Abstract
Respiratory syncytial virus (RSV) is an important cause of severe respiratory disease in older adults. Understanding the disease burden is crucial for guiding vaccination policy and raising disease awareness. We estimated the burden of RSV hospitalizations and deaths in adults in five middle-income countries: Argentina, Brazil, Chile, Mexico, and Malaysia. Hospital discharge and death statistics due to any respiratory disease (ICD-10 codes: J00–99) from 2010 to 2022 were obtained. The RSV attributable burden on hospitalizations and deaths by age group was determined for 2019 using previously published estimates. Latin American countries showed distinct annual peaks in respiratory-related hospitalizations and deaths during winter months that were absent in Malaysia. Among ≥20-year-olds in 2019, there were 14,604 RSV-attributable hospitalizations nationally in Argentina, 44,323 in Brazil, 4529 in Chile, 7416 in Malaysia, and 8651 in Mexico, and 60–74% in ≥65-year-olds. There were also 3518 RSV-attributable deaths in Argentina, 9115 in Brazil, 801 in Chile, 704 in Malaysia, and 3806 in Mexico 79–88% in ≥65-year-olds. Incidences of RSV-attributable hospitalizations in ≥75-year-olds ranged between 256.3 and 294.3 per 100,000 population, and deaths between 33.6 and 112.9 per 100,000 population. RSV is associated with a substantial disease burden beyond pediatric age groups, and preventive vaccines could have a major impact on this burden, especially in older adults.
1. Introduction
Respiratory syncytial virus (RSV) is a common cause of severe respiratory disease in children and older adults. The risk of severe disease in adults is strongly age-dependent, with the highest hospitalization and mortality observed in adults over the age of 65 years [1,2]. In industrialized countries, the incidence of hospitalization for RSV in adults ≥65 years of age is 157 per 100,000 person-years, with an in-hospital fatality rate of 6.1% [3]. Risk factors for severe RSV disease are comorbid chronic or immunocompromising diseases [4,5,6]. Under-recognition is a significant issue due to symptom overlap with other viral infections [3], lack of awareness, and infrequent or delayed virology testing. Currently there is no specific therapy for RSV; therefore, there is a perception that a viral diagnosis will have no impact on the clinical management of cases. This leads to under-recognition and under-estimation of the disease burden.
The first RSV vaccines were approved in 2023 for the prevention of lower respiratory tract disease caused by RSV in adults 60 years of age and older [7,8]. Vaccine acceptance and high uptake will be contingent upon improving disease awareness amongst healthcare providers and the general public. In this regard, estimates of the disease burden will help to guide policy development by health authorities.
In high-income countries, a significant proportion of the severe RSV burden occurs in older adults, who account for 92% of RSV-associated hospitalizations and most deaths [9,10]. A modelling study conducted in the United Kingdom (UK) using national health data sources including laboratory results of viral testing, found that the burden of RSV was comparable to influenza in terms of general practitioner episodes (consultations), hospitalizations and deaths in adults aged ≥65 years [11]. Much less is known about the RSV disease burden in adults living in middle-income and low-income countries, although the available evidence points to a similar concentration of the burden in older adults [12,13,14]. The Global Burden of Disease Study reports higher attributable incidences of RSV than Influenza, as well as a higher burden of low respiratory tract infections in older adults than in pediatric populations in these countries [15,16].
We aimed to estimate the RSV burden in adults living in five middle-income countries using national hospital discharge and death statistics for any respiratory diseases (ICD-10 codes: J00–J99) available publicly or by request under information transparency law. In the absence of detailed RSV proportions by age and disease type in the analyzed countries, we used the attributable risk of RSV reported by Fleming et al. [11] for the UK to estimate the RSV burden.
A plain language statement is provided at the end of this article. An interactive graphical abstract is available as supplementary material (File S1).
2. Materials and Methods
2.1. Data Sources
Aggregate hospital discharge data and death certificate information for Argentina and Chile were requested from the respective Ministries of Health under data-sharing Transparency Laws. In Chile, the Ministry of Health database captures data for 100% of the population. In Argentina, the Hospital Discharge database covers only the hospitals in the public health sector (assisting approximately 36% of the population) [17], and the death certificate database captures all deaths in the country. Missing hospital discharge data observed during certain study years were supplemented as previously described and explained in the Supplement [18].
Similarly, the Brazilian Hospital Discharge database only captures information from hospitals in the public health system (assisting approximately 76.7% of the population) [19]. The death certificate database captures all deaths in the country. Data were obtained from the Unified Brazilian Health System (DATASUS) Hospital Morbidity Database and Mortality Information System [20].
In Mexico, the Mexican public health system covers approximately 80% of the population [21]. Hospital discharge and death certificate data were obtained from System of the Dynamic Analysis of Information (Cubos Dinamicos) from the Ministry of Health [22].
Hospital discharges and deaths data for Malaysia were obtained from the Malaysian Health Informatics Center (Pusat Informatik Kesihatan) operated by the planning division of the Ministry of Health, which captures data for 100% of the population [23].
Population data were obtained from official sources in each country [24,25,26,27,28].
The study used public and anonymous aggregate data. Ethics approval and patient consent were not applicable for this research and thus were not obtained.
2.2. Outcomes
The monthly number of hospital discharges and deaths with a primary diagnosis classified by International Classification of Diseases version 10 codes as any respiratory disease (ICD-10 codes: J00–J99) and age group were identified between January 2010 and December 2022. RSV-specific disease codes were not used for case identification because of the low rates of virological testing in middle-income countries.
Country data from 2019 were selected for the analysis of the RSV burden in order to have the latest available data prior to the coronavirus disease 2019 (COVID-19) pandemic. Data are presented for the following age group strata: 20–49 years, 50–64 years, 65–74 years, and ≥75 years, except for Chile, where data were available for adults aged 18–49 years instead of 20–49 years.
2.3. Statistical Analysis
Crude monthly incidences of hospitalization and monthly mortality due to any respiratory disease were calculated by age group from the national data sets using annual population estimates adjusted for the proportion of residents covered in the hospital discharges and deaths databases. The age-specific RSV attributable risk from any respiratory disease was derived from the modelling study of the RSV burden conducted in the UK and reported by Fleming et al., 2015 (Table 1) [11], who reported the RSV attributable risk by age group, by disease outcome (medical visit, hospitalization and death) and by certain ICD-10 code groups. The study by Fleming et al. 2015 was selected because of the robustness of the analysis and level of detail of the RSV data provided. Although the published study reported only a point estimate of different RSV attributable risks, we computed upper and lower levels of all attributable risks from other data reported in the same study. Fleming et al. 2015 reported RSV-attributable risks were applied to national hospitalization and death data considering similar age groups, health outcomes (hospitalization or death) and ICD-10 codes (codes for all respiratory diseases were considered, J00–J99) to estimate RSV burden in the five middle-income countries of interest.

