Journal Description
Infectious Disease Reports
Infectious Disease Reports
is an international, scientific, peer-reviewed open access journal on infectious diseases published bimonthly online by MDPI (from Volume 12 Issue 3 - 2020).
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, ESCI (Web of Science), PubMed, PMC, Embase, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 33.5 days after submission; acceptance to publication is undertaken in 4.9 days (median values for papers published in this journal in the first half of 2025).
- Journal Rank: CiteScore - Q2 (Infectious Diseases)
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Benefits of Publishing: We aim to be a leading journal on infectious diseases and to be in the top 20 journals listed in the Journal Citation Report (JCR) in this specific category in the near future.
Impact Factor:
2.4 (2024);
5-Year Impact Factor:
2.2 (2024)
Latest Articles
Distribution and Factors Associated with Neisseria gonorrhoeae Cases in Kampala, Uganda, 2016–2020
Infect. Dis. Rep. 2025, 17(5), 132; https://doi.org/10.3390/idr17050132 - 17 Oct 2025
Abstract
Background: Gonorrhoea is a common sexually transmitted infection with serious health consequences if not well-treated. Resistance to common therapeutic agents and limited diagnostics further heighten its burden on sexual and reproductive health. This study determined the positivity level, spatial distribution and factors
[...] Read more.
Background: Gonorrhoea is a common sexually transmitted infection with serious health consequences if not well-treated. Resistance to common therapeutic agents and limited diagnostics further heighten its burden on sexual and reproductive health. This study determined the positivity level, spatial distribution and factors influencing test positivity for Neisseria gonorrhoeae in Kampala, Uganda. Methods: Clinical data and urethral swabs were primarily collected from men with urethritis at 10 high-volume surveillance facilities. Laboratory analysis followed conventional microbiology techniques. Statistical analysis was conducted using R 4.4.3. Results: Among 1663 participants, 923 (56%, 95% CI: 53–58%) tested positive for N. gonorrhoeae, with comparable levels in Kampala divisions. Co-positivity of HIV and N. gonorrhoeae ranged from 5–27%. At bivariable analysis, there was a lower risk of testing positive for N. gonorrhoeae among participants aged above 24 years. Individuals who never use condoms or infrequently use them were marginally at a higher risk for positivity compared to routine users. Only age was the independent predictor for positivity with N. gonorrhoeae (aPR = 0.93, 95% CI: 0.87–0.99, p-value = 0.017), with men aged above 24 years being less likely to test positive for N. gonorrhoeae. Conclusions: Spatial distribution of N. gonorrhoeae positivity in Kampala was found not to be significantly influenced by location in any of the five divisions. Public health interventions should be tailored to focus on the high-risk groups such as men aged below 25 years, incorporating targeted education and prevention programs, particularly emphasizing consistent condom use among sexually active individuals to improve sexual and reproductive health in Kampala and greater Uganda.
Full article
(This article belongs to the Section Sexually Transmitted Diseases)
►
Show Figures
Open AccessArticle
Development of a PCR Assay for the Detection of Legionella micdadei in the Environment
by
William N. Bélanger, Martine Bastien, Eve Bérubé, Martin Gagnon, Yesmine G. Sahnoun, Valérie Dancause, Karel Boissinot, Cindy Lalancette, Christian Riel-Roberge, Marieve Jacob-Wagner, Sylvie Trottier, Damien Biot-Pelletier, Annie Ruest, Isabelle Tétreault, Mathieu Thériault and Sandra Isabel
Infect. Dis. Rep. 2025, 17(5), 131; https://doi.org/10.3390/idr17050131 - 17 Oct 2025
Abstract
Background/Objectives: Legionella micdadei is a clinically significant species within the Legionella genus, requiring accurate detection methods, surveillance, and precise clinical diagnosis. Our objective was to develop a sensitive polymerase chain reaction (PCR) assay specific for L. micdadei to detect its presence in environmental
[...] Read more.
Background/Objectives: Legionella micdadei is a clinically significant species within the Legionella genus, requiring accurate detection methods, surveillance, and precise clinical diagnosis. Our objective was to develop a sensitive polymerase chain reaction (PCR) assay specific for L. micdadei to detect its presence in environmental specimens. Methods: We targeted the 23S–5S intergenic spacer region, which can differentiate Legionella spp. We tested the detection of L. micdadei with 20 strains and determined the limit of detection with 2 strains. We verified assay specificity with 17 strains of other Legionella spp., 62 strains of other bacterial and fungal genera, and three human DNA specimens. We evaluated intra- and inter-run precision. We tested 15 environmental specimens (water, swabs of water faucets, mulch, and soil) by PCR. Results: The PCR assay demonstrated 100% analytical specificity (no cross-reactivity with non-targeted species), 100% inclusivity (detection of all L. micdadei strains), and high precision, with a coefficient of variation ≤ 2% across replicates. The limit of detection was estimated at 5 genomic DNA copies per reaction. We detected L. micdadei in environmental specimens. Conclusions: This PCR assay enables accurate detection of L. micdadei and is not subject to competition with other Legionella spp., thereby addressing limitations of current broad-spectrum Legionella approaches. The evaluation supports its application in environmental detection for surveillance.
Full article
(This article belongs to the Special Issue Prevention, Diagnosis and Treatment of Infectious Diseases)
►▼
Show Figures

Figure 1
Open AccessCase Report
Quantification of Bacterial and Drug-Resistant DNA Using dPCR in a Pediatric Patient with CVC-Related Bloodstream Infection
by
Masato Kojima, Hiroki Kitagawa, Kayoko Tadera, Ryo Touge, Sho Kurihara, Mari Tanaka, Maiko Shimomura, Isamu Saeki and Hiroki Ohge
Infect. Dis. Rep. 2025, 17(5), 130; https://doi.org/10.3390/idr17050130 - 16 Oct 2025
Abstract
►▼
Show Figures
Background: Digital polymerase chain reaction (dPCR) is a highly sensitive molecular method that allows rapid detection of bacterial DNA and resistance genes, requiring only a small blood volume. Although not a new technology, its application in pediatric patients with suspected catheter-related bloodstream
[...] Read more.
