A.; Shaw, J.; Wei, L.; Wynn, N.T.; Smithee, S.E.; Bujaki, E.; Te Yeh, M.; Laassri, M.; et al. Development of a new oral poliovirus vaccine for the eradication end game using codon deoptimization. NPJ Vaccines 2020, 5, 26. [Google Scholar] [CrossRef] [PubMed]
- Yeh, M.T.; Bujaki, E.; Dolan, P.T.; Smith, M.; Wahid, R.; Konz, J.; Weiner, A.J.; Bandyopadhyay, A.S.; Van Damme, P.; De Coster, I.; et al. Engineering the Live-Attenuated Polio Vaccine to Prevent Reversion to Virulence. Cell Host Microbe 2020, 27, 736–751.e8. [Google Scholar] [CrossRef] [PubMed]
- Macadam, A.J.; Ferguson, G.; Stone, D.M.; Meredith, J.; Knowlson, S.; Auda, G.; Almond, J.W.; Minor, P.D. Rational design of genetically stable, live-attenuated poliovirus vaccines of all three serotypes: Relevance to poliomyelitis eradication. J. Virol. 2006, 80, 8653–8663. [Google Scholar] [CrossRef] [PubMed]
- Burns, C.C.; Campagnoli, R.; Shaw, J.; Vincent, A.; Jorba, J.; Kew, O. Genetic inactivation of poliovirus infectivity by increasing the frequencies of CpG and UpA dinucleotides within and across synonymous capsid region codons. J. Virol. 2009, 83, 9957–9969. [Google Scholar] [CrossRef] [PubMed]
- Bandyopadhyay, A.S.; Cooper, L.V.; Zipursky, S. One billion doses and WHO prequalification of nOPV2: Implications for the global polio situation and beyond. PLOS Glob. Public Health 2024, 4, e0002920. [Google Scholar] [CrossRef]
- WHO. Meeting of Strategic Advisory Group of Experts on Immunization, October 2021: Conclusions and recommendations. Wkly. Epidemiol. Rec. 2021, 50, 613–632. [Google Scholar]
- Yeh, M.T.; Smith, M.; Carlyle, S.; Konopka-Anstadt, J.L.; Burns, C.C.; Konz, J.; Andino, R.; Macadam, A. Genetic stabilization of attenuated oral vaccines against poliovirus types 1 and 3. Nature 2023, 619, 135–142. [Google Scholar] [CrossRef]
- Albrecht, P.; Enterline, J.C.; Boone, E.J.; Klutch, M.J. Poliovirus and polio antibody assay in HEp-2 and Vero cell cultures. J. Biol. Stand. 1983, 11, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Bey, E.; Golombick, T. A comparison of three methods for titration of poliovirus vaccines. J. Virol. Methods 1984, 9, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Magrath, D.I.; Seagroatt, V. The standardization of infectivity titrations of poliovaccines—A WHO collaborative study. J. Biol. Stand. 1985, 13, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Manukyan, H.; Rodionova, E.; Zagorodnyaya, T.; Lin, T.L.; Chumakov, K.; Laassri, M. Multiplex PCR-based titration (MPBT) assay for determination of infectious titers of the three Sabin strains of live poliovirus vaccine. Virol. J. 2019, 16, 122. [Google Scholar] [CrossRef]
- Manukyan, H.; Zagorodnyaya, T.; Ruttimann, R.; Manor, Y.; Bandyopadhyay, A.; Shulman, L.; Chumakov, K.; Laassri, M. Quantitative multiplex one-step RT-PCR assay for identification and quantitation of Sabin strains of poliovirus in clinical and environmental specimens. J. Virol. Methods 2018, 259, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Kärber, G. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Arch. Exp. Pathol. Pharmakol. 1931, 162, 480–483. [Google Scholar] [CrossRef]