Table 1.
RSV-attributable risk in adult populations reported by outcome, age group, and ICD-10 codes for the United Kingdom. Data from Fleming et al., 2015 [11].
Analyses were performed using Microsoft Excel for Microsoft 365 MSO (Version 2308; Microsoft Corporation, Redmond, WA, USA).
3. Results
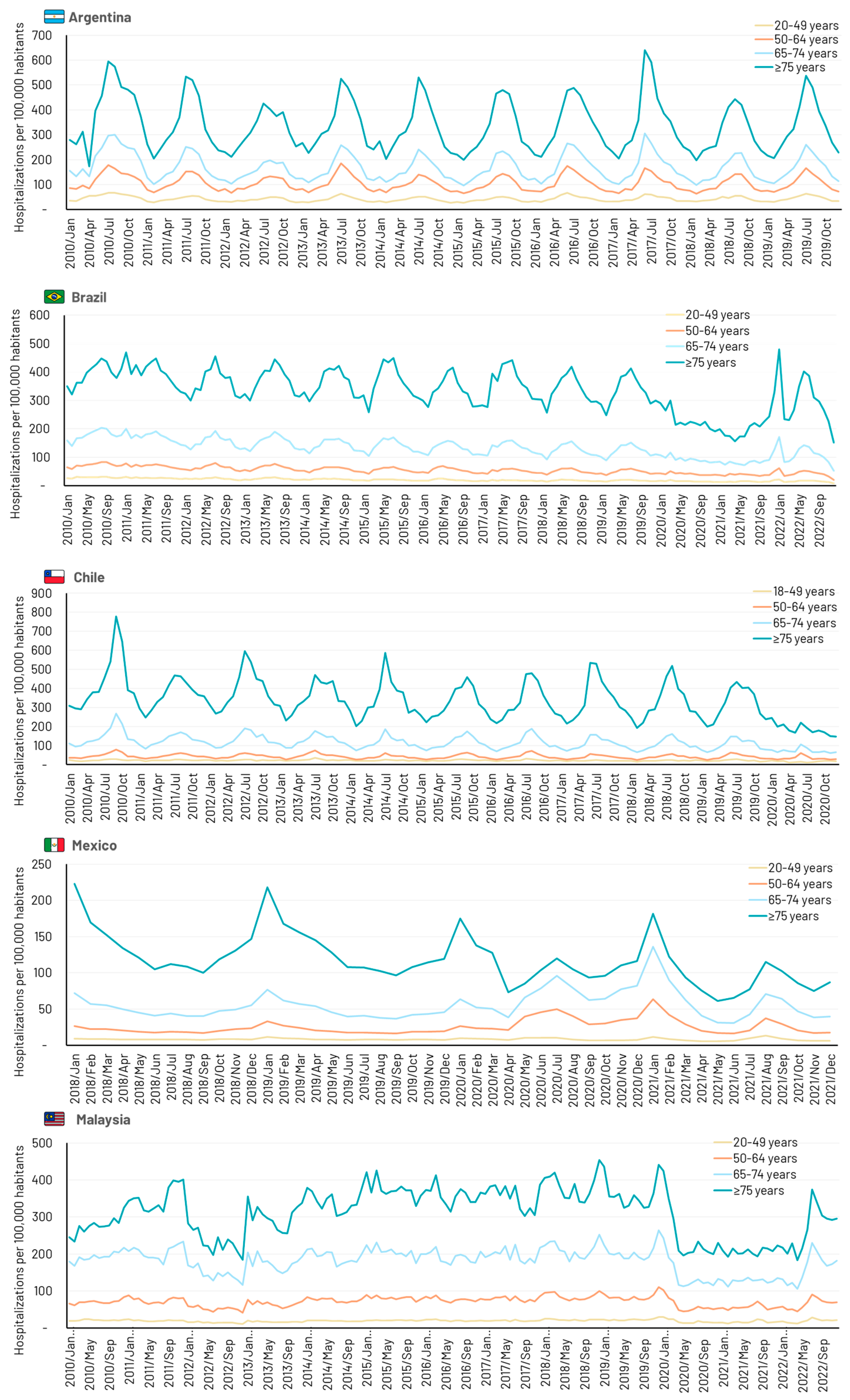
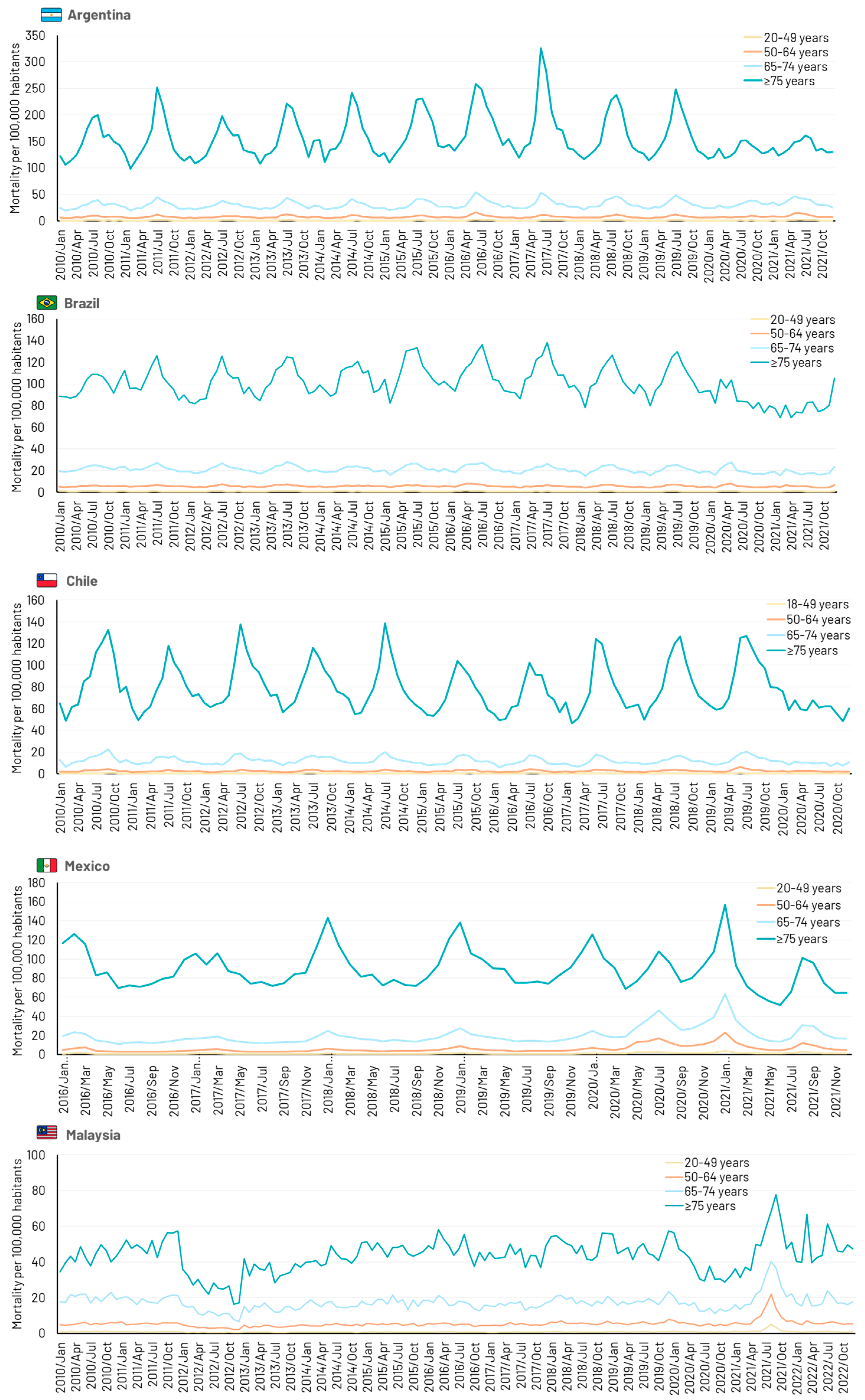
All four Latin American countries showed distinct annual peaks in respiratory-related hospitalizations and deaths during northern or southern hemisphere winter months (Figure 1). Cyclical activity was absent in Malaysia where similar incidences of respiratory hospitalizations occurred all year round. The impact