Background: Digital polymerase chain reaction (dPCR) is a highly sensitive molecular method that allows rapid detection of bacterial DNA and resistance genes, requiring only a small blood volume. Although not a new technology, its application in pediatric patients with suspected catheter-related bloodstream infection (CRBSI) remains limited. Case presentation: A 16-year-old female, diagnosed with recurrent acute myelogenous leukemia, received re-induction chemotherapy through a peripherally inserted central venous catheter (PICC). The patient developed a fever, and the blood culture (BC) drawn from the PICC was positive for methicillin-resistant S. epidermidis, leading to suspicion of CRBSI. Several antibiotics were used, and the PICC was replaced. Eventually, the fever subsided, and the BC was negative after PICC removal. The levels of S. epidermidis-specific DNA sequences and mecA genes were correlated with the results of the BC and clinical course. Turnaround time was significantly shorter in dPCR (3.5 h) than in the BC (14–21 h); dPCR was performed using only 400 µL of blood. Conclusions: This case highlights the potential of dPCR as a complementary tool to conventional BCs in the management of pediatric CRBSI. dPCR may support rapid decision-making and monitoring of the treatment response, particularly when sample volumes are limited.
Full article
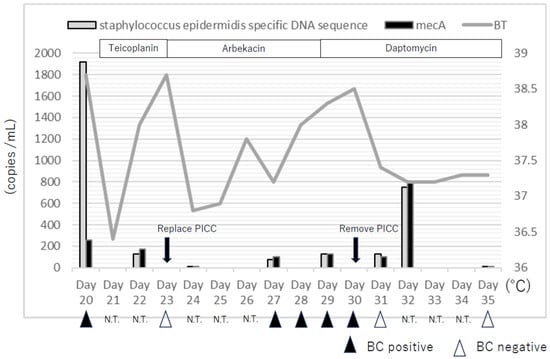
Figure 1
Open AccessArticle
Assessment of Cryptosporidium spp. Sub-Families and Giardia duodenalis Assemblages A and B in Ghanaian HIV Patients, Including Socio-Economic, Clinical, and Immunological Associations
by
Lynn Glyschewski, Hagen Frickmann, Fred Stephen Sarfo, Betty Roberta Norman, Albert Dompreh, Emmanuel Acheamfour-Akowuah, Martin Kofi Agyei, Shadrack Osei Asibey, Richard Boateng, Edmund Osei Kuffour, Veronica Di Cristanziano, Sven Poppert, Felix Weinreich, Albert Eisenbarth, Tafese Beyene Tufa, Torsten Feldt and Kirsten Alexandra Eberhardt
Infect. Dis. Rep. 2025, 17(5), 129; https://doi.org/10.3390/idr17050129 - 15 Oct 2025
Abstract
►▼
Show Figures
Background: Cryptosporidium spp. cause opportunistic infections in immunosuppressed individuals, such as people living with HIV (PLWH). However, the association between giardiasis and HIV infection remains uncertain. This study assessed co-infections in Ghanaian PLWH and HIV-negative individuals, analyzing socio-economic, clinical, and immunological implications,
[...] Read more.
Background: Cryptosporidium spp. cause opportunistic infections in immunosuppressed individuals, such as people living with HIV (PLWH). However, the association between giardiasis and HIV infection remains uncertain. This study assessed co-infections in Ghanaian PLWH and HIV-negative individuals, analyzing socio-economic, clinical, and immunological implications, including the Giardia duodenalis assemblage and Cryptosporidium spp. sub-family levels. Methods: Stool samples from Ghanaian PLWH were tested using several real-time PCR assays targeting G. duodenalis at the species level and assemblages A and B to optimize diagnostic accuracy. GD60 gene-based Sanger sequencing was used for Cryptosporidium spp. subtyping. Results were correlated with anonymized patient data to evaluate interactions with HIV infection. Results: In PLWH, C. hominis Ib, C. hominis Ie, and C. parvum IIc were detected at similar frequencies, followed by C. hominis Ia, C. hominis Id, and C. parvum IIe in decreasing order. Only C. parvum IIc was repeatedly observed in individuals with CD4+ T cell counts above 200/µL, while other sub-families occurred preferentially in those with lower counts. C. hominis Ia and Ib were associated with PLWH not receiving antiretroviral therapy; C. hominis Ia was linked to recently diagnosed HIV infections. No relevant associations between G. duodenalis assemblages and HIV infection were found. Conclusions: Sub-families Ia and Ib of C. hominis preferentially occur in individuals with severe immunosuppression, while C. parvum IIc is also detectable in individuals with better immune function. The prevalence of giardiasis in Ghana appears to be influenced by factors other than HIV-induced immunosuppression.
Full article

Figure 1
Open AccessArticle
HIV-1 Subtype Diversity in Morocco: Signals of Change and Implications for National Surveillance
by
Maryam Ahmina, Hicham El Annaz, Nada Lamrak, Ahmed Reggad, Mohamed Rida Tagajdid, Rachid Abi, Mohamed Elqatni, Abdelilah Laraqui, Safae Elkochri, Elarbi Bouaiti, Youssef Aadi, Bouchra El Mchichi, Nadia Touil, Khalid Ennibi and Idriss Lahlou Amine
Infect. Dis. Rep. 2025, 17(5), 128; https://doi.org/10.3390/idr17050128 - 14 Oct 2025
Abstract
►▼
Show Figures
Background: Limited molecular surveillance continues to constrain Morocco’s HIV response, leaving subtype dynamics largely underreported. Once characterized by a predominance of subtype B, the Moroccan epidemic now appears to reflect shifting patterns shaped by regional and international connectivity. This study aimed to investigate
[...] Read more.
Background: Limited molecular surveillance continues to constrain Morocco’s HIV response, leaving subtype dynamics largely underreported. Once characterized by a predominance of subtype B, the Moroccan epidemic now appears to reflect shifting patterns shaped by regional and international connectivity. This study aimed to investigate HIV-1 molecular diversity, monitor circulating HIV-1 genetic variants, and inter-gene recombination in a cohort of people living with HIV in Morocco. Methods: We conducted an analysis of individuals diagnosed with HIV-1 infection or receiving follow-up care. Demographic and clinical data were extracted. Genotypic testing was performed on the protease/reverse transcriptase (PR/RT) and integrase (IN) regions of the pol gene using the HIV-1 Genotyping Kit with Integrase. Subtypes were assigned via Stanford HIVdb and HIV Blast, and phylogenetic relationships were analyzed using MEGA 12. Results: Of the 73 individuals enrolled, 64 were successfully sequenced. The median age was 43 years (IQR 35–51.3), with over half aged 25–44, and 85.9% were male. Heterosexual transmission was the main route (87.5%), and 59.4% were ART-naïve. Non-B subtypes predominated (87.5%), led by CRF02_AG (73.4%), followed by B (12.5%), C (7.8%), and A3 (3.1%). The cohort showed significant genetic diversity, including multiple CRFs such as CRF45_cpx (1.6%), CRF01_AE (1.6%), B/CRF02_AG (7.8%), G/CRF02_AG (3.1%), C/CRF02_AG (1.6%), CRF02_AG/CRF45_cpx (1.6%) and CRF02_AG/CRF22_01A1 (1.6%). Conclusions: This study provides updated insight into HIV-1 diversity in Morocco, showing a predominance of non-B subtypes, particularly CRF02_AG, and signals of increasing heterogeneity compared with reports from more than a decade ago that described subtype B predominance. These findings suggest a viral transition shaped in part by regional connectivity and highlight a gap in Morocco’s HIV strategy, underscoring the need to implement nationwide molecular surveillance to inform future HIV control efforts.