- Chocarro, L.B.; Manau, M.V. Test of the potency of trivalent oral polio vaccines: Comparison of 2 methods of reading. Rev. Argent. Microbiol. 1987, 19, 65–69. [Google Scholar] [PubMed]
- WHO. Recommendations to Assure the Quality, Safety and Efficacy of Poliomyelitis Vaccines (Oral, Live, Attenuated), Annex 2, TRS No 1045; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Manukyan, H.; Tritama, E.; Wahid, R.; Anstadt, J.; Konz, J.; Chumakov, K.; Laassri, M. Improvement of the qmosRT-PCR Assay and Its Application for the Detection and Quantitation of the Three Serotypes of the Novel Oral Polio Vaccine in Stool Samples. Vaccines 2023, 11, 1729. [Google Scholar] [CrossRef]
- WHO. Polio Laboratory Manual, 4th ed.; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Ecarma, M.J.Y.; Nolden, A.A. A review of the flavor profile of metal salts: Understanding the complexity of metallic sensation. Chem. Senses 2021, 46, bjab043. [Google Scholar] [CrossRef]
- Wang, Y.; Zajac, A.L.; Lei, W.; Christensen, C.M.; Margolskee, R.F.; Bouysset, C.; Golebiowski, J.; Zhao, H.; Fiorucci, S.; Jiang, P. Metal Ions Activate the Human Taste Receptor TAS2R7. Chem. Senses 2019, 44, 339–347. [Google Scholar] [CrossRef]
- Cooper, L.A.; Scott, T.W. Differential evolution of eastern equine encephalitis virus populations in response to host cell type. Genetics 2001, 157, 1403–1412. [Google Scholar] [CrossRef] [PubMed]
- LaBarre, D.D.; Lowy, R.J. Improvements in methods for calculating virus titer estimates from TCID50 and plaque assays. J. Virol. Methods 2001, 96, 107–126. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.Y.; Kam, Y.W.; Fric, J.; Malleret, B.; Koh, E.G.; Prakash, C.; Huang, W.; Lee, W.W.; Lin, C.; Lin, R.T.; et al. Chikungunya virus neutralization antigens and direct cell-to-cell transmission are revealed by human antibody-escape mutants. PLoS Pathog. 2011, 7, e1002390. [Google Scholar] [CrossRef]
- Lopez-Bueno, A.; Mateu, M.G.; Almendral, J.M. High mutant frequency in populations of a DNA virus allows evasion from antibody therapy in an immunodeficient host. J. Virol. 2003, 77, 2701–2708. [Google Scholar] [CrossRef]
- Takenaka, A.; Gibbs, C.J., Jr.; Gajdusek, D.C. Antiviral neutralizing antibody to Hantaan virus as determined by plaque reduction technique. Arch. Virol. 1985, 84, 197–206. [Google Scholar] [CrossRef]
- Liu, B.M.; Mulkey, S.B.; Campos, J.M.; DeBiasi, R.L. Laboratory diagnosis of CNS infections in children due to emerging and re-emerging neurotropic viruses. Pediatr. Res. 2024, 95, 543–550. [Google Scholar] [CrossRef]
- Roldao, A.; Oliveira, R.; Carrondo, M.J.; Alves, P.M. Error assessment in recombinant baculovirus titration: Evaluation of different methods. J. Virol. Methods 2009, 159, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Burns, C.C.; Jorba, J.; Shulman, L.M.; Macadam, A.; Klapsa, D.; Majumdar, M.; Bullows, J.; Frolov, A.; Mate, R.; et al. Genetic Characterization of Novel Oral Polio Vaccine Type 2 Viruses During Initial Use Phase Under Emergency Use Listing-Worldwide, March-October 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 786–790. [Google Scholar] [CrossRef]
- Bivalent Poliomyelitis Vaccine Type 1 & Type 3, Live (Oral) [Packaging Insert]; Bulk Source: PT; Biofarma: Bandung, Indonesia, 2019.
