Geographic Medical Overview of Noncommunicable Diseases (Cardiovascular Diseases and Diabetes) in the Territory of the AP Vojvodina (Northern Serbia)
Abstract
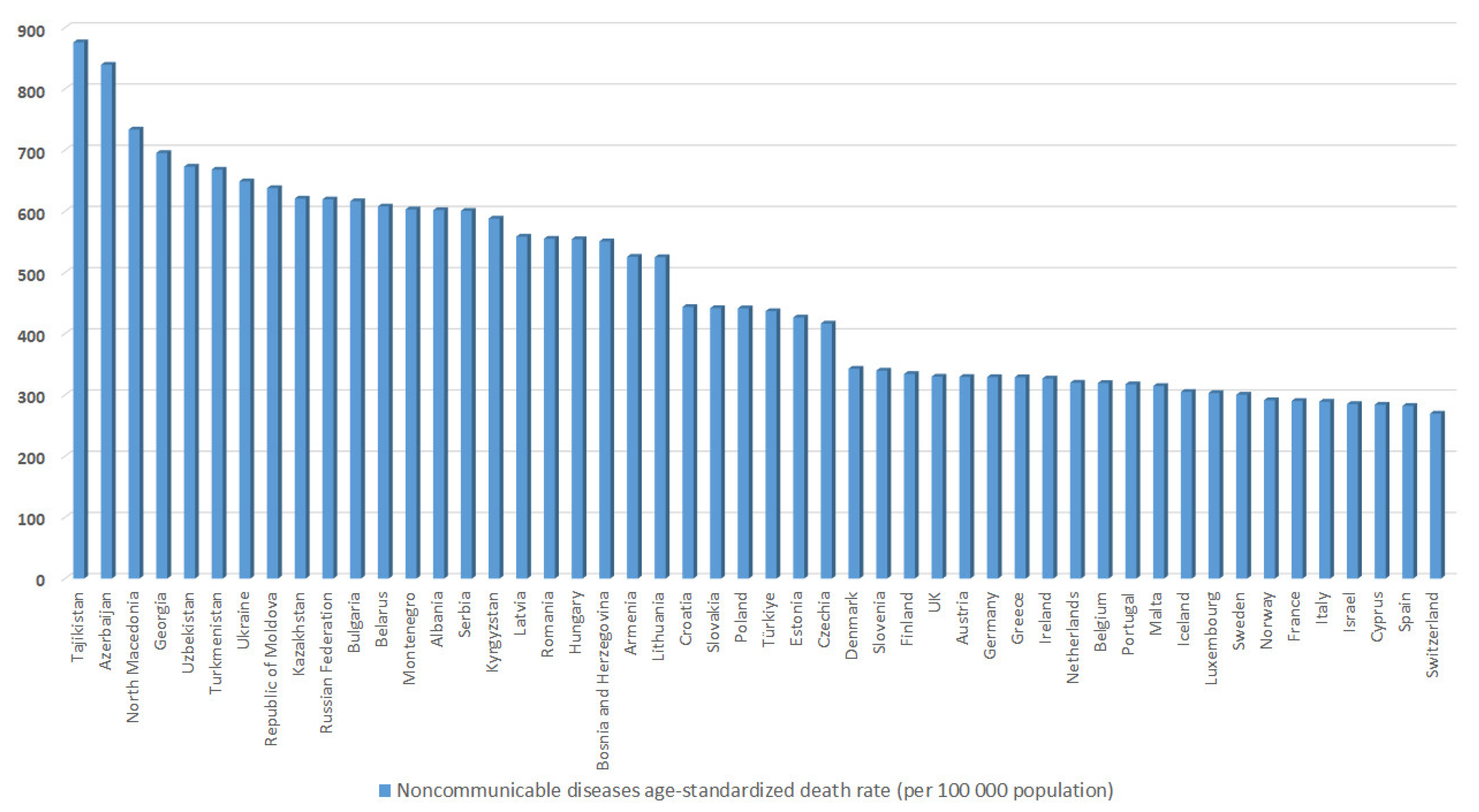
:1. Introduction
2. Materials and Methods
3. Results
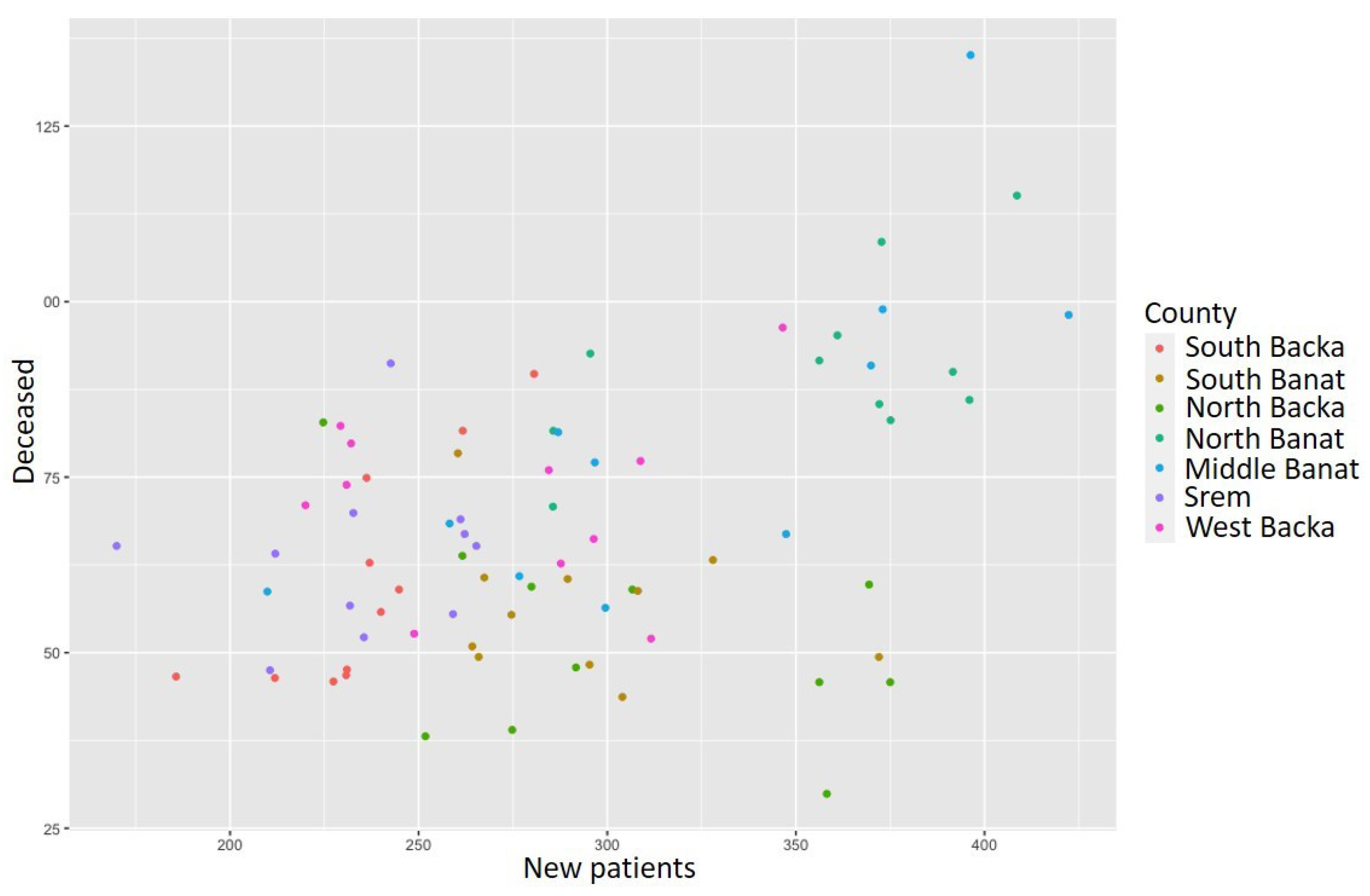
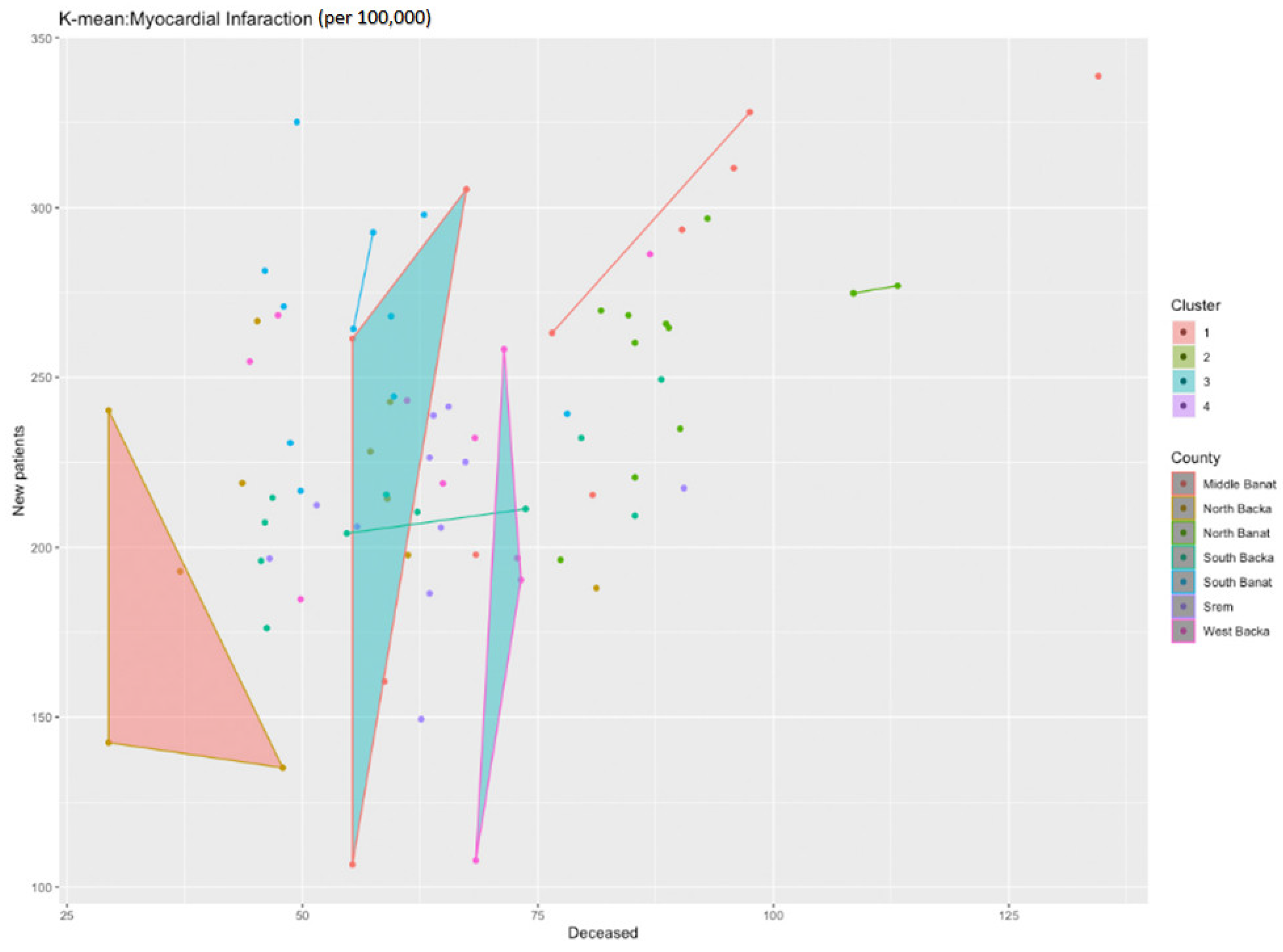
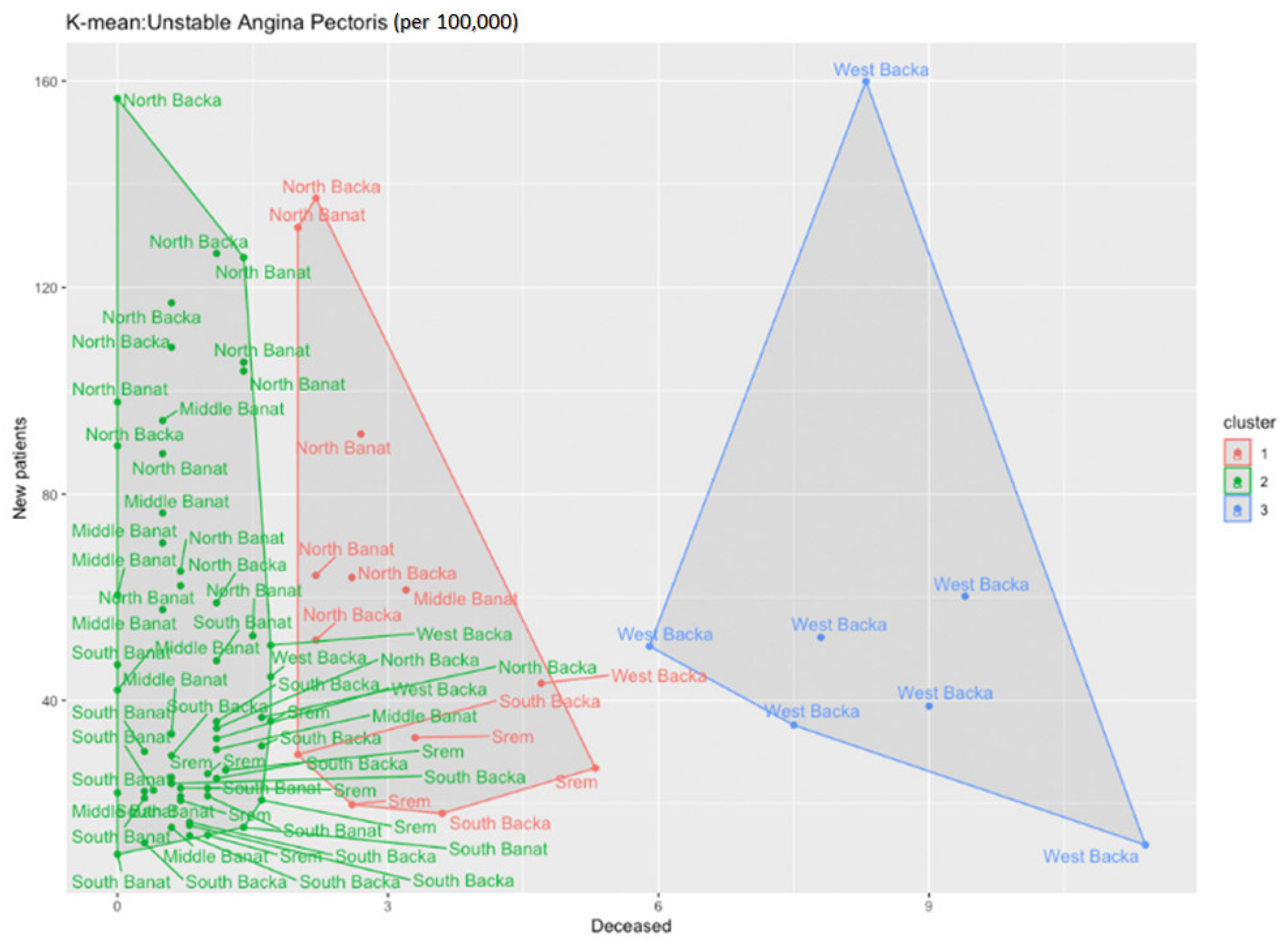
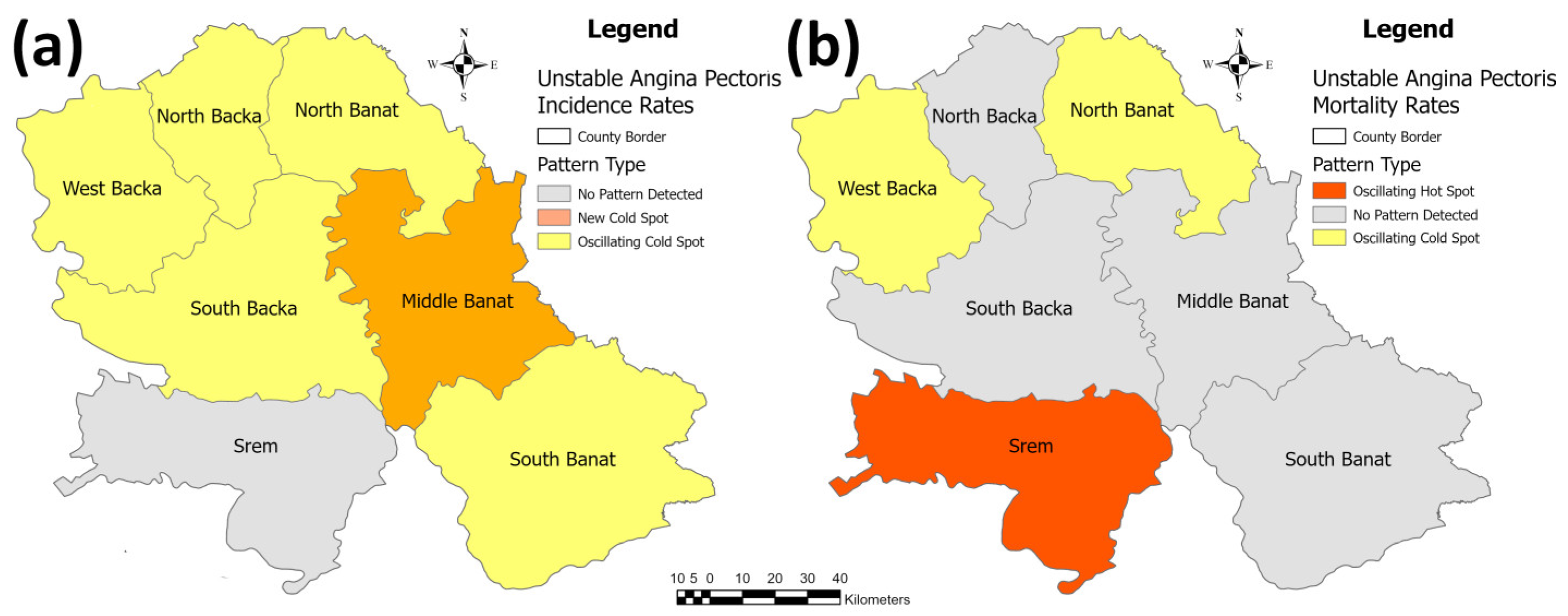
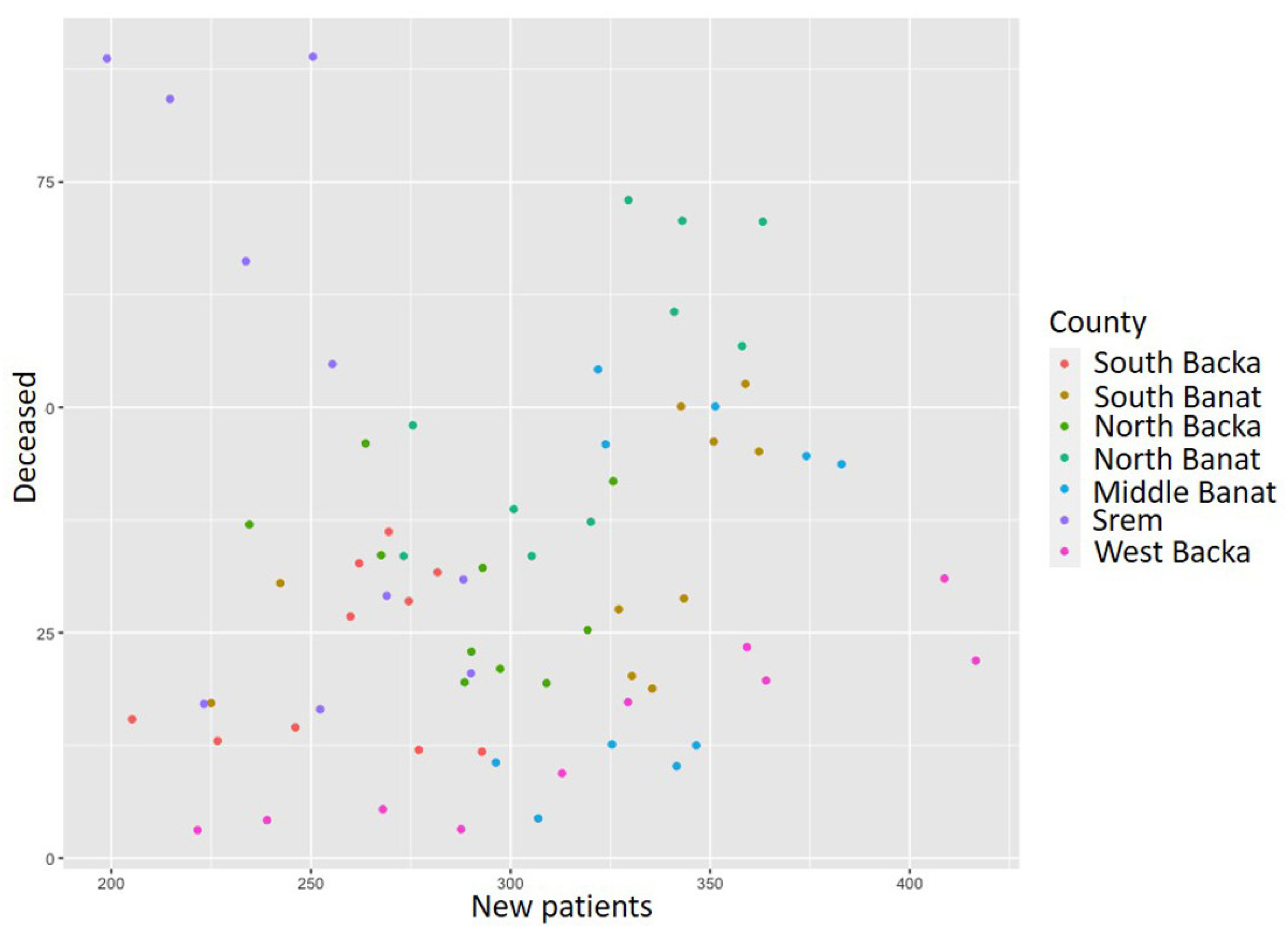
3.1. The Results of the Cardiovascular Diseases Research
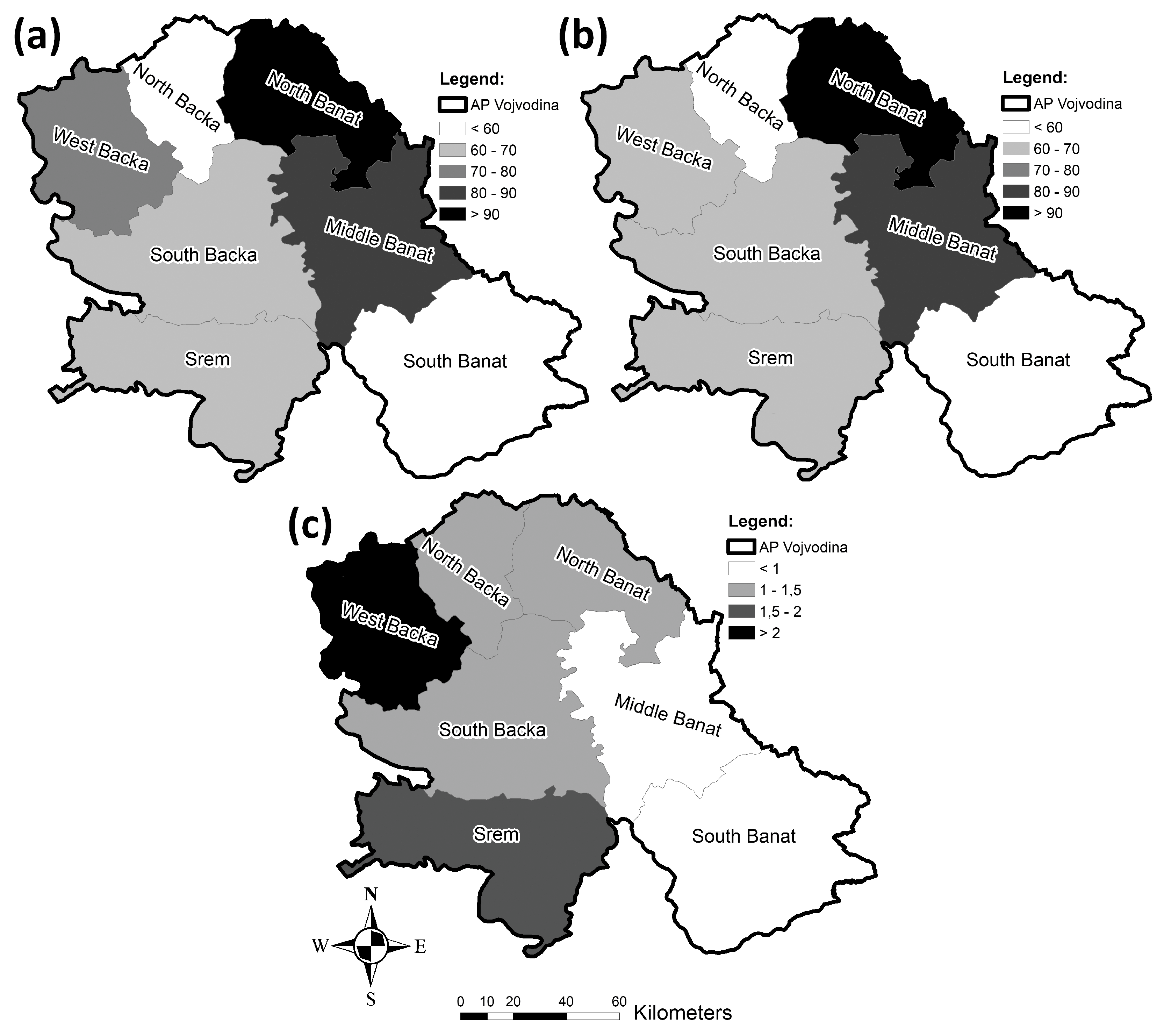
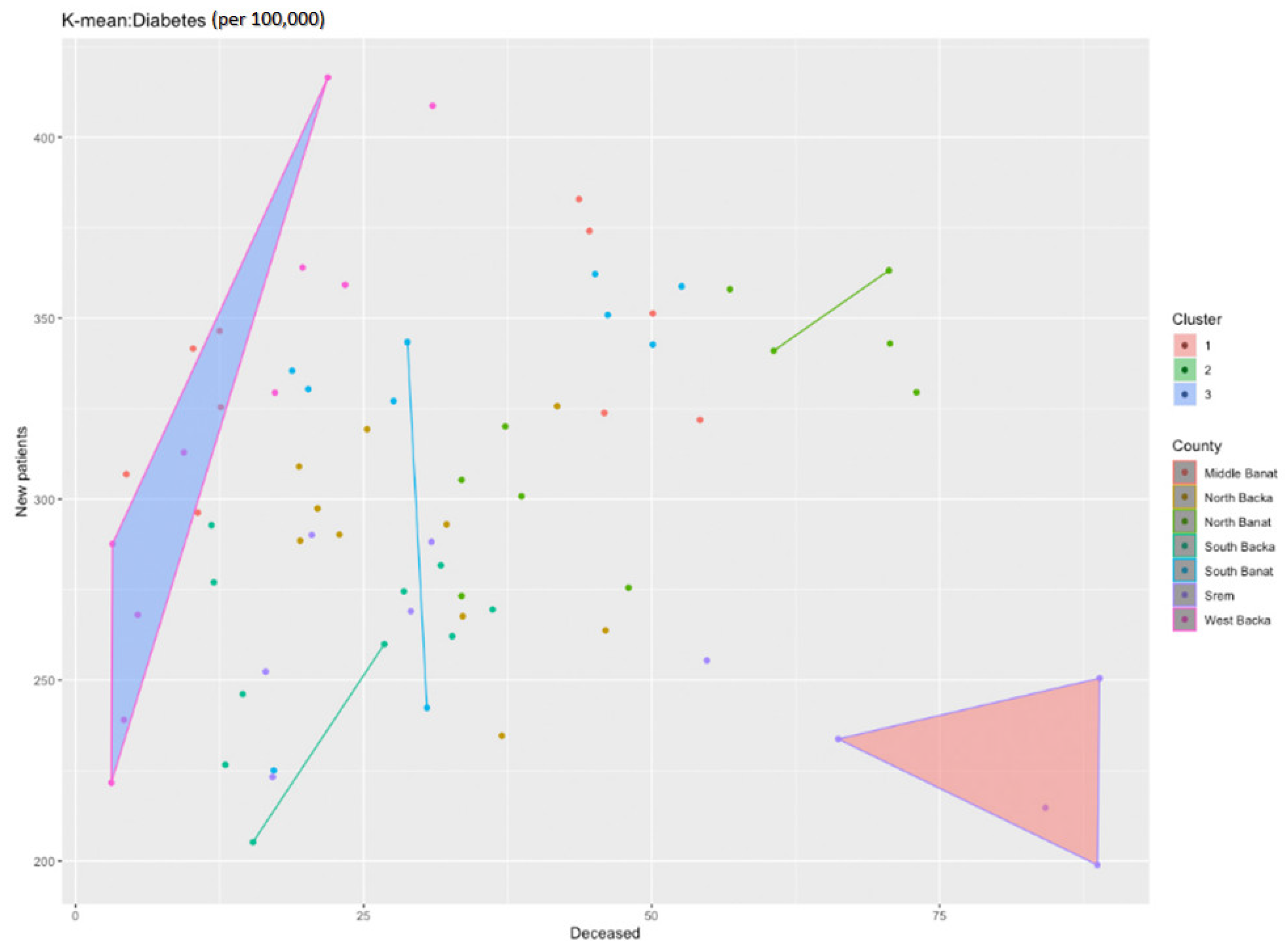
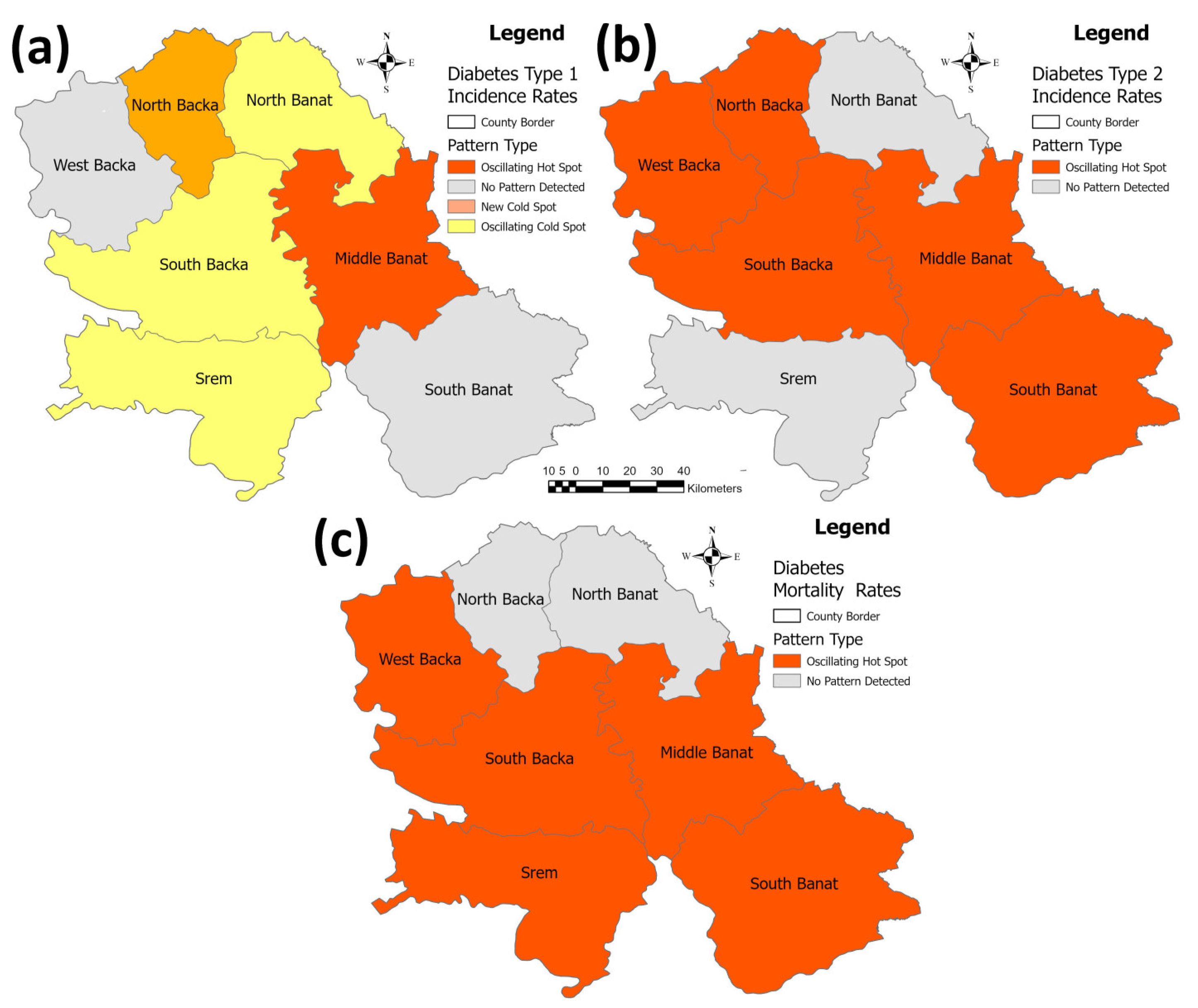
3.2. The Results of the Diabetes Research in the Studied Area
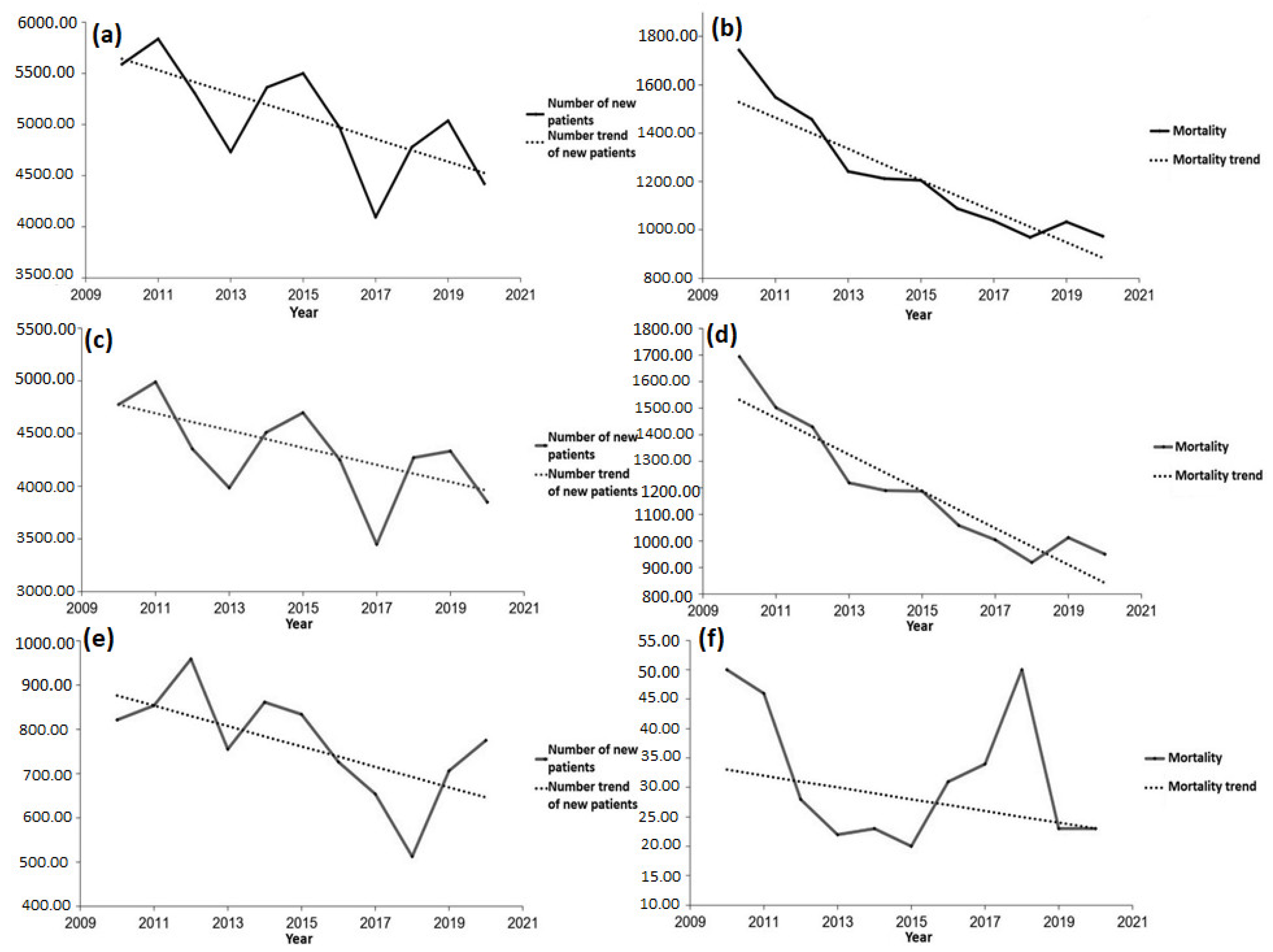
3.3. The Results of the Trends in Cardiovascular Diseases and Diabetes in the Researched Area
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Year | Province/County | Acute Coronary Syndrome | Year | Province/County | Acute Coronary Syndrome | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| New Patients | Mortality | New Patients | Mortality | ||||||||
| Number | Per 100,000 | Number of Deceased | Per 100,000 | Number | Per 100,000 | Number of Deceased | Per 100,000 | ||||
| 2010 | Vojvodina | 5594 | 285.8 | 1744 | 89.1 | 2016 | Vojvodina | 4974 | 264.4 | 1088 | 58.2 |
| South Backa | 1708 | 280.6 | 546 | 89.7 | Soth Backa | 1426 | 231 | 294 | 47.6 | ||
| South Banat | 777 | 260.4 | 234 | 78.4 | South Banat | 778 | 274.6 | 157 | 55.4 | ||
| North Backa | 429 | 224.7 | 158 | 82.8 | North Backa | 646 | 356.2 | 83 | 45.8 | ||
| North Banat | 621 | 408.6 | 175 | 115.1 | North Banat | 548 | 391.6 | 126 | 90 | ||
| Middle Banat | 757 | 396.3 | 258 | 135.1 | Middle Banat | 531 | 296.7 | 138 | 77.1 | ||
| Srem | 752 | 232.7 | 226 | 69.9 | Srem | 638 | 210.6 | 144 | 47.5 | ||
| West Backa | 550 | 284.5 | 147 | 76 | West Backa | 407 | 229.3 | 146 | 82.3 | ||
| 2011 | Vojvodina | 5839 | 300.1 | 1548 | 79.6 | 2017 | Vojvodina | 4099 | 219 | 1038 | 55.5 |
| South Backa | 1595 | 261.7 | 497 | 81.6 | South Backa | 1426 | 230.8 | 289 | 46.8 | ||
| South Banat | 970 | 328 | 187 | 63.2 | South Banat | 743 | 264.2 | 143 | 50.9 | ||
| North Backa | 496 | 261.6 | 121 | 63.8 | North Backa | 646 | 358.2 | 54 | 29.9 | ||
| North Banat | 560 | 372.7 | 163 | 108.5 | North Bnaat | 548 | 396 | 119 | 86 | ||
| Middle Banat | 705 | 373 | 187 | 98.9 | Middle Banat | 531 | 299.5 | 100 | 56.4 | ||
| Srem | 851 | 265.3 | 209 | 65.2 | Srem | 638 | 212 | 193 | 64.1 | ||
| West Backa | 662 | 346.5 | 184 | 96.3 | West Backa | 407 | 232.1 | 140 | 79.8 | ||
