Reducing the Risk of Healthcare Associated Infections from Legionella and Other Waterborne Pathogens Using a Water Management for Construction (WMC) Infection Control Risk Assessment (ICRA) Tool
Abstract
:1. Introduction
2. Background/Literature Review
3. Materials and Methods
3.1. Developing WMC-ICRA Project Types
3.1.1. Adjusting for Water Age/Dormancy
3.1.2. Defining Construction Scope of Work for Water System Components
3.2. Developing WMC-ICRA Class of Precautions
3.2.1. Monitoring Residual Oxidant (Free or Total)
3.2.2. Monitoring Temperature
3.2.3. Implementing Flushing Protocols
3.2.4. Utilizing Filtration
3.2.5. Installing Physical Barriers
3.2.6. Recirculation and Hot Water Storage
3.2.7. Equipment Installation, Cleaning, and Maintenance
3.2.8. Disinfection
3.3. Determining WMC-ICRA Sampling Plans for Verification and Validation Testing
4. Results
4.1. WMC-ICRA Project Categories
4.1.1. Construction Scope of Work
4.1.2. Stratified Water Age Categories
4.2. WMC-ICRA Building Occupant Risk Groups
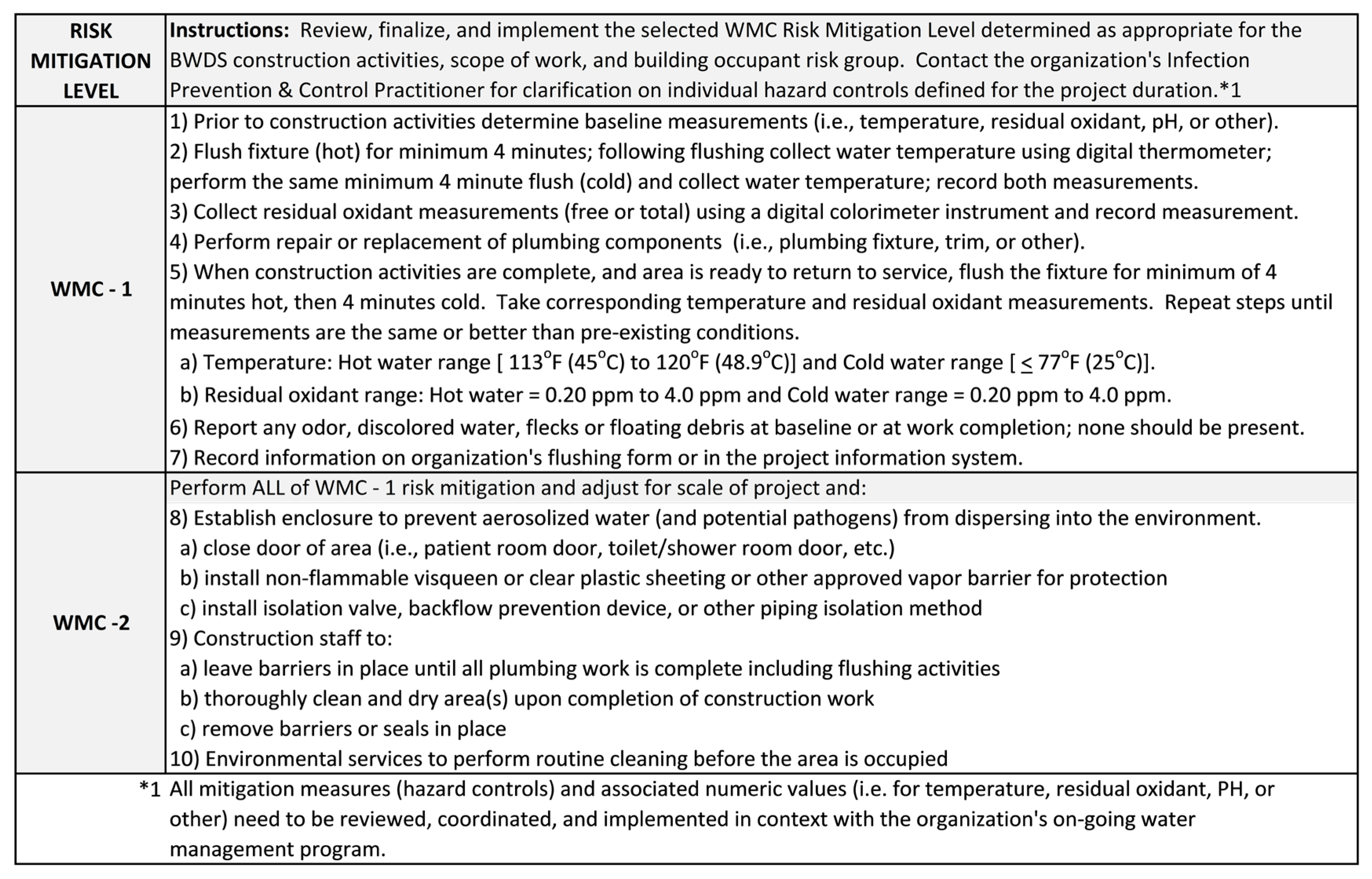
4.3. WMC Risk Mitigation Levels
4.4. WMC-ICRA Verification and Validation Testing
5. Discussion
5.1. Health and Built Environment Perspective
5.2. Infection Prevention and Control Perspective
5.2.1. Increased Planning and Consistent Implementation
5.2.2. Extending Patient Safety to Other WMP Team Members
5.2.3. Increasing IPC Practitioner Core Competencies
5.3. Industrial Hygiene Perspective
5.4. Limitations
6. Conclusions
- Reduce the likelihood of a disease case, injury, or death from a healthcare associated infection emerging from exposure to the BWDS during and after construction activities;
- Reduce the likelihood of waterborne pathogen growth and spread in a BWDS undergoing any form or range of project involving construction activities;
- Improve regulatory alignment with healthcare standards and policies requiring risk mitigation for waterborne pathogen growth and spread during construction activities;
- Expand use of existing ICRA framework commonly used for airborne pathogens to align with waterborne pathogens for ease of healthcare industry implementation;
- Extend collaboration of water management programs and teams to allied industries from planning, design, and construction to include water safety as a common protection for building occupants as part of licensed professionals’ duty and standard of care to protect the health, safety, and welfare of the public related to any renovated or newly constructed BWDS and its components.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Scanlon, M.M.; Gordon, J.L.; McCoy, W.F.; Cain, M.F. Water management for construction: Evidence for risk characterization in community and healthcare settings: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 2168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrison, L.E.; Kunz, J.M.; Cooley, L.A.; Moore, M.R.; Lucas, C.; Schrag, S.; Sarisky, J.; Whitney, C.G. Vital Signs: Deficiencies in Environmental Control Identified in Outbreaks of Legionnaires’ Disease—North America, 2000–2014. Am. J. Transplant. 