Prevention of Musculoskeletal Injuries in Gastrointestinal Endoscopists
Abstract
1. Introduction
2. Materials and Methods
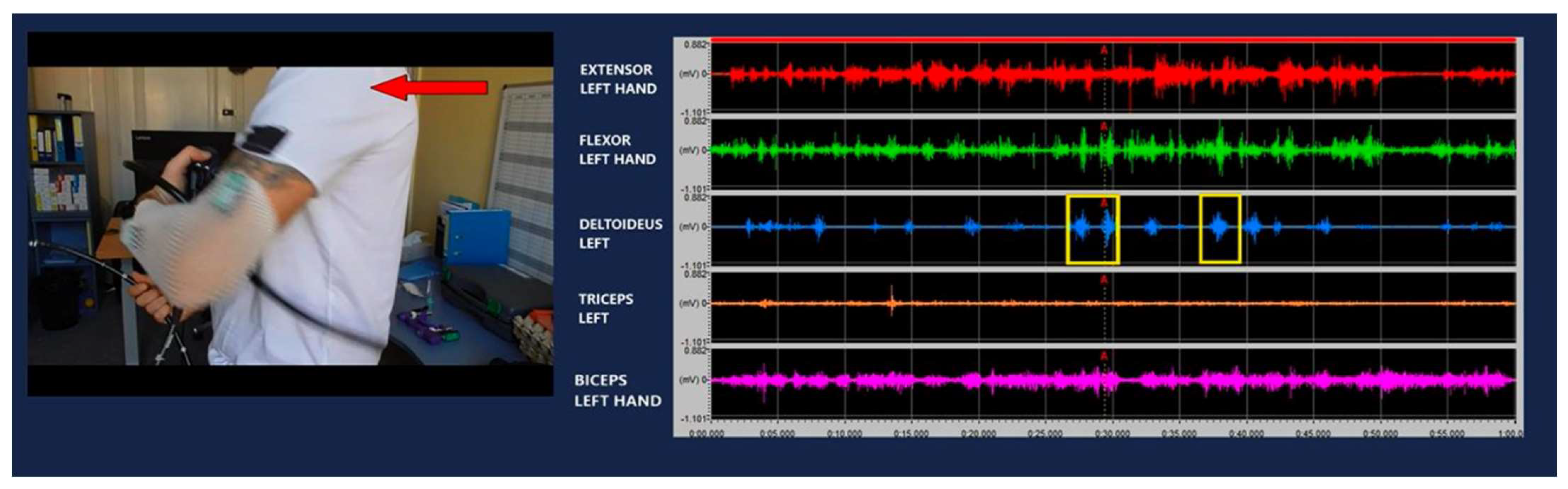
2.1. EMG Measurements of Basic Endoscopic Movements
2.2. Development of Standardized Procedure
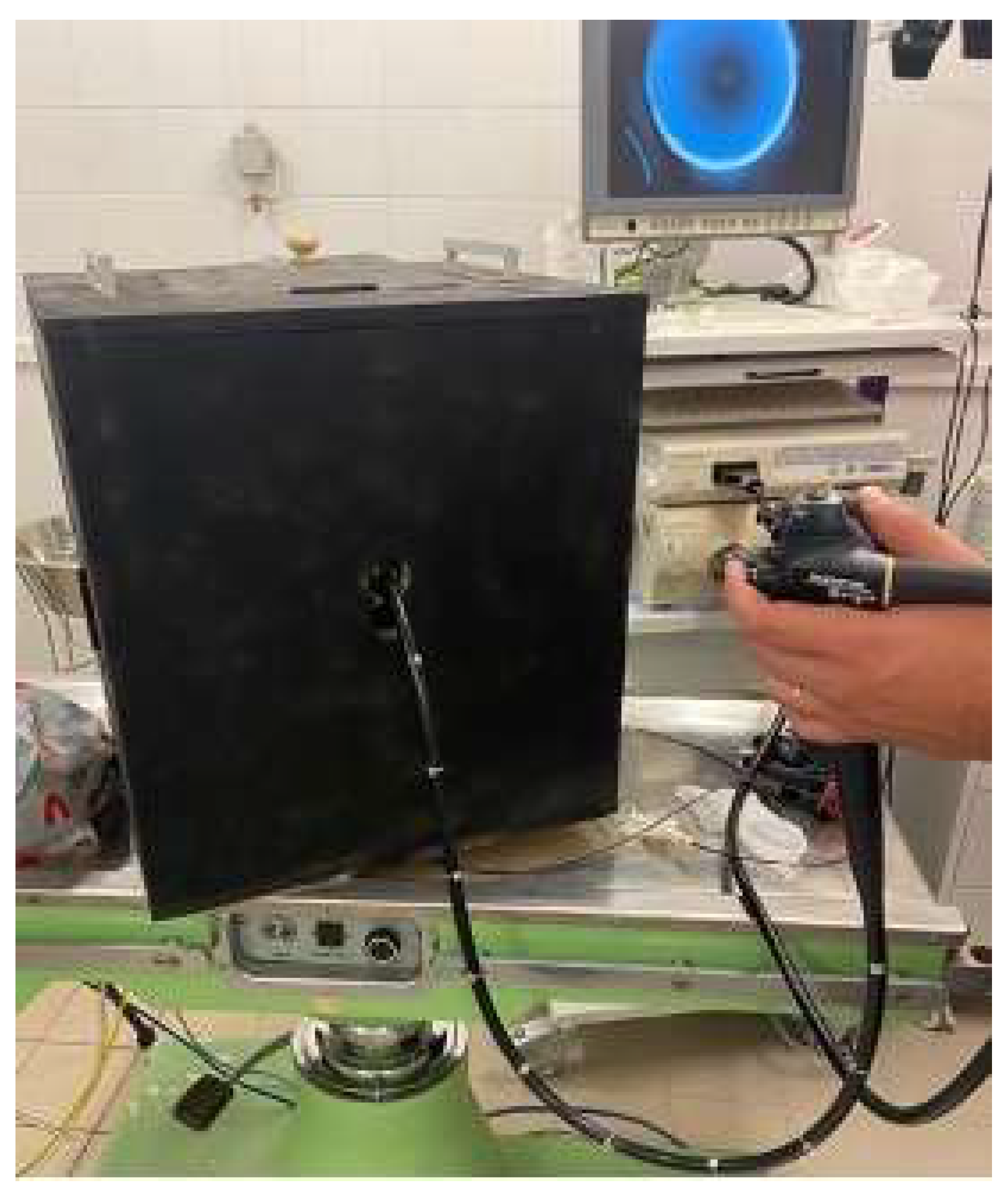
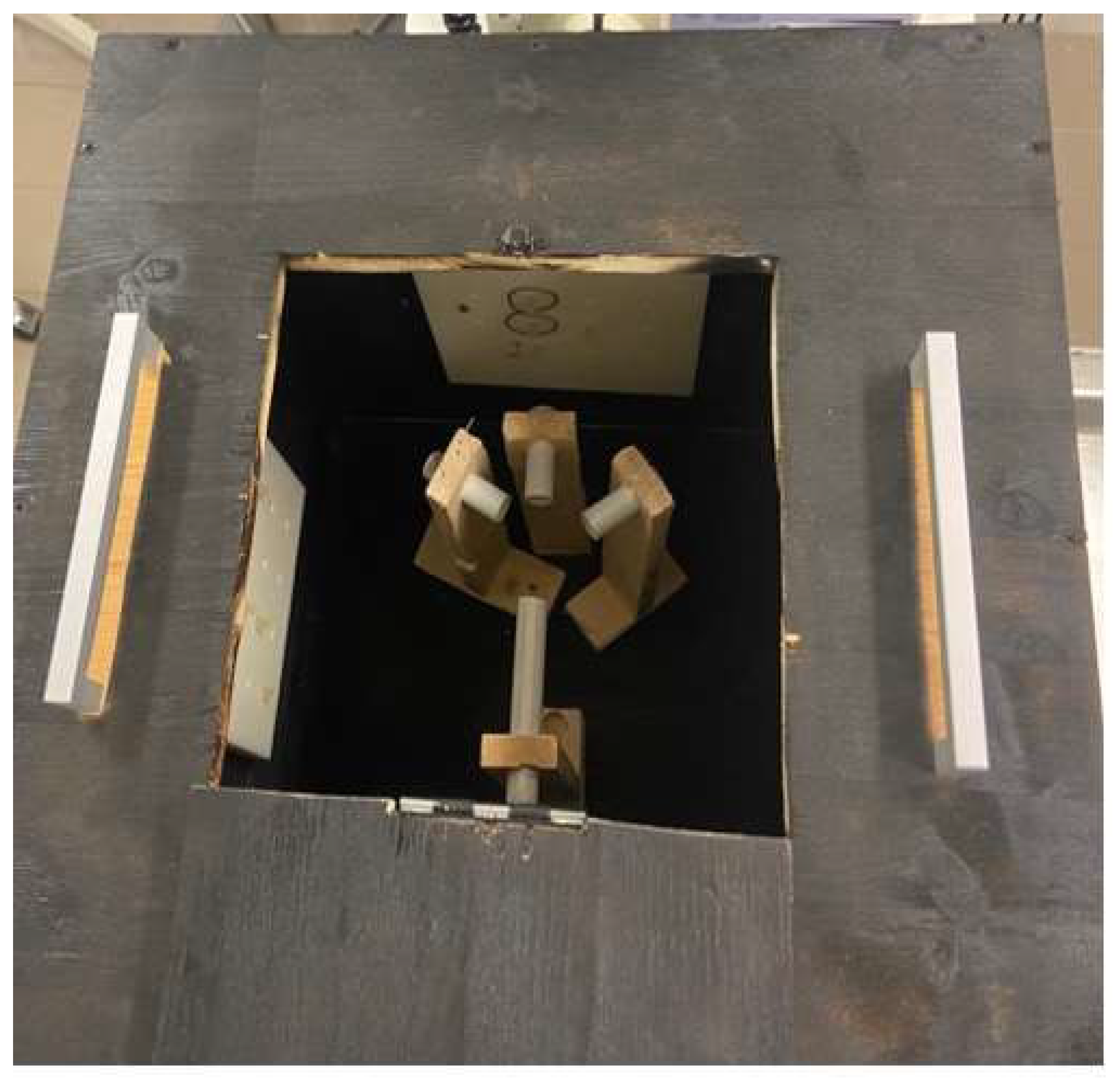
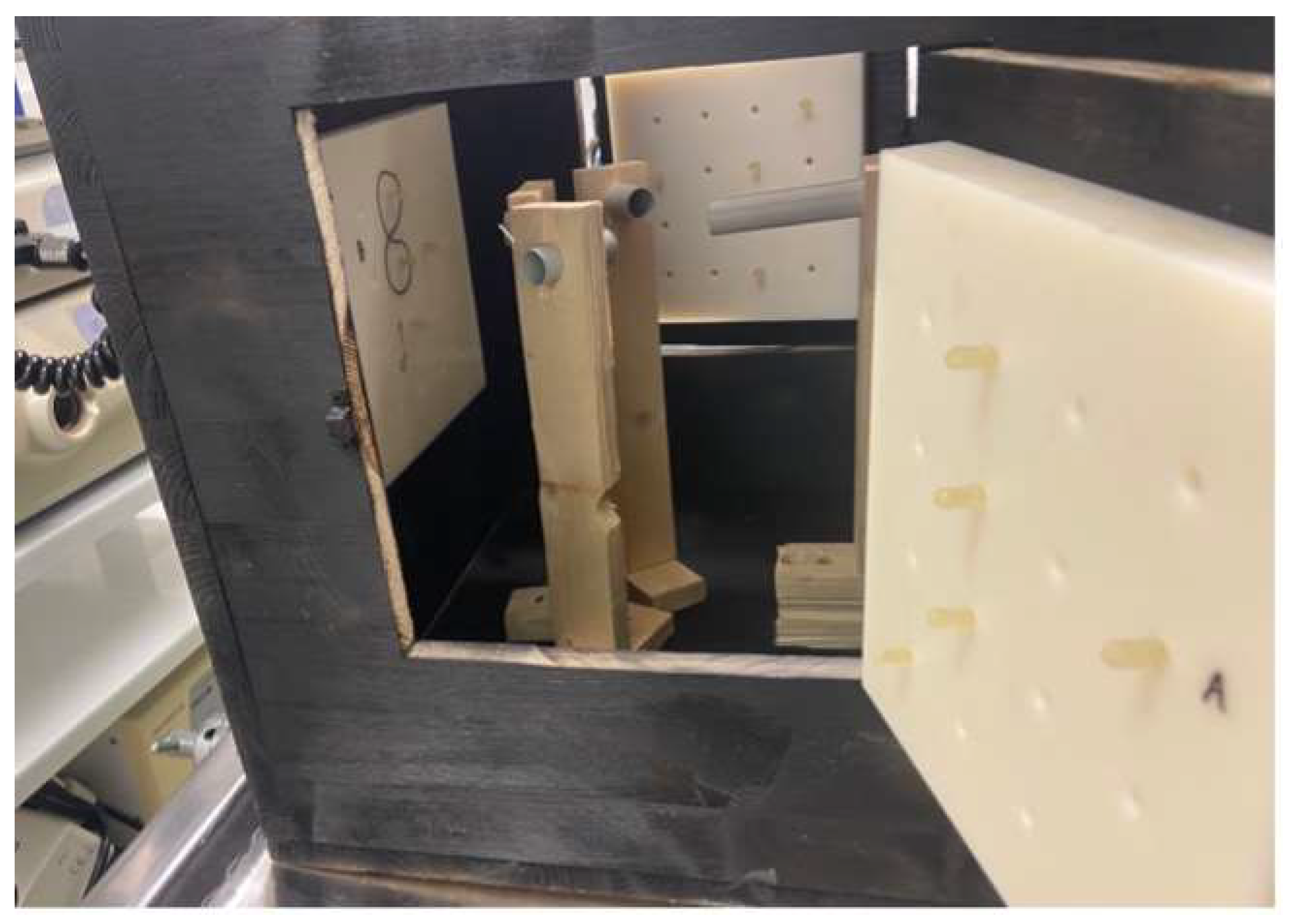
2.2.1. Training Box Development and Manufacturing
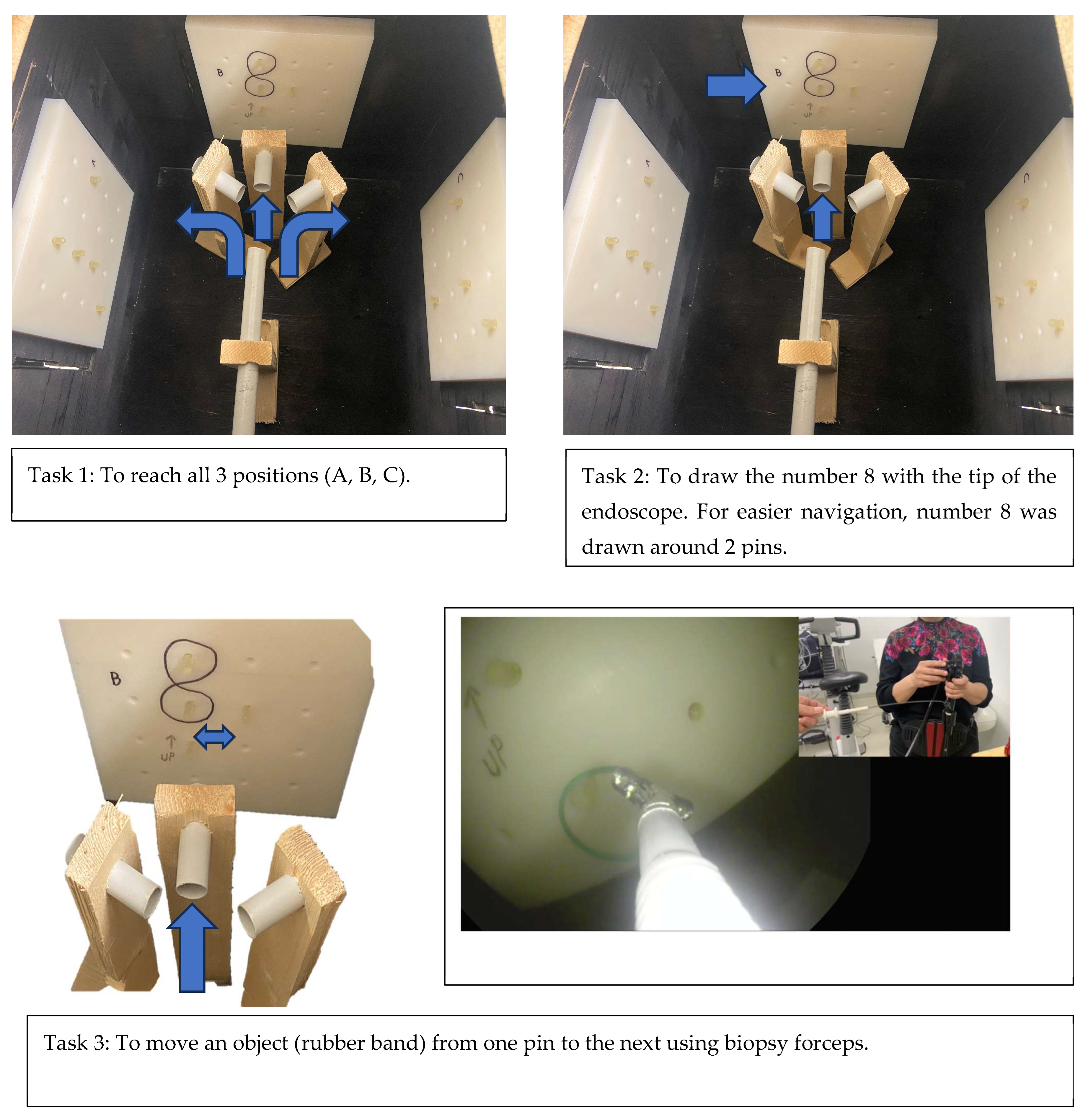
2.2.2. Task Design
2.3. Muscle Tension and Microbreak Measurements
2.4. Muscle Tension and Microbreak Measurements with Support System
2.5. Participants
2.6. Statistics
- If p > 0.05, it suggests that there is not enough evidence to conclude a significant difference between the two groups (FAIL).
- If p < 0.05, it indicates that the difference between the two groups is statistically significant (PASS).
3. Results