| 2012 | Vojvodina | 5313 | 276.4 | 1457 | 75.8 | 2018 | Vojvodina | 4781 | 256.8 | 969 | 52 |
| South Backa | 1454 | 236.2 | 461 | 74.9 | South Backa | 1406 | 227.4 | 284 | 45.9 | ||
| South Banat | 780 | 267.4 | 177 | 60.7 | South Banat | 849 | 304 | 122 | 43.7 | ||
| North Backa | 542 | 291.7 | 89 | 47.9 | North Backa | 493 | 274.8 | 70 | 39 | ||
| North Banat | 521 | 356.2 | 134 | 91.6 | North Banat | 391 | 285.6 | 97 | 70.8 | ||
| Middle Banat | 688 | 369.9 | 169 | 90.9 | Middle Banat | 486 | 276.7 | 107 | 60.9 | ||
| Srem | 753 | 242.6 | 283 | 91.2 | Srem | 775 | 259.1 | 166 | 55.5 | ||
| West Backa | 575 | 308.8 | 144 | 77.3 | West Backa | 381 | 220 | 123 | 71 | ||
| 2013 | Vojvodina | 4736 | 249,6 | 1241 | 64.9 | 2019 | Vojvodina | 5039 | 272.1 | 1034 | 55.8 |
| South Backa | 1443 | 237 | 387 | 62.8 | South Backa | 1311 | 211.9 | 287 | 46.4 | ||
| South Banat | 850 | 295.3 | 140 | 48.3 | South Banat | 1032 | 372 | 137 | 49.4 | ||
| North Backa | 561 | 306.65 | 109 | 59 | North Backa | 449 | 251.8 | 68 | 38.1 | ||
| North Banat | 411 | 285.7 | 118 | 81.6 | North Banat | 489 | 361 | 129 | 95.2 | ||
| Middle Banat | 527 | 287 | 150 | 81.4 | Middle Banat | 449 | 258.2 | 119 | 68.4 | ||
| Srem | 522 | 169.95 | 201 | 65.2 | Srem | 776 | 261.1 | 205 | 69 | ||
| West Backa | 422 | 230.9 | 136 | 73.9 | West Backa | 533 | 311.6 | 89 | 52 | ||
| 2014 | Vojvodina | 5368 | 282.2 | 1213 | 62.2 | 2020 | Vojvodina | 4421 | 240.2 | 973 | 52.9 |
| South Backa | 1479 | 240 | 344 | 55.8 | South Backa | 1149 | 185.7 | 288 | 46.6 | ||
| South Banat | 833 | 289.5 | 174 | 60.5 | South Banat | 732 | 265.9 | 136 | 49.4 | ||
| North Backa | 514 | 279.9 | 109 | 59.4 | North Backa | 664 | 375 | 81 | 45.8 | ||
| North Banat | 537 | 375.1 | 119 | 83.1 | North Banat | 400 | 295.5 | 124 | 92.6 | ||
| Middle Banat | 771 | 422.3 | 179 | 98.1 | Middle Banat | 361 | 209.9 | 101 | 58.7 | ||
| Srem | 711 | 231.8 | 174 | 56.7 | Srem | 695 | 235.5 | 154 | 52.2 | ||
| West Backa | 523 | 287.7 | 114 | 62.7 | West Backa | 420 | 248.8 | 89 | 52.7 | ||
| 2015 | Vojvodina | 5502 | 290.8 | 1206 | 64.,15 | ||||||
| South Backa | 1510 | 244.8 | 364 | 59 | |||||||
| South Banat | 880 | 308.1 | 168 | 58.8 | |||||||
| North Backa | 674 | 369.4 | 109 | 59.7 | |||||||
| North Banat | 527 | 372.1 | 121 | 85.4 | |||||||
| Middle Banat | 628 | 347.4 | 121 | 66.9 | |||||||
| Srem | 799 | 262.2 | 204 | 66.9 | |||||||
| West Backa | 484 | 296.4 | 119 | 66.2 | |||||||
| Year | Province/County | Myocardial Infarction | Unstable Angina Pectoris | ||||||
|---|---|---|---|---|---|---|---|---|---|
| New Patients | Mortality | New Patients | Mortality | ||||||