Full article
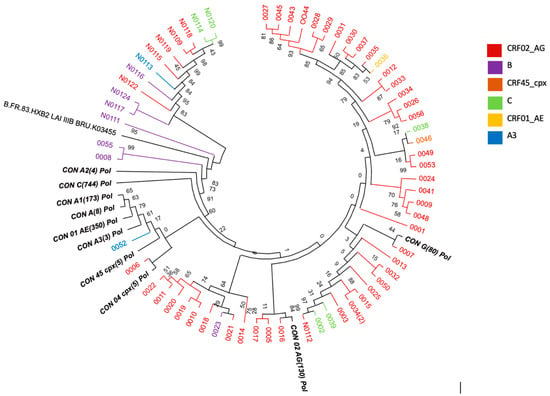
Figure 1
Open AccessArticle
The Neutrophil/Lymphocyte Ratio Was Identified as a Marker of Severe Influenza During the 2024–2025 Outbreak in France
by
Matteo Vassallo, Marion Derollez, Marc-Hadrien Veaute, Nicolas Clement, Roxane Fabre, Laurene Lotte, Yanis Kouchit, Sabrina Manni, Ursula Moracchini, Elea Blanchouin, Julie Better, Ludivine Rerolle, Raphael Chambon, Pierre Alfonsi Bertrand, Sarah Baccialone, Jerome Lemoine, Audrey Sindt and Pierre-Marie Bertrand
Infect. Dis. Rep. 2025, 17(5), 127; https://doi.org/10.3390/idr17050127 - 10 Oct 2025
Abstract
Background/Objectives: Influenza continues to cause high morbidity and mortality rates worldwide, inflicting a major burden on the public health system. There is little data available on the 2024–2025 seasonal outbreak. Moreover, biomarkers for rapidly identifying subjects at higher risk for severe forms are
[...] Read more.
Background/Objectives: Influenza continues to cause high morbidity and mortality rates worldwide, inflicting a major burden on the public health system. There is little data available on the 2024–2025 seasonal outbreak. Moreover, biomarkers for rapidly identifying subjects at higher risk for severe forms are needed. Methods: We retrospectively collected hospitalization data for influenza in Cannes, France, during the 2024–2025 seasonal outbreak. Severe forms were defined as cases either requiring admission to the Intensive Care Unit (ICU) or resulting in death. They were compared to uncomplicated forms. Main demographic, clinical, radiological, and laboratory characteristics were collected for each patient. Results: From October 2024 to May 2025, 59 patients were admitted to either the Infectious Diseases Department or the ICU (56% male, age 72 years, 27% vaccinated, influenza type A 93%, symptom duration 3.5 days prior to hospitalization, 31% admissions to ICU, 14% deaths). Vaccination status did not differ between severe and uncomplicated forms. In the univariate analysis, severe forms had higher neutrophil/lymphocyte and platelet/lymphocyte ratios upon admission and included more cases of acute hepatitis, pneumonia, and oseltamivir use than uncomplicated forms. A neutrophil/lymphocyte ratio > 15 was independently associated with severity (ORadj 8.79, 95% CI: 1.34–57.6, p = 0.023), with 40.9% sensitivity, 94.6% specificity, 81.8% positive predictive value, and 72.3% negative predictive value for predicting a severe form. Conclusions: The N/L ratio was an easy-to-perform predictive marker for influenza severity during the 2024–2025 seasonal outbreak, warranting further prospective studies
Full article
Open AccessArticle
Knowledge, Attitudes, and Practices Associated with Human Papillomavirus Vaccine Recommendation Among Healthcare Professionals: A Cross-Sectional Study
by
Layla M. Abdelhadi, Fatima S. Aryan, Rania Alsabi, Ghounan A. Samhan and Ayman M. Al-Qaaneh
Infect. Dis. Rep. 2025, 17(5), 126; https://doi.org/10.3390/idr17050126 - 9 Oct 2025
Abstract
►▼
Show Figures
Background: Cervical cancer remains a significant global public health concern, with human papillomavirus (HPV) vaccination serving as an effective preventive measure. Despite its proven efficacy, HPV vaccine uptake in Jordan remains low. This study aimed to assess the knowledge, attitudes, and practices (KAP)
[...] Read more.
Background: Cervical cancer remains a significant global public health concern, with human papillomavirus (HPV) vaccination serving as an effective preventive measure. Despite its proven efficacy, HPV vaccine uptake in Jordan remains low. This study aimed to assess the knowledge, attitudes, and practices (KAP) influencing HPV vaccine recommendation among healthcare professionals. Methods: A cross-sectional survey was conducted between August 2023 and February 2024 among 304 healthcare professionals and trainees in Amman, Jordan, using a pre-validated questionnaire. Descriptive statistics, correlational analyses, and Firth’s penalized logistic regression were employed to examine predictors of vaccine recommendation behavior. Results: Positive attitudes (OR = 3.89; p < 0.001) and active clinical practice (OR = 5.02; p < 0.001) were strong predictors of HPV vaccine recommendation. Unexpectedly, higher knowledge scores were associated with reduced likelihood of recommending the vaccine (OR = 0.44; p = 0.032). Significant variation in KAP scores was observed across professional groups, with physicians and academic staff demonstrating higher levels of engagement. Conclusions: Attitudes and practical engagement were more influential than knowledge alone in shaping HPV vaccine recommendation behavior among healthcare professionals. These findings underscore the need for interventions that not only enhance knowledge but also foster supportive attitudes and strengthen clinical advocacy skills. The results provide actionable evidence to inform targeted strategies for increasing HPV vaccine uptake and reducing cervical cancer incidence in Jordan.
Full article

Figure 1
Open AccessCase Report
Cutaneous Leishmaniasis in the Immunocompromised: Diagnostic and Therapeutic Insights from a Case Documented in Central Italy
by
Laura Povolo, Anna Barbiero, Michele Spinicci, Nicola Petrosillo, Alessandro Bartoloni and Lorenzo Zammarchi
Infect. Dis. Rep. 2025, 17(5), 125; https://doi.org/10.3390/idr17050125 - 8 Oct 2025
Abstract
Introduction: Cutaneous leishmaniasis (CL) poses a number of challenges when it comes to diagnosis and treatment, due to the variety of clinical presentations that mimic other conditions and hinder the choice of the most appropriate therapeutic approach, especially in the context of immunodepression.
