Abstract
Klebsiella (K.) pneumoniae is a major pathogen in human and veterinary medicine, known for its high resistance rates. Comprehensive resistance data are essential to combat global antibiotic resistance. This study aims to (a) document the prevalence of resistant K. pneumoniae and (b) assess the utility of routine laboratory data for passive monitoring. We analyzed a dataset of 175,171 samples from diseased dogs and cats in Germany collected between 2019 and 2021, identifying 1185 K. pneumoniae isolates with measurable minimum inhibitory concentration values. We evaluated resistance rates to a third-generation cephalosporin (cefovecin) (16.3%), chloramphenicol (16.1%), doxycycline (13.9%), enrofloxacin (8.9%), gentamicin (6.0%), nitrofurantoin (24.8%), and sulfamethoxazole-trimethoprim (15.0%). Notably, feline K. pneumoniae isolates from the urinary tract showed a high cefovecin resistance rate of 70.0%. Comparing our findings with third-generation cephalosporin-resistant human isolates from the Antimicrobial Resistance Surveillance database (ARS) maintained by the Robert Koch Institute revealed a lower resistance rate (7.7%). This study presents Germany’s most comprehensive dataset on K. pneumoniae resistance in companion animals over a three-year period. These findings can strengthen national resistance monitoring efforts and enhance data interpretation through substantial datasets.
1. Introduction
The emergence of antibiotic-resistant pathogens poses a significant threat to public health. Third-generation cephalosporin-resistant (3GCR) Klebsiella (K.) pneumoniae is, together with 3GCR Escherichia (E.) coli and methicillin-resistant Staphylococcus aureus, a major contributor to the highest health impact and the largest burden of disease of all pathogens tested by the ECDC in Europe in the years 2016–2020 [1]. The seriousness of the situation is underlined by the latest ECDC 2022 report, which shows that at least one third of K. pneumoniae isolates are resistant to 3GC [1].
The concerning trend in antibiotic resistance is a result of bacterial evolutionary adaptation to the presence of antibiotics, with accelerated development when these medications are used incorrectly or too frequently [2,3]. Recognizing the severity of this issue, the World Health Organization (WHO) launched a global action plan in 2015 to address the threat of antibiotic resistance [4]. Since then, a comprehensive framework of regulations and laws has been created both at the European Union level and in Germany to monitor the use of antibiotics and the occurrence of resistances [5,6,7,8]. GERM-Vet, as a national resistance monitoring program, systematically collects data on bacterial resistance in both food-producing and companion animals across Germany [9].
K. pneumoniae is an opportunistic pathogen that carries several virulence factors, including pili, capsules, and lipopolysaccharide and iron carriers. Its ability to form biofilms, combined with an assortment of resistance genes, empowers it with resilience against aminoglycosides, quinolones, polymyxins, and ß-lactams [10]. Due to the large number of chromosomal and plasmid-encoded antibiotic resistance genes, K. pneumoniae frequently exhibits multidrug resistance (MDR) [11]. As a highly pathogenic bacterium in companion animals, it frequently causes infections in the urogenital tract, but it can also affect the digestive, respiratory, and reproductive systems. Additionally, K. pneumoniae is able to cause otitis, abscesses, hepatitis, pyodermatitis, sepsis, and conjunctivitis. This bacterium has the potential to infect nearly every organ or tissue in companion animals [12].
In human medicine, K. pneumoniae is often divided into classical K. pneumoniae (cKp) and hypervirulent K. pneumoniae (hvKp). While classical K. pneumoniae is known to cause pneumonia, urogenital infections, and bacteremia in immunocompromised patients who are often hospitalized, hypervirulent K. pneumoniae variants can cause disease in healthy individuals. They can cause suppurative liver abscesses and are capable of infecting distant tissues such as the eye, lung, central nervous system, and others [13].
This study is the second part of our work on 3GCR Enterobacterales and aimed to investigate the usability of routine laboratory data for passive monitoring. The 3GC resistance proportions in K. pneumoniae are often higher than in E. coli, making monitoring of K. pneumoniae susceptibility of major importance [14]. Our aim was to document and visualize the resistance proportions in K. pneumoniae isolates from dogs and cats in Germany. These findings could provide valuable support for active monitoring, such as the national animal pathogen resistance monitoring GERM-Vet.
2. Materials and Methods
2.1. Samples and Sample Processing
Between 2019 and 2021, Laboklin, an accredited veterinary diagnostic laboratory, supplied data on 175,171 clinical samples from dogs and cats, including wound and skin swabs, respiratory and genital tract swabs or lavages, as well as blood and urine. The samples were collected from animals presented in veterinary medical facilities (n = 3491) across Germany, constituting 33.1% of practices and clinics [15]. Further data (e.g., on sampling time or antimicrobial pre-treatment) was not available to us.
2.2. Bacterial Isolation and Identification
Bacterial culture with a 3-phase streaking pattern on Columbia agar with 5% sheep blood and BD Endo agar was carried out. Furthermore, an enrichment culture of the swab in tryptic soy broth (Becton Dickinson GmbH, Heidelberg, Germany) was executed. The cultures were incubated for 24 h under aerobic conditions at 36 °C. Following incubation, the enrichment culture was streaked on Columbia agar with 5% sheep blood and Endo agar and incubated under the same conditions. Subsequently, it was then determined whether bacterial growth had occurred after enrichment. Additionally, separate pure cultures were prepared on blood and endo-agar plates [16].
The bacterial strains were identified by observing their growth morphology by biochemical reactions such as oxidase (MAST Diagnostica GmbH, Reinfeld, Germany) and Matrix-assisted Laser Desorption Ionization Time of Flight Mass Spectrometry (MALDI-TOFMS) from Bruker Corporation, Bremen, Germany [16].
2.3. Antimicrobial Susceptibility Testing
The antimicrobial susceptibility testing (AST) results were evaluated using the CLSI (Clinical and Laboratory Standards Institute, Berwyn, PA, USA) documents Vet01S ED6 and M100 ED33 [17,18]. They were categorized as sensitive (S), intermediate (I), and resistant (R). Laboklin uses panels customized to its requirements for Gram-negative pathogens. Broth microdilution testing, carried out by the Micronaut system from MERLIN Gesellschaft für mikrobiologische Diagnostik mbH, Bornheim-Hersel, Germany, was used for AST [16].