of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic is evident in countries with data extending through 2020, with marked decreases in hospitalizations reflecting the impact of lockdowns and social distancing. Deaths due to respiratory disease also decreased during the pandemic period, except in Malaysia, where a sharp increase in deaths was observed from mid-2021 in all age groups (Figure 2).
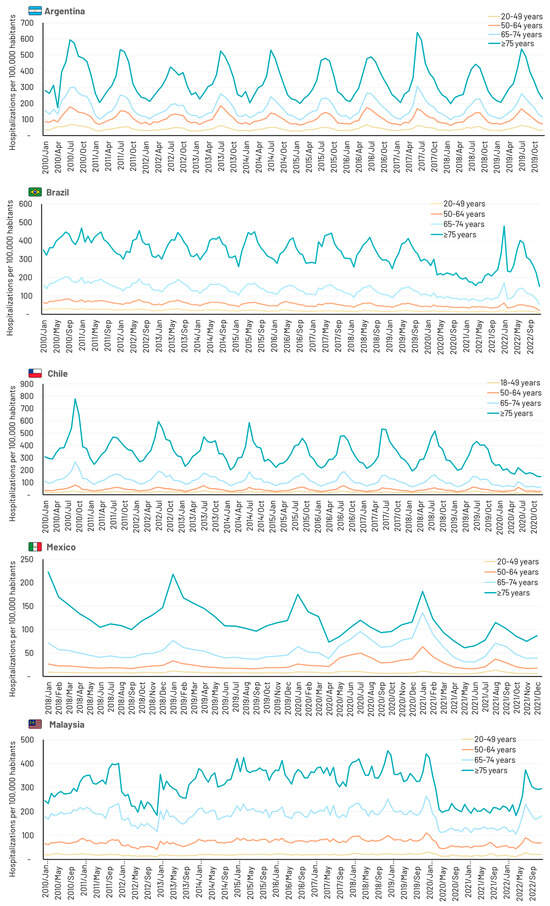
Figure 1.
Time series showing monthly hospitalizations due to any respiratory disease (J00–J99) in five middle-income countries.
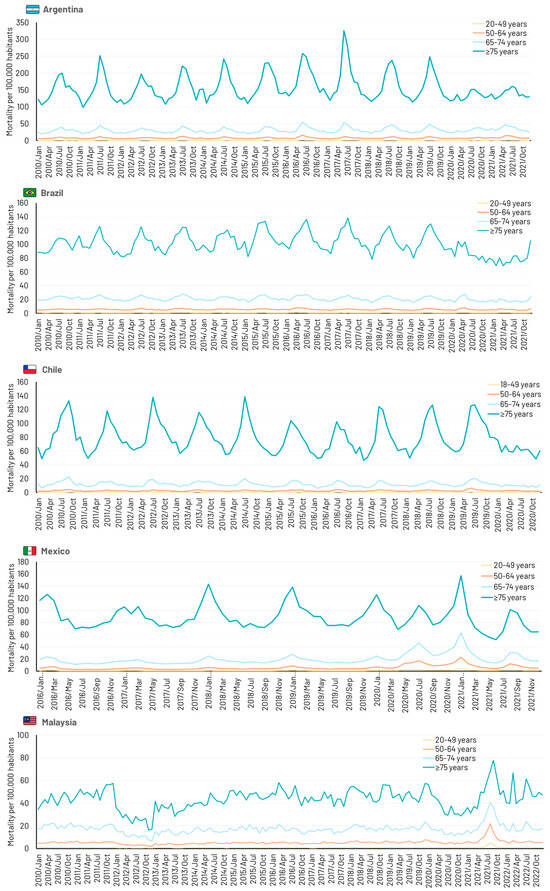
Figure 2.
Time series showing monthly deaths due to any respiratory disease (J00–J99) in five middle-income countries.