2016, 16, 3049–3058. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Water Safety in Buildings; Cunliffe, D., Bartram, J., Briand, E., Chartier, Y., Colbourne, J., Drury, D., Lee, J., Schaefer, B., Surman-Lee, S., Eds.; World Health Organization: Geneva, Switzerland; w/Ringgold Inc.: Portland, OR, USA, 2011. [Google Scholar]
- McFarlane, M. Infection Control Risk Assessments: Prevention Across the Construction Continuum. Prof. Saf. 2014, 59, 83. [Google Scholar]
- Facility Guideline Institute. Guidelines for the Design and Construction of Hospitals; FGI with American Society of Healthcare Engineering: Dallas, TX, USA, 2018; pp. 1–337. [Google Scholar]
- Collins, W.; Holley, P.; Chavan, A.; Sattineni, A. General Contractor Knowledge of Infection Control Requirements on Hospital Renovation Construction Projects. In Proceedings of the 11th International Conference on Construction in the 21st Century for the Collaboration and Integration in Construction, Engineering, Management and Technology, London, UK, 9–11 September 2019; pp. 63–67. [Google Scholar]
- Bartley, J.M. APIC State-of-the-Art Report: The role of infection control during construction in health care facilities. Am. J. Infect. Control 2000, 28, 156–169. [Google Scholar] [CrossRef]
- APIC. Infection Prevention Manual for Construction & Renovation, 1st ed.; Vogel, R., Ed.; Association for Professionals in Infection Control and Epidemiology: Arlington, VA, USA, 2015; p. 164. [Google Scholar]
- Bartley, J.M.; Olmsted, R.N.; Haas, J. Current views of health care design and construction: Practical implications for safer, cleaner environments. AJIC Am. J. Infect. Control 2010, 38, S1–S12. [Google Scholar] [CrossRef]
- Talento, A.F.; Fitzgerald, M.; Redington, B.; O’Sullivan, N.; Fenelon, L.; Rogers, T.R. Prevention of healthcare-associated invasive aspergillosis during hospital construction/renovation works. J. Hosp. Infect. 2019, 103, 1–12. [Google Scholar] [CrossRef]
- Gamage, S.D.; Ambrose, M.; Kralovic, S.M.; Roselle, G.A. Water Safety and Health Care: Preventing Infections Caused by Opportunistic Premise Plumbing Pathogens. Infect. Dis. Clin. N. Am. 2021, 35, 667–695. [Google Scholar] [CrossRef]
- Sehulster, L.; Chinn, R.; Arduino, M.; Carpenter, J.; Donlan, R.; Ashford, D.; Besser, R.; Fields, B.; McNeil, M.; Whitney, C.; et al. Guidelines for Environmental Infection Control in Health-Care Facilities; U.S. Department of Health and Human Services Centers for Disease Control and Prevention (CDC): Atlanta, GA, USA, 2004; p. 240. [Google Scholar]