2.4. Preparation for Statistical Analysis
Our evaluation encompassed a subset of antimicrobial substances chosen based on their relevance to therapy in both small animal and human medicine. The included antimicrobials were categorized as follows: beta-lactams (cefovecin, FOV S ≤ 2; R ≥ 8), aminoglycosides (gentamicin, GEN S ≤ 2; R ≥ 8), fluoroquinolones (enrofloxacin, ENR S ≤ 0.5; R ≥ 4), tetracyclines (doxycycline, DOX S ≤ 4; R ≥ 16), phenicols (chloramphenicol, CHL S ≤8; R ≥ 32), folate pathway inhibitors (sulfamethoxazole + trimethoprim, SXT S ≤ 2/38; R ≥ 4/76), and nitrofurans (nitrofurantoin, NIT S ≤ 32; R ≥ 128).
All samples were classified into one of six organ system categories. Those associated with wounds, musculoskeletal systems, and surgical samples were collectively grouped under the term “wound”. The category “skin/soft tissue” (SST) included samples related to skin, soft tissue, and secondary reproductive organs such as the mammary gland. “Other” comprised samples associated with other organ systems and the gastrointestinal tract. Additionally, distinct categories were established for “urogenital tract infections” (UTI), “respiratory tract”, and “reproductive tract”.
2.5. Statistical Analyses
Statistical analysis was carried out using R version 4.2.2 from the R Foundation Vienna [19] and the AMR package [20]. Our presentation features resistance proportions alongside their corresponding 95% Wilson confidence intervals (95% CI). These proportions and intervals are determined for various subgroups, such as species and species/sample type. Temporal trends in cefovecin resistance were assessed using the Cochrane–Armitage test.
3. Results
In total, there were 175,171 samples collected, with 122,831 originating from dogs and 52,340 from cats. The dataset contained a total of 1234 K. pneumoniae samples, of which 1074 were from dogs and 160 were from cats. Pure K. pneumoniae cultures accounted for 459 (37.2%) of our 1234 samples. The remaining 775 samples (62.8%) were from mixed cultures with two or more bacterial species. In the mixed canine samples, in addition to K. pneumoniae, Staphylococcus pseudintermedius was detected in 220 samples, ß-hemolytic Streptococcus sp. in 117 samples, Pseudomonas aeruginosa in 99 samples, Proteus mirabilis in 66 samples, Escherichia coli in 58 samples, aerobic spore formers in 52 samples, in 48 samples Enterococcus sp., in 47 samples alpha-hemolytic Streptococcus sp., in 46 samples hemolytic Escherichia coli, in 29 samples methicillin-resistant Staphyloccus pseudintermedius, and in 21 samples Pasteurella sp. Other pathogens such as Staphylococcus aureus, Pantoea agglomerans, or Streptococcus canis were also found, but with less than 10 samples each.
In the feline samples, in addition to K. pneumoniae, Staphylococcus felis was isolated in 20 samples, Pasteurella multocida in 16 samples, Enterococcus sp. in 13 samples, Staphylococcus aureus in 8 samples, ß-hemolytic Streptococcus sp. in 8 samples, hemolytic Escherichia coli in 6 samples, Proteus mirabilis in 6 samples, and Staphylococcus pseudintermedius in 6 further samples. Other pathogens, such as Pseudomonas aeruginosa, Acinetobacter baumannii, and others, were also found, but in no more than five samples each.
In 110 (10.2%) of the canine samples, K. pneumoniae could only be isolated after enrichment. Of these 110 canine samples, the following were isolated before enrichment: Staphylococcus pseudintermedius in 37 samples, Pseudomonas aeruginosa in 12 samples, aerobic spore formers in 10 samples, hemolytic Escherichia coli in 10 samples, Pasteurella sp. in 9 samples, and ß-hemolytic Streptococcus sp. in 9 further samples. Several other bacterial species were isolated, but in fewer samples. In 20 canine samples, no other bacteria than K. pneumoniae after enrichment could be isolated. In feline samples, K. pneumoniae was detected in 34 cases (21.3%) only after enrichment. Staphylococcus felis (n = 7), Pasteurella multocida (n = 6), and Escherichia coli (n = 5) were isolated from the feline samples prior to enrichment. Other bacterial species were also present here, but in smaller numbers. In four feline samples, no other bacteria than K. pneumoniae after enrichment could be isolated.
Among the canine samples, 1027 K. pneumoniae isolates underwent antimicrobial susceptibility testing, allowing for assessable MICs. Similarly, 158 feline K. pneumoniae isolates were subjected to the same analysis. The results presented in Table 1 refer to K. pneumoniae isolates with evaluable MIC.

Table 1.
Distribution of canine and feline K. pneumoniae isolates, including yearly (2019–2021) and organ-specific isolates.
K. pneumoniae was isolated in 0.9% of all wound samples, totaling 16,111 samples. Of the total of 21,398 respiratory tract samples, 1.2% contained K. pneumoniae. In skin and soft tissue samples, which amounted to 67,293, K. pneumoniae was found in 0.4%. Among the 11,479 UTI samples, 0.8% were K. pneumoniae isolates. For reproductive tract samples (9428), 0.7% contained K. pneumoniae. Finally, in all other types of samples, totaling 49,463, K. pneumoniae was isolated in 0.7%.
Forty-nine K. pneumoniae isolates had to be excluded because they did not obtain MIC values.
