First Report of Streptococcus ruminantium in Wildlife: Phenotypic Differences with a Spanish Domestic Ruminant Isolate
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bacterial Identification and Genotyping
2.2. Isolates Characterization
2.3. Histopathology
3. Results
3.1. Specific PCR Is a Suitable Method for Identification of S. ruminantium
3.2. S. ruminantium Isolates Presented Phenotypic Differences
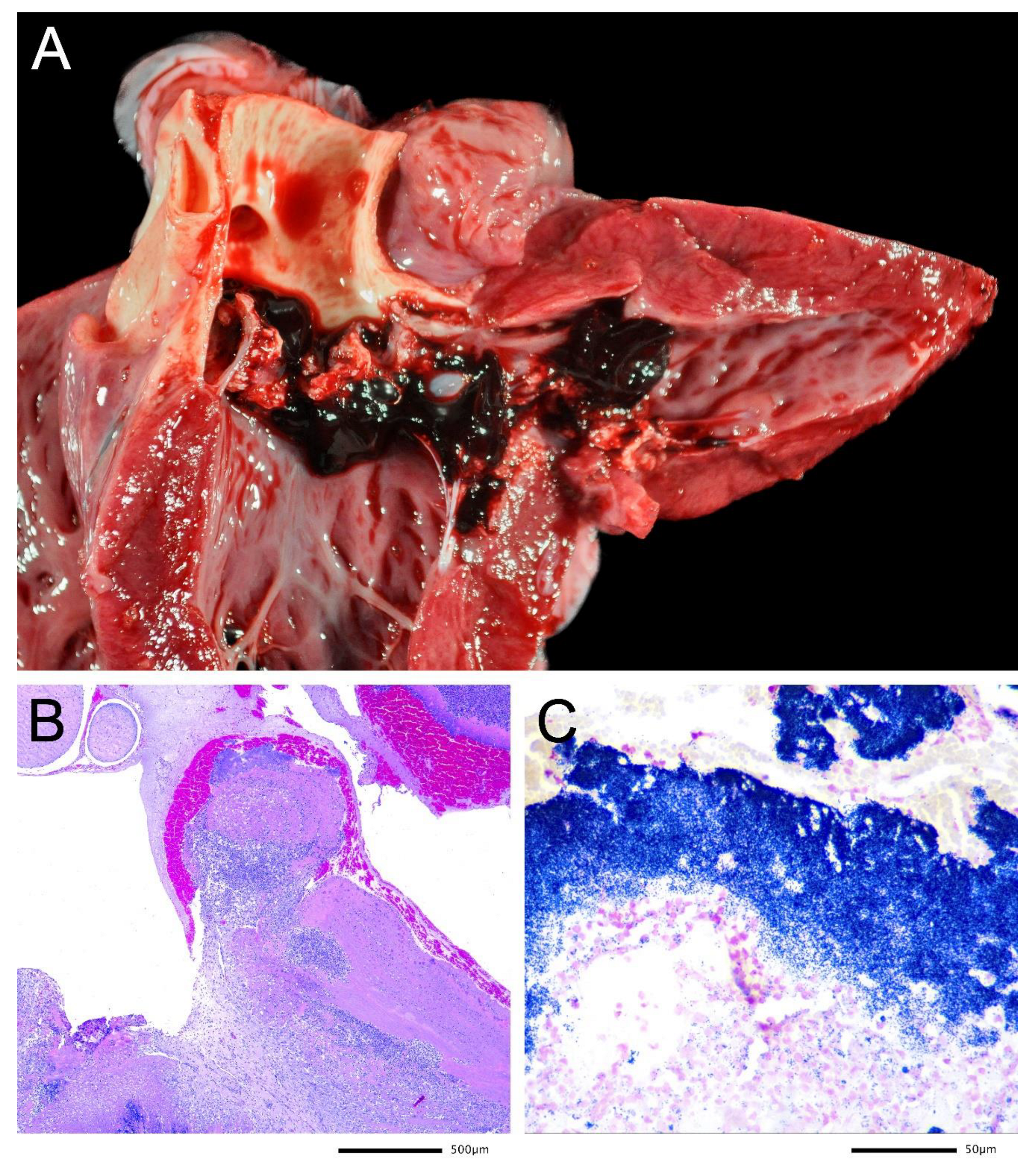
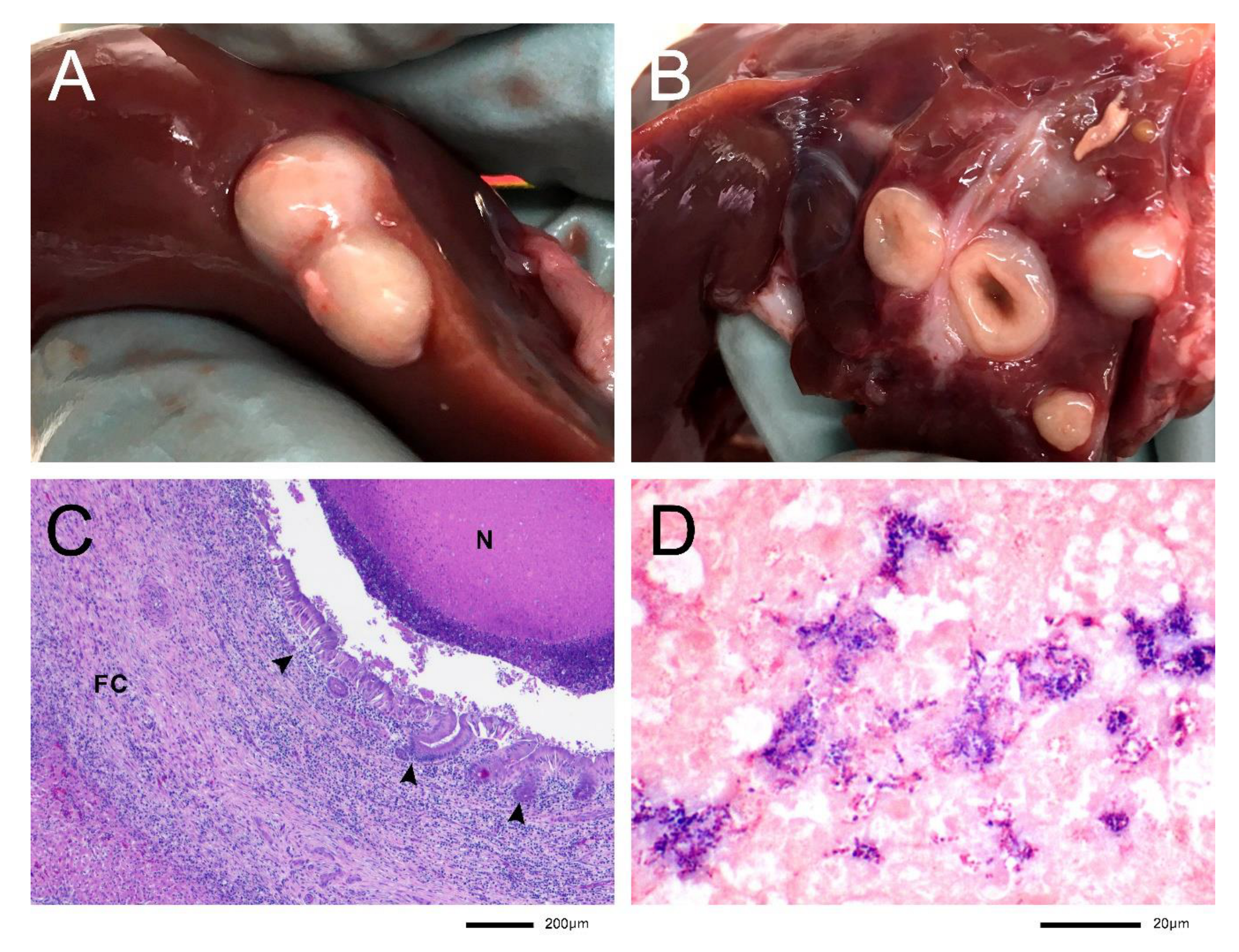
3.3. Lesions Associated with S. ruminantium Isolation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parte, A.C.; Carbasse, J.S.; Meier-Kolthoff, J.P.; Reimer, L.C.; Göker, M. List of Prokaryotic names with Standing in Nomenclature (LPSN) moves to the DSMZ. Int. J. Syst. Evol. Microbiol. 2020, 70, 5607–5612. [Google Scholar] [CrossRef] [PubMed]
- Krzyściak, W.; Pluskwa, K.K.; Jurczak, A.; Kościelniak, D. The pathogenicity of the Streptococcus genus. Eur. J. Clin. Microbiol. 2013, 32, 1361–1376. [Google Scholar] [CrossRef] [Green Version]
- Gottschalk, M.; Segura, M. Streptococci. In Diseases of Swine, 11th ed.; Zimmerman, J.J., Karriker, L.A., Ramirez, A., Schwartz, K.J., Stevenson, G.W., Zhang, J., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2019; pp. 934–950. [Google Scholar]
- Tohya, M.; Arai, S.; Tomida, J.; Watanabe, T.; Kawamura, Y.; Katsumi, M.; Ushimizu, M.; Ishida-Kuroki, K.; Yoshizumi, M.; Uzawa, Y.; et al. Defining the taxonomic status of Streptococcus suis serotype 33: The proposal for Streptococcus ruminantium sp. nov. Int. J. Syst. Evol. Microbiol. 2017, 67, 3660–3665. [Google Scholar] [CrossRef] [PubMed]
- Okura, M.; Maruyama, F.; Ota, A.; Tanaka, T.; Matoba, Y.; Osawa, A.; Sadaat, S.M.; Osaki, M.; Toyoda, A.; Ogura, Y.; et al. Genotypic diversity of Streptococcus suis and the S. suis-like bacterium Streptococcus ruminantium in ruminants. Veter. Res. 2019, 50, 94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gottschalk, M.; Lacouture, S.; Fecteau, G.; DesRochers, A.; Boa, A.; Saab, M.E.; Okura, M. Canada: Isolation of Streptococcus ruminantium (Streptococcus suis-like) from diseased ruminants in Canada. Can. Vet. J. 2020, 61, 473–475. [Google Scholar]
- Zhu, Y.; Dong, W.; Ma, J.; Zhang, Y.; Zhong, X.; Pan, Z.; Liu, G.; Wu, Z.; Yao, H. Comparative genetic analyses provide clues about capsule switching in Streptococcus suis 2 strains with different virulence levels and genetic backgrounds. Microbiol. Res. 2021, 250, 126814. [Google Scholar] [CrossRef] [PubMed]