| Number | Per 100,000 | Number of Deceased | Per 100,000 | Number | Per 100,000 | Number of Deceased | Per 100,000 | ||
| 2010 | Vojvodina | 4773 | 243.8 | 1694 | 86.5 | 821 | 41.9 | 50 | 2.6 |
| South Backa | 1518 | 249.4 | 536 | 88.1 | 190 | 31.2 | 10 | 1.6 | |
| South Banat | 714 | 239.3 | 233 | 78.1 | 63 | 21.1 | 1 | 0.3 | |
| North Backa | 359 | 188 | 155 | 81.2 | 70 | 36.7 | 3 | 1.6 | |
| North Bnaat | 421 | 277 | 172 | 113.2 | 200 | 131.6 | 3 | 2 | |
| Middle Banat | 647 | 338.7 | 257 | 134.5 | 110 | 57.6 | 1 | 0.5 | |
| Srem | 665 | 205.8 | 209 | 64.7 | 87 | 26.9 | 17 | 5.3 | |
| West Backa | 449 | 232.2 | 132 | 68.3 | 101 | 52.2 | 15 | 7.8 | |
| 2011 | Vojvodina | 4986 | 256.2 | 1502 | 77.2 | 853 | 43.8 | 46 | 2.4 |
| South Backa | 1415 | 232.2 | 485 | 79.6 | 180 | 29.5 | 12 | 2 | |
| South Banat | 881 | 297.9 | 186 | 62.9 | 89 | 30.1 | 1 | 0.3 | |
| North Backa | 375 | 197.7 | 116 | 61.2 | 121 | 63.8 | 5 | 2.6 | |
| North Banat | 413 | 274.8 | 163 | 108.5 | 147 | 97.8 | 0 | 0 | |
| Middle Banat | 589 | 311.6 | 181 | 95.8 | 116 | 61.4 | 6 | 3.2 | |
| Srem | 766 | 238.8 | 205 | 63.9 | 85 | 26.5 | 4 | 1.2 | |
| West Backa | 547 | 286.3 | 166 | 86.9 | 115 | 60.2 | 18 | 9.4 | |
| 2012 | Vojvodina | 4354 | 226.5 | 1429 | 74.3 | 959 | 49.9 | 28 | 1.5 |
| South Backa | 1301 | 211.3 | 454 | 73.7 | 153 | 24.9 | 7 | 1.1 | |
| South Banat | 713 | 244.4 | 174 | 59.7 | 67 | 23 | 3 | 1 | |
| North Backa | 251 | 135.1 | 89 | 47.9 | 291 | 156.6 | 0 | 0 | |
| North Banat | 387 | 264.6 | 130 | 88.9 | 134 | 91.6 | 4 | 2.7 | |
| Middle Banat | 546 | 293.5 | 168 | 90.3 | 142 | 76.3 | 1 | 0.5 | |
| Srem | 675 | 217.4 | 281 | 90.5 | 78 | 25.1 | 2 | 0.6 | |
| West Backa | 481 | 258.3 | 133 | 71.4 | 94 | 50.5 | 11 | 5.9 | |
| 2013 | Vojvodina | 3981 | 208.2 | 1219 | 63.8 | 755 | 39.5 | 22 | 1.2 |
| South Backa | 1296 | 210.4 | 383 | 62.2 | 147 | 23.9 | 4 | 0.6 | |
| South Banat | 785 | 270.9 | 139 | 48 | 65 | 22.4 | 1 | 0.3 | |
| North Backa | 396 | 214.3 | 109 | 59 | 165 | 89.3 | 0 | 0 | |
| North Banat | 284 | 196.3 | 112 | 77.4 | 127 | 87.8 | 1 | 0.5 | |
| Middle Banat | 397 | 215.4 | 149 | 80.8 | 130 | 70.5 | 1 | 0.5 | |
| Srem | 461 | 149.4 | 193 | 62.6 | 61 | 19.8 | 8 | 2.6 | |
| West Backa | 362 | 196.8 | 134 | 72.8 | 60 | 32.6 | 2 | 1.1 | |
| 2014 | Vojvodina | 4507 | 237 | 1190 | 62.6 | 861 | 45.3 | 23 | 1.2 |
| South Backa | 1258 | 204.1 | 337 | 54.7 | 221 | 35.9 | 7 | 1.1 | |
| South Banat | 771 | 268 | 171 | 59.4 | 62 | 21.5 | 3 | 1 | |
| North Backa | 419 | 228.2 | 105 | 57.2 | 95 | 51.7 | 4 | 2.2 | |
| North Banat | 386 | 269.7 | 117 | 81.7 | 151 | 105.5 | 2 | 1.4 | |