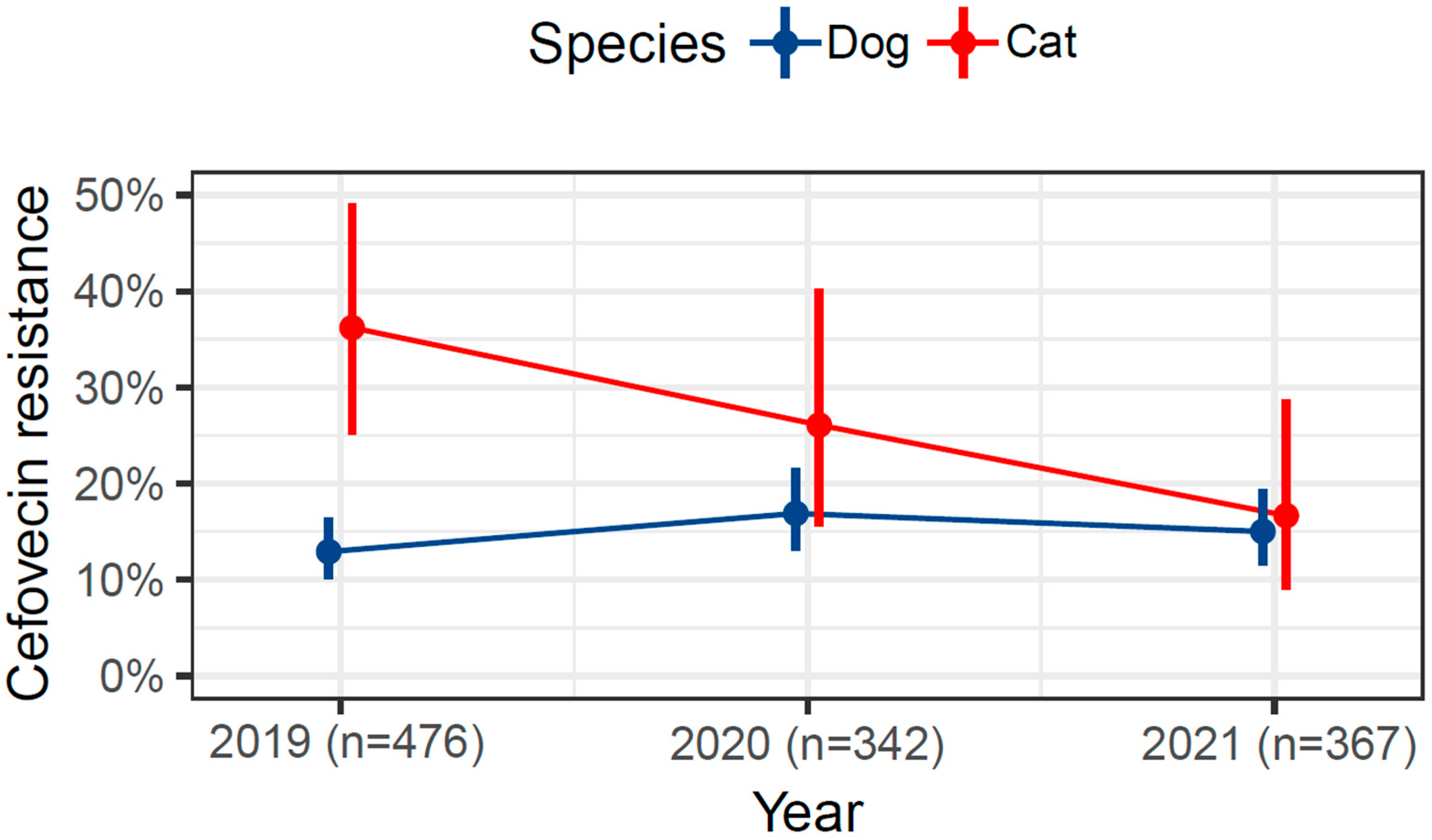
In Figure 1, we conducted a comparison of cefovecin resistance proportions between feline (n = 158) and canine (n = 1027) K. pneumoniae isolates. Interestingly, in 2019, the prevalence of cefovecin resistance in isolates from cats (36%) was more than twice as high as in isolates from dogs (14%). Subsequently, there was a remarkable decline in cefovecin-resistant isolates obtained from cats, with proportions dropping to 26% in 2020 and further to 16% in 2021, approaching the resistance level observed in isolates obtained from dogs. Meanwhile, the resistance proportion among canine K. pneumoniae isolates remained relatively stable, experiencing a slight increase to 17% in 2020 before decreasing again to 15% in 2021.
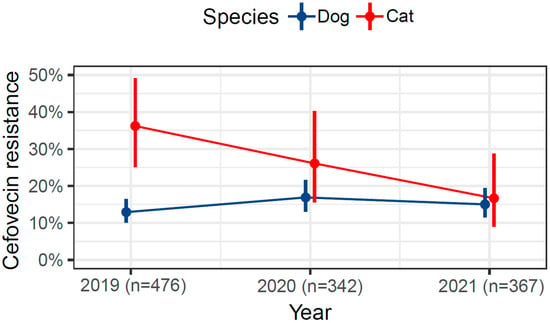
Figure 1.
Trends in cefovecin resistance in K. pneumoniae among dogs and cats from 2019 to 2021.
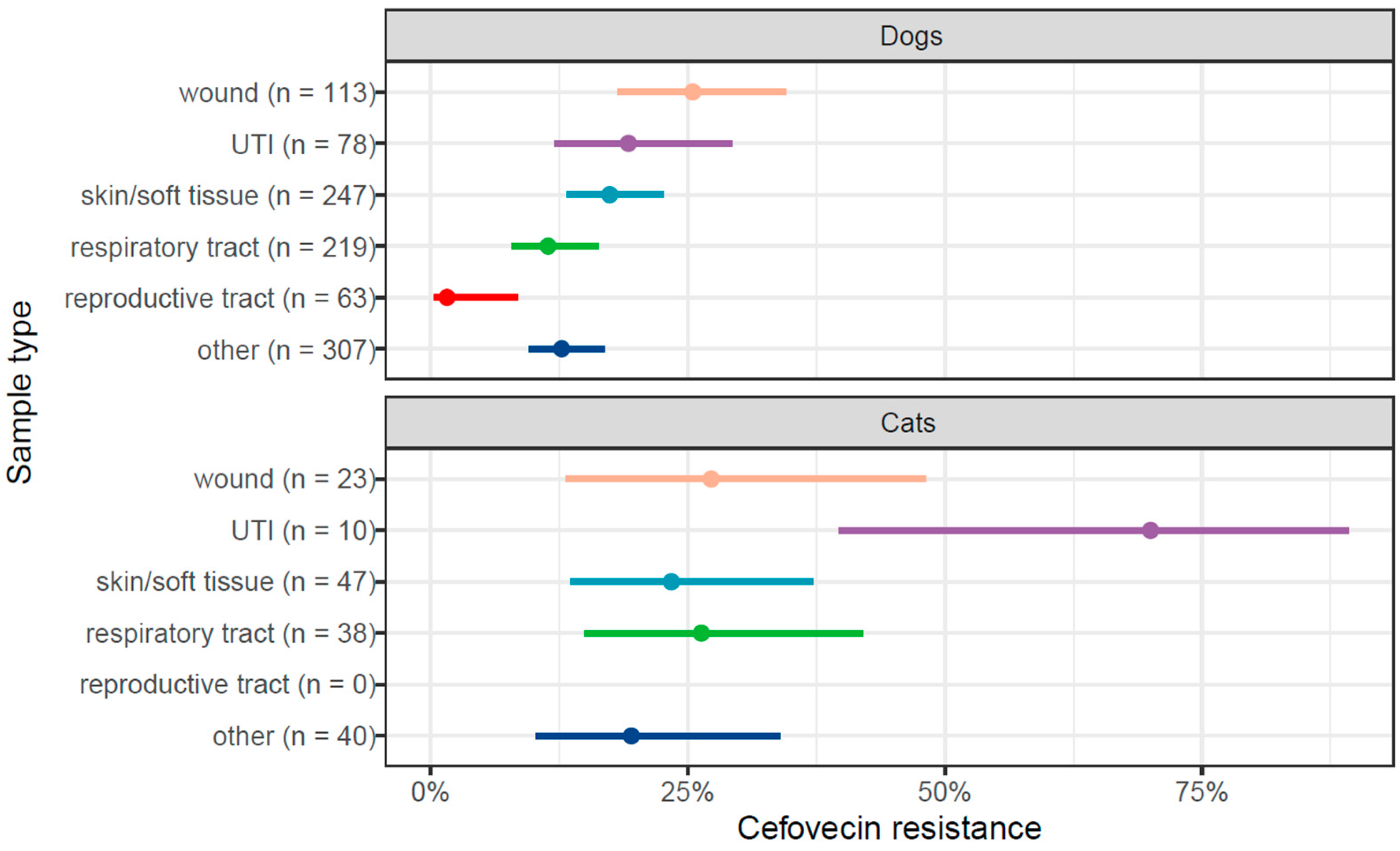
Figure 2 displays the cefovecin resistance proportions in K. pneumoniae isolates obtained from dogs and cats categorized by organ system. Among canine isolates, resistance proportions varied from 0% to 25%. The highest resistance was observed in wound isolates at 25%. Interestingly, none of the reproductive tract isolates showed resistance to cefovecin.
