Excess Mortality on Italian Small Islands during the SARS-CoV-2 Pandemic: An Ecological Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Background
2.2. Population Data
2.3. Data about COVID-19
2.4. Statistical Analysis
3. Results
3.1. Demographics
3.2. Characteristics of COVID-19 Pandemic
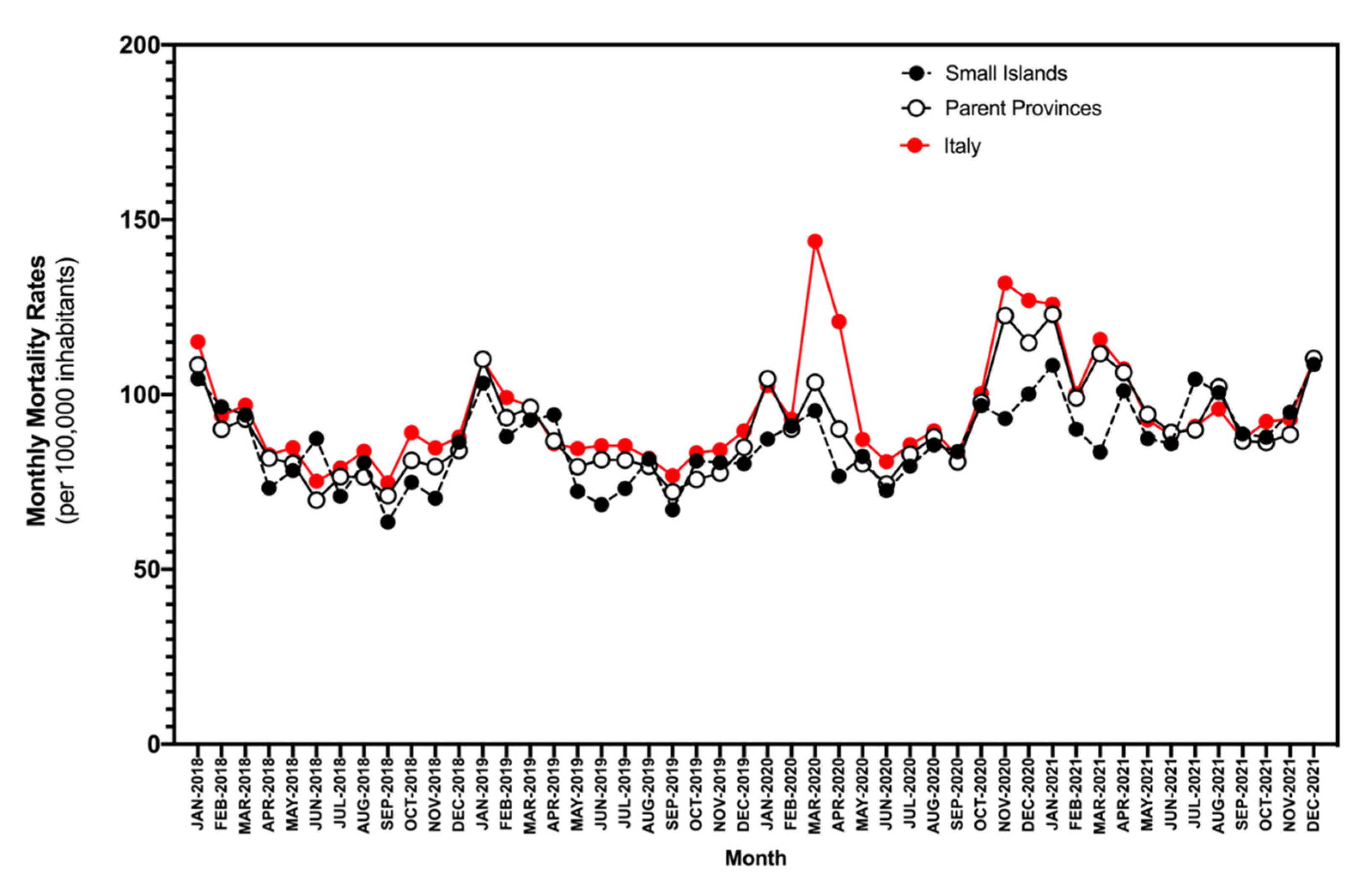
3.3. Excess Mortality
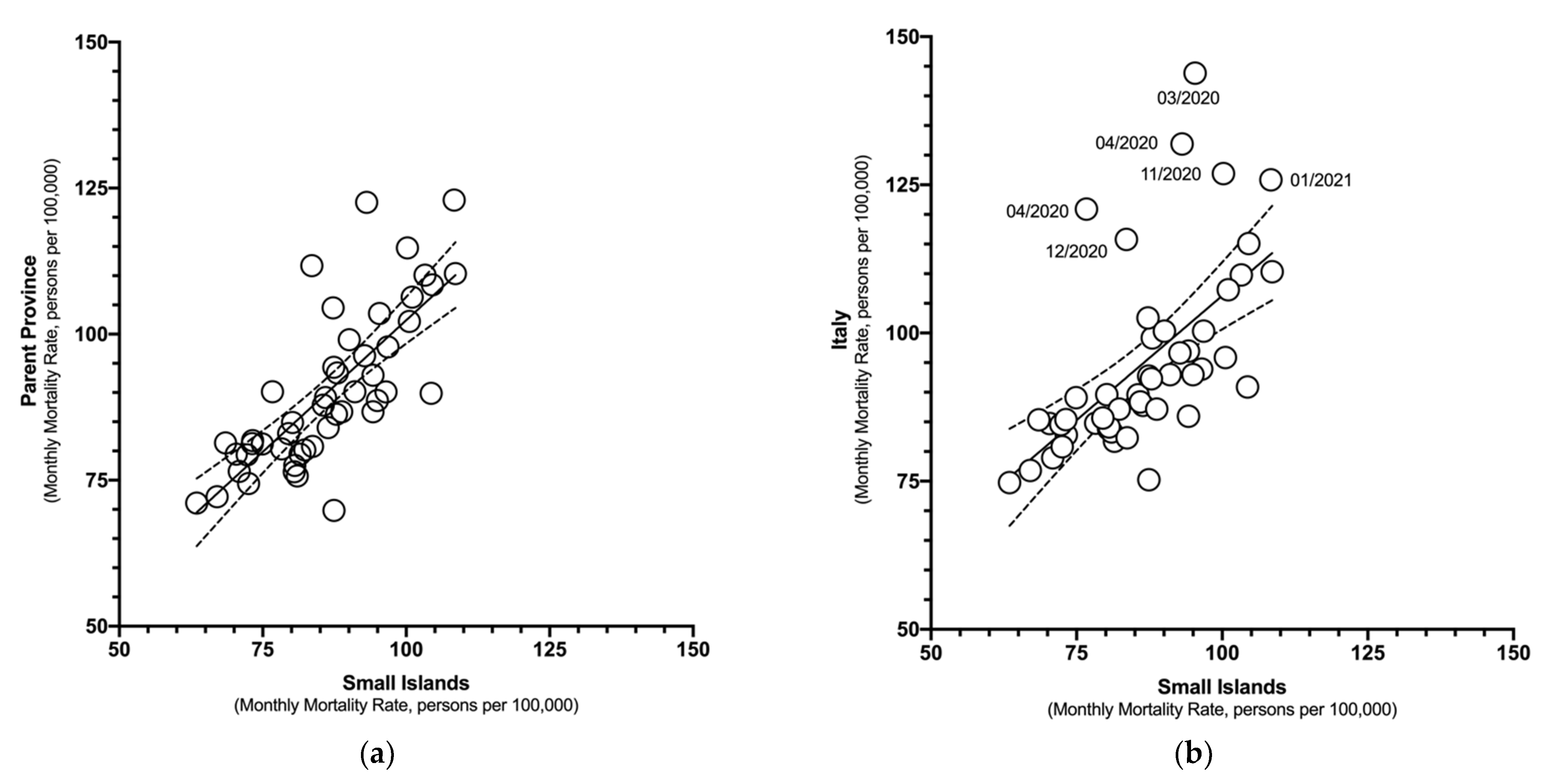
3.4. Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Municipality | Province | Region | Island(s) | Surface (km2) | Availability Of Hospital Infrastructure on the Main Island | Availability of ICU | Average Annual Income per Capita (€) | Total Population (2020) (No., % of All Small Islands) | Total Population (2021) (No., % of All Small Islands) | Total Deaths (2020) (No., % of All Small Islands) | Total Deaths (2021) (No., % of All Small Islands) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Anacapri | Naples | Campania | Capri | 6.47 | NO | NO | 15,203.09 | 6954 | 6901 | 63 | 82 |
| Barano d’Ischia | Naples | Campania | Ischia | 10.96 | YES | YES | 19,493.79 | 10,027 | 9859 | 71 | 88 |
| Calasetta | South Sardinia | Sardinia | Sant’Antioco | 31.06 | NO | NO | 14,338.55 | 2819 | 2783 | 38 | 44 |
| Campo nell’Elba | Livorno | Tuscany | Elba | 55.79 | YES | NO | 24,036.92 | 4654 | 4691 | 58 | 54 |
| Capoliveri | Livorno | Tuscany | Elba | 39.56 | YES | NO | 16,807.08 | 4013 | 3884 | 36 | 47 |
| Capraia | Livorno | Tuscany | Capraia | 19.33 | NO | NO | 16,012.67 | 394 | 384 | 3 | 4 |
| Capri | Naples | Campania | Capri | 4.06 | NO | NO | 16,579.63 | 7042 | 6916 | 82 | 89 |
| Carloforte | South Sardinia | Sardinia | San Pietro | 51.10 | NO | NO | 16,422.76 | 5987 | 5960 | 89 | 82 |
| Casamicciola Terme | Naples | Campania | Ischia | 5.85 | YES | NO | 21,115.95 | 7949 | 7752 | 64 | 63 |
| Favignana | Trapani | Sicily | Aegadian Islands (Favignana, Levanzo, Marettino, Formica, and Maraone) | 37.45 | NO | NO | 14,190.88 | 4294 | 4359 | 60 | 71 |
| Forio | Naples | Campania | Ischia | 13.08 | YES | NO | 13,476.61 | 17,538 | 17,392 | 141 | 161 |
| Ischia | Naples | Campania | Ischia | 8.14 | YES | NO | 14,730.70 | 19,442 | 19,571 | 188 | 205 |
| Isola del Giglio | Grosseto | Tuscany | Isola del Giglio | 24.01 | NO | NO | 24,047.75 | 1358 | 1340 | 22 | 25 |
| Isole Tremiti | Foggia | Apulia | Tremiti Islands (San Domino, San Nicola, Capraia, Cretaccio, and Pianosa) | 3.18 | NO | NO | 18,341.20 | 449 | 453 | 4 | 4 |