| Middle Banat | 599 | 328.1 | 178 | 97.5 | 172 | 94.2 | 1 | 0.5 | |
| Srem | 632 | 206.1 | 171 | 55.8 | 779 | 25.8 | 3 | 1 | |
| West Backa | 442 | 243.2 | 111 | 61.1 | 81 | 44.6 | 3 | 1.7 | |
| 2015 | Vojvodina | 4699 | 246.8 | 1186 | 63.1 | 833 | 44 | 20 | 1.1 |
| South Backa | 1329 | 215.5 | 360 | 58.9 | 181 | 29.3 | 4 | 0.6 | |
| South Banat | 836 | 292.7 | 164 | 57.5 | 44 | 15.4 | 4 | 1.4 | |
| North Backa | 443 | 242.8 | 107 | 59.3 | 231 | 126.6 | 2 | 1.1 | |
| North Banat | 380 | 268.3 | 119 | 84.6 | 147 | 103.8 | 2 | 1.4 | |
| Middle Banat | 552 | 305.4 | 121 | 67.4 | 76 | 42 | 0 | 0 | |
| Srem | 736 | 241.4 | 199 | 65.5 | 63 | 20.7 | 5 | 1.6 | |
| West Backa | 393 | 218.8 | 116 | 64.9 | 91 | 50.7 | 3 | 1.7 | |
| 2016 | Vojvodina | 4248 | 225.8 | 1057 | 56.2 | 726 | 38.6 | 31 | 1.6 |
| South Backa | 1325 | 214.6 | 289 | 46.8 | 101 | 16.4 | 5 | 0.8 | |
| South Banat | 749 | 264.3 | 157 | 55.4 | 29 | 10.2 | 0 | 0 | |
| North Backa | 397 | 218.9 | 79 | 43.6 | 249 | 137.3 | 4 | 2.2 | |
| North Banat | 372 | 265.8 | 124 | 88.6 | 176 | 125.8 | 2 | 1.4 | |
| Middle Banat | 471 | 263.1 | 137 | 76.5 | 60 | 33.5 | 1 | 0.6 | |
| Srem | 596 | 196.7 | 141 | 46.5 | 42 | 13.9 | 3 | 1 | |
| West Backa | 338 | 190.4 | 130 | 73.2 | 69 | 38.9 | 16 | 9 | |
| 2017 | Vojvodina | 3446 | 184.1 | 1004 | 53.6 | 653 | 34.9 | 34 | 1.8 |
| South Backa | 1281 | 207.3 | 284 | 46 | 85 | 13.8 | 5 | 0.8 | |
| South Banat | 609 | 216.6 | 140 | 49.8 | 134 | 47.7 | 3 | 1.1 | |
| North Backa | 257 | 142.5 | 53 | 29.4 | 211 | 117 | 1 | 0.6 | |
| North Banat | 360 | 260.2 | 118 | 85.3 | 86 | 62.2 | 1 | 0.7 | |
| Middle Banat | 189 | 106.6 | 98 | 55.3 | 54 | 30.5 | 2 | 1.1 | |
| Srem | 561 | 186.4 | 191 | 63.5 | 62 | 20.6 | 2 | 0.7 | |
| West Backa | 189 | 107.8 | 120 | 68.4 | 21 | 12 | 20 | 11.4 | |
| 2018 | Vojvodina | 4269 | 229.3 | 919 | 53.6 | 512 | 27.5 | 50 | 2.7 |
| South Backa | 1294 | 209.3 | 96 | 85.3 | 112 | 18.1 | 22 | 3.6 | |
| South Banat | 786 | 281.4 | 262 | 46 | 63 | 22.6 | 1 | 0.4 | |
| North Backa | 431 | 240.3 | 68 | 29.4 | 62 | 34.6 | 2 | 1.1 | |
| North Banat | 302 | 220.6 | 96 | 85.3 | 89 | 65 | 1 | 0.7 | |
| Middle Banat | 459 | 261.4 | 106 | 55.3 | 27 | 15.4 | 1 | 0.6 | |
| Srem | 677 | 226.4 | 156 | 63.5 | 98 | 32.8 | 10 | 3.3 | |
| West Backa | 320 | 184.7 | 110 | 49.8 | 61 | 35.2 | 13 | 7.5 | |
| 2019 | Vojvodina | 4333 | 234 | 1.,011 | 54.6 | 706 | 38.1 | 23 | 1.2 |
| South Backa | 1213 | 196 | 282 | 45.6 | 98 | 15.8 | 5 | 0.8 | |
| South Banat | 902 | 325.2 | 137 | 49.4 | 130 | 46.9 | 0 | 0 | |
| North Backa | 344 | 192.9 | 66 | 37 | 105 | 58.9 | 2 | 1.1 | |
| North Banat | 402 | 296.8 | 126 | 93 | 87 | 64.2 | 3 | 2.2 | |