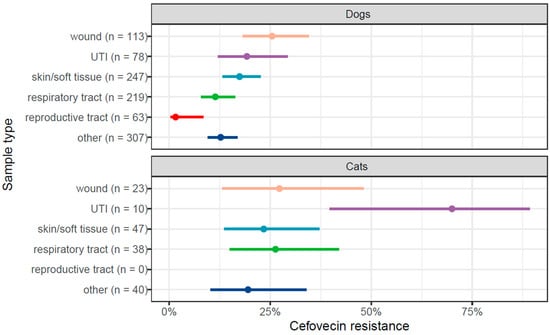
Figure 2.
Organ-specific proportion of cefovecin resistance among K. pneumoniae isolated from dogs and cats’ samples, including 95% confidence intervals.
Feline urinary tract infection isolates showed a resistance proportion of 70%; however, it is important to note the relatively small number of isolates that leads to a large 95% CI. K. pneumoniae isolated from wound swabs, skin/soft tissues, and the respiratory tract displayed approximately 25% resistance. Notably, no Klebsiella isolates were identified from the reproductive tract.
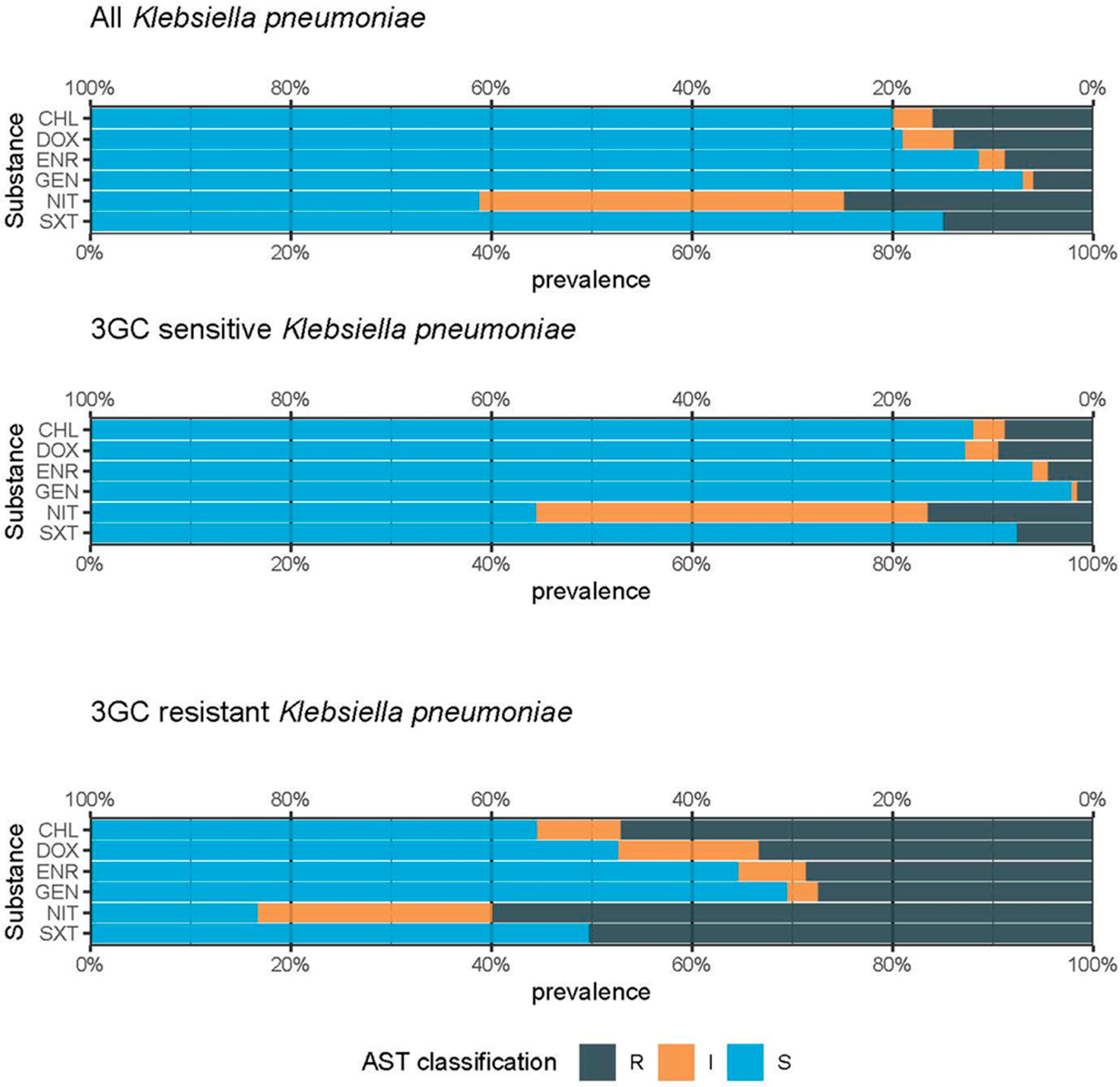
The resistance proportions of K. pneumoniae isolates to various antimicrobial agents (CHL, DOX, ENR, GEN, NIT, and SXT) are presented in Figure 3. Initially, all K. pneumoniae isolates were analyzed, followed by subgroups of 3GC-sensitive K. pneumoniae isolates and 3GC-resistant K. pneumoniae isolates. The highest resistance proportions were observed among the 3GCR K. pneumoniae isolates. Notably, the highest resistance proportion was recorded against NIT (60%), while the lowest resistance proportions were observed for ENR and GEN (below 30%). Resistance proportions exceeding 30% were noted for all other antibiotic agents.