| La Maddalena | Sassari | Sardinia | La Maddalena Islands (La Maddalena, Caprera, Santo Stefano, Spargi, Budelli, Santa Maria, Razzoli) | 52.01 | YES | NO | 16,465.69 | 10,865 | 10,674 | 104 | 132 |
| Lacco Ameno | Naples | Campania | Ischia | 2.08 | YES | NO | 15,726.12 | 4741 | 4648 | 44 | 53 |
| Lampedusa e Linosa | Agrigento | Sicily | Pelagie Islands (Lampedusa, Linosa, Lampione) | 25.22 | NO | NO | 17,774.39 | 6360 | 6337 | 36 | 53 |
| Leni | Messina | Sicily | Salina | 8.79 | NO | 15,227.14 | 681 | 685 | 8 | 7 | |
| Lipari | Messina | Sicily | Aeolian Islands (Lipari, Vulcano, Panarea, Stromboli, Filicudi, and Alicudi) | 89.72 | YES | NO | 13,926.59 | 12,415 | 12,351 | 117 | 132 |
| Malfa | Messina | Sicily | Salina | 8.74 | NO | NO | 14,975.85 | 995 | 979 | 10 | 10 |
| Marciana | Livorno | Tuscany | Elba | 45.45 | YES | NO | 15.118.69 | 2096 | 2048 | 27 | 39 |
| Marciana Marina | Livorno | Tuscany | Elba | 5.86 | YES | NO | 15,685.86 | 1911 | 1880 | 20 | 29 |
| Pantelleria | Trapani | Sicily | Pantelleria | 84.53 | YES | NO | 16,770.52 | 7441 | 7367 | 102 | 104 |
| Ponza | Latina | Latium | Pontian Islands (Ponza, Palmarola, Gavi, Zannone) | 10.16 | NO | NO | 15,590.95 | 3301 | 3306 | 32 | 37 |
| Porto Azzurro | Livorno | Tuscany | Elba | 13.33 | YES | NO | 15,564.11 | 3650 | 3692 | 37 | 35 |
| Porto Torres | Sassari | Sardinia | Asinara, Isola Piana | 104.41 | NO | NO | 14,101.53 | 21,618 | 21,274 | 252 | 199 |
| Porto Venere | La Spezia | Liguria | Palmaria | 7.66 | NO | NO | 17,748.37 | 3380 | 3331 | 52 | 54 |
| Portoferraio | Livorno | Tuscany | Elba | 48.48 | YES | NO | 16,899.45 | 11,903 | 11,897 | 112 | 139 |
| Procida | Naples | Campania | Procida, Vivara | 4.26 | YES | NO | 18,264.82 | 10,295 | 10,162 | 104 | 131 |
| Rio | Livorno | Tuscany | Elba | 36.52 | YES | NO | 19,467.12 | 3363 | 3341 | 49 | 40 |
| Sant’Antioco | South Sardinia | Sardinia | Sant’Antioco | 87.90 | NO | NO | 16,620.89 | 10,842 | 10,705 | 152 | 141 |
| Santa Marina Salina | Messina | Sicily | Salina | 8.78 | NO | NO | 18,668.81 | 857 | 852 | 14 | 11 |
| Serrara Fontana | Naples | Campania | Ischia | 6.44 | YES | NO | 19,135.50 | 3083 | 3027 | 29 | 35 |
| Ustica | Palermo | Sicily | Ustica | 8.65 | NO | NO | 17,225.64 | 1298 | 1280 | 18 | 12 |
| Ventotene | Latina | Latium | Ventotene, Santo Stefano | 1.75 | NO | NO | 17,548.52 | 717 | 717 | 9 | 12 |

References
- EUROSTAT Glossary: Island Region. Available online: https://ec.europa.eu/eurostat/statistics-explained/SEPDF/cache/73764.pdf (accessed on 17 March 2022).