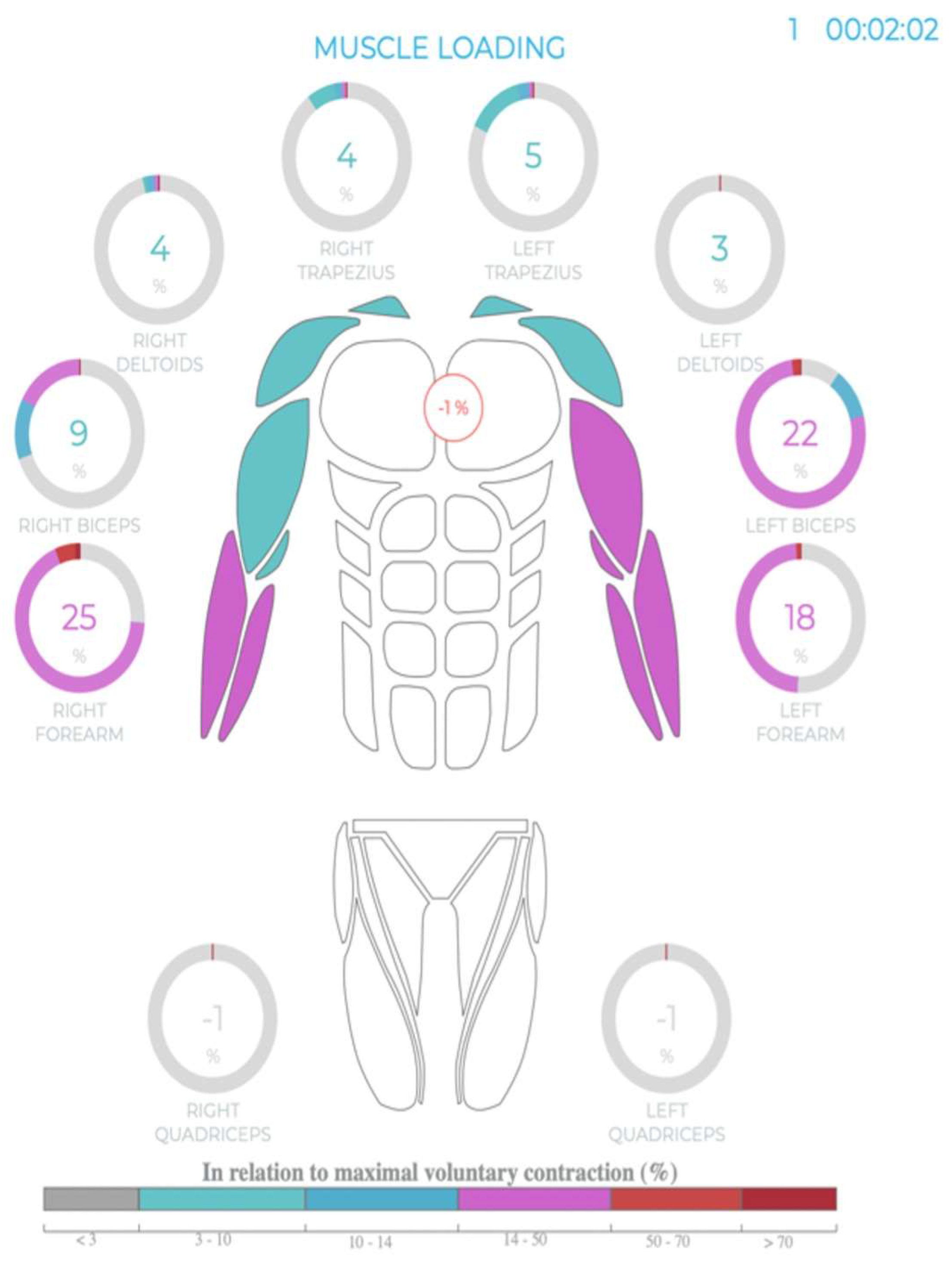
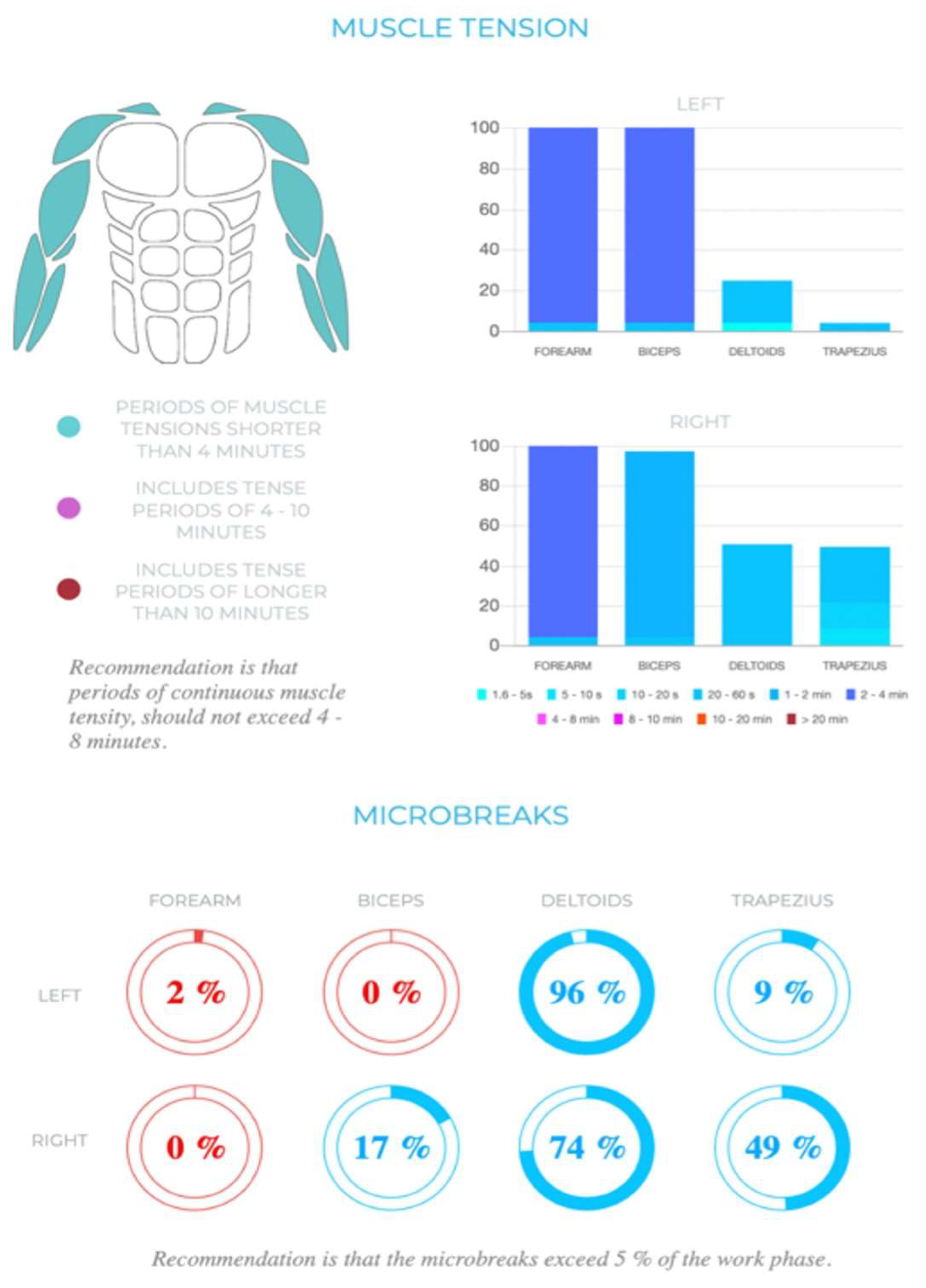
3.1. EMG Potentials during Endoscopy
3.2. Differences between Endoscopists and Non-Endoscopists
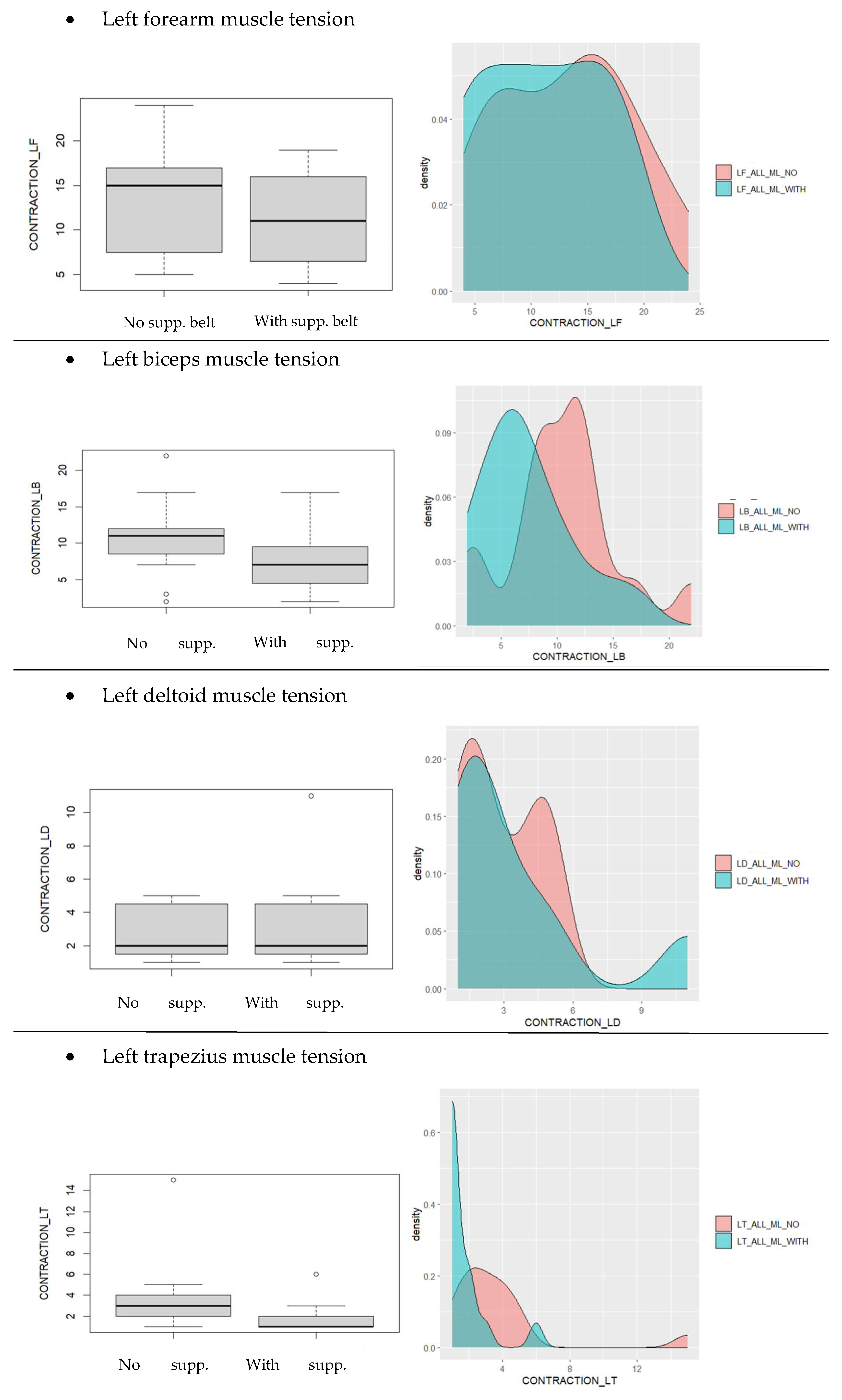
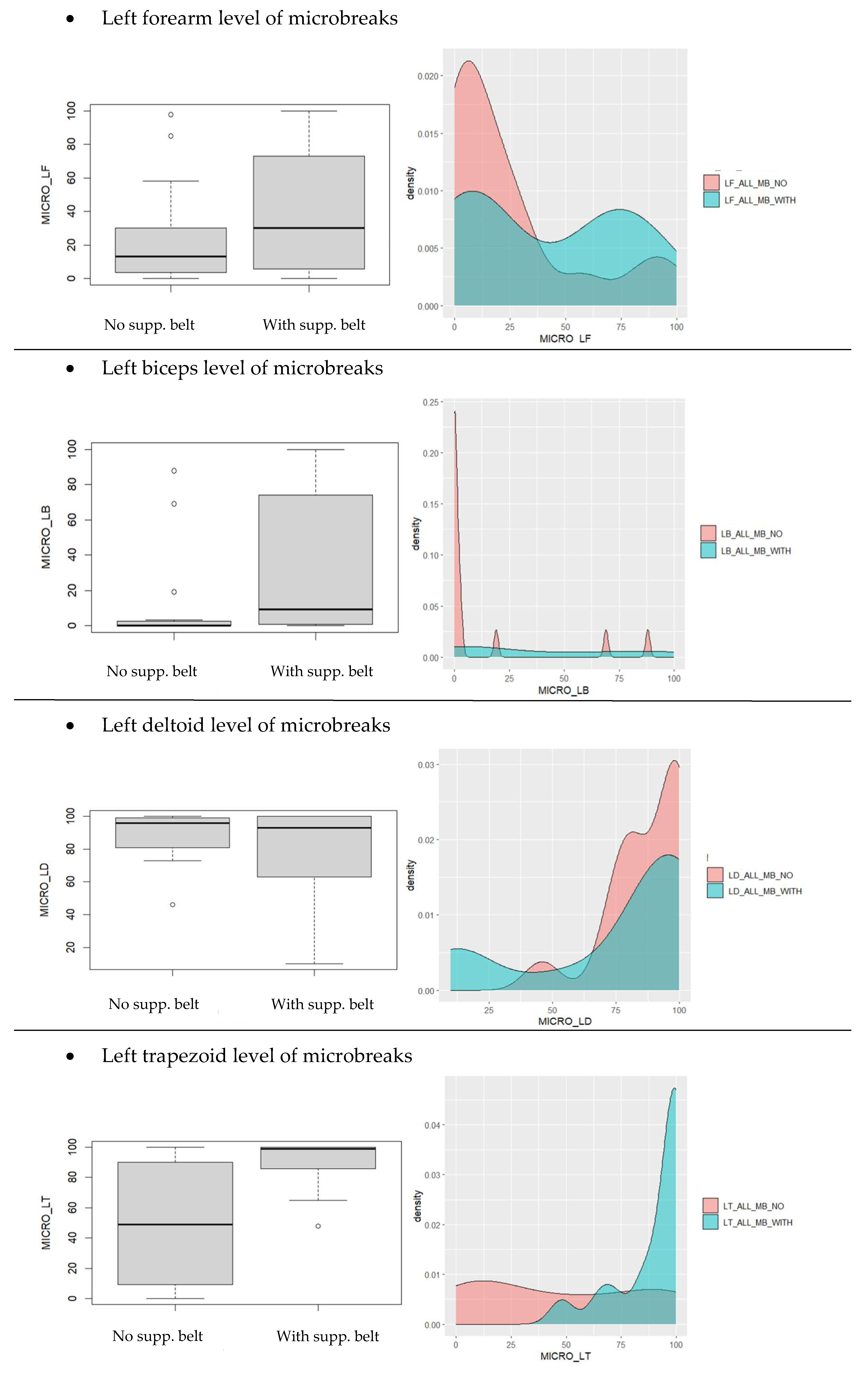
3.3. Differences between Groups When Using the Belt-like Support System
3.4. Statistical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shergill, A.K.; Adamson, C.H. Failure of an engineered system: The gastrointestinal endoscope. Tech. Gastrointest. Endosc. 2019, 21, 116–123. [Google Scholar] [CrossRef]
- Yung, D.E.; Banfi, T.; Ciuti, G.; Arezzo, A.; Dario, P.; Koulaouzidis, A. Musculoskeletal injuries in gastrointestinal endoscopists: A systematic review. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 939–947. [Google Scholar] [CrossRef] [PubMed]