[...] Read more.
Introduction: Cutaneous leishmaniasis (CL) poses a number of challenges when it comes to diagnosis and treatment, due to the variety of clinical presentations that mimic other conditions and hinder the choice of the most appropriate therapeutic approach, especially in the context of immunodepression. Case presentation: We present the case of a 63-year-old woman on anti-tumor necrosis factor (TNF) therapy, who underwent surgical excision for the diagnostic purposes of a chronic non-healing lesion located on her right arm. The histopathological examination revealed the presence of Leishmania amastigotes. CL relapsed in the following months, with new lesions appearing both close to the excision scar and at a different body site. At this point, in order to avoid another surgical intervention, cutaneous swabs for Leishmania Polymerase Chain Reaction (PCR) were performed on both lesions. Both samples yielded positive results, and the patient was treated with a 4-week course of miltefosine. Conclusions: These results support the use of cutaneous swabs as a highly sensitive and less invasive tool for the diagnostic workup of CL. In addition, our case prompts a reflection on the management of immunosuppressed patients with CL, with particular emphasis on the risk of reactivation or simultaneous involvement of multiple anatomical sites, thus suggesting the need for specific considerations and personalized management for this group of subjects.
Full article
(This article belongs to the Section Neglected Tropical Diseases)
►▼
Show Figures

Figure 1
Open AccessReview
Public Health Impact of the MVA-BN Vaccine During the 2022 Mpox Outbreak: A Systematic Review
by
Sarah C. Katsandres, Suzanne K. Scheele, Takako Kiener and Lisa Bloudek
Infect. Dis. Rep. 2025, 17(5), 124; https://doi.org/10.3390/idr17050124 - 7 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Previously endemic to sub-Saharan Africa, mpox has since emerged globally, resulting in more than 150,000 cases in over 100 countries in the 2022 outbreak. The Modified Vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine is licensed and recommended for at-risk populations in many countries and
[...] Read more.
Background/Objectives: Previously endemic to sub-Saharan Africa, mpox has since emerged globally, resulting in more than 150,000 cases in over 100 countries in the 2022 outbreak. The Modified Vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine is licensed and recommended for at-risk populations in many countries and received World Health Organization (WHO) pre-qualification in September 2024. Methods: We conducted this systematic literature review (SLR) to compare analyses, published from 2022 through 2024, of cases averted due to mpox vaccination during the 2022 outbreak to assess the feasibility of estimating the impact on the United States (US). The search included studies that utilized reported case data from any country. Results: Nine studies were identified. Four estimated the impact of the vaccine as directly modeled in the 2022 outbreak, and cases averted ranged from 10% to 79%. One assessed the projected impact on future outbreaks. Four estimated the impact of hypothetical vaccination strategies. Only one model utilized assumptions appropriate for the US outbreak and population, to allow for an estimate of US cases averted (53,499 cases averted due to the synergistic effects of the vaccine and behavioral changes, with 8096 due to the mpox vaccine alone and 5478 due to behavioral changes alone). Conclusions: Variation in estimates for the impact of the vaccine can typically be explained by differing model approaches, assumptions, inputs, and epidemic peaks and vaccination campaign roll-out. Most models were not generalizable to the US outbreak and population, but one yielded a reasonable estimate. Nevertheless, all models emphasized the importance of vaccination combined with other public health interventions.
Full article

Figure 1
Open AccessArticle
Dolutegravir Resistance in Mozambique: Insights from a Programmatic HIV Resistance Testing Intervention in a Highly Antiretroviral Therapy-Experienced Cohort
by
Maria Ruano, Antonio Flores, Aleny Couto, Irénio Gaspar, Sabine Yerly, Ana Gabriela Gutierrez Zamudio, Rosa Bene, Adelina Maiela, Helder Macuacua, Jeff Lane, Florindo Mudender and Edy Nacarapa
Infect. Dis. Rep. 2025, 17(5), 123; https://doi.org/10.3390/idr17050123 - 30 Sep 2025
Abstract
►▼
Show Figures
Background: Treatment failure continues to play a role in HIV-related morbidity in Mozambique. Antiretroviral therapy (ART) regimen switches are decided empirically, as HIV genotypic resistance testing (HIV-GT) is unavailable in Mozambique’s public health system. Since 2016, Médecins Sans Frontières (MSF) and I-TECH
[...] Read more.
Background: Treatment failure continues to play a role in HIV-related morbidity in Mozambique. Antiretroviral therapy (ART) regimen switches are decided empirically, as HIV genotypic resistance testing (HIV-GT) is unavailable in Mozambique’s public health system. Since 2016, Médecins Sans Frontières (MSF) and I-TECH have provided access to HIV-GT at Alto Maé Health Center, Maputo. We describe the cohort of people with virologic failure (VF) that underwent HIV-GT and analyze dolutegravir (DTG) resistance (R) patterns. Methods: This cross-sectional assessment of routine programmatic data between July 2020 and February 2024 was conducted to guide future program enhancements. People living with HIV (PLWH) receiving ART beyond the first line with confirmed VF were included. Mutations were interpreted according to the Stanford HIVdb algorithm. We applied Bayesian bootstrapping for analysis, and the threshold for significance of effects was defined as a probability of 95%. Results: A total of 106 persons underwent HIV-GT following a structured adherence strategy, 62 (58.5%) of whom were on a DTG-based regimen. Fifty-seven of the 62 samples from persons on a DTG-based regimen were sequenced, and 51 (89.5% [95% CrI: 80.7, 96.2]) had confirmed resistance to DTG; the mean DTG-R score was 70.2 (95% CrI: 62.2, 78). Samples with DTG-R had a median of three INSTI mutations (IQR 1–4). Major DTG-associated mutations were found in 46 out of 57 samples: G118R (n = 28), R263K (n = 15), and Q148RK (n = 7). None of the people on the protease inhibitor regimen had an INSTI mutation. Conclusions: In contexts with limited access to resistance testing, the introduction of algorithms to identify PLWH at risk of developing drug resistance is strongly recommended. The proposed algorithm incorporates adherence reinforcement strategies, as recommended in national policies, followed by a short, supervised antiretroviral therapy (ART) support strategy. This approach has shown a high predictive value for identifying PLWH with resistance mutations to dolutegravir (DTG), thereby allowing the continuation of the effective DTG regimen without unnecessary regimen switches.