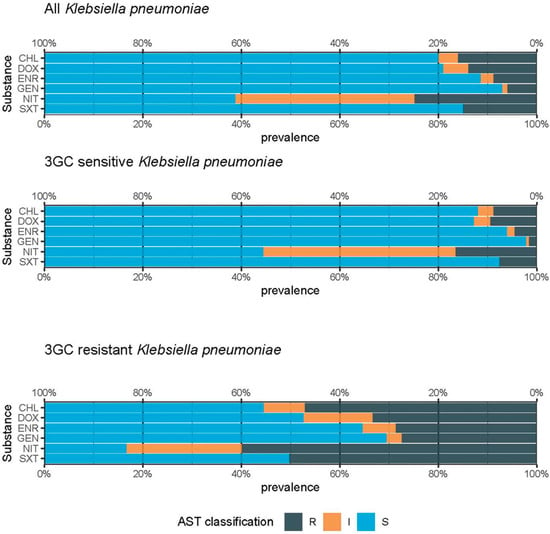
Figure 3.
Antimicrobial susceptibility patterns in 1185 K. pneumoniae isolates in dogs and cats. This figure includes resistance against chloramphenicol (CHL), doxycycline (DOX), enrofloxacin (ENR), gentamicin (GEN), nitrofurantoin (NIT), and sulfamethoxazole/trimethoprim (SXT) over 3 years (2019–2021).
With regard to 3GC-sensitive K. pneumoniae, the isolates showed resistance proportions of less than 20% to all antimicrobial substances.
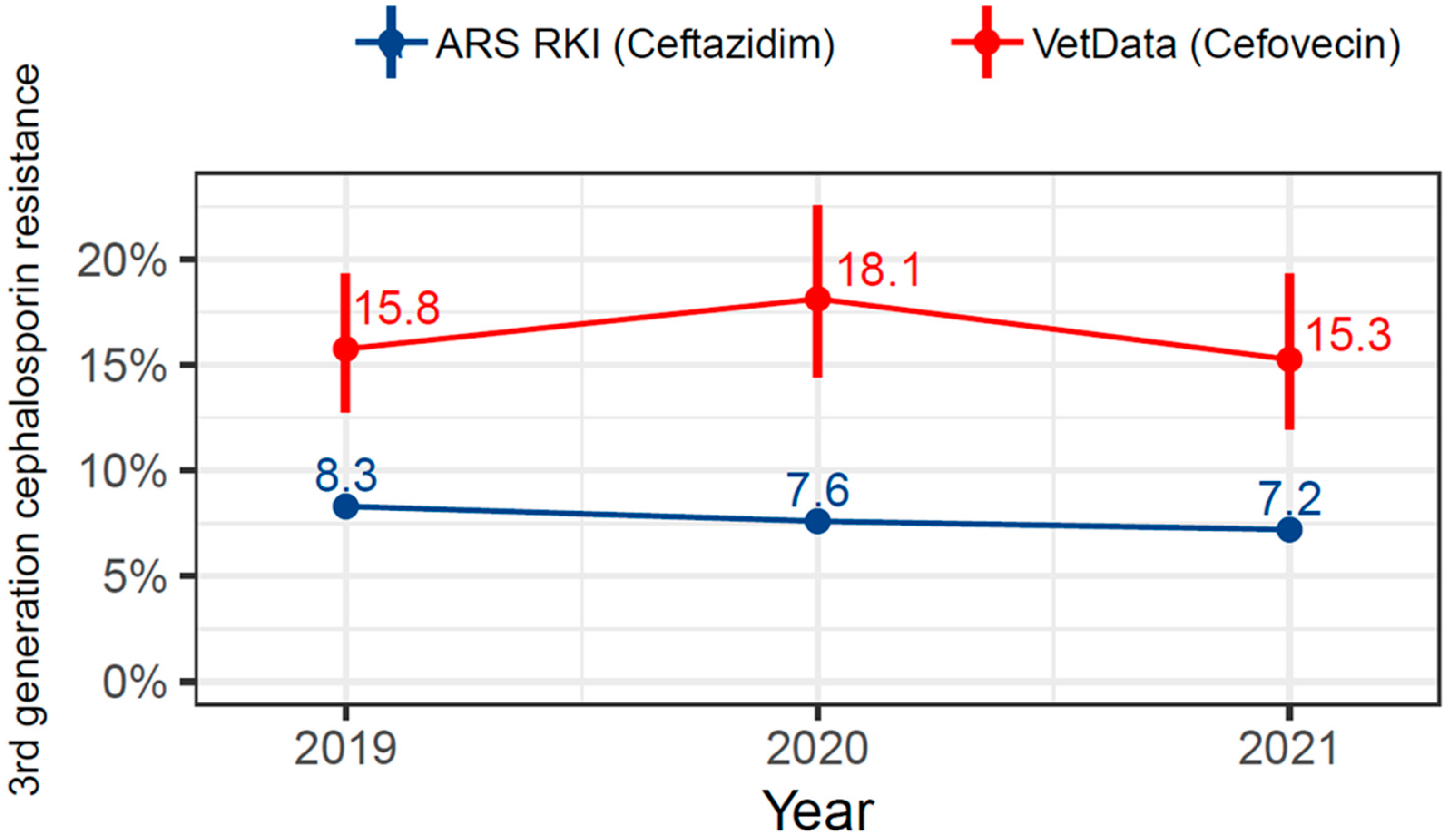
Figure 4 presents a comparative analysis between data sourced from the Antimicrobial Resistance Surveillance (ARS) database and our own dataset. Specifically, it contrasts the resistance proportions of K. pneumoniae isolates from human medicine to ceftazidime with the resistance proportions of our K. pneumoniae isolates to cefovecin. While the resistance proportion in K. pneumoniae isolated from companion animals was 15.8% in 2019, then rose slightly to 18.1% before falling again to 15.3%, the ARS showed a downward trend over the three years (2019—8.3%; 2020—7.6%; 2021—7.2%) [21].