| Middle Banat | 344 | 197.8 | 119 | 68.4 | 105 | 60.4 | 0 | 0 | |
| Srem | 669 | 225.1 | 200 | 67.3 | 107 | 36 | 5 | 1.7 | |
| West Backa | 459 | 268.3 | 81 | 47.4 | 74 | 43.3 | 8 | 4.7 | |
| 2020 | Vojvodina | 3848 | 209 | 950 | 51.6 | 775 | 42.1 | 23 | 1.2 |
| South Backa | 1090 | 176.2 | 286 | 46.2 | 77 | 12.4 | 2 | 0.3 | |
| South Banat | 695 | 230.7 | 134 | 48.7 | 59 | 21.4 | 2 | 0.7 | |
| North Backa | 472 | 266.6 | 80 | 45.2 | 192 | 108.4 | 1 | 0.6 | |
| North Banat | 318 | 234.9 | 122 | 90.1 | 71 | 52.5 | 2 | 1.5 | |
| Middle Banat | 276 | 160.5 | 101 | 58.7 | 38 | 22.1 | 0 | 0 | |
| Srem | 627 | 212.4 | 152 | 51.5 | 68 | 23 | 2 | 0.7 | |
| West Backa | 430 | 254.7 | 75 | 44.4 | 270 | 159.9 | 14 | 8.3 | |
| Year | County | Diabetes Type 1 | Diabetes Type 2 | Mortality (Both Types) | Year | County | Diabetes Type 1 | Diabetes Type 2 | Mortality (Both Types) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| New Patients | New Patients | New Patients | New Patients | ||||||||||||
| Number | Per 100,000 | Number | Per 100,000 | Number of Deceased | Per 100,000 | Number | Per 100,000 | Number | Per 100,000 | Number of Deceased | Per 100,000 | ||||
| 2010 | South Backa | 19 | 8.7 | 1196 | 196.5 | 94 | 15.4 | 2015 | South Backa | 32 | 15.4 | 1567 | 254.1 | 223 | 36.2 |
| South Banat | 12 | 11.4 | 689 | 230.9 | 91 | 30.5 | South Banat | 5 | 5.5 | 963 | 337.2 | 143 | 50.1 | ||
| North Backa | 17 | 26.2 | 540 | 282.8 | 37 | 19.4 | North Backa | 7 | 12.2 | 459 | 251.5 | 84 | 46 | ||
| North Banat | 6 | 11.7 | 401 | 263.8 | 73 | 48 | North Banat | 6 | 13.7 | 495 | 349.5 | 100 | 70.6 | ||
| Middle Banat | 8 | 12.4 | 598 | 313 | 24 | 12.6 | Middle Banat | 2 | 3.5 | 579 | 320.3 | 83 | 45.9 | ||
| Srem | 13 | 11.3 | 833 | 257.7 | 94 | 29.1 | Srem | 9 | 9.4 | 735 | 241.1 | 271 | 88.9 | ||
| West Backa | 6 | 9.5 | 410 | 212.1 | 6 | 3,1 | West Backa | 8 | 14.9 | 565 | 314.5 | 31 | 17.3 | ||
| 2011 | South Backa | 29 | 13.4 | 1299 | 213.2 | 79 | 13 | 2016 | South Backa | 26 | 12.6 | 1661 | 269.1 | 196 | 31.7 |
| South Banat | 17 | 16.4 | 617 | 208.6 | 51 | 17.2 | South Banat | 12 | 13.5 | 956 | 337.4 | 131 | 46.2 | ||
| North Backa | 15 | 23.5 | 561 | 295.8 | 48 | 25.3 | North Backa | 11 | 19.4 | 450 | 248.2 | 61 | 33.6 | ||
| North Banat | 8 | 16 | 457 | 304.1 | 56 | 37.3 | North Banat | 8 | 18.6 | 454 | 324.4 | 99 | 70.7 | ||
| Middle Banat | 6 | 9.5 | 542 | 286.8 | 20 | 10.6 | Middle Banat | 6 | 10.7 | 557 | 311.2 | 97 | 54.2 | ||
| Srem | 10 | 8.8 | 896 | 279.4 | 99 | 30.9 | Srem | 7 | 7.4 | 628 | 207.3 | 255 | 84.2 | ||