Full article

Figure 1
Open AccessArticle
Profile, Infection, and Vaccination Uptake: A Cohort of Canadian Retail Workers During the SARS-CoV-2 Pandemic
by
Mathieu Thériault, Kim Santerre, Nicholas Brousseau, Samuel Rochette, Rabeea F. Omar, Joelle N. Pelletier, Caroline Gilbert, Jean-François Masson, Mariana Baz, Denis Boudreau and Sylvie Trottier
Infect. Dis. Rep. 2025, 17(5), 122; https://doi.org/10.3390/idr17050122 - 29 Sep 2025
Abstract
Background/Objectives: Retail workers may have been at an increased risk of contracting SARS-CoV-2 during the COVID-19 pandemic. To better understand this group, we set up a longitudinal cohort to document the occurrence of SARS-CoV-2 infection, vaccination uptake and to study immune response. Methods:
[...] Read more.
Background/Objectives: Retail workers may have been at an increased risk of contracting SARS-CoV-2 during the COVID-19 pandemic. To better understand this group, we set up a longitudinal cohort to document the occurrence of SARS-CoV-2 infection, vaccination uptake and to study immune response. Methods: Participants were enrolled between 20 April and 22 October 2021 and attended up to 5 visits over 48 weeks. Information collected was: participant characteristics, SARS-CoV-2 detection tests performed, COVID-19 symptoms, and vaccination (influenza and SARS-CoV-2). Findings: We included 304 participants aged 18 to 75; of those, 117 had a first positive SARS-CoV-2 test, mostly (85.5%) during Omicron wave. Forty-two (13.8%) participants got seasonal influenza vaccine within the year (2020–2021) prior to the first visit, and 95.9% had received the primary series of 2 doses of SARS-CoV-2 vaccine by the beginning of Omicron wave. Participants vaccinated for influenza (adjusted hazard ratio (aHR) 2.48; 95% confidence interval (CI): 1.54–3.98) and older patients (aHR 2.39; 95% CI: 1.40–4.10), were more likely to get a first booster of SARS-CoV-2 vaccine compared to those who did not receive influenza vaccine. In contrast, participants who traveled (aHR 0,62; 95% CI: 0.43–0.91) or participated in frequent gatherings (aHR 0.58; 95% CI: 0.39–0.85) were less likely to be boosted. Conclusions: Variations in vaccine uptake that are usually observed within populations had little effect on completion of the primary SARS-CoV-2 vaccine series. However, these differences became apparent for booster doses, at a period during which most infections in this cohort were recorded.
Full article
(This article belongs to the Special Issue Prevention, Diagnosis and Treatment of Infectious Diseases)
►▼
Show Figures

Figure 1
Open AccessCase Report
More than Mucositis: Pediatric RIME Following Co-Infection with SARS-CoV-2 and Mycoplasma pneumoniae—A Case Report and Mini-Review
by
Alina Corina Grama, Ovidiu Grama, Măriuca Mănescu and Mihaela Chinceșan
Infect. Dis. Rep. 2025, 17(5), 121; https://doi.org/10.3390/idr17050121 - 24 Sep 2025
Abstract
Background: Reactive Infectious Mucocutaneous Eruption (RIME) is a mucositis-predominant syndrome that usually follows respiratory infections in children. Although Mycoplasma pneumoniae is a well-established trigger, viral pathogens as triggers—especially SARS-CoV-2—have been increasingly reported. RIME is often misclassified as Stevens–Johnson syndrome (SJS), which may lead
[...] Read more.
Background: Reactive Infectious Mucocutaneous Eruption (RIME) is a mucositis-predominant syndrome that usually follows respiratory infections in children. Although Mycoplasma pneumoniae is a well-established trigger, viral pathogens as triggers—especially SARS-CoV-2—have been increasingly reported. RIME is often misclassified as Stevens–Johnson syndrome (SJS), which may lead to inappropriate management. Case Presentation: We describe a 12-year-old previously healthy boy who presented with fever, dry cough, odynophagia, and vomiting for 9 days. On admission, he had severe oral ulcerations, bilateral conjunctivitis, and a non-blanching maculopapular rash. Laboratory tests confirmed co-infection with M. pneumoniae and SARS-CoV-2. Inflammatory markers were mildly elevated. Notably, the patient also developed asymptomatic sinus bradycardia, with no signs of structural heart disease. He was treated with antibiotics, intravenous corticosteroids, and supportive care. His mucosal symptoms improved rapidly, and he was discharged in stable condition on day 7. Follow-up at 12 days showed near-complete resolution of all lesions. Conclusions: This case illustrates several clinically relevant features. First, it highlights a dual infectious trigger—M. pneumoniae and SARS-CoV-2—that may have contributed to a more severe mucosal reaction. Second, the patient developed transient sinus bradycardia without myocardial involvement, suggesting a possible inflammatory autonomic response, rarely reported in RIME. Finally, this case supports the early use of corticosteroids in severe mucosal disease, with good outcomes and no complications. Prompt recognition of RIME, especially in the context of viral–bacterial coinfection, is essential to avoid misdiagnosis and to guide appropriate, multidisciplinary management.
Full article
(This article belongs to the Section Bacterial Diseases)
►▼
Show Figures

Figure 1
Open AccessEditor’s ChoiceReview
Clean to Prevent, Monitor to Protect: A Scoping Review on Strategies for Monitoring Cleaning in Hospitals to Prevent HAIs
by
Biagio Santella, Antonio Donato, Luigi Fortino, Vittoria Satriani, Rosaria Flora Ferrara, Emanuela Santoro, Walter Longanella, Gianluigi Franci, Mario Capunzo and Giovanni Boccia
Infect. Dis. Rep. 2025, 17(5), 120; https://doi.org/10.3390/idr17050120 - 21 Sep 2025
Abstract
Background/Objectives: Hospital environmental contamination represents a significant source of healthcare-associated infections, yet standardized monitoring approaches are still inconsistent globally. This scoping review aimed to find and assess various tools and strategies used to monitor hospital environmental cleaning and disinfection practices, mapping current evidence
[...] Read more.