- Espunyes, J.; Cabezón, O.; Dias-Alves, A.; Miralles, P.; Ayats, T.; Cerdà-Cuéllar, M. Assessing the role of livestock and sympatric wild ruminants in spreading antimicrobial resistant Campylobacter and Salmonella in alpine ecosystems. BMC Veter. Res. 2021, 17, 79. [Google Scholar] [CrossRef]
- Ramey, A.M.; Ahlstrom, C.A. Antibiotic Resistant Bacteria in Wildlife: Perspectives on Trends, Acquisition and Dissemination, Data Gaps, and Future Directions. J. Wildl. Dis. 2020, 56, 1–15. [Google Scholar] [CrossRef]
- Ishida, S.; Tien, L.H.T.; Osawa, R.; Tohya, M.; Nomoto, R.; Kawamura, Y.; Takahashi, T.; Kikuchi, N.; Kikuchi, K.; Sekizaki, T. Development of an appropriate PCR system for the reclassification of Streptococcus suis. J. Microbiol. Methods 2014, 107, 66–70. [Google Scholar] [CrossRef]
- Versalovic, J.; Koeuth, T.; Lupski, R. Distribution of repetitive DNA sequences in eubacteria and application to finerpriting of bacterial enomes. Nucleic Acids Res. 1991, 19, 6823–6831. [Google Scholar] [CrossRef]
- Lane, D.J. 16S/23S rRNA Sequencing. In Nucleic Acid Techniques in Bacterial Systematics, 1st ed.; Stackebrandt, E., Goodfellow, M., Eds.; John Wiley & Sons: New York, NY, USA, 1991; pp. 115–175. [Google Scholar]
- CLSI. Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals, 4th ed.; Clinical and Laboratory Standards Institute: Malvern, PA, USA, 2018. [Google Scholar]
- CLSI. Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals, 5th ed.; Clinical and Laboratory Standards Institute: Malvern, PA, USA, 2020. [Google Scholar]
- Vilček, Š.; Herring, A.J.; Herring, J.A.; Nettleton, P.F.; Lowings, J.P.; Paton, D.J. Pestiviruses isolated from pigs, cattle and sheep can be allocated into at least three genogroups using polymerase chain reaction and restriction endonuclease analysis. Arch. Virol. 1994, 136, 309–323. [Google Scholar] [CrossRef] [PubMed]
- White, A.; Hughes, J.M. Critical Importance of a One Health Approach to Antimicrobial Resistance. EcoHealth 2019, 16, 404–409. [Google Scholar] [CrossRef] [Green Version]
- Torres-Blas, I.; Aguilar, X.F.; Cabezón, O.; Aragon, V.; Migura-García, L. Antimicrobial Resistance in Pasteurellaceae Isolates from Pyrenean Chamois (Rupicapra pyrenaica) and Domestic Sheep in an Alpine Ecosystem. Animals 2021, 11, 1686. [Google Scholar] [CrossRef] [PubMed]