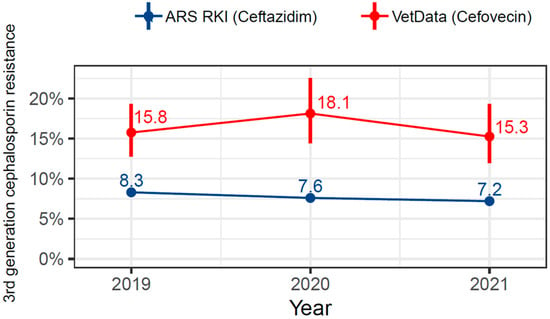
Figure 4.
Comparison of resistance proportion in K. pneumoniae regarding ceftazidime (ARS RKI) and cefovecin from our veterinary data.
4. Discussion
This study was conducted to gain comprehensive insight into the phenotypic resistance properties of K. pneumoniae in companion animals within Germany, providing a significant amount of data in this field.
Since cefovecin is the only third-generation cephalosporin (3GC) approved for use in dogs and cats in Germany in our study, we have chosen to focus on this cephalosporin. Several studies have demonstrated that the various 3GC typically involve the same resistance mechanisms, predominantly ESBL and AmpC beta-lactamases [11,22,23], so that cefovecin can be regarded as a representative for general 3GC.
K. pneumoniae isolated from feline samples exhibited a notably high resistance proportion in 2019, followed by a substantial decline over the subsequent two years (2019—36.0%; 2020—26.0%; 2021—16.0%). This significant reduction in resistance proportions during the period 2019–2021 may be linked to the TÄHAV amendment in 2018 [24]. This legislative update introduced stringent restrictions regarding antimicrobial susceptibility testing for third- and fourth-generation cephalosporins, as well as for fluoroquinolones.
Supporting this hypothesis, Moerer et al. conducted a survey revealing a notable shift in antibiotic usage practices. Participants expressed intentions to adopt a more prudent approach towards antibiotics, emphasizing increased antimicrobial susceptibility testing and reduced reliance on the highest priority critically important antimicrobials [24]. An influence of the COVID-19 pandemic on resistance proportions is also possible. Quarantine regulations, changes in veterinary practice structures, and the increase in telemedicine could have resulted in fewer patients and therefore also fewer antibiotic prescriptions and antimicrobial susceptibility testing. Conversely, the surge in pet ownership during the pandemic might have increased the number of veterinary patients, potentially leading to more antibiotic prescriptions and antimicrobial susceptibility testing in veterinary practices [25].
The resistance levels among canine K. pneumoniae isolates displayed a consistent trend with a marginal increase to 17% in 2020, followed by a slight decline to 15% in 2021. One factor contributing to the higher resistance proportions observed in isolates from cats compared to isolates from dogs may be due to the more frequent use of cefovecin in cats [26].
According to Araújo et al., resistance proportions to 3GCs (cefoperazone, cefotaxime, and cefpodoxime) in isolates from clinically ill cats and dogs (n = 255) in Portugal ranged from 38 to 60% over the study period from 2020 to 2022 [22]. This finding aligns with the cefovecin resistance observed in our feline isolates in 2019 but demonstrates a notably higher resistance compared to the remaining data in our study. Furthermore, their investigation identified ESBL resistance genes (blaTEM, blaSHV, and blaCTX-M), with alarming 50% of the Klebsiella isolates demonstrating multidrug resistance [22].
Similarly, a study from South Korea reported elevated resistance proportions exceeding 50% for 3GCs (cefpodoxime, ceftriaxone, cefotaxime, and ceftazidime) also in isolates acquired from clinically ill dogs and cats (n = 366) [27]. A Japanese study conducted between 2003 and 2015, involving 103 Klebsiella spp. isolates from clinical cases in dogs and cats, reported a 3GC (cefotaxime, CTX) resistance proportion of 34% [23]. All studies adhered to CLSI guidelines for MIC evaluation and included samples from various organ systems. Notably, information on pretreatment was generally absent, except in Lee et al., where subjects received no antibiotic pretreatment. The higher resistance proportions observed in these studies may be attributable to various factors, including different practices regarding antibiotic use, the response of public infrastructure to increased resistance rates, local legislation, and other regional specifics [28].
Concerning the different organ systems, among canine K. pneumoniae isolates, resistance proportions ranged from 0% to 25%, while none of the isolates from the reproductive tract showed any resistance to cefovecin. Approximately 25% of feline K. pneumoniae isolates from wound swabs, skin/soft tissues, and the respiratory tract were resistant against cefovecin, while K. pneumoniae isolates from urinary tract infections showed a significant resistance proportion of 70%, partly aligning with Marques et al., who found a 60% cefovecin resistance proportion in companion animal isolates (n = 25) from urinary tract infections in both humans and animals [29]. ESBL blaCTX-M-15 was most frequently detected in over 80% of the isolates. The most common genotype was blaTEM/blaOXA-1/blaCTX-M-15 (56.2%). In addition, 80% of companion animal K. pneumoniae were multidrug resistant (MDR) and resistant to more than five antimicrobials [29]. Another study from Spain unveiled notably high resistance proportions in K. pneumoniae isolates from urinary tract infections from dogs (n = 3270) and cats (n = 1673) [30]. A total of 70 K. pneumoniae isolates from dogs and 20 from cats were identified. The canine and feline cefovecin resistance proportion was 40% and 70%, respectively, which also corresponds to our results. These studies indicate that feline K. pneumoniae isolates from the urinary tract are particularly resistant to 3GC.