- European Union. The ESPON 2013 Programme The Development of the Islands-European Islands and Cohesion Policy (EUROISLANDS) Targeted Analysis 2013/2/8; ESPON EGTC: Bruxelles, Belgium, 2013. [Google Scholar]
- Brookfield, H.B.R.; McLean, R.F.; Macpherson, J.; Bayliss-Smith, T.; Salvat, B. The UNESCO/UNFPA Population and Environment Project in the Eastern Islands of Fiji—Island Reports No.4; Australian National University: Melbourne, Australia, 1978. [Google Scholar]
- Brookfield, H.; Doube, L. Global Change, the Human Dimension, 1st ed.; Brookfield, H., Doube, L., Eds.; Academy of the Social Sciences in Australia/Australian National University, Research School of Pacific Studies: Canberra, Australia, 1990. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Guidelines for the Implementation of Non-Pharmaceutical Interventions against COVID-19 Key Messages General Considerations on NPI to Control. COVID-19; ECDC: Stockholm, Sweden, 2020.
- Cuschieri, S.; Pallari, E.; Hatziyianni, A.; Sigurvinsdottir, R.; Sigfusdottir, I.D.; Sigurðardóttir, Á.K. A Year of Covid-19: Experiences and Lessons Learnt by Small European Island States—Cyprus, Iceland and Malta. Eur. J. Public Health 2022, 32, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Filho, W.L.; Lütz, J.M.; Sattler, D.N.; Nunn, P.D. Coronavirus: COVID-19 Transmission in Pacific Small Island Developing States. Int. J. Environ. Res. Public Health 2020, 17, 5409. [Google Scholar] [CrossRef]
- Cuschieri, S.; Grech, S. At-Risk Population for COVID-19: Multimorbidity Characteristics of a European Small Island State. Public Health 2021, 192, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, S.; Pallari, E.; Hatziyianni, A.; Sigurvinsdottir, R.; Sigfusdottir, I.D.; Sigurðardóttir, K. Mortality Comparisons of COVID-19 with All-Cause and Non-Communicable Diseases in Cyprus, Iceland and Malta: Lessons Learned and Forward Planning. Public Health 2022, 202, 52–57. [Google Scholar] [CrossRef]
- Calleja, N.; Gualtieri, A.; Terzic, N.; Scoutellas, V.; Calleja-Agius, J. Managing COVID-19 in Four Small Countries: Initial Response to the Pandemic in San Marino, Montenegro, Malta and Cyprus. Health Policy 2022, 126, 281–286. [Google Scholar] [CrossRef]
- Italian Ministry of Health (Ministero della Salute); Direzione Generale della Programmazione Sanitaria. Osservatorio Nazionale per La Verifica Dell’Assistenza Sanitaria Nelle Isole Minori; Italian Ministry of Health: Rome, Italy, 2016.