| West Backa | 7 | 11.3 | 435 | 227.7 | 8 | 4.2 | West Backa | 11 | 20.9 | 609 | 343.1 | 35 | 19.7 | ||
| 2012 | South Backa | 21 | 9.8 | 1455 | 236.3 | 87 | 14.5 | 2017 | South Backa | 13 | 8.8 | 1565 | 253.3 | 202 | 32.7 |
| South Banat | 12 | 12.6 | 927 | 317.8 | 59 | 20.2 | South Banat | 7 | 11.4 | 977 | 347.4 | 148 | 52.6 | ||
| North Backa | 9 | 14.9 | 525 | 282.5 | 39 | 21 | North Backa | 6 | 19.6 | 493 | 273.4 | 58 | 32.2 | ||
| North Banat | 5 | 10.7 | 384 | 262.5 | 49 | 33.5 | North Banat | 5 | 16.6 | 433 | 312.9 | 101 | 73 | ||
| Middle Banat | 14 | 23.3 | 592 | 318.3 | 19 | 10.2 | Middle Banat | 3 | 10.9 | 644 | 363.2 | 79 | 44.6 | ||
| Srem | 10 | 9.9 | 662 | 213.3 | 53 | 17.1 | Srem | 6 | 11.8 | 563 | 187.1 | 267 | 88.7 | ||
| West Backa | 10 | 17.4 | 503 | 270.2 | 6 | 3.2 | West Backa | 2 | 3.9 | 623 | 355.3 | 41 | 23.4 | ||
| 2013 | South Backa | 26 | 12.3 | 1631 | 264.7 | 74 | 12 | 2018 | South Backa | 24 | 11.9 | 1624 | 262.6 | 176 | 28.5 |
| South Banat | 7 | 7.5 | 926 | 319.6 | 80 | 27.6 | South Banat | 7 | 8.1 | 989 | 354.1 | 126 | 45.1 | ||
| North Backa | 8 | 13.5 | 508 | 275 | 36 | 19.5 | North Backa | 9 | 16.3 | 555 | 309.4 | 75 | 41.8 | ||
| North Banat | 7 | 15.3 | 413 | 285.5 | 56 | 38.7 | North Banat | 6 | 14.5 | 447 | 326.5 | 83 | 60.6 | ||
| Middle Banat | 13 | 22 | 598 | 324.5 | 23 | 12.5 | Middle Banat | 8 | 14.8 | 591 | 336.5 | 88 | 50.1 | ||
| Srem | 12 | 12.1 | 741 | 240.2 | 51 | 16.5 | Srem | 8 | 8.7 | 673 | 225 | 198 | 66.2 | ||
| West Backa | 8 | 14.2 | 467 | 253.8 | 10 | 5.4 | West Backa | 10 | 19.9 | 687 | 396.6 | 38 | 21.9 | ||
| 2014 | South Backa | 24 | 11.5 | 1734 | 281.3 | 73 | 11.8 | 2019 | South Backa | 23 | 11.4 | 1538 | 248.5 | 166 | 26.8 |
| South Banat | 10 | 10.9 | 934 | 324.6 | 54 | 18.8 | South Banat | 10 | 11.7 | 920 | 331.7 | 80 | 28.8 | ||
| North Backa | 5 | 8.6 | 517 | 281.6 | 42 | 22.9 | North Backa | 5 | 9.1 | 402 | 225.5 | 66 | 37 | ||
| North Banat | 5 | 11.2 | 421 | 294.1 | 48 | 33.5 | North Banat | 6 | 14.7 | 465 | 343.3 | 77 | 56.8 | ||
| Middle Banat | 8 | 13.8 | 535 | 293.1 | 8 | 4.4 | Middle Banat | 10 | 18.8 | 633 | 364.1 | 76 | 43.7 | ||
| Srem | 17 | 17.5 | 836 | 272.6 | 63 | 20.5 | Srem | 14 | 15.5 | 713 | 239.9 | 163 | 54.8 | ||
| West Backa | 9 | 16.4 | 539 | 296.5 | 17 | 9,4 | West Backa | 2 | 4.1 | 692 | 404.6 | 53 | 31 | ||
References
- Cvejin-Martinov, M.; Grujić, V.; Šušnjević, S.; Kvrgić, S.; Arsić, M.; Nikolič, A. Health of the population of Vojvodina. Med. Pregl. 2007, 60, 559–563. (In Serbian) [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Data Portal. Available online: https://ncdportal.org/ (accessed on 12 October 2022).