- WHO. Polio Vaccines: WHO Position Paper; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Liu, B.; Forman, M.; Valsamakis, A. Optimization and evaluation of a novel real-time RT-PCR test for detection of parechovirus in cerebrospinal fluid. J. Virol. Methods 2019, 272, 113690. [Google Scholar] [CrossRef]
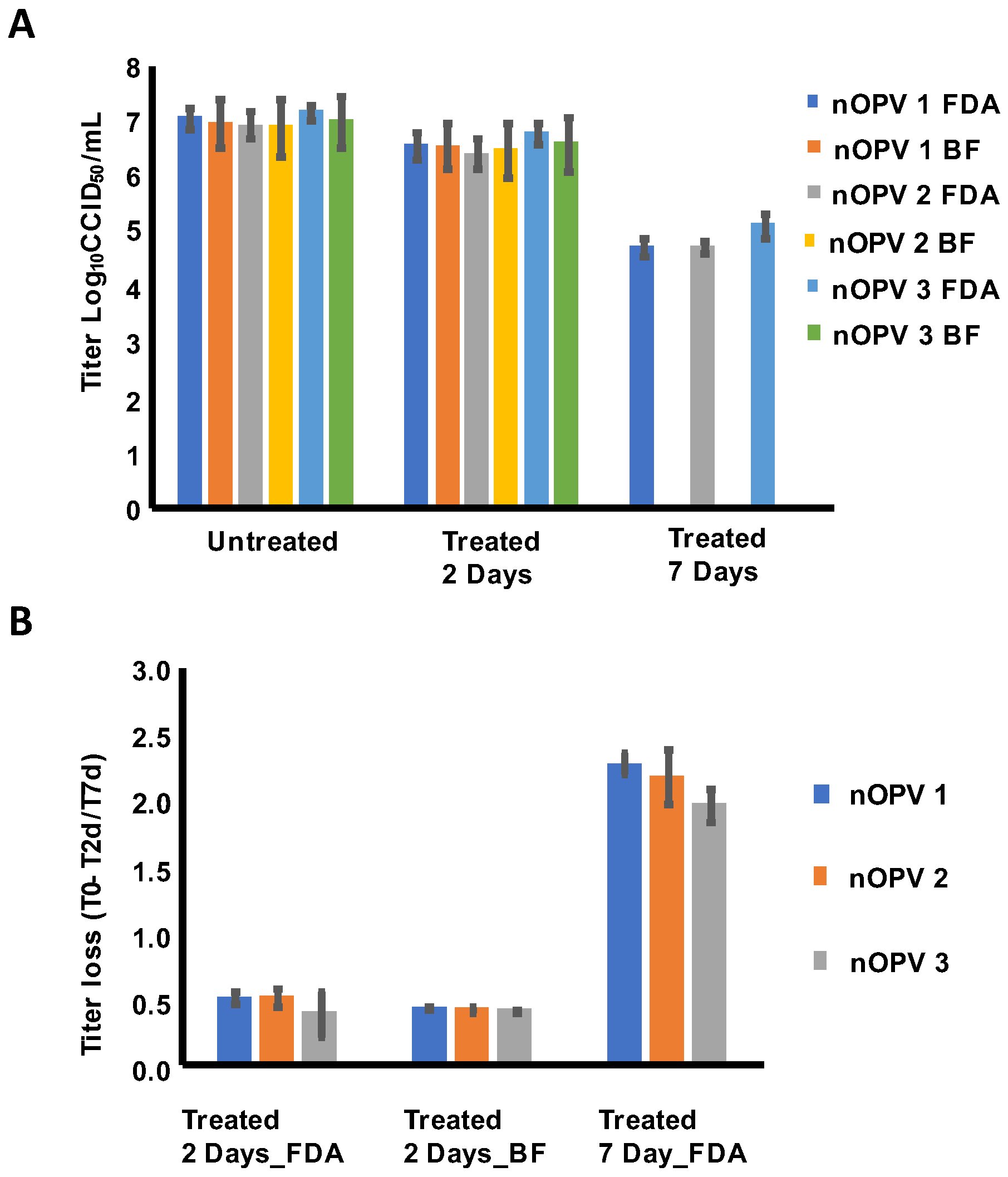
 —nOPV1,
—nOPV1,  —nOPV2,
—nOPV2,  —nOPV3.