- Staub, K.; Panczak, R.; Matthes, K.L.; Floris, J.; Berlin, C.; Junker, C.; Weitkunat, R.; Mamelund, S.-E.; Zwahlen, M.; Riou, J. Historically High Excess Mortality During the COVID-19 Pandemic in Switzerland, Sweden, and Spain. Ann. Intern. Med. 2022, 175, 523–532. [Google Scholar] [CrossRef]
- Scortichini, M.; dos Santos, R.S.; Donato, F.D.; De Sario, M.; Michelozzi, P.; Davoli, M.; Masselot, P.; Sera, F.; Gasparrini, A. Excess mortality during the COVID-19 outbreak in Italy: A two-stage interrupted time-series analysis. Int. J. Epidemiol. 2020, 49, 1909–1917. [Google Scholar] [CrossRef]
- Ricco, M.; Peruzzi, S.; Balzarini, F. Epidemiology of West Nile Virus Infections in Humans, Italy, 2012–2020: A Summary of Available Evidences. Trop. Med. Infect. Dis. 2021, 6, 61. [Google Scholar] [CrossRef]
- Alicandro, G.; Remuzzi, G.; Centanni, S.; Gerli, A.; Vecchia, C. la Excess Total Mortality during the Covid-19 Pandemic in Italy: Updated Estimates Indicate Persistent Excess in Recent Months. Med. Lav. 2022, 113, e2022021. [Google Scholar] [CrossRef]
- Caranci, N.; di Girolamo, C.; Bartolini, L.; Fortuna, D.; Berti, E.; Sforza, S.; Rossi, P.G.; Moro, M.L. General and COVID-19-Related Mortality by Pre-Existing Chronic Conditions and Care Setting during 2020 in Emilia-Romagna Region, Italy. Int. J. Environ. Res. Public Health 2021, 18, 13224. [Google Scholar] [CrossRef]
- R Development Core Team. R a Language and Environment for Statistical Computing: Reference Index; R Foundation for Statistical Computing: Vienna, Austria, 2010; ISBN 3900051070. [Google Scholar]
- Cuschieri, S.; Agius, S.; Souness, J.; Brincat, A.; Grech, V. The Fastest National COVID Vaccination in Europe—Malta’s Strategies. Health Sci. Rev. 2021, 1, 100001. [Google Scholar] [CrossRef]
- Grande, E.; Fedeli, U.; Pappagallo, M.; Crialesi, R.; Marchetti, S.; Minelli, G.; Iavarone, I.; Frova, L.; Onder, G.; Grippo, F. Variation in Cause-Specific Mortality Rates in Italy during the First Wave of the COVID-19 Pandemic: A Study Based on Nationwide Data. Int. J. Environ. Res. Public Health 2022, 19, 805. [Google Scholar] [CrossRef]
- de Nadai, M.; Roomp, K.; Lepri, B.; Oliver, N. The Impact of Control and Mitigation Strategies during the Second Wave of Coronavirus Infections in Spain and Italy. Sci. Rep. 2022, 12, 1–13. [Google Scholar] [CrossRef]
- Adorni, F.; Jesuthasan, N.; Perdixi, E.; Sojic, A.; Giacomelli, A.; Noale, M.; Trevisan, C.; Franchini, M.; Pieroni, S.; Cori, L.; et al. Epidemiology of SARS-CoV-2 Infection in Italy Using Real-World Data: Methodology and Cohort Description of the Second Phase of Web-Based EPICOVID19 Study. Int. J. Environ. Res. Public Health 2022, 19, 1274. [Google Scholar] [CrossRef]
- Altobelli, E.; Marzi, F.; Angelone, A.M.; Mazzocca, R.; Mastrodomenico, M.; Petrocelli, R.; Marziliano, C. Burden of COVID-19 and Vaccination Coverage in the Italian Population as of October 2021. Int. J. Environ. Res. Public Health 2022, 19, 496. [Google Scholar] [CrossRef]
- Signorelli, C.; Scognamiglio, T.; Odone, A. COVID-19 in Italy: Impact of Containment Measures and Prevalence Estimates of Infection in the General Population. Acta Biomerd 2020, 91, 175–179. [Google Scholar] [CrossRef]
- Gatto, M.; Bertuzzo, E.; Mari, L.; Miccoli, S.; Carraro, L.; Casagrandi, R.; Rinaldo, A. Spread and Dynamics of the COVID-19 Epidemic in Italy: Effects of Emergency Containment Measures. Proc. Natl. Acad. Sci. USA 2020, 117, 10484–10491. [Google Scholar] [CrossRef] [Green Version]
- Costantino, C.; Cannizzaro, E.; Verso, M.G.; Tramuto, F.; Maida, C.M.; Lacca, G.; Alba, D.; Cimino, L.; Conforto, A.; Cirrincione, L.; et al. SARS-CoV-2 Infection in Healthcare Professionals and General Population During “First Wave” of COVID-19 Pandemic: A Cross-Sectional Study Conducted in Sicily, Italy. Front. Public Health 2021, 9, 644008. [Google Scholar] [CrossRef]
- de Flora, S.; la Maestra, S. Growth and Decline of the COVID-19 Epidemic Wave in Italy from March to June 2020. J. Med. Virol. 2021, 93, 1613–1619. [Google Scholar] [CrossRef]
- Loconsole, D.; Centrone, F.; Morcavallo, C.; Campanella, S.; Sallustio, A.; Accogli, M.; Fortunato, F.; Parisi, A.; Chironna, M. Rapid Spread of the Sars-cov-2 Variant of Concern 202012/01 in Southern Italy (December 2020–March 2021). Int. J. Environ. Res. Public Health 2021, 18, 4766. [Google Scholar] [CrossRef]
- Borghese, L. UNLOCKING THE WORLD—One of the Italy’s Most Idyllic Islands Is “Covid-Free”. Available online: https://edition.cnn.com/travel/article/capri-covid-free-vaccination/index.html (accessed on 20 April 2022).