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018.
- Timmis, A.; Vardas, P.; Townsend, N.; Torbica, A.; Katus, H.; De Smedt, D.; Gale, C.P.; Maggioni, A.P.; Petersen, S.E.; Huculeci, R.; et al. European Society of Cardiology, on behalf of the Atlas Writing Group, European Society of Cardiology: Cardiovascular disease statistics 2021. Eur. Heart J. 2022, 43, 716–799. [Google Scholar] [CrossRef] [PubMed]
- Maksimović, Z.; Jovanović, T.; Ršumović, M.; Đorđević, M. Magnesium and calcium in drinking water in relation to cadiovascular mortality in Serbia. In Magnesium in the Environment and Organisms; SANU, Scientific Meetings; Book 1; Department of Mathematics, Physics and Geo-Sciences, Department of Chemical and Biological Sciences: Belgrade, Serbia, 1999; Volume XCII, pp. 21–27. [Google Scholar]
- Velicki, R. Determining the Connection between the Mediterranean Diet and Risk Factors for the Onset of Acute Coronary Syndrome Using the “MedDiet” Score. Ph.D. Dissertation, Faculty of Medicine, University in Novi Sad, Novi Sad, Serbia, 2017. (In Serbian). [Google Scholar]
- Poloniecki, J.; Atkinson, R.; de Leon, A.; Anderson, H. Daily time series for cardiovascular hospital admissions and previous day’s air pollution in London, UK. Occup. Environ. Med. 1997, 54, 35–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jevtić, M.; Dragić, N.; Bijelović, S.; Popović, M. Cardiovascular diseases and air pollution in Novi Sad, Serbia. Int. J. Occup. Med. Environ. Health 2014, 27, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health of the Republic of Serbia. The Republic’s expert commission for the development and implementation of good clinical practice guidelines. In National Guide to Good Clinical Practice Diabetes Mellitus; Agency for Accreditation of Medical Institutions of Serbia: Belgrade, Serbia, 2013; pp. 1–82. (In Serbian) [Google Scholar]
- Samuelsson, U.; Löfman, O. Geographical mapping of type 1 diabetes in children and adolescents in south east Sweden. J. Epidemiol. Community Health 2004, 58, 388–392. [Google Scholar] [CrossRef] [Green Version]
- Samuelsson, U.; Westerberg, L.; Aakesson, K.; Birkebaek, N.H.; Bjarnason, R.; Drivvoll, A.K.; Skrivarhaug, T.; Svensson, J.; Thorsson, A.; Hanberger, L. Nordic Childhood Diabetes Registry Study Group, NordicDiabKids. Geographical variation in the incidence of type 1 diabetes in the Nordic countries: A study within NordicDiabKids. Pediatr. Diabetes 2020, 2, 259–265. [Google Scholar] [CrossRef]
- Jovanović, D. Association between Arsenic in Drinking Water and the Occurrence of Type 2 Diabetes. Ph.D. Thesis, Faculty of Medicine, University in Belgrade, Belgrade, Serbia, 26 December 2013. (In Serbian). [Google Scholar]
- International Diabetes Federation. IDF Diabetes Atlas 2021—10th edition. Available online: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf (accessed on 12 October 2022).
- Register for Diabetes in Serbia. Incidence and Mortality from Diabetes 2019; Report no. 14; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for Diabetes in Serbia: Belgrade, Serbia, 2020; pp. 1–92. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2019; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2020; pp. 1–149. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2018; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2019. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2020; Report no. 15; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2021; pp. 1–101. (In Serbian) [Google Scholar]
- Bahri, M.A.S.; Sabri, S.; Johar, F.; Kararbassi, Z.; Majid, M.R.; Ludin, A.N.M. Comparison of Spatial Autocorrelation Analysis Methods for Distribution Pattern of Diabetes Type II Patients in Iskandar Malaysia Neighbourhoods. In International Conference on Urban and Regional Planning; Universiti Teknologi Malaysia: Johor Bahru, Malaysia, 2014. [Google Scholar]
- Kuznetsov, A.; Sadovskaya, V. Spatial Variation and Hotspot Detection of COVID-19 Cases in Kazakhstan, 2020. Spat. Spatiotemporal. Epidemiol. 2021, 39, 100430. [Google Scholar] [CrossRef]
- Shariati, M.; Mesgari, T.; Kasraee, M.; Jahangiri-rad, M. Spatiotemporal Analysis and Hotspots Detection of COVID-19 Using Geographic Information System. J. Environ. Health Sci. Eng. 2020, 18, 1499–1507. [Google Scholar] [CrossRef]
- McEntee, J.C.; Ogneva-Himmelberger, Y. Diesel Particulate Matter, Lung Cancer, and Asthma Incidences along Major Traffic Corridors in MA, USA: A GIS Analysis. Health Place 2008, 14, 817–828. [Google Scholar] [CrossRef]
- Termeh, S.R.; Niaraki, A.S.; Choi, S.M. Asthma prone areas modeling using a machine learning model. Sci. Rep. 2021, 11, 1912. [Google Scholar] [CrossRef]
- Mahara, G.; Karki, M.; Yang, K.; Chen, S.; Wang, W.; Guo, X. Space-Time Cluster Analysis of Tuberculosis Incidence in Beijing, China. J. Tuberc. Res. 2018, 6, 302–319. [Google Scholar] [CrossRef] [Green Version]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2010; Report no. 5; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2011; pp. 1–127. ISBN 978-86-7358-045-6. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2011; Report no. 6; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2012; pp. 1–107. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in SERBIA for 2012; Report no. 7; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2013; pp. 1–98. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2013; Report no. 8; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2014; pp. 1–96. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2014; Report no. 9; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2015; pp. 1–98. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2015; Report no. 10; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2016; pp. 1–98. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2016; Report no. 11; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2017; pp. 1–97. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2017; Report no. 12; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2018; pp. 1–100. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2018; Report no. 13; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2019; pp. 1–101. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Registry for acute coronary syndrome in Serbia. In Incidence and Mortality from Acute Coronary Syndrome in Serbia for 2019; Report no. 14; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2020; pp. 1–101. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2010; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2011. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2011; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2012. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2012; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2013. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2013; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2014. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2014; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2015. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2015; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2016. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2016; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2017. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2017; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2018. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2019; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2020. (In Serbian) [Google Scholar]
- Institute of Public Health of Serbia “Dr Milan Jovanović Batut”. Health and Statistical Yearbook of the Republic of Serbia 2020; Institute of Public Health of Serbia “Dr Milan Jovanović Batut”: Belgrade, Serbia, 2021. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2006; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2007; pp. 1–187. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2009; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2010; pp. 1–197. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2010; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2011; pp. 1–188. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2011; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2012; pp. 1–172. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2012; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2013; pp. 1–90. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2013; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2014; pp. 1–203. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2014; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2015; pp. 1–97. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2015; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2016; pp. 1–119. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2016; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2017; pp. 1–126. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2017; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2018. (In Serbian) [Google Scholar]