—nOPV3.
 —nOPV1,
—nOPV1,  —nOPV2,
—nOPV2,  —nOPV3.
—nOPV3.
 —nOPV1,
—nOPV1,  —nOPV2,
—nOPV2,  —nOPV3. * For (A,B), p-value < 0.05 for regular significance test indicates that significant titer loss from T0 to T2d (A) or T7d (B) is detected. For comparison between T0 and FT3 (C) within each institution, where the goal is to confirm the comparability between institutions, p-value < 0.05 for equivalence test or 90% CI for difference within ±0.5 log10 equivalence margin is required to demonstrate equivalence.
—nOPV3. * For (A,B), p-value < 0.05 for regular significance test indicates that significant titer loss from T0 to T2d (A) or T7d (B) is detected. For comparison between T0 and FT3 (C) within each institution, where the goal is to confirm the comparability between institutions, p-value < 0.05 for equivalence test or 90% CI for difference within ±0.5 log10 equivalence margin is required to demonstrate equivalence.
 —nOPV1,
—nOPV1,  —nOPV2,
—nOPV2,  —nOPV3. * For (A,B), p-value < 0.05 for regular significance test indicates that significant titer loss from T0 to T2d (A) or T7d (B) is detected. For comparison between T0 and FT3 (C) within each institution, where the goal is to confirm the comparability between institutions, p-value < 0.05 for equivalence test or 90% CI for difference within ±0.5 log10 equivalence margin is required to demonstrate equivalence.
—nOPV3. * For (A,B), p-value < 0.05 for regular significance test indicates that significant titer loss from T0 to T2d (A) or T7d (B) is detected. For comparison between T0 and FT3 (C) within each institution, where the goal is to confirm the comparability between institutions, p-value < 0.05 for equivalence test or 90% CI for difference within ±0.5 log10 equivalence margin is required to demonstrate equivalence.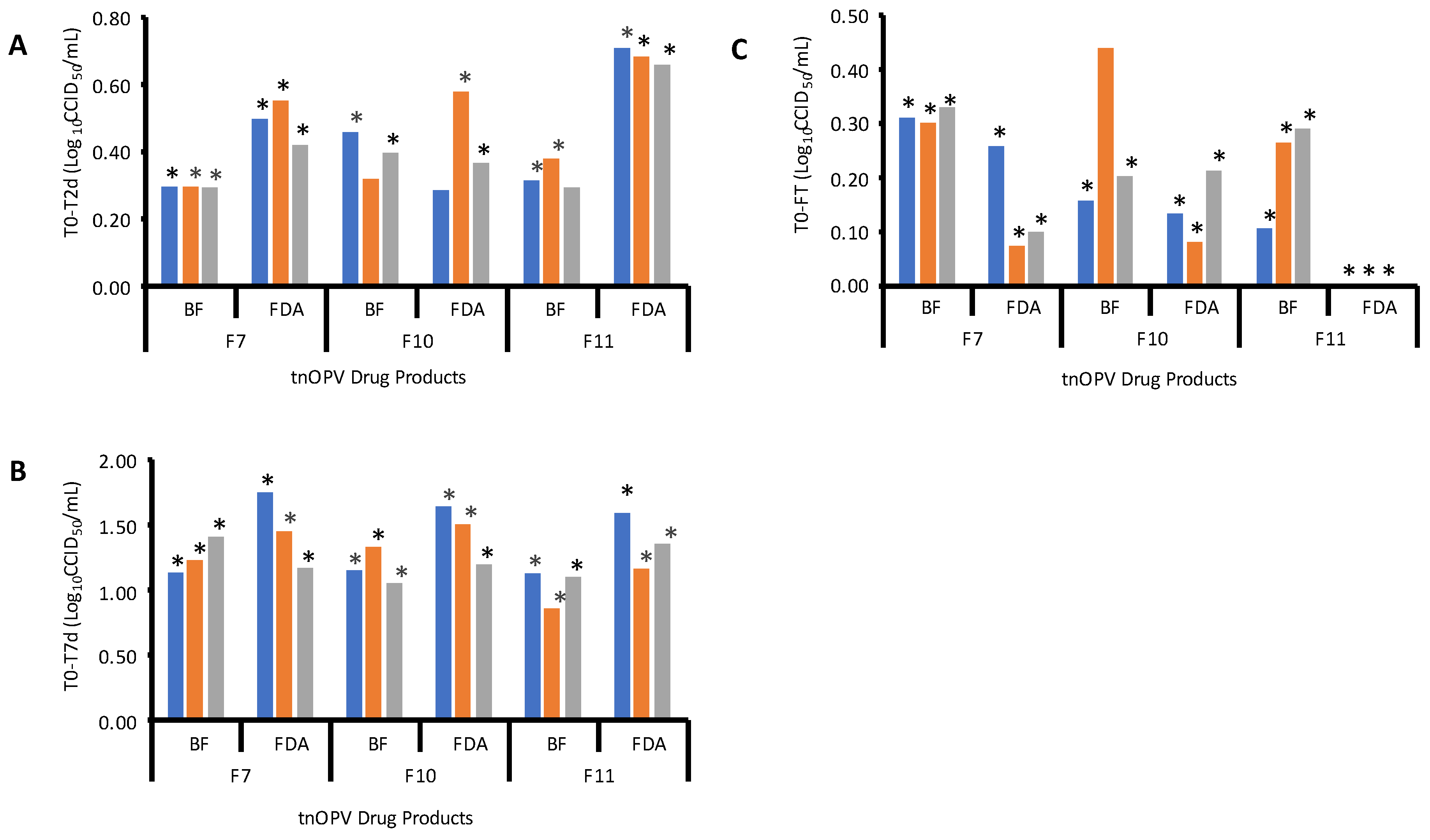
| Formulation | Composition (W/V) % | tnOPV Dug Product Titer |