- Winfield, N. Italy Set to Vaccinate Small Island Populations in One Go; ABC News/Assoc. Press: New York, NY, USA, 2021; Available online: https://apnews.com/article/coronavirus-pandemic-business-lifestyle-health-europe-5421d180391a47cd2b50713b9b887375 (accessed on 20 April 2022).
- Italian Association of Municipalities from Small Islands (ANCIM). Italian Association of Municipalities from Small Islands (ANMIC): Report of the SARS-CoV-2 Vaccination Campaign, May 2021; ANCIM Rome, Italy. 2021. Available online: https://www.ancim.it/situazione-vaccini-nelle-isole-minori.htm (accessed on 31 March 2022).
- Dolci, M.; Signorini, L.; Cason, C.; Campisciano, G.; Kunderfranco, P.; Pariani, E.; Galli, C.; Petix, V.; Ferrante, P.; Delbue, S.; et al. Circulation of SARS-CoV-2 Variants among Children from November 2020 to January 2022 in Trieste (Italy). Microorganisms 2022, 10, 612. [Google Scholar] [CrossRef]
- Micheli, V.; Bracchitta, F.; Rizzo, A.; Mancon, A.; Mileto, D.; Lombardi, A.; Stefanelli, P.; Gismondo, M.R. First Identification of the New SARS-CoV-2 Omicron Variant (B.1.1.529) in Italy. Clin. Infect. Dis. 2022, Online ahead of print, ciab1044. [Google Scholar] [CrossRef]
- Antonucci, F.; Fiore, J.R.; de Feo, L.; Granato, T.; di Stefano, M.; Faleo, G.; Farhan, A.M.; Margaglione, M.; Centra, M.; Santantonio, T.A. Increased SARS-CoV-2 Seroprevalence in Healthy Blood Donors after the Second Pandemic Wave in South-Eastern Italy: Evidence for Asymptomatic Young Donors as Potential Virus Spreaders. Infect. Dis. 2022, 54, 241–246. [Google Scholar] [CrossRef]
- Chen, C.; Frey, C.B.; Presidente, G. Culture and Contagion: Individualism and Compliance with COVID-19 Policy. J. Econ. Behav. Organ. 2021, 190, 191–200. [Google Scholar] [CrossRef]
- Lu, J.G.; Jin, P.; English, A.S. Collectivism Predicts Mask Use during COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2021793118. [Google Scholar] [CrossRef]
- Porcher, S. Culture and the Quality of Government. Public Adm. Rev. 2021, 81, 333–343. [Google Scholar] [CrossRef]
- Porcher, S.; Renault, T. Social Distancing Beliefs and Human Mobility: Evidence from Twitter. PLoS ONE 2021, 16, e0246949. [Google Scholar] [CrossRef] [PubMed]
- Binns, C.; Hokama, T.; Low, W.Y. Island Health: Hope and Challenges for Public Health. Asia Pac. J. Public Health 2010, 22, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Kontodimopoulos, N.; Nanos, P.; Niakas, D. Balancing Efficiency of Health Services and Equity of Access in Remote Areas in Greece. Health Policy 2006, 76, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Núñez, A.; Sreeganga, S.D.; Ramaprasad, A. Access to Healthcare during Covid-19. Int. J. Environ. Res. Public Health 2021, 18, 2980. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.É.; Marynak, K.; Clarke, K.E.N.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; Mcmillan, H.; Wiley, J.F.; Weaver, M.D.; et al. MMWR, Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns—United States, June 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1250–1257. [Google Scholar] [CrossRef]
- Matteo Riccò Impact of Lockdown and Non-Pharmaceutical Interventions on the Epidemiology of Legionnaires’ Disease. Acta Biomed. 2022, 93, e2022090.
- Signorelli, C.; Riccò, M.; Odone, A. The Italian National Health Service Expenditure on Workplace Prevention and Safety (2006-2013): A National-Level Analysis. Ann. Di Ig. 2016, 28, 313–318. [Google Scholar] [CrossRef]
- Verelst, F.; Kuylen, E.; Beutels, P. Indications for Healthcare Surge Capacity in European Countries Facing an Exponential Increase in Coronavirus Disease (COVID-19) Cases, March 2020. Eurosurveillance 2020, 25, 2000323. [Google Scholar] [CrossRef] [Green Version]
- Morgenstern, H. Ecologic Studies in Epidemiology: Concepts, Principles, and Methods. Annu. Rev. Public Health 1995, 16, 61–62. [Google Scholar] [CrossRef]
- Roland, M.; Nolte, E. The Future Shape of Primary Care. Br. J. Gen. Pract. 2014, 64, 63–64. [Google Scholar] [CrossRef] [Green Version]