- Institute of Public Health of Vojvodina. Population Health Status of Vojvodina in 2018; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2019; pp. 1–156. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2010; Report no. 5; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for diabetes in Serbia: Belgrade, Serbia, 2011; pp. 1–95. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2011; Report no. 6; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for diabetes in Serbia: Belgrade, Serbia, 2012; pp. 1–96. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2012; Report no. 7; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for diabetes in Serbia: Belgrade, Serbia, 2013; pp. 1–84. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2013; Report no. 8; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for diabetes in Serbia: Belgrade, Serbia, 2014; pp. 1–83. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2014; Report no. 9; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for diabetes in Serbia: Belgrade, Serbia, 2015; pp. 1–82. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2015; Report no. 10; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for diabetes in Serbia: Belgrade, Serbia, 2016; pp. 1–80. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2016; Report no. 11; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Register for diabetes in Serbia: Belgrade, Serbia, 2017; pp. 1–81. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2017; Report no. 12; Institute of Public Health of Serbia “Dr Milan Jovanović Batut and Register for diabetes in Serbia: Belgrade, Serbia, 2018; pp. 1–89. (In Serbian) [Google Scholar]
- Register for diabetes in Serbia. Incidence and Mortality from Diabetes 2018; Report no. 13; Institute of Public Health of Serbia “Dr Milan Jovanović Batut and Register for diabetes in Serbia: Belgrade, Serbia, 2019; pp. 1–90. (In Serbian) [Google Scholar]
- Čvoro, J.; Golubović, P. Geography of Yugoslavia; National Library of Serbia: Belgrade, Serbia, 2001. (In Serbian) [Google Scholar]
- Tomić, P.; Romelić, J.; Kicošev, S.; Lazić, L. Population of Vojvodina, 2nd ed.; Association of Geographers of Vojvodina: Novi Sad, Serbia, 2004. [Google Scholar]
- Proroković, D. Threats to regional security and consequences for the geopolitical position of Vojvodina. In The Culture of Polis, Journal for Fostering a Democratic Political Structure, Special ed. 15(1); Vojvodina as a potential geopolitical focal point in the Republic of Serbia: Belgrade, Serbia, 2018; pp. 25–38. (In Serbian) [Google Scholar]
- Meggiorin, M.; Passadore, G.; Bertoldo, S.; Sottani, A.; Rinaldo, A. Assessing the long-term sustainability of the groundwater resources in the Bacchiglione basin (Veneto, Italy) with the Mann–Kendall test: Suggestions for higher reliability. Acque Sotter.-Ital. J. Groundw. 2021, 499, 35–48. [Google Scholar] [CrossRef]
- Gavrilov, M.B.; Marković, S.B.; Jarad, A.; Korać, V.M. The Analysis of Temperature Trends in Vojvodina (Serbia) from 1949 to 2006. Therm. Sci. 2015, 19 (Suppl. S2), 339–350. [Google Scholar] [CrossRef]
- Mann, H.B. Non-parametric tests against trend. Econometrica 1945, 13, 245–259. [Google Scholar] [CrossRef]
- Kendall, M.G. Rank Correlation Methods, 4th ed.; Charles Griffin: London, UK, 1975. [Google Scholar]
- Lettenmaier, D.P. Multivariate Nonparametric Tests for Trend in Water Quality. Water Resour. Bull. 1988, 24, 505–512. [Google Scholar] [CrossRef]
- Ghalharia, G.F.; Dastjerdib, J.K.; Nokhandanc, M.H. Using Mann Kendal and t-test methods in identifying trends of climatic elements: A case study of northern parts of Iran. Manag. Sci. Lett. 2012, 2, 911–920. [Google Scholar] [CrossRef]
- Hirsch, R.M.; Slack, J.R.; Smith, R.A. Techniques of trend analysis for monthly water quality data. Water Resour. 1982, 18, 107–121. [Google Scholar] [CrossRef] [Green Version]
- Gavrilov, M.B.; Marković, S.B.; Janc, N.; Nikolić, M.; Valjarević, A.Đ.; Komac, B.; Zorn, M.; Punišić, M.; Bačević, N. Assessing average annual air temperature trends using the Mann-Kendall test in Kosovo. Acta Geogr. Slov. 2017, 58, 7–26. [Google Scholar] [CrossRef] [Green Version]
- Zainuddin, A.A.; Rahim, A.; Rasyid, H.; Ramadany, S.; Dharmayani, H.; Abdullah, A.A. Personal communication. 2022. Geospatial Analysis of Diabetes Type 2 and Hypertension in South Sulawesi, Indonesia, Preprint. 2022. Available online: Assets.researchsquare.com/files/rs-2031474/v1/0fa625c9-fd2b-4ca6-a7a8-a631f60f63e2.pdf?c=1663716153 (accessed on 12 October 2022).
- Kumari, B.; Pandey, A.C. MODIS Based Forest Fire Hotspot Analysis and Its Relationship with Climatic Variables. Spat. Inf. Res. 2020, 28, 87–99. [Google Scholar] [CrossRef]
- Said, S.N.B.M.; Zahran, E.-S.M.M.; Shams, S. Forest Fire Risk Assessment Using Hotspot Analysis in GIS. Open Civ. Eng. J. 2017, 11, 786–801. [Google Scholar] [CrossRef]
- Vizuete-Jaramillo, E.; Meza-Figueroa, D.; Reyes-Castro, P.A.; Robles-Morua, A. Using a Sensitivity Analysis and Spatial Clustering to Determine Vulnerability to Potentially Toxic Elements in a Semiarid City in Northwest Mexico. Susainability 2022, 14, 10461. [Google Scholar] [CrossRef]
- Kričković, E.; Novković, I.; Lukić, T.; Kričković, Z. Using DPSEEA Framework to Investigate the Relation between Arsenic Concentration Values in Waters and Cancer Rates in AP Vojvodina (North Serbia). Pol. J. Environ. Stud. 2022, 31, 2117–2129. [Google Scholar] [CrossRef]
- Olsen, F. Cluster analysis and disease mapping—Why, when, and how? A step by step guide. BMJ 1996, 313, 863–866. [Google Scholar] [CrossRef] [Green Version]
- ESRI. How Hot Spot Analysis (Getis-Ord Gi*) Works. Available online: https://pro.arcgis.com/en/pro-app/latest/tool-reference/spatial-statistics/h-how-hot-spot-analysis-getis-ord-gi-spatial-stati.htm (accessed on 12 October 2022).
- Statistical Office of the Republic of Serbia. Demographic Yearbook 2018; Statistical Office of the Republic of Serbia: Belgrade, Serbia, 2019; pp. 1–415. (In Serbian)
- Statistical Office of the Republic of Serbia. Online Database in 2021. Available online: https://data.stat.gov.rs/?caller=SDDB&languageCode=en-US (accessed on 12 October 2022).
- EUROSTAT. Available online: https://ec.europa.eu/eurostat/web/quality/european-quality-standards/european-statisticscode-of-practice (accessed on 12 October 2022).
- Obradović-Arsić, D. Medical-Geographical Factors in Planning and Protection of Space; Faculty of Geography: Belgrade, Serbia, 2014; pp. 1–331. (In Serbian) [Google Scholar]
- Vorgučin, I.; Vlaški, J.; Naumović, N.; Katanić, D. Comparison of two defined criteria for diagnosing metabolic syndrome in overnourished and obese children in Vojvodina, Vojnosanitetski pregled. Mil. Med. Pharm. J. Serb. 2011, 68, 500–505. [Google Scholar] [CrossRef]
- Radić, I. Obesity and Physical Inactivity as Public Health Problems of the Adult Population of Vojvodina. Ph.D. Thesis, Faculty of Medicine, University in Novi Sad, Novi Sad, Serbia, 28 October 2016. (In Serbian). [Google Scholar]
- Milić, N.; Stanisavljević, D.; Krstić, M.; Jovanović, B.; Brcanski, J.; Kilibarda, B.; Ljubičić, M.; Živković-Šulović, M.; Boričić, K.; Živanović-Radnić, K.; et al. Research on the Health of the Population of Serbia in 2019; Milić, N., Stanisavljević, D., Krstić, M., Eds.; Institute of Public Health of Serbia “Dr Milan Jovanović Batut” and Statistical Office of the Republic of Serbia: Belgrade, Serbia, 2021; pp. 1–144. (In Serbian) [Google Scholar]
- Hadživuković, N.; Kulić, V.; Živanović, V.; Šuić, V.; Joković, S.; Pavlović, J. Health care and family support for lung cancer patients. Sestrin. Reč 2017, 21, 20–23. (In Serbian) [Google Scholar] [CrossRef]
- Institute of Oncology of Vojvodina. Available online: http://www.onk.ns.ac.rs/pdf/UputstvaPacijenti/Informator_za_pacijente-CaBUBREGA.pdf (accessed on 12 October 2022).











| Type of Disease | Number of New Patients | Number of the Deceased | ||||
|---|---|---|---|---|---|---|
| Z | α | b | Z | A | b | |
| Acute coronary syndrome | −2.02 | * | −0.0112 | −3.89 | *** | −0.643 |
| Myocardial infarction | −1.87 | + | −0.816 | −3.74 | *** | −0.690 |
| Unstable angina pectoris | −1.87 | + | −0.230 | −0.63 | / | −1.000 |
| Type 1 diabetes | −2.23 | * | −1.833 | −0.72 | / | −0.110 |
| Type 2 diabetes | 2.42 | * | 0.773 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kričković, E.; Lukić, T.; Jovanović-Popović, D. Geographic Medical Overview of Noncommunicable Diseases (Cardiovascular Diseases and Diabetes) in the Territory of the AP Vojvodina (Northern Serbia). Healthcare 2023, 11, 48. https://doi.org/10.3390/healthcare11010048
Kričković E, Lukić T, Jovanović-Popović D. Geographic Medical Overview of Noncommunicable Diseases (Cardiovascular Diseases and Diabetes) in the Territory of the AP Vojvodina (Northern Serbia). Healthcare. 2023; 11(1):48. https://doi.org/10.3390/healthcare11010048
Chicago/Turabian StyleKričković, Emina, Tin Lukić, and Dejana Jovanović-Popović. 2023. "Geographic Medical Overview of Noncommunicable Diseases (Cardiovascular Diseases and Diabetes) in the Territory of the AP Vojvodina (Northern Serbia)" Healthcare 11, no. 1: 48. https://doi.org/10.3390/healthcare11010048