- ASHRAE. ASHRAE Guideline 12-2020 Managing the Risk of Legionellosis Associated with Building Water Systems; ASHRAE: Atlanta, GA, USA, 2020; pp. 1–54. [Google Scholar]
- ASHRAE. ANSI/ASHRAE Standard 188 Legionellosis: Risk Management for Building Water Systems; ASHRAE: Atlanta, GA, USA, 2021; pp. 1–24. [Google Scholar]
- Proctor, C.R.; Rhoads, W.J.; Keane, T.; Salehi, M.; Hamilton, K.; Pieper, K.J.; Cwiertny, D.M.; Prévost, M.; Whelton, A.J. Considerations for large building water quality after extended stagnation. AWWA Water Sci. 2020, 2, e1186. [Google Scholar] [CrossRef]
- American Hospital Association. AHA Hospital Statistics: A Comprehensive Reference for Analysis and Comparison of Hospital Trends; American Hospital Association: Chicago, IL, USA, 2021. [Google Scholar]
- AHCA. About American Health Care Association & National Center for Assisted Living. Available online: https://www.ahcancal.org/About/Pages/default.aspx (accessed on 12 December 2021).
- Simmons, S. ASHRAE to Continue Development of Building Water Management Standard; ASHRAE: Atlanta, GA, USA, 2019. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. Management of Legionella in Water Systems; The National Academies Press: Washington, DC, USA, 2020; p. 290. [Google Scholar]
- CMS. Requirement to Reduce Legionella Risk in Healthcare Facility Water Systems to Prevent Cases and Outbreaks of Legionnaires’ Disease. In Policy and Memos to States and Regions; Centers for Medicare & Medicaid Services: Baltimore, MD, USA, 2018; pp. 1–4. [Google Scholar]
- Olmsted, R.N. Reimagining Construction and Renovation of Health Care Facilities During Emergence from a Pandemic. Infect. Dis. Clin. N. Am. 2021, 35, 697–716. [Google Scholar] [CrossRef]
- Collander, T.; Conway, J.; Fishbeck, J.; Gacki-Smith, J.; Jorgenson, C.; Kulczycki, M.; Labson, M.; Maurer, J.; Olea, S.; Podgorny, K.; et al. Infection Prevention and Control Issues in the Environment of Care, 3rd ed.; Hible, L., Ed.; Joint Commission Resources: Oakpark Terrace, IL, USA, 2017; p. 176. [Google Scholar]
- U.S. Department of Veterans Affairs. Prevention of Health Care-Associated Legionella Disease and Scald Injury from Water Systems. In VHA Directive 1061; U.S. Department of Veterans Affairs: Washington, DC, USA, 2021; pp. 1–60. [Google Scholar]
- CDC. Developing a Water Management Program to Reduce Legionella Growth and Spread in Buildings: A Practical Guide to Implementing Industry Standards; CDC: Atlanta, GA, USA, 2021; pp. 1–36. [Google Scholar]
- CDC. Toolkit for Controlling Legionella in Common Sources of Exposure: Information on Controlling Legionella in Commonly Implicated Sources of Legionnaires’ Disease Outbreaks; CDC: Atlanta, GA, USA, 2021; pp. 1–27. [Google Scholar]
- CDC. Safe Water System: Free Chorine Testing (FRO). Available online: https://www.cdc.gov/safewater/chlorine-residual-testing.html (accessed on 29 December 2021).