- Cohen, H.W. Limitations of an Ecological Study: A Review. Am. J. Hypertens. 2005, 18, 750. [Google Scholar] [CrossRef] [Green Version]
- Perico, L.; Tomasoni, S.; Peracchi, T.; Perna, A.; Pezzotta, A.; Remuzzi, G.; Benigni, A. COVID-19 and Lombardy: TESTing the Impact of the First Wave of the Pandemic: The Prevalence of SARS-CoV-2 Infection in Northern Italy. EBioMedicine 2020, 61, 103069. [Google Scholar] [CrossRef]
- Dessie, Z.G.; Zewotir, T. Mortality-Related Risk Factors of COVID-19: A Systematic Review and Meta-Analysis of 42 Studies and 423,117 Patients. BMC Infect. Dis. 2021, 21, 1–28. [Google Scholar] [CrossRef]




| 2015 No. (%) | 2016 No. (%) | 2017 No. (%) | 2018 No. (%) | 2019 No. (%) | 2020 No. (%) | 2021 No. (%) | Diff. 2015–2021 % | ||
|---|---|---|---|---|---|---|---|---|---|
| Italy | Total Population | 60,295,497 (100%) | 60,163,712 (100%) | 60,066,734 (100%) | 59,937,769 (100%) | 59,816,673 (100%) | 59,641,488 (100%) | 59,236,213 (100%) | −1.8% |
| Total deaths | 647,571 (100%) | 615,261 (100%) | 649,061 (100%) | 633,133 (100%) | 634,417 (100%) | 740,317 (100%) | 709,035 (100%) | +9.5% | |
| Male | 29,228,315 (48.5%) | 29,193,044 (48.5%) | 29,178,654 (48.6%) | 29,156,469 (48.6%) | 29,131,195 (48.7%) | 29,050,096 (48.7%) | 28,866,226 (48.7%) | −1.2% | |
| Female | 31,067,182 (51.5%) | 30.970,668 (51.5%) | 30,888,080 (51.4%) | 30,781,300 (51.4%) | 30,685,478 (51.3%) | 30,591,392 (51.3%) | 30,369,987 (51.3%) | −2.2% | |
| <20 years | 11,172,613 (18.5%) | 11,086,243 (18.4%) | 10,986,232 (18.3%) | 10,882,099 (18.2%) | 10,745,563 (18.0%) | 10,598,610 (17.8%) | 10,493,558 (17.7%) | −6.1% | |
| 20–39 years | 14,033,525 (23.3%) | 13,730,145 (22.8%) | 13,483,326 (22.4%) | 13,282,229 (22.2%) | 13,113,139 (21.9%) | 12,939,014 (21.7%) | 12,712,317 (21.5%) | −9.4% | |
| 40–59 years | 18,295,227 (30.3%) | 18,401,053 (30.6%) | 18,454,245 (30.7%) | 18,457,834 (30.8%) | 18,445,702 (30.8%) | 18,351,424 (30.8%) | 18,142,711 (30.6%) | −0.8% | |
| 60–79 years | 12,837,919 (21.3%) | 12,919,210 (21.5%) | 13,036,923 (21.7%) | 13,136,844 (21.9%) | 13,215,981 (22.1%) | 13,332,737 (22.4%) | 13,408,810 (22.6%) | +4.4% | |
| ≥ 80 years | 3,956,213 (6.6%) | 4,027,061 (6.7%) | 4,106,008 (6.8%) | 4,178,763 (7.0%) | 4,296,288 (7.2%) | 4,419,703 (7.4%) | 4,478,817 (7.6%) | +13.2% | |
| Small Islands | Total population | 218,008 (0.4%) | 217,391 (0.4%) | 216,899 (0.4%) | 216,569 (0.4%) | 215,841 (0.4%) | 215,200 (0.4%) | 213,093 (0.4%) | −2.3% |
| Total deaths | 2206 (0.3%) | 2115 (0.3%) | 2224 (0.3%) | 2250 (0.4%) | 2118 (0.3%) | 2247 (0.3%) | 2409 (0.3%) | +9.2% | |
| Male | 108,251 (49.7%) | 108,125 (49.7%) | 107,888 (49.7%) | 107,686 (49.7%) | 107,427 (49.7%) | 107,080 (49.8%) | 105,823 (49.7%) | −2.2% | |
| Female | 109,757 (50.3%) | 109,266 (50.3%) | 109,011 (50.3%) | 108,883 (50.3%) | 108,414 (50.3%) | 108,120 (50.3%) | 107,270 (50.3%) | −2.3% | |
| <20 years | 38,637 (17.7%) | 38,066 (17.5%) | 37,526 (17.3%) | 36,998 (17.1%) | 36,324 (16.8%) | 35,067 (16.3%) | 35,283 (16.6%) | −9.5% | |
| 20–39 years | 52,405 (24.0%) | 51,227 (23.6%) | 50,028 (23.1%) | 49,183 (22.7%) | 48,227 (22.3%) | 47,375 (22.0%) | 45,474 (21.3%) | −15.4% | |
| 40–59 years | 67,150 (30.8%) | 67,530 (31.1%) | 67,774 (31.2%) | 67,797 (31.3%) | 67,759 (31.4%) | 67,477 (31.5%) | 66,538 (31.2%) | −0.9% | |
| 60–79 years | 47,590 (21.8%) | 47,979 (22.1%) | 48,604 (22.4%) | 49,241 (22.7%) | 49,806 (23.1%) | 50,618 (23.5%) | 51,034 (23.9%) | +6.7% | |
| ≥ 80 years | 12,226 (5.6%) | 12,589 (5.8%) | 12,967 (6.0%) | 13,350 (6.1%) | 13,725 (6.4%) | 14,148 (6.6%) | 14,663 (6.9%) | +16.6% |
| Province (Region) | County | Mortality Rates (Deaths per 100 Persons, [95% Confidence Intervals]) | ||
|---|---|---|---|---|
| 2015–2019 | 2020 | 2021 | ||
| Foggia (Apulia) | Isole Tremiti | 1.035 [0.657; 1.548] | 0.891 [0.243; 2.265] | 0.883 [0.241; 2.245] |
| Naples (Campania) | Anacapri | 0.923 [0.823; 1.031] | 0.906 [0.697; 1.158] | 1.188 [0.946; 1.473] |