Furthermore, we compared the resistance proportions against CHL, DOX, ENR, GEN, NIT, and SXT in all K. pneumoniae isolates with subgroups of cefovecin-sensitive K. pneumoniae isolates and cefovecin-resistant K. pneumoniae isolates. As expected, the resistance proportions among the 3GCR K. pneumoniae isolates were substantially higher than in 3GC susceptible isolates. This is consistent with our findings on 3GC E. coli (not yet published) and methicillin-resistant Staphylococcus aureus (MRSA) in the same dataset [31]. This seems to be due to the fact that different resistance genes are encoded on the same plasmids. For example, not only resistance genes that mediate 3GCR are transmitted, but also those against fluoroquinolones, aminoglycosides, tetracyclines, and others [32].
Harada et al. conducted an analysis on 103 isolates of Klebsiella spp. (89 K. pneumoniae) obtained from animal clinics in Japan [23]. They performed antimicrobial susceptibility testing, yielding the following results: CTX 34.0%, ENR 37.9%, GEN 31.1%, CHL 28.2%, and SXT 35.0%. When comparing these results to our evaluation of all K. pneumoniae isolates, the resistance proportions were significantly higher than in our data. The most frequently detected ESBL was blaCTX-M-15, followed by blaCTX-M-14 and blaCTX-M-55 [23]. A Chinese study examining K. pneumoniae (n = 35) from clinically diseased dogs and cats reported even higher resistance proportions, with 62.9% for cefotaxime (3GC), 60.0% for enrofloxacin (ENR), 62.9% for gentamicin (GEN), 65.7% for doxycycline (DOX), and 77.1% for trimethoprim-sulfamethoxazole (SXT) [33]. In this case, the reasons for higher levels of resistance appear to be multicausal too. There are links to antibiotic use, regulatory requirements, or regional differences [28].
The French active monitoring (Resapath resistance report from Anses) showed a 30% resistance proportion to 3GC (ceftiofur) in isolates from dogs [14]. Unfortunately, the current GERM-Vet resistance report—an active monitoring program conducted in Germany by the Federal Institute for Consumer Protection and Food Safety—does not include data on K. pneumoniae from dogs and cats [9].
The K. pneumoniae resistance proportions in the ARS of 7.7% from human medicine to ceftazidime, which includes outpatient data, are in contrast with the resistance proportion of 16.4% of our isolates to cefovecin [21]. The K. pneumoniae isolates in both datasets showed a slight downward trend over the course of 2019–2021. The resistance data in the ARS originate from participating routine laboratories. They come from all regions of Germany and, like our samples, are from different material groups. Depending on the participating laboratory, they have been evaluated according to CLSI or EUCAST, which has to be considered in this context.
Our data did not include information on genetic analysis or virulence testing, and we did not receive information whether antibiotic pre-treatment had occurred. Furthermore, in samples that contained more bacterial species than K. pneumoniae, it remains unclear whether K. pneumoniae is the causative pathogen of the disease. Nevertheless, we believe that the publication of these data is valid as it is the largest dataset on K. pneumoniae in dogs and cats in Germany to date and provides valuable information on its resistance proportions. As one of the ESKAPE pathogens—an acronym comprising six highly virulent and antibiotic-resistant bacterial pathogens—K. pneumoniae is also of great importance in human medicine, and the transfer of resistance genes from animals to humans and vice versa cannot be excluded [29,34,35,36,37,38]. This makes it a critical issue in the context of One Health. Thus, with these data, we aim to provide a comprehensive overview of the current resistance situation in K. pneumoniae and encourage the use of data from commercial laboratories alongside national monitoring approaches. Furthermore, by strengthening our monitoring efforts and data sharing, we can better address the evolving challenges posed by antibiotic-resistant pathogens.
5. Conclusions
Antimicrobial resistance is a major threat to our society, and K. pneumoniae plays an important role in both human and veterinary medicine. Its resilience and ability to cause severe and even fatal infections in humans and animals make it one of the most dangerous bacterial pathogens. We have shown that K. pneumoniae can exhibit high rates of resistance to common antimicrobial agents. Routine laboratory data are an ideal source of such data for passive monitoring as they provide large amounts of data and are cost-effective. They can therefore greatly support active surveillance approaches such as the German monitoring system GERM-Vet, although these active surveillance initiatives remain essential as they include both phenotypic and genotypic identification of resistance. However, their disadvantage is the often small amount of data. By integrating passive surveillance, we can continuously collect and analyze data from clinical samples and gain real-time insights into emerging resistance trends. This method also allows for broader geographical coverage and the inclusion of a larger number of isolates, increasing the representativeness of the data. Our strategy therefore aims to close this knowledge gap by using passive monitoring to provide important resistance data.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/microbiolres15030108/s1. The dataset used for our analysis is provided as a CSV file (Supplementary Materials S1) in the Supplementary Materials.
Author Contributions
Conceptualization, S.K.F. and R.M.; methodology, S.K.F., B.K. and R.M.; validation, S.K.F., L.F., A.L.-B. and R.M.; formal analysis, S.K.F. and R.M.; investigation, B.K.; resources, B.K.; data curation, B.K., S.K.F. and L.F.; writing—original draft preparation, S.K.F.; writing—review and editing, L.F., A.L.-B., W.B., R.M. and B.K.; visualization, S.K.F. and R.M.; supervision, R.M. and W.B.; project administration, R.M. and W.B.; funding acquisition, R.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the German Federal Ministry of Food and Agriculture (BMEL) following a decision by the Parliament of the Federal Republic of Germany, with the grant provided by the Federal Office for Agriculture and Food (BLE; grant number 2820HS002). The publication of this article was funded by Freie Universität Berlin.
Institutional Review Board Statement
This study received approval from the Central Ethics Committee of Freie Universität Berlin with the assigned Approval Number 2021-018.
Informed Consent Statement
Patient consent was not required as the human data was not newly collected; instead, the human patient data was sourced from the ARS database. This data has already been published and was not collected by us.