3.1. Argentina
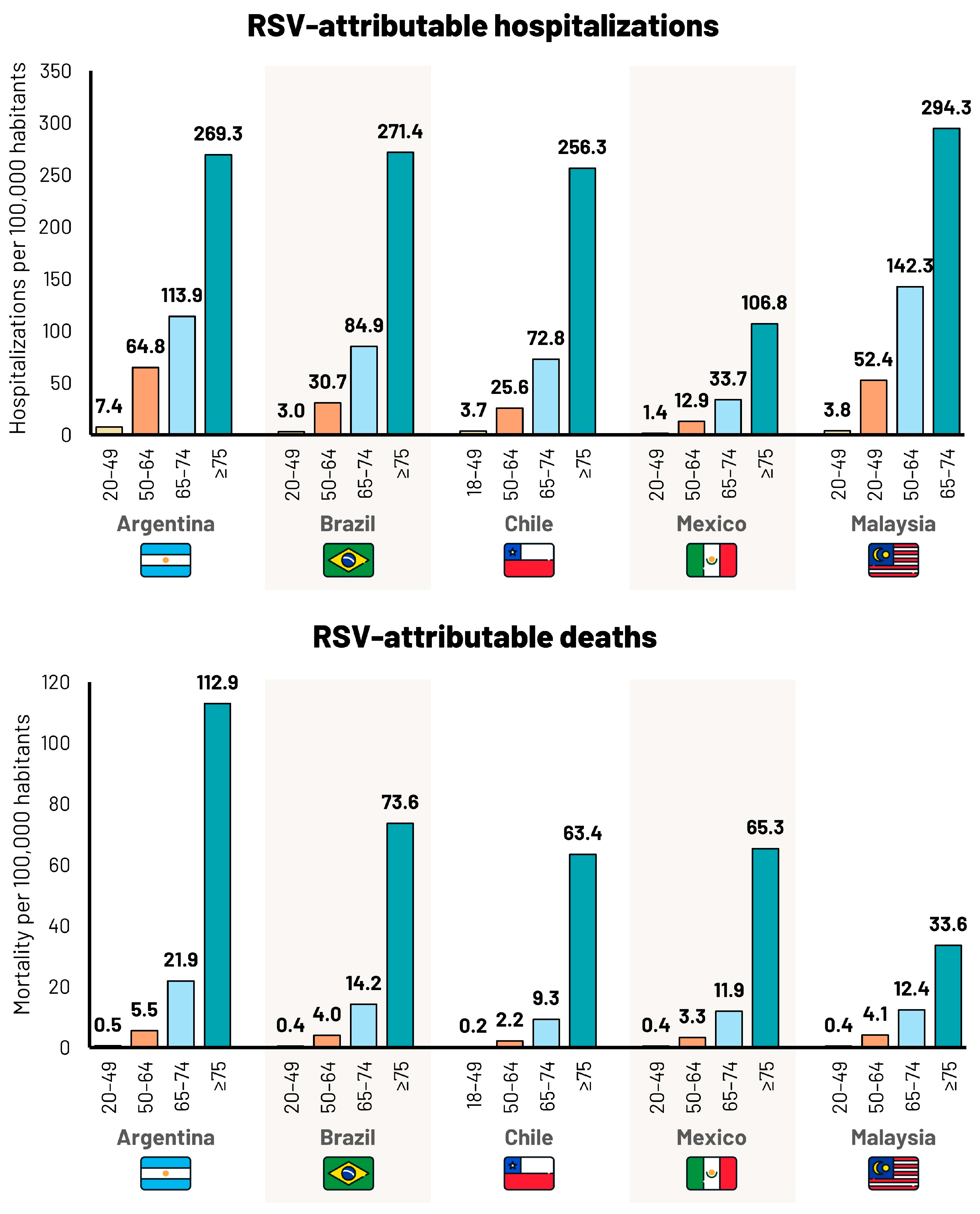
There were 1,073,139 hospital discharges with a primary diagnosis of any respiratory disease between 2010 and 2019 in the Argentinian Public Health sector (Table S1). The overall incidences per 100,000 population were 508 in 20–49-year-olds, 1257 in 50–64-year-olds, 2007 in 65–74-year-olds, and 4042 in ≥75-year-olds. Incidences tended to remain stable over the study period in all age groups. In 2019, the estimated number of hospitalizations attributed to RSV extrapolated to the total population was 14,604 (lower limit [LL] 11,205; upper limit [UL] 18,269), of which 63% were in ≥65-year-olds (Table 2). The incidence of hospitalizations attributed to RSV increased with age, from 7.4 per 100,000 population (LL 6.6; UL 11.1) in 20–49-year-olds, to 269.3 per 100,000 population (LL 207.4; UL 335.4) in ≥75-year-olds (Table 2, Figure 3).

Table 2.
Incidence of hospitalizations due to any respiratory disease (J00–J99) and the RSV-attributable portion, by age group (years) and country (2019 data).
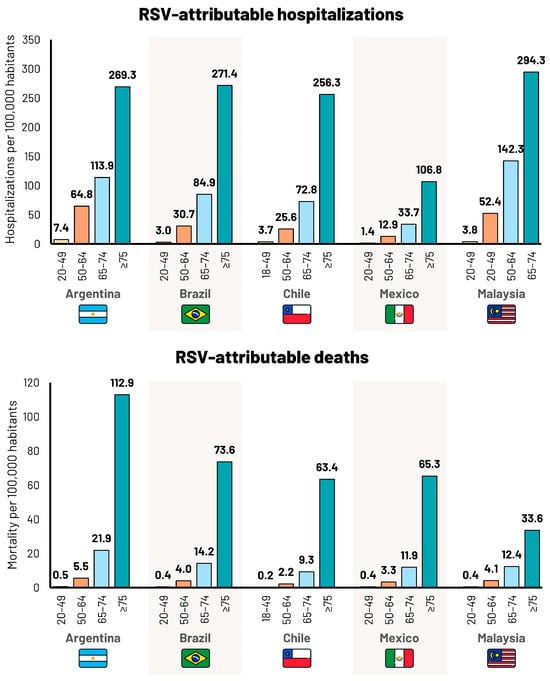
Figure 3.
Incidence per 100,000 population of RSV-attributable hospitalizations and deaths per 100,000 population, by age group (years) and country (2019 data).
There were 669,185 deaths due to any respiratory disease between 2010 and 2021 in Argentina, of which, 86% occurred in ≥65-year-olds, with an incidence of 84.6 per 100,000 (Table S2). In 2019, the estimated number of deaths attributed to RSV was 3518 (LL 2448; UL 4683), of which, 88% were ≥65-year-olds (Table 3). The incidence of deaths attributed to RSV increased with age from 0.5 per 100,000 population (LL 0.0; UL 1.1) in 20–49-year-olds, to 112.9 per 100,000 population (LL 78.8; UL 155.4) in ≥75-year-olds (Table 3, Figure 3).

Table 3.
Mortality due to any respiratory disease (J00–J99) and RSV-attributable portion by age group (years) and country (2019 data).