- Conrad, P.A.; Meek, L.A.; Dumit, J. Operationalizing a One Health approach to global health challenges. Comp. Immunol. Microbiol. Infect. Dis. 2013, 36, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Vittecoq, M.; Godreuil, S.; Prugnolle, F.; Durand, P.; Brazier, L.; Renaud, N.; Arnal, A.; Aberkane, S.; Jean-Pierre, H.; Gauthier-Clerc, M.; et al. Antimicrobial resistance in wildlife. J. Appl. Ecol. 2016, 53, 519–529. [Google Scholar] [CrossRef] [Green Version]
- Mühldorfer, K.; Rau, J.; Fawzy, A.; Heydel, C.; Glaeser, S.P.; Van Der Linden, M.; Kutzer, P.; Knauf-Witzens, T.; Hanczaruk, M.; Eckert, A.S.; et al. Streptococcus castoreus, an uncommon group A Streptococcus in beavers. Antonie van Leeuwenhoek. Int. J. Gen. Mol. Microbiol. 2019, 112, 1663–1673. [Google Scholar] [CrossRef]
- EMA. Sales of Veterinary Antimicrobial Agents in 31 European Countries in 2018—EMA/24309/2020. 2020. Available online: https://www.ema.europa.eu/en/documents/report/sales-veterinary-antimicrobial-agents-31-european-countries-2018-trends-2010-2018-tenth-esvac-report_en.pdf (accessed on 12 January 2022).
- Liegeon, G.; Delory, T.; Picardeau, M. Antibiotic susceptibilities of livestock isolates of leptospira. Int. J. Antimicrob. Agents 2018, 51, 693–699. [Google Scholar] [CrossRef]
- Bourély, C.; Cazeau, G.; Jouy, E.; Haenni, M.; Madec, J.-Y.; Jarrige, N.; Leblond, A.; Gay, E. Antimicrobial resistance of Pasteurella multocida isolated from diseased food-producing animals and pets. Veter. Microbiol. 2019, 235, 280–284. [Google Scholar] [CrossRef]
- Haenni, M.; Lupo, A.; Madec, J.-Y. Antimicrobial Resistance in Streptococcus spp. In Antimicrobial Resistance in Bacteria from Livestock and Companion Animals, 1st ed.; Schwarz, S., Cavaco, L.M., Jianzhong, S., Aarestrup, F.M., Eds.; American Society of Microbiology: Washington, DC, USA, 2018. [Google Scholar] [CrossRef]
- Allen, H.K.; Donato, J.; Wang, H.H.; Cloud-Hansen, K.A.; Davies, J.; Handelsman, J. Call of the Wild: Antibiotic resistance genes in natural environments. Nat. Rev. Microbiol. 2010, 8, 251–259. [Google Scholar] [CrossRef]
- Staats, J.J.; Feder, I.; Okwumabua, O.; Chengappa, M.M. Streptococcus Suis: Past and Present. Vet. Res. Commun. 1997, 21, 381–407. [Google Scholar] [CrossRef]