- Villa, E.; Attar, B.; Trick, W.; Kotwal, V. Endoscopy-related musculoskeletal injuries in gastroenterology fellows. Endosc. Int. Open 2019, 7, E808–E812. [Google Scholar] [CrossRef] [PubMed]
- Shergill, A.K.; McQuaid, K.R.; Rempel, D. Ergonomics and GI endoscopy. Gastrointest. Endosc. 2009, 70, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Siau, K.; Anderson, J.T. Ergonomics in endoscopy: Should the endoscopist be considered and trained like an athlete? Endosc. Int. Open. 2019, 7, E813–E815. [Google Scholar] [CrossRef] [PubMed]
- Walsh, C.M.; Qayed, E.; Aihara, H.; Anand, G.S.; Byrne, K.; Chahal, P.; Dacha, S.; James, T.W.; Kowalski, T.E.; Repaka, A.; et al. Core curriculum for ergonomics in endoscopy. Gastrointest. Endosc. 2021, 93, 1222–1227. [Google Scholar] [CrossRef] [PubMed]
- Shergill, A.K.; McQuaid, K.R. Ergonomic endoscopy: An oxymoron or realistic goal? Gastrointest. Endosc. 2019, 90, 966–970. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.A.; Mitchell, J.; Fehmi, S.M.A. Optimizing ergonomics during endoscopy. VideoGIE 2017, 2, 170. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.T. Optimizing ergonomics during endoscopy training. Tech. Gastrointest. Endosc. 2019, 21, 143–149. [Google Scholar] [CrossRef]
- Singla, M.; Kwok, R.M.; Deriban, G.; Young, P.E. Training the Endo-Athlete: An Update in Ergonomics in Endoscopy. Clin. Gastroenterol. Hepatol. 2018, 16, 1003–1006. [Google Scholar] [CrossRef] [PubMed]
- Peper, E.; Gibney, K.H. Physiological Rationale for Microbreaks. In Biofeedback; Spring: Berlin/Heidelberg, Germany, 2005; pp. 38–39. [Google Scholar]
- Chaillou, T.; Koulmann, N.; Simler, N.; Meunier, A.; Serrurier, B.; Chapot, R.; Peinnequin, A.; Beaudry, M.; Bigard, X. Hypoxia transiently affects skeletal muscle hypertrophy in a functional overload model. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2012, 302, R643–R654. [Google Scholar] [CrossRef] [PubMed]