3.2. Brazil
There were 8,708,898 hospital discharges with a primary diagnosis of any respiratory disease between 2010 and 2022 in the Brazilian public health sector (Table S1). The overall incidences per 100,000 population were 244 in 20–49-year-olds, 643 in 50–64-year-olds, 1563 in 65–74-year-olds, and 3940 in ≥75-year-olds. Incidences tended to remain stable over the study period. In 2019, the estimated number of hospitalizations attributed to RSV extrapolated to the total population was 44,323 (LL 33,857; UL 55,108), of which 71% were in ≥65-year-olds (Table 2). The incidence of hospitalizations attributed to RSV increased with age, from 3.0 per 100,000 population (LL 2.7; UL 4.5) in 20–49-year-olds to 271.4 per 100,000 population (LL 209.1; UL 338.0) in ≥75-year-olds (Table 2, Figure 3).
There were 1,675,021 deaths due to respiratory disease between 2010 and 2021 in Brazil. The overall incidences per 100,000 population were 10 in 20–49-year-olds, 68 in 50–64-year-olds, 252 in 65–74-year-olds, and 1201 in ≥75-year-olds (Table S2). In 2019, the estimated number of deaths attributed to RSV was 9115 (LL 6284; UL 12,129), of which, 82% were ≥65-year-olds (Table 3). The incidence of deaths attributed to RSV increased with age from 0.4 per 100,000 population (LL 0.0; UL 0.9) in 20–49-year-olds to 73.6 per 100,000 population (LL 51.4; UL 101.3) in ≥75-year-olds (Table 3, Figure 3).
3.3. Chile
There were 949,066 hospital discharges with a primary diagnosis of any respiratory disease between 2010 and 2020 in Chile (Table S1). The overall incidences per 100,000 population were 270 in 18–49-year-olds, 510 in 50–64-year-olds, 1367 in 65–74-year-olds, and 3980 in ≥75-year-olds. Incidences tended to decrease in all age groups over the study period. In 2019, the estimated number of hospitalizations attributed to RSV was 4529 (LL 3472; UL 5650), of which, 74% were ≥65-year-olds (Table 2). The incidence of hospitalizations attributed to RSV increased with age, from 3.7 per 100,000 population (LL 3.4; UL 5.6) in 18–49-year-olds to 256.3 per 100,000 population (LL 197.5; UL 319.2) in ≥75-year-olds (Table 2, Figure 3).
There were 115,865 deaths due to respiratory disease between 2010 and 2020 in Chile. The overall incidences per 100,000 population were in 18–49-year-olds, 31 in 50–64-year-olds, 144 in 65–74-year-olds, and 944 in ≥75-year-olds (Table S2). In 2019, the estimated number of deaths attributed to RSV was 801 (LL 559, UL 1070), of which, 89% were ≥65-year-olds (Table 3). The incidence of deaths attributed to RSV increased with age from 0.2 per 100,000 population (LL 0.0; UL 0.4) in 18–49-year-olds to 63.4 per 100,000 population (LL 44.2; UL 87.2) in ≥75-year-olds (Table 3, Figure 3).
3.4. Mexico
There were 630,082 hospital discharges with a primary diagnosis of any respiratory disease between 2018 and 2021 in Mexico (Table S1). The overall incidences per 100,000 population were 97 in 20–49-year-olds, 307 in 50–64-year-olds, 672 in 65–74-year-olds, and 141 in ≥75-year-olds, and tended to be stable over the study period. After analyzing the hospital discharge data obtained from official sources in Mexico, we concluded cases of any respiratory disease were most probably underreported. In 2019, the estimated number of hospitalizations attributed to RSV extrapolated to the total population was 8651 (LL 6638; UL 10,814), of which, 66% were ≥65-year-olds (Table 2). The incidence of hospitalizations attributed to RSV increased with age, from 1.4 per 100,000 population (LL 1.2; UL 2.1) in 20–49-year-olds to 106.8 per 100,000 population (LL 82.3; UL 133.1) in ≥75-year-olds (Table 2, Figure 3).
There were 422,873 deaths due to respiratory disease between 2016 and 2021 in Mexico. The overall incidences per 100,000 population were 13 in 20–49-year-olds, 73 in 50–64-year-olds, 243 in 65–74-year-olds, and 1069 in ≥75-year-olds (Table S2). There was a trend toward an increase in the incidence of respiratory deaths over time. In 2019, the estimated number of deaths attributed to RSV was 3806 (LL 2571; UL 5130), of which, 79% were ≥65-year-olds (Table 3). The incidence of deaths attributed to RSV increased with age from 0.4 per 100,000 population (LL 0.0; UL 0.9) in 20–49-year-olds to 65.3 per 100,000 population (LL 45.6; UL 89.9) in ≥75-year-olds (Table 3, Figure 3).
3.5. Malaysia
There were 1,230,600 hospital discharges with a primary diagnosis of any respiratory disease between 2010 and 2022 in Malaysia (Table S1). The overall incidences per 100,000 population were 235 in 20–49-year-olds, 901 in 50–64-year-olds, 2321 in 65–74-year-olds, and 4054 in ≥75-year-olds. There was considerable variation in incidence from year to year over the study period. In 2019, the estimated number of hospitalizations attributed to RSV was 7416 (LL 5645; UL 9208), of which, 60% were ≥65-year-olds (Table 2). The incidence of hospitalizations attributed to RSV increased with age, from 3.8 per 100,000 population (LL 3.4; UL 5.7) in 20–49-year-olds to 294.3 per 100,000 population (LL 226.7; UL 366.5) in ≥75-year-olds (Table 2, Figure 3).
There were 137,248 deaths due to respiratory disease between 2010 and 2022 in Malaysia. The overall incidences per 100,000 population were 10 in 20–49-year-olds, 66 in 50–64-year-olds, 209 in 65–74-year-olds, and 530 in ≥75-year-olds (Table S2). In 2019, the estimated number of deaths attributed to RSV was 704 (LL 468, UL 931), of which, 63% were ≥65-year-olds (Table 3). The incidence of deaths attributed to RSV increased with age from 0.4 per 100,000 population (LL 0.0; UL 1.0) in 20–49-year-olds to 33.6 per 100,000 population (LL 23.5; UL 46.3) in ≥75-year-olds (Table 3, Figure 3).
4. Discussion
This study applied published estimates for the RSV-attributable risk to national hospitalization and death data to obtain estimates of the RSV burden in five middle-income countries where the adult RSV burden is not well documented. Among ≥20-year-olds in 2019, we estimated 14,604 RSV hospitalizations nationally in Argentina, 44,323 in Brazil, 4529 in Chile, 8651 in Mexico, and 7416 in Malaysia. Individuals ≥65-year-olds accounted for 60–74% of all adult RSV-attributable hospitalizations in Latin American countries and Malaysia. In the same year, we estimated 3518, 9115, 801, 3806, and 704 deaths due to RSV in Argentina, Brazil, Chile, Mexico, and Malaysia, respectively, of which, 79–89% were ≥65-year-olds in Latin American countries versus 63% in Malaysia. Incidences of RSV hospitalizations and deaths were substantially higher in ≥65-year-olds versus other age groups. The incidence of RSV hospitalization in older adults was lower in our study than in a meta-analysis of United States (US) data, while RSV mortality was higher in our study than in a US analysis [29,30]. Conversely, estimates for both outcomes were well aligned with a meta-analysis conducted across high-income countries, and with the Fleming et al. study in the UK [10,11].