Background/Objectives: Hospital environmental contamination represents a significant source of healthcare-associated infections, yet standardized monitoring approaches are still inconsistent globally. This scoping review aimed to find and assess various tools and strategies used to monitor hospital environmental cleaning and disinfection practices, mapping current evidence and finding research gaps to inform evidence-based recommendations for healthcare facilities. Methods: Following PRISMA Scoping Review guidelines, we conducted comprehensive searches on PubMed and Scopus databases from 2010–2025 using terms related to environmental monitoring, surface sampling, air sampling, and infection control in hospital settings. Eighteen studies met inclusion criteria; data were extracted using standardized forms and synthesized narratively, organizing findings by monitoring approach categories. Results: These studies revealed diverse monitoring approaches including fluorescent markers (22.2%), ATP bioluminescence assays (33.3%), microbiological methods (44.4%), and direct observation techniques (27.8%). MRSA was the most frequently targeted pathogen (55.6%), with limited attention to Gram-negative multidrug-resistant organisms and fungi. Studies showed significant variability in pass/fail thresholds (ATP: 50–500 RLU) and lack of standardized benchmarks. Recent research (50% post-2021) increasingly incorporates molecular techniques and digital technologies, though implementation remains resource intensive. Conclusions: A multimodal approach combining visual inspection, ATP assays, and microbiological methods appears most effective for comprehensive environmental monitoring. Critical gaps include lack of standardized thresholds, limited pathogen diversity focus, and insufficient integration of emerging digital technologies. Future research should focus on setting universal standards, expanding pathogen coverage, and assessing cost-effective monitoring strategies, all while ensuring legal compliance with hygiene regulations to enhance patient safety.
Full article
(This article belongs to the Special Issue Containment Strategies of Infectious Diseases: Epidemiology, Surveillance and Prophylaxis)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Characterization of Carbapenem-Resistant Gram-Negative Bacilli Isolates in Multispecialty Private Hospitals in Lagos, Nigeria
by
Moruf Salau, Uraiwan Kositanont, Pirom Noisumdaeng, Folasade Ogunsola, Abdul-Wahab Omo-ope Ettu, Damilola Adewojo, Chinonso Ojimma, Omamode Ojomaikre and Kanjana Changkaew
Infect. Dis. Rep. 2025, 17(5), 119; https://doi.org/10.3390/idr17050119 - 21 Sep 2025
Abstract
Background/Objectives: Carbapenem-resistant Gram-negative bacilli (CR-GNB) pose a growing challenge to public health worldwide due to limited treatment options. This cross-sectional study investigated the characteristics of CR-GNB isolated from clinical specimens in Lagos, Nigeria. Methods: Gram-negative bacilli (GNB) and clinical data were obtained from
[...] Read more.
Background/Objectives: Carbapenem-resistant Gram-negative bacilli (CR-GNB) pose a growing challenge to public health worldwide due to limited treatment options. This cross-sectional study investigated the characteristics of CR-GNB isolated from clinical specimens in Lagos, Nigeria. Methods: Gram-negative bacilli (GNB) and clinical data were obtained from three multi-specialist private hospitals between March and June 2023. The GNB were identified using the Analytical Profile Index (API) and investigated for CR-GNB by disk diffusion. Antimicrobial resistance patterns and carbapenemase gene data for presumptive carbapenemase-producing Gram-negative bacilli (CP-GNB) were analyzed using Vitek-2 and polymerase chain reaction (PCR). Results: Of 317 GNB, 29.0% (n = 92) were CR-GNB. Significantly higher numbers of CR-GNB were reported from the intensive care unit and oncology department (p = 0.009). Of all CR-GNB, 17 isolates (18.5%) were classified as presumptive CP-GNB. In this subgroup, resistance rates of ampicillin/sulbactam (100.0%) and trimethoprim/sulfamethoxazole (100.0%) were highest. Ten (10) CP-GNB were confirmed, representing 3.15% of all GNB tested. Seven isolates of New Delhi Metallo-β-lactamase (blaNDM) were found among P. aeruginosa, K. pneumoniae, E. coli, and A. baumannii. The blaNDM was identified in strains classified as extensively drug-resistant (XDR) and pandrug-resistant. Conversely, the blaKPC was detected solely in multidrug-resistant and XDR strains. Conclusions: Emerging CR-GNB, specifically CP-GNB, in Nigeria emphasize the need for specific therapeutic management of infected patients. Antimicrobial stewardship and long-term surveillance efforts must be implemented in healthcare settings, as well as improved, accelerated microorganism identification techniques.
Full article
(This article belongs to the Section Antimicrobial Stewardship and Resistance)
►▼
Show Figures

Figure 1
Open AccessEditor’s ChoiceEditorial
Recombinant Yeast-Based Vaccines: Importance and Applications
by
Ravinder Kumar
Infect. Dis. Rep. 2025, 17(5), 118; https://doi.org/10.3390/idr17050118 - 18 Sep 2025
Abstract
Vaccines are biological preparations used to elicit an immune response, in order to prevent future infections or minimize damage from possible future infection [...]
Full article
Open AccessReview
State of the Art on Vaccine Development Against Dengue Infection: Scoping Review of the Literature
by
Davide Marangoni, Anna Barbiero, Michele Spinicci, Alessandro Bartoloni, Andrea Rossanese, Paolo Bonanni and Lorenzo Zammarchi
Infect. Dis. Rep. 2025, 17(5), 117; https://doi.org/10.3390/idr17050117 - 17 Sep 2025
Abstract
Background: Dengue virus infection is a significant challenge for global health, with 100 million symptomatic cases, 2.3 million DALYs and 20,000 deaths annually. Dengue vaccines must provide long-lasting immunity against all four virus serotypes, especially in dengue-naïve individuals, in order to avoid the
[...] Read more.
Background: Dengue virus infection is a significant challenge for global health, with 100 million symptomatic cases, 2.3 million DALYs and 20,000 deaths annually. Dengue vaccines must provide long-lasting immunity against all four virus serotypes, especially in dengue-naïve individuals, in order to avoid the severe manifestations of secondary infections. Methods: This scoping review summarizes current evidence on licensed dengue vaccines and vaccine candidates, focusing on immunogenicity, efficacy, and safety outcomes. To identify relevant trials, in October 2023 we queried ClinicalTrials.gov using the search term “dengue vaccines” to identify past and present vaccine candidates; the search was repeated in February 2025. Vaccines were categorized into licensed (CYD-TDV and TAK-003), late-stage (TV003/TV005), and early-stage candidates (TDEN, DPIV, V180, TVDV). Results: CYD-TDV (Dengvaxia®) showed moderate efficacy in large trials, with higher efficacy in seropositive than in seronegative individuals. Following commercialization, an increased hospitalization risk was discovered in the latter group. Due to these findings and impossibility of screening for prior exposure in endemic settings newer vaccines are now preferred and CYD-TDV production has recently been discontinued due to declining demand. TAK-003 (Qdenga®) demonstrated high efficacy against virologically confirmed dengue (VCD) and dengue-related hospitalization. This vaccine was generally well tolerated and is currently recommended by scientific societies and national authorities for travelers and by WHO for routine use in adults and children in endemic settings. TV003 and TV005, developed by NIAID, showed strong immunogenicity and efficacy in phase II trials and human challenge models. Preliminary results show that a single-dose of TV003 has an efficacy of 79.6% in seronegatives and 89.2% in seropositives against VCD at a 2-year follow-up. Both formulations elicited tetravalent responses with an acceptable safety profile. Other vaccine strategies, including TDEN (live-attenuated), DPIV (purified inactivated), V180 (subunit), and TVDV (DNA-based) are still in early-phase development and suffer from waning antibody titers and limited efficacy in naïve subjects. Conclusions: The development of a safe and effective vaccine remains complex due to immunologic challenges. Currently, TAK-003 is regarded as the best option for broad implementation, while TV003 and TV005 remain promising candidates due to their shorter schedule and robust immunogenicity. Further research is needed to optimize vaccine strategies in seronegative populations, immunocompromised subjects, older adults, and travelers.