- Okwumabua, O.; Peterson, H.; Hsu, H.-M.; Bochsler, P.; Behr, M. Isolation and partial characterization of Streptococcus suis from clinical cases in cattle. J. Veter. Diagn. Investig. 2017, 29, 160–168. [Google Scholar] [CrossRef] [Green Version]
- Marco, I.; Cabezón, O.; Velarde, R.; Fernández-Sirera, L.; Colom-Cadena, A.; Serrano, E.; Rosell, R.; Casas-Díaz, E.; Lavín, S.; Ferron, E.S. The two sides of border disease in Pyrenean chamois (Rupicapra pyrenaica): Silent persistence and population collapse. Anim. Health Res. Rev. 2015, 16, 70–77. [Google Scholar] [CrossRef]
- Galina, L.; Pijoan, C.; Sitjar, M.; Christianson, W.; Rossow, K.; Collins, J. Interaction between Streptococcus suis serotype 2 and porcine reproductive and respiratory syndrome virus in specific pathogen-free piglets. Veter. Rec. 1994, 134, 60–64. [Google Scholar] [CrossRef]
- Thanawongnuwech, R.; Brown, G.B.; Halbur, P.G.; Roth, J.A.; Royer, R.L.; Thacker, B.J. Pathogenesis of Porcine Reproductive and Respiratory Syndrome Virus-induced Increase in Susceptibility to Streptococcus suis Infection. Veter. Pathol. 2000, 37, 143–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, W.-H.; Laster, S.M.; Tompkins, M.; Brown, T.; Xu, J.-S.; Altier, C.; Gomez, W.; Benfield, D.; McCaw, M.B. In Utero Infection by Porcine Reproductive and Respiratory Syndrome Virus Is Sufficient to Increase Susceptibility of Piglets to Challenge by Streptococcus suis Type II. J. Virol. 2001, 75, 4889–4895. [Google Scholar] [CrossRef] [Green Version]
- Lin, X.; Huang, C.; Shi, J.; Wang, R.; Sun, X.; Liu, X.; Zhao, L.; Jin, M. Investigation of Pathogenesis of H1N1 Influenza Virus and Swine Streptococcus suis Serotype 2 Co-Infection in Pigs by Microarray Analysis. PLoS ONE 2015, 10, e0124086. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Zhou, H.; Hao, Q.; Li, M.; Liu, J.; Fan, H. Coinfection with porcine circovirus type 2 and Streptococcus suis serotype 2 enhances pathogenicity by dysregulation of the immune responses in piglets. Veter. Microbiol. 2020, 243, 108653. [Google Scholar] [CrossRef] [PubMed]
- Iglesias, J.G.; Trujano, M.; Xu, J. Inoculation of pigs with Streptococcus suis type 2 alone or in combination with pseudorabies virus. Am. J. Veter. Res. 1992, 53, 364–367. [Google Scholar]
- Sanchez Armengol, E.; Harmanci, M.; Laffleur, F. Current strategies to determine antifungal and antimicrobial activity of natural compounds. Microbiol. Res. 2021, 252, 126867. [Google Scholar] [CrossRef] [PubMed]