We observed the hospitalizations for any respiratory disease were substantially lower in Mexico than in other countries. This could reflect significant under-registration, and/or differences in healthcare-seeking behaviors, access to medical care, or clinical thresholds for hospitalization. The Ministry of Health hospital discharge database captures information from public and private hospitals and we consider that this lower level of hospitalization rates most probably originated as a problem of under-registration. This difference was not observed in the number of deaths identified in the Mexican database or in RSV mortality estimated for Mexico.
The data suggest a substantial burden of RSV in the countries studied, with a high disease burden in terms of hospitalizations and death in older adults aged 65+, which is consistent with patterns observed in high-income countries. Underlying risk factors such as chronic obstructive airway disease, asthma, and heart failure may increase this risk even more [31]. Results from the individual countries in our study are difficult to compare because of differences in healthcare systems, clinical practice and thresholds for hospitalization, and potential differences in ICD coding conventions and guidelines for coding from death certificates, or completeness of reporting. For example, the rate of hospitalizations in Argentina in ≥65-year-olds was not commensurate with the observed mortality rate, which could reflect ICD coding conventions on death certificates in Argentina.
Seasonal patterns of RSV outbreaks vary according to climate. Strong seasonal trends with peaks during winter months are typical in temperate climates but are not observed in tropical climates where RSV outbreaks may be related to rainy seasons [32,33]. Raw national data showed strong seasonality in the incidence of respiratory diseases in Argentina, Brazil, Chile and Mexico, which have mixed climates and include temperate and sub-tropical regions, and little impact of the season in tropical Malaysia. Similar seasonal patterns were observed in the RSV epidemiologic surveillance in these countries, including epidemiologic data in the pediatric population in Malaysia [34]. While national epidemiologic surveillance systems may be limited in geographic/population coverage and their capabilities to estimate the countrywide RSV burden, their reported virological seasonal data are aligned with the seasonality observed in our analysis [35,36,37].
Statistical modelling is a useful way to estimate the full burden of disease for infections where epidemiological surveillance data are lacking or incomplete [1]. Studies using methods similar to our own were used in other countries to this end, adding validity to our approach [38,39]. Our study provides important insights into the burden of RSV in adults living in five middle-income countries. A key strength is that the computed estimations for the RSV burden are not biased by the quality, or the sensitivity of viral diagnostic methods, the frequency of viral testing, or the type or quality of sample taken for viral testing. These limitations are typical of RSV surveillance and are one of the main constraints to identifying the full burden of RSV, with flow-on effects when raising awareness amongst clinicians and policy makers about the burden of RSV in older adults.
Potential limitations of our study are those associated with the use of healthcare databases that may be subject to incomplete reporting or incorrect coding practices that could impact disease estimates. Even though each country we studied captures 100% of deaths, translation of information on death certificates into ICD-10 codes may follow different conventions in different countries, further reducing their comparability. We only had access to primary diagnosis codes, and hospitalizations or deaths for other morbidities triggered or exacerbated by RSV were not captured, potentially leading to an underestimation of the disease burden. In addition, our study relies on the assumption that the RSV-attributable risk observed in the UK and reported by Fleming et al. is directly applicable to Latin American countries. Strong seasonality in respiratory diseases was similar in Latin American countries and the UK, suggesting that the application of UK data is likely appropriate in these settings, and the limited available data suggest similar epidemiology in Latin American countries versus the UK [11,40,41]. Nevertheless, the UK has a temperate climate and is geographically and ethnically distinct from Latin America and Asia, and the impact of these and other possible country-based factors on RSV epidemiology is not known. Furthermore, the study by Fleming et al. was subject to its own methodological limitations that may have produced inaccuracies in the attributable risks calculated. Our analysis shows Malaysia as a country without seasonality and a different age distribution of respiratory deaths compared to Latin America and our reference study from the UK [11]. Some COVID-19-related events could have contributed to the excess of mortality in Malaysia from mid-2021. However, we are uncertain how reporting guidelines developed by the different epidemiological surveillance systems may have impacted our data during this period.
RSV has a disproportionate effect on older adults, putting them at higher risk of severe outcomes (hospitalization and death). The burden of disease caused by influenza in older adults has long been recognized and global vaccination recommendations reflecting this burden have been in place for decades. RSV is deserving of similar attention, and prioritization of vaccination of older adults could have substantial impacts on healthcare resource utilization and budgets while contributing to healthy aging.
Plain language statement
What is the context?
- Respiratory syncytial virus (RSV) is an important cause of severe respiratory disease in older adults but may frequently go unrecognized.
- Understanding the burden of disease guides the use of preventative vaccines.
What is new?
- By using hospital and death statistics from Argentina, Brazil, Chile, Mexico, and Malaysia, this study showed large numbers of hospitalizations and deaths due to RSV in each country. Rates were highest in winter and were much higher in adults from the age of 65 years. Almost all RSV deaths occurred in this age group.
What is the impact?
- In view of the frequency and severity of RSV infections in older adults, prevention through vaccination should be prioritized.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/idr16040057/s1, Argentine Hospital Discharge data, Table S1: Number and incidence of hospitalizations for any respiratory disease (J00–J99) by age group (years) and country; Table S2: Number of deaths and mortality (per 100,000 population) due to any respiratory disease (J00–J99) by age group (years) and country; File S1: Interactive Graphical Abstract.
Author Contributions
Conceptualization and methodology, J.A.G., O.C., D.A.M.v.O., A.G.-H., A.B. and A.E.H.; formal analysis and visualization, J.A.G., D.A.M.v.O. and A.G.-H.; investigation, A.G.-H., S.P. and H.J.; writing—review and editing, all authors.; supervision, J.A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by GlaxoSmithKline Biologicals SA (VEO-000968). GlaxoSmithKline Biologicals SA was involved in all stages of the study conduct, including the analysis of the data. GlaxoSmithKline Biologicals SA also took charge of all costs associated with the development and publishing of this manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the use of public and anonymous aggregate data.
Informed Consent Statement
Patient consent was waived due to the use of public and anonymous aggregate data.