Full article
(This article belongs to the Section Immunology and Vaccines)
►▼
Show Figures

Figure 1
Open AccessEditor’s ChoiceBrief Report
Pathways to Diagnose Infectious Pulmonary Vascular Disease in Rural Mozambique
by
Yolanda Sabino, Cizália Ribeiro, Joshua Mungue and Ana Olga Mocumbi
Infect. Dis. Rep. 2025, 17(5), 116; https://doi.org/10.3390/idr17050116 - 15 Sep 2025
Abstract
Background: Schistosomiasis, HIV, and tuberculosis frequently lead to pulmonary hypertension in low- and middle-income countries. Lack of specific testing and limited access to right heart catheterization hamper confirmation of the etiology of pulmonary hypertension due to schistosomiasis. In addition, low health literacy and
[...] Read more.
Background: Schistosomiasis, HIV, and tuberculosis frequently lead to pulmonary hypertension in low- and middle-income countries. Lack of specific testing and limited access to right heart catheterization hamper confirmation of the etiology of pulmonary hypertension due to schistosomiasis. In addition, low health literacy and poor socioeconomic status further compromise prevention, early diagnosis, and treatment. Clinical algorithms for early screening, including hand-held echocardiography and point-of-care testing performed by non-specialists, are needed in rural Sub-Saharan Africa to decentralize care and improve outcomes. Methods: We describe a case of pulmonary hypertension diagnosed in a child living in Mozambique, to discuss the challenges for the diagnosis of infectious pulmonary arterial hypertension in rural settings in Africa, based on a short literature review.
Full article
(This article belongs to the Special Issue Pulmonary Vascular Manifestations of Infectious Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Uneven Implementation of Nirsevimab Prophylaxis Resulted in Non-Uniform Reductions in RSV-Related Hospitalizations in Italy
by
Melodie O. Aricò, Francesco Accomando, Daniela Trotta, Giulia Marozzi, Anthea Mariani, Claudia Rossini, Claudio Cafagno, Letizia Lorusso, Martina Fornaro, Enrico Valletta, Désirée Caselli and Maurizio Aricò
Infect. Dis. Rep. 2025, 17(5), 115; https://doi.org/10.3390/idr17050115 - 12 Sep 2025
Abstract
Background/Objectives: Respiratory syncytial virus (RSV) bronchiolitis remains a leading cause of hospitalization in infants. In the 2024–2025 season, passive newborn immunization with nirsevimab, a long-acting anti-RSV monoclonal antibody, was introduced for the first time in Italy. However, the immunization campaign was not uniformly
[...] Read more.
Background/Objectives: Respiratory syncytial virus (RSV) bronchiolitis remains a leading cause of hospitalization in infants. In the 2024–2025 season, passive newborn immunization with nirsevimab, a long-acting anti-RSV monoclonal antibody, was introduced for the first time in Italy. However, the immunization campaign was not uniformly implemented on a regional basis due to supply and organizational difficulties. The aim of the study was to assess the real-world impact of nirsevimab prophylaxis during the 2024–2025 bronchiolitis season in four regions of Italy. Methods: This multicenter observational study included infants <12 months hospitalized for bronchiolitis across four Italian centers. Hospitalizations due to RSV and non-RSV bronchiolitis were compared across the 2023–2024 and 2024–2025 seasons, in relation to the timing and coverage of nirsevimab’s introduction in each of the four regions. Results: Early and widespread nirsevimab administration was associated with a significant reduction in RSV hospitalizations and severity of disease. Centers located in regions that had delayed implementation of immunization observed higher RSV burden and intensive care unit admissions. Admissions for non-RSV bronchiolitis remained stable. Conclusions: Timely and universal administration of nirsevimab significantly reduced RSV hospitalizations and severity, while delayed implementation resulted in limited benefit. These findings support early and uniform prophylaxis to mitigate health disparities and seasonal pressure on pediatric healthcare systems.
Full article
(This article belongs to the Section Infection Prevention and Control)
►▼
Show Figures
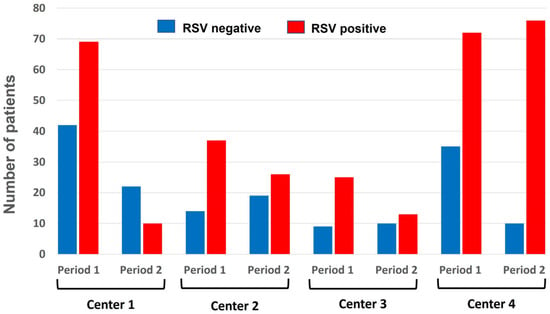
Figure 1
Open AccessArticle
Uncommon Pathogens in Common Presentations: Genetic Profiling and Virulence Determinants of Vibrio alginolyticus Isolated from a Case of External Otitis
by
Radu Ovidiu Togănel, Razvan Lucian Coșeriu, Anca Delia Mare, Camelia Vintilă, Ioan-Ovidiu Sîrbu, Aimée Rodica Chis, Cristina Elena Gîrbovan and Adrian Man
Infect. Dis. Rep. 2025, 17(5), 114; https://doi.org/10.3390/idr17050114 - 12 Sep 2025
Abstract
Backgrunod/Objectives: Routine identification of common bacterial pathogens is typically efficient, utilizing standardized, cost-effective methods. However, the diagnostic process becomes significantly more complex when dealing with rare or unexpected microorganisms, especially as they can be considered colonizers in many cases. Methods: This
[...] Read more.