| Isolate | Organ of Isolation | Host Species | Age and Sex | Cause of Death | Main Necropsy Findings | Place | Date |
|---|---|---|---|---|---|---|---|
| RP15178-A2 | Lung lesion | Chamois (Rupicapra pyrenaica) | 4 years, male | Seasonal controlled hunting | Infectious queratoconjunctivitis, diarrhea, and bacterial cranioventral suppurative bronchopneumonia | Freser-Setcases National Game Reserve (Queralbs, Catalonia, Spain) | December 2015 |
| RP16030-M1 | Lung lesion | Chamois (Rupicapra pyrenaica) | 4 years, female | Seasonal controlled hunting | Old fibrous pleural adhesions from previous pneumonia and cysticercosis in peritoneum and diaphragm | Freser-Setcases National Game Reserve (Queralbs, Catalonia, Spain) | May 2016 |
| CCGMV933 | Lung lesion | Chamois (Rupicapra pyrenaica) | 14 months, male | Severe pestivirus infection * | Cachexia, bacterial cranioventral suppurative bronchopneumonia, multifocal acute suppurative hepatitis, and nonsuppurative viral meningoencephalitis | Aigüestortes i Estany de Sant Maurici National Park (La Vall de Boí, Catalonia, Spain) | August 2020 |
| CCGMV935 | Heart valves vegetation | Chamois (Rupicapra pyrenaica) | 5 months, male | Bacterial septicemia * | Bacterial suppurative endocarditis, meningoencephalitis, embolic pneumonia, hepatitis, nephritis, splenitis, lymphadenitis, myelitis, contagious ecthyma, verminous pneumonia, and bronchopneumonia | Freser-Setcases National Game Reserve (Queralbs, Catalonia, Spain) | October 2020 |
| CCGMV928 | Liver abscess | Domestic sheep (Ovis aries) | 3 months, male | Slaughterhouse | Liver abscesses and cranioventral suppurative bronchopneumonia | Municipal slaughterhouse (Farm located in Catalonia, Spain) | September 2019 |
| PCR | Primers | Primer sequence | Reference |
|---|---|---|---|
| 16S | 358F 907R | CTACGGGAGGCAGCAGT CCGTCWATTCMTTTGAGTTT | Amplification and sequencing of the V2-V5 region of the 16S rRNA gene [12]. |
| recN-S. suis | SSrecN-F SSrecN-R | CTACAAACAGCTCTCTTCT ACAACAGCCAATTCATGGCGTGATT | PCR based on the S. suis recombination/repair protein (recN) [10]. |
| S. ruminantium | Forward Reverse | GCAAGTGGAACGCAACTTTTCA CTATGTATCGTTGCCTTGGTAG | PCR designed to discriminate S. ruminantium from S. suis. [5]. |
| ERIC | ERIC-1F ERIC-2R | ATGTAAGCTCCTGGGGATTCAC AAGTAAGTGACTGGGGTGAGCG | Enterobacterial repetitive intergenic consensus PCR [11]. |