- McLean, L.; Tingley, M.; Scott, R.N.; Rickards, J. Computer terminal work and the benefit of microbreaks. Appl. Ergon. 2001, 32, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Jirapinyo, P.; Kumar, N.; Thompson, C.C. Validation of an endoscopic part-task training box as a skill assessment tool. Gastrointest. Endosc. 2015, 81, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Moser, T.; Lecours, J.; Michaud, J.; Bureau, N.J.; Guillin, R.; Cardinal, É. The deltoid, a forgotten muscle of the shoulder. Skelet. Radiol. 2013, 42, 1361–1375. [Google Scholar] [CrossRef] [PubMed]





| Endoscopists | |
| Mean muscle tension % | Freehand |
| Left forearm | 9.4 |
| Left biceps | 9.5 |
| Left deltoid | 1.7 |
| Left trapezius | 3.1 |
| Mean microbreaks % | Freehand |
| Left forearm | 31.9 |
| Left biceps | 22.7 |
| Left deltoid | 96.6 |
| Left trapezius | 32.6 |
| Non-endoscopists | |
| Mean muscle tension % | Freehand |
| Left forearm | 16.5 |
| Left biceps | 11.3 |
| Left deltoid | 3.9 |
| Left trapezius | 4.3 |
| Mean microbreaks % | Freehand |
| Left forearm | 18.6 |
| Left biceps | 3.1 |
| Left deltoid | 79.3 |
| Left trapezius | 60.1 |
| Endoscopists | |
| Mean muscle tension % | Belt holder |
| Left forearm | 8.6 |
| Left biceps | 6.4 |
| Left deltoid | 1.4 |
| Left trapezius | 1.4 |
| Mean microbreaks % | Belt holder |
| Left forearm | 48.1 |
| Left biceps | 40.4 |
| Left deltoid | 99.1 |
| Left trapezius | 94.9 |
| Non-endoscopists | |
| Mean muscle tension % | Belt holder |
| Left forearm | 13.3 |
| Left biceps | 8.3 |
| Left deltoid | 5.4 |
| Left trapezius | 2.1 |
| Mean microbreaks % | Belt holder |
| Left forearm | 34.4 |
| Left biceps | 32.5 |
| Left deltoid | 53.9 |
| Left trapezius | 85.6 |
| p-Values | |||