Backgrunod/Objectives: Routine identification of common bacterial pathogens is typically efficient, utilizing standardized, cost-effective methods. However, the diagnostic process becomes significantly more complex when dealing with rare or unexpected microorganisms, especially as they can be considered colonizers in many cases. Methods: This study presents diagnostic details of an uncommon pathogen, Vibrio alginolyticus, isolated from auricular discharge in a patient with non-Hodgkin lymphoma diagnosed with persistent otitis externa and explores its identification through both conventional and modern laboratory approaches. Sequential ear discharge cultures resulted in phenotypically similar but genomically different Vibrio alginolyticus isolates. We complemented classical methods like conventional culture (on Columbia agar and CLED agar), Vitek2 Compact identification, and EUCAST disk diffusion antimicrobial susceptibility testing (following the EUCAST version 12.0 guidelines) with MALDI-TOF mass spectrometry and Illumina/Nanopore whole genome sequencing. Comparative analysis of the genomes was performed with the PeGAS pipeline, Unicycler, and 1928Diagnostics SNP analysis. Results: The Vitek2 analysis identified both isolates as V. alginolyticus with 99% confidence, and this was supported by the MALDI-TOF MS results. The first isolate (A) was fully susceptible to the antibiotics tested, while the second (B) showed resistance to ciprofloxacin. Whole genome sequencing revealed 99.23% and 98.60% nucleotide identity to the V. alginolyticus reference genome for isolates A and B, respectively, with a 99.8% match between them. Isolate B acquired a gyrA (c.1870C>T) mutation that correlates with the ciprofloxacin resistance (MIC > 0.5 mg/L). Both genomes carry hlyA (hemolysin), toxR (cholera toxin regulator), genes involved in biofilm formation (rpoN, relA, spoT, opp), luxS (motility), proA, vacB (virulence factors), and tet(34) (oxytetracycline resistance). A core genome SNP distance of <100 indicates clonal relatedness. Our integrated (phenotypic and genomic) diagnostic approach confirmed V. alginolyticus and documented host resistance evolution, with a virulence repertoire that could explain the clinical evolution. Conclusions: This case highlights the utility of molecular methods in confirming species identity, detecting resistance markers, characterizing virulence determinants, and differentiating a pathogen from a colonizer, supporting targeted clinical management.
Full article
Open AccessArticle
Imported Dengue Fever in Milan, Italy: A Seven-Year Retrospective Study
by
Margherita Eleonora Pieruzzi, Davide Mileto, Alessandra Helen Behring, Stefania Caronni, Alessandro Mancon, Luigi Vezzosi, Alberto Rizzo, Andrea Poloni, Andrea Gori, Andrea Giacomelli and Spinello Antinori
Infect. Dis. Rep. 2025, 17(5), 113; https://doi.org/10.3390/idr17050113 - 12 Sep 2025
Abstract
Background: Dengue fever is an arboviral infection transmitted by Aedes mosquitoes that has recently become a public health concern also in Europe, causing many outbreaks of autochthonous cases. Methods: We retrospectively retrieved dengue cases in returning travelers from tropical areas diagnosed at the
[...] Read more.
Background: Dengue fever is an arboviral infection transmitted by Aedes mosquitoes that has recently become a public health concern also in Europe, causing many outbreaks of autochthonous cases. Methods: We retrospectively retrieved dengue cases in returning travelers from tropical areas diagnosed at the Luigi Sacco Hospital between January 2018 and December 2024. All patients with positive serology for DENV (IgM alone or IgM and IgG or neutralizing antibodies detection) and/or positive real-time polymerase chain reaction (RT-PCR) for DENV RNA on plasma and urine were considered. Analyses were descriptive. Results: This analysis included 159 travelers with confirmed (n = 138; 86.8%) or probable (n = 21; 13.2%) dengue fever. The median age was 38 years (interquartile range [IQR] 30–50); 87 (54.7%) were females. The median time between symptom onset and seeking medical attention was four days (IQR 3–6); 29.6% required hospitalization, with a median stay of four days (IQR 0–5). The most common symptoms included fever (100%), myalgia (52.2%), and headache (49.1%). Laboratory findings revealed thrombocytopenia (53.8%), leukopenia (64.1%), elevated ALT (51.9%), and LDH (60.2%). Among the confirmed cases, 128 (92.8%) were diagnosed with RT-PCR. Serotypes 1 and 2 were the most prevalent (28.9% and 27.3%, respectively). Most cases were classified as dengue without warning signs (150, 94.3%), eight cases (5.0%) as dengue with warning signs, and one as severe dengue. Conclusions: Dengue fever is an important cause of fever among travelers returning to Italy from endemic areas. Although severe dengue is rare among travelers, further prospective studies need to address this issue. Diagnosis should be pursued by using molecular tools because of cross-reactivity with other arboviruses.
Full article
(This article belongs to the Special Issue Epidemiology, Prevention and Research on Dengue Virus)
►▼
Show Figures

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Infectious Disease Reports, Insects, IJERPH, Pathogens, TropicalMed, Zoonotic Diseases
Vector-Borne Disease Spatial Epidemiology, Disease Ecology, and Zoonoses
Topic Editors: Chad L. Cross, Louisa Alexandra MessengerDeadline: 31 December 2025
Topic in
IJERPH, TropicalMed, Microorganisms, Infectious Disease Reports, Pathogens
Genetic, Environmental, and Climatic Drivers of Emerging Arboviruses and Public Health Implications
Topic Editors: André Ricardo Ribas Freitas, Pedro María Alarcón-Elbal, Luciano Pamplona de Góes CavalcantiDeadline: 20 January 2027
Topic in
Diseases, Epidemiologia, Infectious Disease Reports, Medicina, TropicalMed
Surveillance Systems and Predictive Analytics for Epidemics
Topic Editors: Georgia Kourlaba, Elisavet StavropoulouDeadline: 31 January 2027

Special Issues
Special Issue in
Infectious Disease Reports
Emerging and Re-Emerging Infections: Surveillance, Diagnostics, and Global Health Impacts
Guest Editors: Massimo Ciccozzi, Marta Giovanetti, Francesco BrandaDeadline: 31 October 2025
Special Issue in
Infectious Disease Reports
Epidemiology, Prevention and Research on Dengue Virus
Guest Editor: Alessandro BartoloniDeadline: 31 December 2025
Special Issue in
Infectious Disease Reports
Containment Strategies of Infectious Diseases: Epidemiology, Surveillance and Prophylaxis
Guest Editors: Giovanni Boccia, Gianluigi Franci, Enrica SerretielloDeadline: 31 December 2025
Special Issue in
Infectious Disease Reports
Prevention, Diagnosis and Treatment of Healthcare-Associated Infections
Guest Editor: Emine Alp MeşeDeadline: 31 May 2026