|---|---|---|
| F1 | 35% Sucrose * | Type 1 Titer: log10 7.3 CCID50/mL Type 2 Titer: log10 6.6 CCID50/mL Type 3 Titer: log10 7.3 CCID50/mL |
| F2 | 28% Sucrose | |
| F3 | 1M MgCl2 6H2O | |
| F4 | 1M MgCl2 6H2O + 0.05% PS80 | |
| F6 | 28% Sucrose + 1M MgCl2.6H2O | |
| F7 | 28% Sucrose + 0.5% Histidine | |
| F8 | 28% Sucrose + 0.5% PEG8000 | |
| F9 | 28% Sucrose + 0.5% Arginine | |
| F10 | 14% Sucrose + 1M MgCl2.6H2O | |
| F11 | 14% Sucrose + 0.5% Histidine | |
| F12 | 14% Sucrose + 0.5% PEG8000 | |
| F13 | 14% Sucrose + 0.5% Arginine |
| nOPV Type (Lot) | CCID50 Assay | SPBT Assay | MPBT Assay | CCID50 Assay | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Run 1 | Run 2 | Mean ± SD | Run 1 | Run2 | Mean ± SD | Run 1 | Run 2 | Mean ± SD | ±0.5 log10 Range | ||
| 11 twofold serial dilutions, 8 repeats, whole plate, and starting dilution is 10−5 | LL | UL | |||||||||
| 1 (1) | 8.03 | 8.07 | 8.05 ± 0.03 | 8.30 | 8.03 | 8.16 ± 0.19 | 7.96 | 8.30 | 8.13 ± 0.24 | 7.55 | 8.55 |
| 2 (1) | 7.92 | 7.99 | 7.96 ± 0.05 | 8.22 | 8.07 | 8.14 ± 0.11 | 8.41 | 8.22 | 8.31 ± 0.13 | 7.46 | 8.46 |
| 3 (1) | 7.58 | 7.66 | 7.62 ± 0.05 | 7.66 | 7.77 | 7.71 ± 0.08 | 7.77 | 7.54 | 7.66 ± 0.16 | 7.12 | 8.12 |
| 7 threefold serial dilutions, 6 repeats, half plate, starting dilution is 10−6 | |||||||||||
| 1 (1) | 7.72 | 7.80 | 7.76 ± 0.06 | 7.87 | 8.19 | 8.03 ± 0.22 | 8.19 | 7.72 | 7.95 ± 0.34 | 7.26 | 8.26 |
| 2 (1) | 7.95 | 7.87 | 7.91 ± 0.06 | 7.80 | 8.27 | 8.03 ± 0.34 | 8.11 | 7.87 | 7.99 ± 0.17 | 7.41 | 8.41 |
| 3 (1) | 7.72 | 8.11 | 7.91 ± 0.28 | 7.95 | 7.72 | 7.83 ± 0.17 | 7.72 | 7.72 | 7.72 ± 0 | 7.41 | 8.41 |
| 7 threefold serial dilutions, 6 repeats, half plate, and starting dilution is 10−5 | |||||||||||
| 1 (2) | 7.67 | 7.59 | 7.63 ± 0.06 | 7.67 | 7.75 | 7.71 ± 0.06 | 7.51 | 7.67 | 7.59 ± 0.11 | 7.13 | 8.13 |