- Singh, R.; Hamilton, K.A.; Rasheduzzaman, M.; Yang, Z.; Kar, S.; Fasnacht, A.; Masters, S.V.; Gurian, P.L. Managing water quality in premise plumbing: Subject matter experts’ perspectives and a systematic review of guidance documents. Water 2020, 12, 347. [Google Scholar] [CrossRef] [Green Version]
- Krageschmidt, D.A.; Kubly, A.F.; Browning, M.S.; Wright, A.J.; Lonneman, J.D.; Detmer, M.J.; McCoy, W.F. A Comprehensive Water Management Program for Multicampus Healthcare Facilities. Infect. Control Hosp. Epidemiol. 2014, 35, 556–563. [Google Scholar] [CrossRef] [PubMed]
- Knox, N.C.; Weedmark, K.A.; Conly, J.; Ensminger, A.W.; Hosein, F.S.; Drews, S.J. Unusual Legionnaires’ outbreak in cool, dry Western Canada: An investigation using genomic epidemiology. Epidemiol. Infect. 2017, 145, 254–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miragliotta, G.; Del Prete, R.; Sabato, R.; Cassano, A.; Carnimeo, N. Legionellosis Associated with Artesian Well Excavation. Eur. J. Epidemiol. 1992, 8, 748–749. [Google Scholar] [CrossRef] [PubMed]
- Coscollá, M.; Fenollar, J.; Escribano, I.; González-Candelas, F. Legionellosis outbreak associated with asphalt paving machine, Spain, 2009. Emerg. Infect. Dis. 2010, 16, 1381. [Google Scholar] [CrossRef] [Green Version]
- Yiek, W.-K.; Coenen, O.; Nillesen, M.; Ingen, J.V.; Bowles, E.C.; Tostmann, A. Outbreaks of healthcare-associated infections linked to water-containing hospital equipment: A literature review. Antimicrob. Resist. Infect. Control 2021, 10, 77–96. [Google Scholar] [CrossRef]
- Gamage, S.D.; Ambrose, M.; Kralovic, S.M.; Roselle, G.A. Water Safety and Legionella in Health Care. Infect. Dis. Clin. N. Am. 2016, 30, 689–712. [Google Scholar] [CrossRef]
- Kanamori, H.; Weber, D.J.; Rutala, W.A. Healthcare outbreaks associated with a water reservoir and infection prevention strategies. Clin. Infect. Dis. 2016, 62, 1423–1435. [Google Scholar] [CrossRef]
- Lautenschlager, K.; Boon, N.; Wang, Y.; Egli, T.; Hammes, F. Overnight stagnation of drinking water in household taps induces microbial growth and changes in community composition. Water Res. 2010, 44, 4868–4877. [Google Scholar] [CrossRef]
- ESGLI. European Technical Guidelines for the Prevention, Control and Investigation of Infections Caused by Legionella Species; European Society of Clinical Microbiology and Infectious Diseases: Stockholm, Sweden, 2017; p. 126. [Google Scholar]
- CDC. Healthcare Environmental Infection Prevention: Reducing Risk from Water from Plumbing to Patients. Available online: https://www.cdc.gov/hai/prevent/environment/water.html (accessed on 15 November 2021).
- Rhoads, W.J.; Pruden, A.; Edwards, M.A. Interactive Effects of Corrosion, Copper, and Chloramines on Legionella and Mycobacteria in Hot Water Plumbing. Environ. Sci. Technol. 2017, 51, 7065–7075. [Google Scholar] [CrossRef]
- McCoy, W.F.; Rosenblatt, A.A.; LeChevallier, M.W. HACCP-Based Programs for Preventing Disease and Injury from Premise Plumbing: A Building Consensus. Pathogens 2015, 4, 513–528. [Google Scholar] [CrossRef]
- Mousavi, E.; Sharma, V.; Gajjar, D.; Shoai Naini, S. Renovation in hospitals: A case study on the use of control cubes for local repairs in health-care facilities. J. Facil. Manag. 2020, 18, 247–257. [Google Scholar] [CrossRef]
- Decker, B.K.; Palmore, T.N. The role of water in healthcare-associated infections. Curr. Opin. Infect. Dis. 2013, 26, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.W.; Stout, J.E.; Anderson, D.J.; Sexton, D.J.; Smith, B.; Moehring, R.W.; Huslage, K.; Hostler, C.J.; Lewis, S.S. Tap Water Avoidance Decreases Rates of Hospital-onset Pulmonary Nontuberculous Mycobacteria. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2021, 73, 524–527. [Google Scholar] [CrossRef] [PubMed]
- The Joint Commission. Prepublication Requirements—New Water Management Requirements. Available online: https://www.jointcommission.org/standards/prepublication-standards/new-water-management-requirements/ (accessed on 27 December 2021).