Data Availability Statement
Anonymized data and study documents can be requested for further research from https://www.gsk-studyregister.com/en/, accessed on 7 August 2024.
Acknowledgments
The authors thank Business and Decision Life Sciences Medical Communication Service Center for its editorial assistance and manuscript coordination, on behalf of GSK. Joanne Wolter (independent, on behalf of GSK) provided writing support.
Conflicts of Interest
J.G., O.C., A.B., H.J., S.P., A.E.H., D.V.O. and A.G. are employees of GSK. J.G., O.C., A.B., A.E.H. D.V.O. and A.G. hold shares in GSK. The authors declare no other financial and non-financial relationships and activities. The funder was involved in the collection, analyses and interpretation of data; in the writing of the manuscript; and in the decision to publish the results.
References
- Cong, B.; Dighero, I.; Zhang, T.; Chung, A.; Nair, H.; Li, Y. Understanding the age spectrum of respiratory syncytial virus associated hospitalisation and mortality burden based on statistical modelling methods: A systematic analysis. BMC Med. 2023, 21, 224. [Google Scholar] [CrossRef]
- Redondo, E.; Rivero-Calle, I.; Mascaros, E.; Ocana, D.; Jimeno, I.; Gil, A.; Diaz-Maroto, J.L.; Linares, M.; Onieva-Garcia, M.A.; Gonzalez-Romo, F.; et al. Vaccination against community-acquired pneumonia in Spanish adults: Practical recommendations by the NeumoExperts Prevention Group. Antibiotics 2023, 12, 138. [Google Scholar] [CrossRef] [PubMed]
- Kenmoe, S.; Nair, H. The disease burden of respiratory syncytial virus in older adults. Curr. Opin. Infect. Dis. 2024, 37, 129–136. [Google Scholar] [CrossRef]
- Villarruel, G.R.; Langley, G.E.; Abedi, G.R.; Anderson, L.J. Respiratory syncytial virus activity—United States, July 2008–December 2009. Morb. Mortal. Wkly. Rep. 2010, 59, 230–233. [Google Scholar]
- Njue, A.; Nuabor, W.; Lyall, M.; Margulis, A.; Mauskopf, J.; Curcio, D.; Kurosky, S.; Gessner, B.D.; Begier, E. Systematic literature review of risk factors for poor outcomes among adults with respiratory syncytial virus infection in high-income countries. Open Forum Infect. Dis. 2023, 10, ofad513. [Google Scholar] [CrossRef] [PubMed]
- Weycker, D.; Averin, A.; Houde, L.; Ottino, K.; Shea, K.; Sato, R.; Gessner, B.D.; Yacisin, K.; Curcio, D.; Begier, E.; et al. Rates of lower respiratory tract illness in US adults by age and comorbidity profile. Infect. Dis. Ther. 2024, 13, 207–220. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. AREXVY Product Information. Available online: https://www.ema.europa.eu/en/documents/product-information/arexvy-epar-product-information_en.pdf (accessed on 12 February 2024).
- European Medicines Agency. Abrysvo Product Information. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/abrysvo (accessed on 12 February 2024).
- Osei-Yeboah, R.; Spreeuwenberg, P.; Del Riccio, M.; Fischer, T.K.; Egeskov-Cavling, A.M.; Boas, H.; van Boven, M.; Wang, X.; Lehtonen, T.; Bangert, M.; et al. Estimation of the number of respiratory syncytial virus-associated hospitalizations in adults in the European Union. J. Infect. Dis. 2023, 228, 1539–1548. [Google Scholar] [CrossRef]
- Savic, M.; Penders, Y.; Shi, T.; Branche, A.; Pircon, J.Y. Respiratory syncytial virus disease burden in adults aged 60 years and older in high-income countries: A systematic literature review and meta-analysis. Influenza Other Respir. Viruses 2023, 17, e13031. [Google Scholar] [CrossRef]
- Fleming, D.M.; Taylor, R.J.; Lustig, R.L.; Schuck-Paim, C.; Haguinet, F.; Webb, D.J.; Logie, J.; Matias, G.; Taylor, S. Modelling estimates of the burden of Respiratory Syncytial virus infection in adults and the elderly in the United Kingdom. BMC Infect. Dis. 2015, 15, 443. [Google Scholar] [CrossRef]
- Tempia, S.; Moyes, J.; Cohen, A.L.; Walaza, S.; McMorrow, M.L.; Treurnicht, F.K.; Hellferscee, O.; Wolter, N.; von Gottberg, A.; Dawood, H.; et al. The national burden of influenza-like illness and severe respiratory illness overall and associated with nine respiratory viruses in South Africa, 2013–2015. Influenza Other Respir. Viruses 2022, 16, 438–451. [Google Scholar] [CrossRef]
- Naorat, S.; Chittaganpitch, M.; Thamthitiwat, S.; Henchaichon, S.; Sawatwong, P.; Srisaengchai, P.; Lu, Y.; Chuananon, S.; Amornintapichet, T.; Chantra, S.; et al. Hospitalizations for acute lower respiratory tract infection due to respiratory syncytial virus in Thailand, 2008–2011. J. Infect. Dis. 2013, 208 (Suppl. S3), S238–S245. [Google Scholar] [CrossRef]
- Shi, T.; Denouel, A.; Tietjen, A.K.; Campbell, I.; Moran, E.; Li, X.; Campbell, H.; Demont, C.; Nyawanda, B.O.; Chu, H.Y.; et al. Global disease burden estimates of respiratory syncytial virus-associated acute respiratory infection in older adults in 2015: A systematic review and meta-analysis. J. Infect. Dis. 2020, 222, S577–S583. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 LRI Collaborators. Age-sex differences in the global burden of lower respiratory infections and risk factors, 1990–2019: Results from the Global Burden of Disease Study 2019. Lancet Infect. Dis. 2022, 22, 1626–1647. [Google Scholar] [CrossRef] [PubMed]
- GBD 2015 LRI Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect. Dis. 2017, 17, 1133–1161. [Google Scholar] [CrossRef]
- Federal Registry of Health Institutions (REFES). Basic Indicators Report. 2018. Available online: https://www.argentina.gob.ar/sites/default/files/indicadores-basicos-2018.pdf (accessed on 12 February 2024).
- Gomez, J.A.; Sordo, M.E.; Gentile, A. Epidemiologic patterns of diarrheal disease in Argentina: Estimation of rotavirus disease burden. Pediatr. Infect. Dis. J. 2002, 21, 843–850. [Google Scholar] [CrossRef]
- National Supplementary Health Agency. Population with ANS Benefits. March 2023. Available online: https://www.gov.br/ans/pt-br (accessed on 12 February 2024).