|---|---|---|---|
| All (with vs. without Belt) | Endoscopists (with vs. without Belt) | Non-Endoscopists (with vs. without Belt) | |
| LF m. tension | 0.012260 | 0.248100 | 0.026560 |
| LB m. tension | 0.000790 | 0.041320 | 0.011690 |
| LD m. tension | 0.278200 | 0.172300 | 0.190600 |
| LT m. tension | 0.003163 | 0.009604 | 0.076940 |
| LF microbreaks | 0.028460 | 0.106400 | 0.169400 |
| LB microbreaks | 0.006564 | 0.175600 | 0.022870 |
| LD microbreaks | 0.105500 | 0.172300 | 0.066260 |
| LT microbreaks | 0.000506 | 0.006452 | 0.020850 |
| All | Endoscopists | Non-Endoscopists | |
| LF m. tension | PASS | FAIL | PASS |
| LB m. tension | PASS | PASS | PASS |
| LD m. tension | FAIL | FAIL | FAIL |
| LT m. tension | PASS | PASS | FAIL |
| LF microbreaks | PASS | FAIL | FAIL |
| LB microbreaks | PASS | FAIL | PASS |
| LD microbreaks | FAIL | FAIL | FAIL |
| LT microbreaks | PASS | PASS | PASS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durič, T.; Cibulkova, I.; Hajer, J. Prevention of Musculoskeletal Injuries in Gastrointestinal Endoscopists. Gastroenterol. Insights 2024, 15, 285-302. https://doi.org/10.3390/gastroent15020021
Durič T, Cibulkova I, Hajer J. Prevention of Musculoskeletal Injuries in Gastrointestinal Endoscopists. Gastroenterology Insights. 2024; 15(2):285-302. https://doi.org/10.3390/gastroent15020021
Chicago/Turabian StyleDurič, Tadej, Ivana Cibulkova, and Jan Hajer. 2024. "Prevention of Musculoskeletal Injuries in Gastrointestinal Endoscopists" Gastroenterology Insights 15, no. 2: 285-302. https://doi.org/10.3390/gastroent15020021
APA StyleDurič, T., Cibulkova, I., & Hajer, J. (2024). Prevention of Musculoskeletal Injuries in Gastrointestinal Endoscopists. Gastroenterology Insights, 15(2), 285-302. https://doi.org/10.3390/gastroent15020021