| Barano d’Ischia | 0.825 [0.747; 0.908] | 0.708 [0.553; 0.892] | 0.893 [0.717; 1.099] | |
| Capri | 1.107 [0.999; 1.225] | 1.164 [0.927; 1.443] | 1.287 [1.035; 1.581] | |
| Casamicciola Terme | 0.902 [0.811; 1.000] | 0.805 [0.621; 1.027] | 0.813 [0.625; 1.039] | |
| Forio | 0.834 [0.773; 0.898 | 0.804 [0.677; 0.948] | 0.926 [0.789; 1.079] | |
| Ischia | 0.945 [0.888; 1.013] | 0.967 [0.834; 1.115] | 1.048 [0.910; 1.200] | |
| Lacco Ameno | 0.927 [0.807; 1.059] | 0.928 [0.675; 1.244] | 1.140 [0.855; 1.489] | |
| Procida | 1.174 [1.083; 1.272] | 1.010 [0.826; 1.223] | 1.289 [1.079; 1.528] | |
| Serrara Fontana | 1.094 [0.932; 1.272] | 0.941 [0.631; 1.348] | 1.156 [0.807; 1.604] | |
| Latina (Latium) | Ponza | 1.245 [1.083; 1.435] | 0.969 [0.664; 1.366] | 1.119 [0.789; 1.539] |
| Ventotene | 1.097 [0.777; 1.502] | 1.255 [0.578; 2.369] | 1.637 [0.868; 2.905] | |
| La Spezia (Liguria) | Porto Venere | 1.767 [1.577; 1.973] | 1.539 [1.151; 2.013] | 1.621 [1.220; 2.110] |
| Sassari (Sardinia) | La Maddalena | 1.033 [0.950; 1.122] | 0.957 [0.783; 1.159] | 1.237 [1.036; 1.465] |
| Porto Torres | 1.767 [1.577; 1.973] | 1.166 [1.027; 1.318] | 0.935 [0.810; 1.074] | |
| South Sardinia (Sardinia) | Calasetta | 1.214 [1.041; 1.408] | 1.348 [0.956; 1.846] | 1.581 [1.151; 2.117] |
| Carloforte | 1.460 [1.328; 1.602] | 1.487 [1.196; 1.826] | 1.376 [1.096; 1.705] | |
| Sant’Antioco | 1.263 [1.172; 1.360] | 1.402 [1.189; 1.641] | 1.317 [1.110; 1.552] | |
| Agrigento (Sicily) | Lampedusa e Linosa | 0.781 [0.687; 0.884] | 0.566 [0.397; 0.783] | 0.836 [0.627; 1.093] |
| Messina (Sicily) | Lipari | 0.950 [0.874; 1.031] | 0.942 [0.780; 1.128] | 1.069 [0.895; 1.266] |
| Leni | 1.054 [0.735; 1.463] | 1.175 [0.509; 2.302] | 1.022 [0.412; 2.094] | |
| Malfa | 1.197 [0.906; 1.552] | 1.005 [0.483; 1.841] | 1.022 [0.491; 1.870] | |
| Santa Marina Salina | 1.196 [0.892; 1.569] | 1.634 [0.890; 2.726] | 1.291 [0.646; 2.298] | |
| Palermo (Sicily) | Ustica | 1.138 [0.896; 1.424] | 1.387 [0.824; 2.183] | 0.938 [0.485; 1.632] |
| Trapani (Sicily) | Favignana | 1.197 [1.055; 1.353] | 1.397 [1.068; 1.759] | 1.629 [1.274; 2.050] |
| Pantelleria | 1.197 [1.088; 1.314] | 1.371 [1.119; 1.662] | 1.412 [1.155; 1.708] | |
| Grosseto (Tuscany) | Isola del Giglio | 1.399 [1.133; 1.707] | 1.620 [1.018; 2.443] | 1.866 [1.211; 2.742] |
| Livorno (Tuscany) | Campo nell’Elba | 1.133 [0.999; 1.280] | 1.246 [0.948; 1.608] | 1.151 [0.866; 1.499] |
| Capoliveri | 1.009 [0.869; 1.166] | 0.897 [0.629; 1.240] | 1.210 [0.890; 1.606] | |
| Capraia | 1.226 [0.787; 1.818] | 0.761 [0.157; 2.209] | 1.042 [0.285; 2.646] | |
| Marciana | 1.604 [1.371; 1.865] | 1.288 [0.851; 1.869] | 1.904 [1.358; 2.594] | |
| Marciana Marina | 1.415 [1.186; 1.675] | 1.047 [0.640; 1.612] | 1.543 [1.035; 2.208] | |
| Portoferraio | 1.186 [1.099; 1.278] | 0.941 [0.775; 1.131] | 1.168 [0.983; 1.378] | |
| Porto Azzurro | 0.934 [0.792; 1.094] | 1.014 [0.715; 1.395] | 0.948 [0.661; 1.316] | |
| Rio | 1.352 [1.178; 1.544] | 1.457 [1.080; 1.922] | 1.197 [0.857; 1.627] | |
| POOLED | 1.105 [1.034; 1.181] | 1.069 [0.983; 1.164] | 1.180 [1.098; 1.269] | |
| Province (Region) | County | Risk Ratio [95% Confidence Intervals] | |
|---|---|---|---|
| 2020 | 2021 | ||
| Foggia (Apulia) | Isole Tremiti | 0.861 [0.299; 2.478] | 0.853 [0.297; 2.456] |
| Naples (Campania) | Anacapri | 0.982 [0.750; 1.286] | 1.288 [1.011; 1.640] |
| Barano d’Ischia | 0.859 [0.668; 1.104] | 1.082 [0.861; 1.361] | |
| Capri | 1.052 [0.829; 1.334] | 1.162 [0.924; 1.462] | |
| Casamicciola Terme | 0.893 [0.685; 1.164] | 0.901 [0.690; 1.177] | |
| Forio | 0.965 [0.805; 1.155] | 1.111 [0.936; 1.318] | |
| Ischia | 1.019 [0.871; 1.192] | 1.104 [0.949; 1.284] | |
| Lacco Ameno | 1.002 [0.725; 1.383] | 1.231 [0.912; 1.660] | |
| Procida | 0.860 [0.699; 1.058] | 1.098 [0.910; 1.325] | |
| Serrara Fontana | 0.860 [0.581; 1.274] | 1.057 [0.736; 1.519] | |
| Latina (Latium) | Ponza | 0.776 [0.535; 1.126] | 0.896 [0.632; 1.271] |