- Ministry of Health. DATASUS Tecnologia da Informação a Serviço do SUS. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/niuf.def (accessed on 12 February 2024).
- NEGI, National Institute of Statistics and Geography. Population with Different Health Coverage. 2020 Population & Households Census. Available online: https://www.inegi.org.mx/temas/derechohabiencia/#informacion_general (accessed on 12 February 2024).
- Ministry of Health. Government of Mexico. General Directorate of Health Information. Cubos Dinámicos, Egresos Hospitalarios, Urgencias y Defunciones. 2016–2021. Available online: http://www.dgis.salud.gob.mx/contenidos/basesdedatos/BD_Cubos_gobmx.html (accessed on 12 February 2024).
- Ministry of Health, Malaysia. Malaysia Health Data Warehouse. Available online: https://www.moh.gov.my/index.php/pages/view/58?mid=19. (accessed on 13 October 2023).
- The National Institute of Statistics and Censuses (INDEC), Republic of Argentina. Available online: https://www.indec.gob.ar/indec/web/Nivel4-Tema-2-24-84 (accessed on 13 October 2023).
- Instituto Brasileiro de Geografia e Estatística. Available online: https://www.ibge.gov.br/en/statistics/social/population/18176-population-projection.html (accessed on 13 October 2023).
- National Statistics Institute—Chile. Demographics and Vitals. Available online: https://www.ine.gob.cl/estadisticas/sociales/demografia-y-vitales/ (accessed on 13 October 2023).
- Government of Mexico. CONAPO. Projections of the Population of Mexico and the Federal Entities, 2020–2070. Available online: https://datos.gob.mx/busca/dataset/proyecciones-de-la-poblacion-de-mexico-y-de-las-entidades-federativas-2020-2070 (accessed on 13 October 2023).
- Department of Statistics, Malaysia. Available online: https://newss.statistics.gov.my/newss-portalx/ep/epLogin.seam (accessed on 13 October 2023).
- Matias, G.; Taylor, R.; Haguinet, F.; Schuck-Paim, C.; Lustig, R.; Shinde, V. Estimates of mortality attributable to influenza and RSV in the United States during 1997–2009 by influenza type or subtype, age, cause of death, and risk status. Influenza Other Respir. Viruses 2014, 8, 507–515. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, J.M.; Khan, F.; Begier, E.; Swerdlow, D.L.; Jodar, L.; Falsey, A.R. Rates of medically attended RSV among US adults: A systematic review and meta-analysis. Open Forum Infect. Dis. 2022, 9, ofac300. [Google Scholar] [CrossRef]
- Falsey, A.R.; Hennessey, P.A.; Formica, M.A.; Cox, C.; Walsh, E.E. Respiratory syncytial virus infection in elderly and high-risk adults. N. Engl. J. Med. 2005, 352, 1749–1759. [Google Scholar] [CrossRef]
- Obando-Pacheco, P.; Justicia-Grande, A.J.; Rivero-Calle, I.; Rodriguez-Tenreiro, C.; Sly, P.; Ramilo, O.; Mejias, A.; Baraldi, E.; Papadopoulos, N.G.; Nair, H.; et al. Respiratory syncytial virus seasonality: A global overview. J. Infect. Dis. 2018, 217, 1356–1364. [Google Scholar] [CrossRef]
- Haynes, A.K.; Manangan, A.P.; Iwane, M.K.; Sturm-Ramirez, K.; Homaira, N.; Brooks, W.A.; Luby, S.; Rahman, M.; Klena, J.D.; Zhang, Y.; et al. Respiratory syncytial virus circulation in seven countries with Global Disease Detection Regional Centers. J. Infect. Dis. 2013, 208 (Suppl. S3), S246–S254. [Google Scholar] [CrossRef] [PubMed]
- Suryadevara, M.; Domachowske, J.B. Epidemiology and seasonality of childhood respiratory syncytial virus infections in the tropics. Viruses 2021, 13, 696. [Google Scholar] [CrossRef]
- Chadha, M.; Hirve, S.; Bancej, C.; Barr, I.; Baumeister, E.; Caetano, B.; Chittaganpitch, M.; Darmaa, B.; Ellis, J.; Fasce, R.; et al. Human respiratory syncytial virus and influenza seasonality patterns-Early findings from the WHO global respiratory syncytial virus surveillance. Influenza Other Respir. Viruses 2020, 14, 638–646. [Google Scholar] [CrossRef]
- Lam, T.T.; Tang, J.W.; Lai, F.Y.; Zaraket, H.; Dbaibo, G.; Bialasiewicz, S.; Tozer, S.; Heraud, J.M.; Drews, S.J.; Hachette, T.; et al. Comparative global epidemiology of influenza, respiratory syncytial and parainfluenza viruses, 2010–2015. J. Infect. 2019, 79, 373–382. [Google Scholar] [CrossRef]
- Noyola, D.E.; Mandeville, P.B. Effect of climatological factors on respiratory syncytial virus epidemics. Epidemiol. Infect. 2008, 136, 1328–1332. [Google Scholar] [CrossRef]
- Haeberer, M.; Bruyndonckx, R.; Polkowska-Kramek, A.; Torres, A.; Liang, C.; Nuttens, C.; Casas, M.; Lemme, F.; Ewnetu, W.B.; Tran, T.M.P.; et al. Estimated respiratory syncytial virus-related hospitalizations and deaths among children and adults in Spain, 2016–2019. Infect. Dis. Ther. 2024, 13, 463–480. [Google Scholar] [CrossRef]
- Polkowska-Kramek, A.; Begier, E.; Bruyndonckx, R.; Liang, C.; Beese, C.; Brestrich, G.; Tran, T.M.P.; Nuttens, C.; Casas, M.; Bayer, L.J.; et al. Estimated incidence of hospitalizations and deaths attributable to respiratory syncytial virus infections among adults in Germany between 2015 and 2019. Infect. Dis. Ther. 2024; online ahead of print. [Google Scholar] [CrossRef]
- Ali, A.; Lopardo, G.; Scarpellini, B.; Stein, R.T.; Ribeiro, D. Systematic review on respiratory syncytial virus epidemiology in adults and the elderly in Latin America. Int. J. Infect. Dis. 2020, 90, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Echavarria, M.; Marcone, D.N.; Querci, M.; Seoane, A.; Ypas, M.; Videla, C.; O’Farrell, C.; Vidaurreta, S.; Ekstrom, J.; Carballal, G. Clinical impact of rapid molecular detection of respiratory pathogens in patients with acute respiratory infection. J. Clin. Virol. 2018, 108, 90–95. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).