| 2 (2) | 6.95 | 7.35 | 7.15 ± 0.28 | 7.11 | 6.95 | 7.03 ± 0.11 | 7.43 | 7.67 | 7.55 ± 0.17 | 6.65 | 7.65 |
| 3 (2) | 8.47 | 8.15 | 8.31 ± 0.22 | 7.67 | 7.51 | 7.59 ± 0.11 | 7.75 | 7.83 | 7.79 ± 0.06 | 7.81 | 8.81 |
| nOPV Type | Sample Titer | MPBT Assay, Log10 titers | Log10 (Difference of Mean) Titers | |||||
|---|---|---|---|---|---|---|---|---|
| Non-Diluted Sample | Threefold Dilution of the Sample | |||||||
| Run 1 | Run 2 | Mean | Run 1 | Run 2 | Mean | |||
| tnOPV sample 1 run by operator 1 on day 1 | ||||||||
| 1 | 7.83 | 7.99 | 7.83 | 7.91 | 7.19 | 7.43 | 7.31 | 0.60 |
| 2 | 7.85 | 8.15 | 7.91 | 8.03 | 7.51 | 7.51 | 7.51 | 0.52 |
| 3 | 7.69 | 7.83 | 8.07 | 7.95 | 7.35 | 7.51 | 7.43 | 0.52 |
| tnOPV sample 1 run by operator 2 on day 2 | ||||||||
| 1 | 7.83 | 7.91 | 7.91 | 7.91 | 7.59 | 7.51 | 7.55 | 0.36 |
| 2 | 7.85 | 7.83 | 8.07 | 7.95 | 7.67 | 7.83 | 7.75 | 0.20 |
| 3 | 7.69 | 8.07 | 8.31 | 8.19 | 7.59 | 7.51 | 7.55 | 0.64 |
| tnOPV sample 2 run by operator 1 on day 2 | ||||||||
| 1 | 7.59 | 8.07 | 7.83 | 7.95 | 7.19 | 7.03 | 7.11 | 0.83 |
| 2 | 7.55 | 7.51 | 7.43 | 7.47 | 7.11 | 7.03 | 7.07 | 0.40 |
| 3 | 7.79 | 7.99 | 7.75 | 7.87 | 7.59 | 7.19 | 7.39 | 0.48 |
| Comparison between non-diluted versus threefold-diluted | ||||||||
| nOPV type | Delta: log10 Observed Titer—Expected log10 Sample Titer | Difference between dilutions | ||||||
| Non-diluted | Threefold-diluted | Non-diluted—threefold-diluted | ||||||
| Mean | SD | Mean | SD | Mean Difference | p-value | |||
| 1 | 0.17 | 0.17 | −0.43 | 0.15 | 0.60 | 0.0001 | ||
| 2 | 0.07 | 0.16 | −0.31 | 0.18 | 0.37 | 0.0006 | ||
| 3 | 0.28 | 0.23 | −0.27 | 0.18 | 0.55 | 0.0004 | ||
| Day | nOPV Type | MPBT Assay (log10CCID50/mL) | Intermediate Precision per Type | ||||
|---|---|---|---|---|---|---|---|
| Run 1 | Run 2 | Run 3 | Mean ± SD | Mean * ± SD * (Type) | %CV * (Type) | ||
| 1 | 1 | 7.58 | 7.32 | 7.39 | 7.43 ± 0.14 | 7.3 ± 0.15 (1) | 36.76% (1) |