| Ventotene | 1.145 [0.560; 2.356] | 1.526 [0.802; 2.906] | |
| La Spezia (Liguria) | Porto Venere | 0.871 [0.651; 1.165] | 0.917 [0.689; 1.222] |
| Sassari (Sardinia) | La Maddalena | 0.927 [0.752; 1.141] | 1.197 [0.991; 1.445] |
| Porto Torres | 1.405 [1.223; 1.615] | 1.128 [0.968; 1.314] | |
| South Sardinia (Sardinia) | Calasetta | 1.110 [0.783; 1.574] | 1.302 [0.938; 1.809] |
| Carloforte | 1.018 [0.812; 1.276] | 0.942 [0.746; 1.191] | |
| Sant’Antioco | 1.110 [0.932; 1.321] | 1.043 [0.871; 1.248] | |
| Agrigento (Sicily) | Lampedusa e Linosa | 0.725 [0.511; 1.027] | 1.071 [0.797; 1.439] |
| Messina (Sicily) | Lipari | 0.992 [0.814; 1.210] | 1.125 [0.932; 1.359] |
| Leni | 1.114 [0.519; 2.391] | 0.969 [0.432; 2.173] | |
| Malfa | 0.840 [0.430; 1.640] | 0.853 [0.437; 1.666] | |
| Santa Marina Salina | 1.366 [0.760; 2.457] | 1.080 [0.565; 2.063] | |
| Palermo (Sicily) | Ustica | 1.219 [0.731; 2.032] | 0.824 [0.449; 1.511] |
| Trapani (Sicily) | Favignana | 1.167 [0.883; 1.544] | 1.361 [1.048; 1.767] |
| Pantelleria | 1.145 [0.925; 1.419] | 1.180 [0.954; 1.459] | |
| Grosseto (Tuscany) | Isola del Giglio | 1.158 [0.731; 1.835] | 1.334 [0.862; 2.065] |
| Livorno (Tuscany) | Campo nell’Elba | 1.100 [0.829; 1.460] | 1.016 [0.759; 1.360] |
| Capoliveri | 0.890 [0.623; 1.269] | 1.199 [0.872; 1.649] | |
| Capraia | 0.621 [0.188; 2.053] | 0.850 [0.296; 2.435] | |
| Marciana | 0.803 [0.536; 1.203] | 1.187 [0.840; 1.677] | |
| Marciana Marina | 0.740 [0.463; 1.180] | 1.090 [0.732; 1.624] | |
| Portoferraio | 0.793 [0.650; 0.968] | 0.985 [0.822; 1.181] | |
| Porto Azzurro | 1.085 [0.759; 1.552] | 1.015 [0.704; 1.463] | |
| Rio | 1.078 [0.792; 1.466] | 0.885 [0.633; 1.238] | |
| TOTAL | 0.992 [0.933; 1.056] | 1.096 [1.049; 1.145] | |
| Province | Risk Ratio [95% Confidence Intervals] | |
|---|---|---|
| 2020 | 2021 | |
| La Spezia | 0.731 [0.569; 0.938] | 0.828 [0.648; 1.057] |
| Livorno | 0.875 [0.792; 0.966] | 1.010 [0.921; 1.108] |
| Grosseto | 1.087 [0.753; 1.570] | 1.287 [0.918; 1.805] |
| La Latina | 0.802 [0.607; 1.060] | 0.929 [0.724; 1.193] |
| Napoli | 0.898 [0.842; 0.956] | 1.004 [0.947; 1.064] |
| Trapani | 1.136 [0.991; 1.303] | 1.139 [1.000; 1.298] |
| Palermo | 1.102 [0.737; 1.649] | 0.713 [0.424; 1.197] |
| Messina | 1.037 [0.898; 1.198] | 1.026 [0.894; 1.177] |
| Agrigento | 0.703 [0.519; 0.951] | 0.935 [0.736; 1.188] |
| Sassari | 1.039 [0.946; 1.141] | 1.014 [0.919; 1.118] |
| South Sardinia | 0.946 [0.849; 1.053] | 0.877 [0.785; 0.979] |
| Foggia | 0.721 [0.296; 1.756] | 0.731 [0.300; 1.782] |
| Total | 0.939 [0.868; 1.756] | 0.992 [0.943; 1.044] |
| β | B | SE | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Constant | 14.931 | 1.031 | 12.886; 16.940 | <0.001 | |
| COVID-19 notification rates in parent province | 0.469 | 0.882 | 0.168 | 0.551; 1.212 | <0.001 |
| COVID-19 related mortality in parent province | 22.768 | 8.385 | 0.294 | 6.285; 39.250 | 0.007 |
| COVID-19 related admissions in parent province | −11.208 | 3.278 | −0.430 | −17.651; −4.765 | 0.001 |
| COVID-19 related admissions to ICUs in parent province | −59.700 | 19.710 | −0.288 | −98.444; −20.956 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riccò, M.; Ferraro, P.; Peruzzi, S.; Zaniboni, A.; Satta, E.; Ranzieri, S. Excess Mortality on Italian Small Islands during the SARS-CoV-2 Pandemic: An Ecological Study. Infect. Dis. Rep. 2022, 14, 391-412. https://doi.org/10.3390/idr14030043
Riccò M, Ferraro P, Peruzzi S, Zaniboni A, Satta E, Ranzieri S. Excess Mortality on Italian Small Islands during the SARS-CoV-2 Pandemic: An Ecological Study. Infectious Disease Reports. 2022; 14(3):391-412. https://doi.org/10.3390/idr14030043
Chicago/Turabian StyleRiccò, Matteo, Pietro Ferraro, Simona Peruzzi, Alessandro Zaniboni, Elia Satta, and Silvia Ranzieri. 2022. "Excess Mortality on Italian Small Islands during the SARS-CoV-2 Pandemic: An Ecological Study" Infectious Disease Reports 14, no. 3: 391-412. https://doi.org/10.3390/idr14030043