| Antimicrobial | RP15178-A2 | RP16030-M1 | CCGMV933 | CCGMV935 | CCGMV928 |
|---|---|---|---|---|---|
| Ampicillin | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 |
| Ceftiofur | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 |
| Clindamycin | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 |
| Danofloxacin | 0.50 * | 0.50 * | 1 * | ≤0.12 | 0.25 |
| Enrofloxacin | 0.50 | 0.50 | 1 | ≤0.12 | 0.25 |
| Florfenicol | 2 | 1 | 2 | 1 | 1 |
| Gamithromycin | ≤1 | ≤1 | ≤1 | ≤1 | ≤1 |
| Gentamicin | 4 | 4 | 4 | 4 | 8 |
| Neomycin | 16 | 8 | 16 | 16 | 16 |
| Penicillin | ≤0.12 | ≤0.12 | ≤0.12 | ≤0.12 | ≤0.12 |
| Spectinomycin | 16 | 16 | 16 | 16 | 16 |
| Sulfadimethoxine | ≤256 | ≤256 | ≤256 | ≤256 | ≤256 |
| Tetracycline | 1 | 1 | 1 | ≤0.5 | >8 * |
| Tiamulin | 4 | 4 | 8 | 16 | 16 |
| Tildipirosin | 16 | 8 | 8 | 16 | 16 |
| Tilmicosin | 8 | 8 | 8 | 16 | 8 |
| Trimethoprim-sulfamethoxazole | ≤2/38 | ≤2/38 | ≤2/38 | ≤2/38 | ≤2/38 |
| Tulathromycin | ≤8 | ≤8 | ≤8 | ≤8 | ≤8 |
| Tylosin tartrate | 1 | ≤0.5 | ≤0.5 | ≤0.5 | ≤0.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neila-Ibáñez, C.; Pintado, E.; Velarde, R.; Fernández Aguilar, X.; Vidal, E.; Aragon, V.; Abarca, M.L. First Report of Streptococcus ruminantium in Wildlife: Phenotypic Differences with a Spanish Domestic Ruminant Isolate. Microbiol. Res. 2022, 13, 102-113. https://doi.org/10.3390/microbiolres13010008
Neila-Ibáñez C, Pintado E, Velarde R, Fernández Aguilar X, Vidal E, Aragon V, Abarca ML. First Report of Streptococcus ruminantium in Wildlife: Phenotypic Differences with a Spanish Domestic Ruminant Isolate. Microbiology Research. 2022; 13(1):102-113. https://doi.org/10.3390/microbiolres13010008
Chicago/Turabian StyleNeila-Ibáñez, Carlos, Ester Pintado, Roser Velarde, Xavier Fernández Aguilar, Enric Vidal, Virginia Aragon, and M. Lourdes Abarca. 2022. "First Report of Streptococcus ruminantium in Wildlife: Phenotypic Differences with a Spanish Domestic Ruminant Isolate" Microbiology Research 13, no. 1: 102-113. https://doi.org/10.3390/microbiolres13010008
APA StyleNeila-Ibáñez, C., Pintado, E., Velarde, R., Fernández Aguilar, X., Vidal, E., Aragon, V., & Abarca, M. L. (2022). First Report of Streptococcus ruminantium in Wildlife: Phenotypic Differences with a Spanish Domestic Ruminant Isolate. Microbiology Research, 13(1), 102-113. https://doi.org/10.3390/microbiolres13010008