| 2 | 7.09 | 7.24 | 7.20 | 7.18 ± 0.08 | 7.14 ± 0.16 (2) | 38.39% (2) | |
| 3 | 7.39 | 7.17 | 7.51 | 7.35 ± 0.17 | 7.29 ± 0.11 (3) | 26.49% (3) | |
| 2 | 1 | 7.35 | 7.24 | 7.35 | 7.32 ± 0.07 | ||
| 2 | 7.24 | 7.13 | 7.39 | 7.25 ± 0.13 | |||
| 3 | 7.32 | 7.28 | 7.35 | 7.32 ± 0.04 | |||
| 3 | 1 | 7.02 | 7.17 | 7.28 | 7.15 ± 0.13 | ||
| 2 | 6.90 | 7.20 | 6.90 | 7.00 ± 0.17 | |||
| 3 | 7.17 | 7.20 | 7.24 | 7.2 ± 0.04 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manukyan, H.; Lal, M.; Zhu, C.; Singh, O.; Lin, T.-L.; Tritama, E.; Chumakov, K.; Lee, S.-M.; Laassri, M. Application of MPBT Assay for Multiplex Determination of Infectious Titers and for Selection of the Optimal Formulation for the Trivalent Novel Oral Poliovirus Vaccine. Viruses 2024, 16, 961. https://doi.org/10.3390/v16060961
Manukyan H, Lal M, Zhu C, Singh O, Lin T-L, Tritama E, Chumakov K, Lee S-M, Laassri M. Application of MPBT Assay for Multiplex Determination of Infectious Titers and for Selection of the Optimal Formulation for the Trivalent Novel Oral Poliovirus Vaccine. Viruses. 2024; 16(6):961. https://doi.org/10.3390/v16060961
Chicago/Turabian StyleManukyan, Hasmik, Manjari Lal, Changcheng Zhu, Olga Singh, Tsai-Lien Lin, Erman Tritama, Konstantin Chumakov, Shwu-Maan Lee, and Majid Laassri. 2024. "Application of MPBT Assay for Multiplex Determination of Infectious Titers and for Selection of the Optimal Formulation for the Trivalent Novel Oral Poliovirus Vaccine" Viruses 16, no. 6: 961. https://doi.org/10.3390/v16060961
APA StyleManukyan, H., Lal, M., Zhu, C., Singh, O., Lin, T.-L., Tritama, E., Chumakov, K., Lee, S.-M., & Laassri, M. (2024). Application of MPBT Assay for Multiplex Determination of Infectious Titers and for Selection of the Optimal Formulation for the Trivalent Novel Oral Poliovirus Vaccine. Viruses, 16(6), 961. https://doi.org/10.3390/v16060961