- Nisar, M.A.; Ross, K.E.; Brown, M.H.; Bentham, R.; Whiley, H. Water Stagnation and Flow Obstruction Reduces the Quality of Potable Water and Increases the Risk of Legionelloses. Front. Environ. Sci. 2020, 8, 611611. [Google Scholar] [CrossRef]
- Morris, D.E.; Cleary, D.W.; Clarke, S.C. Secondary Bacterial Infections Associated with Influenza Pandemics. Front. Microbiol. 2017, 8, 1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chalker, V.; Adler, H.; Ball, R.; Naik, F.; Day, J.; Afshar, B.; Amin, A. Fatal Co-infections with SARS-CoV-2 and Legionella pneumophila, England. Emerg. Infect. Dis. J. 2021, 27, 2950. [Google Scholar] [CrossRef]
- Allam, C.; Gaymard, A.; Descours, G.; Ginevra, C.; Josset, L.; Bouscambert, M.; Beraud, L.; Ibranosyan, M.; Golfier, C.; Friggeri, A.; et al. Co-infection with Legionella and SARS-CoV-2, France, March 2020. Emerg. Infect. Dis. J. 2021, 27, 2864. [Google Scholar] [CrossRef]
- Gupta, R.K.; George, R.; Nguyen-Van-Tam, J.S. Bacterial Pneumonia and Pandemic Influenza Planning. Emerg. Infect. Dis. J. 2008, 14, 1187. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Healthcare Facility Design Safety Risk Assessment Toolkit. Available online: https://www.ahrq.gov/patient-safety/settings/hospital/resource/safety-assess.html (accessed on 8 November 2021).
- Billings, C.; Bernard, H.; Caffery, L.; Dolan, S.A.; Donaldson, J.; Kalp, E.; Mueller, A. Advancing the profession: An updated future-oriented competency model for professional development in infection prevention and control Comment. Am. J. Infect. Control 2019, 47, 602–614. [Google Scholar] [CrossRef]
- Taylor, E. Designing for Safety. In 2014 FGI Guidelines Update Series; Facility Guidelines Institute: St Louis, MO, USA, 2013; pp. 1–7. [Google Scholar]
- U.S. Department of Labor Occupational Safety and Health Administration. Legionellosis (Legionnaires’ Disease and Pontiac Fever). Available online: https://www.osha.gov/legionnaires-disease/background (accessed on 15 December 2021).
- U.S. Department of Labor Occupational Safety and Health Administration. OSH Act of 1970: General Duty Clause. Available online: https://www.osha.gov/laws-regs/oshact/section5-duties (accessed on 27 December 2021).
- Kerbel, W.; Krause, D.; Shleton, B.; Springston, J. Recognition, Evaluation, and Control of Legionella in Building Water Systems; American Industrial Hygiene Association: Falls Church, VA, USA, 2015. [Google Scholar]
- Principe, L.; Tomao, P.; Visca, P. Legionellosis in the occupational setting. Environ. Res. 2017, 152, 485–495. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scanlon, M.M.; Gordon, J.L.; Tonozzi, A.A.; Griffin, S.C. Reducing the Risk of Healthcare Associated Infections from Legionella and Other Waterborne Pathogens Using a Water Management for Construction (WMC) Infection Control Risk Assessment (ICRA) Tool. Infect. Dis. Rep. 2022, 14, 341-359. https://doi.org/10.3390/idr14030039
Scanlon MM, Gordon JL, Tonozzi AA, Griffin SC. Reducing the Risk of Healthcare Associated Infections from Legionella and Other Waterborne Pathogens Using a Water Management for Construction (WMC) Infection Control Risk Assessment (ICRA) Tool. Infectious Disease Reports. 2022; 14(3):341-359. https://doi.org/10.3390/idr14030039
Chicago/Turabian StyleScanlon, Molly M., James L. Gordon, Angela A. Tonozzi, and Stephanie C. Griffin. 2022. "Reducing the Risk of Healthcare Associated Infections from Legionella and Other Waterborne Pathogens Using a Water Management for Construction (WMC) Infection Control Risk Assessment (ICRA) Tool" Infectious Disease Reports 14, no. 3: 341-359. https://doi.org/10.3390/idr14030039