Data Availability Statement
The data of this analysis are provided in Supplementary Materials. Included are ID, bacterium, species, year, sample type, full name, and AST classification of the analyzed antibiotics (FOV, GEN, ENR, DOX, CHL, SXT, and NIT).
Acknowledgments
We would like to thank Alexander Bartel for valuable assistance with data analysis. We would also like to thank Laborgesellschaft Laboklin GmbH & Co KG, Bad Kissingen, Germany, especially Marianne Schneider, for providing these data and for her support in the data analysis.
Conflicts of Interest
The author, Babette Klein, is an employee of Laboklin, which provided the data for our study. Laboklin did not participate in the analysis or interpretation, nor did they fund the publication of this work, but we acknowledge this potential conflict of interest.
References
- European Centre for Disease Prevention and Control; Merk, H.; Diaz Högberg, L.; Plachouras, D.; Suetens, C.; Monet, D.L. Assessing the Health Burden of Infections with Antibiotic-Resistant Bacteria in the EU/EEA, 2016–2020; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2022. [Google Scholar] [CrossRef]
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Read, A.F.; Woods, R.J. Antibiotic resistance management. Evol. Med. Public Health 2014, 2014, 147. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- European Commission. A European One Health Action Plan against Antimicrobial Resistance (AMR); European Commission: Brussels, Belgium, 2017. [Google Scholar]
- European Parliament. Verordnung (EU) 2019/des Europäischen Parlaments und des Rates vom 11. Dezember 2018 über Tierarzneimittel und zur Aufhebung der Richtlinie 2001/82/EG; European Parliament: Strasbourg, France, 2018. [Google Scholar]
- Bundesministerium für Gesundheit. DART 2030—Deutsche Antibiotika-Resistenzstrategie. Available online: www.bundesgesundheitsministerium.de (accessed on 19 November 2023).
- Bundestag; Act on Veterinary Medicinal Products and on Implementing the Provisions of Union Law Concerning Veterinary Medicinal Products (Veterinary Medicinal Products Act—TAMG). Available online: https://www.bmel.de/SharedDocs/Downloads/DE/_Tiere/Tiergesundheit/Tierarzneimittel/Tierarzneimittelgesetz-EN.pdf?__blob=publicationFile&v=6 (accessed on 20 November 2023).
- Bundesamt für Verbraucherschutz und Lebensmittelsicherheit; BVL-Report. 17.6 Bericht zur Resistenzmonitoringstudie 2021. Available online: https://www.bvl.bund.de/SharedDocs/Berichte/07_Resistenzmonitoringstudie/Bericht_Resistenzmonitoring_2021.pdf?__blob=publicationFile&v=2 (accessed on 13 November 2023).
- Wang, G.; Zhao, G.; Chao, X.; Xie, L.; Wang, H. The Characteristic of Virulence, Biofilm and Antibiotic Resistance of Klebsiella pneumoniae. Int. J. Environ. Res. Public Health 2020, 17, 6278. [Google Scholar] [CrossRef]
- Navon-Venezia, S.; Kondratyeva, K.; Carattoli, A. Klebsiella pneumoniae: A major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol. Rev. 2017, 41, 252–275. [Google Scholar] [CrossRef]
- Ribeiro, M.G.; de Morais, A.B.C.; Alves, A.C.; Bolaños, C.A.D.; de Paula, C.L.; Portilho, F.V.R.; de Nardi Júnior, G.; Lara, G.H.B.; de Souza Araújo Martins, L.; Moraes, L.S.; et al. Klebsiella-induced infections in domestic species: A case-series study in 697 animals (1997–2019). Braz. J. Microbiol. 2022, 53, 455–464. [Google Scholar] [CrossRef]
- Choby, J.E.; Howard-Anderson, J.; Weiss, D.S. Hypervirulent Klebsiella pneumoniae—Clinical and molecular perspectives. J. Intern. Med. 2020, 287, 283–300. [Google Scholar] [CrossRef]
- Anses 2023. Resapath: French Surveillance Network for Antimicrobial Resistance in Bacteria from Diseased Animals. Available online: https://www.anses.fr/en/system/files/LABO-Ra-Resapath2022EN.pdf (accessed on 20 March 2024).
- Bundestierärztekammer, e.V. Statistik 2021: Tierärzteschaft in der Bundesrepublik Deutschland. Dtsch. Tierärztebl. 2022, 70, 762–772. [Google Scholar]
- Schwarz, S.; Mensing, N.; Hörmann, F.; Schneider, M.; Baumgärtner, W. Polyarthritis Caused by Acinetobacter kookii in a Rothschild’s Giraffe Calf (Giraffa camelopardalis rothschildi). J. Comp. Pathol. 2020, 178, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Clinical & Laboratory Standards Institute. M100Ed33|Performance Standards for Antimicrobial Susceptibility Testing, 33rd ed.; Clinical & Laboratory Standards Institute: Berwyn, PA, USA, 2024; Available online: https://clsi.org/standards/products/microbiology/documents/m100/ (accessed on 24 July 2023).
- CLSI. Clinical and Laboratory Standard Institute: CLSI Guidlines: VET01S ED6. Available online: https://clsi.org/ (accessed on 24 July 2023).
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org/ (accessed on 24 July 2023).
- Berends, M.S.; Luz, C.F.; Friedrich, A.W.; Sinha, B.N.M.; Albers, C.J.; Glasner, C. AMR: An R Package for Working with Antimicrobial Resistance Data. J. Stat. Soft. 2022, 104, 1–31. [Google Scholar] [CrossRef]
- Robert-Koch-Institut. ARS—Antibiotika-Resistenz-Surveillance. Available online: https://ars.rki.de/ (accessed on 3 April 2024).
- Araújo, D.; Castro, J.; Matos, F.; Oliveira, R.; Ramos, C.; Almeida, C.; Silva, S. Exploring the prevalence and antibiotic resistance profile of Klebsiella pneumoniae and Klebsiella oxytoca isolated from clinically ill companion animals from North of Portugal. Res. Vet. Sci. 2023, 159, 183–188. [Google Scholar] [CrossRef]
- Harada, K.; Shimizu, T.; Mukai, Y.; Kuwajima, K.; Sato, T.; Usui, M.; Tamura, Y.; Kimura, Y.; Miyamoto, T.; Tsuyuki, Y.; et al. Phenotypic and Molecular Characterization of Antimicrobial Resistance in Klebsiella spp. Isolates from Companion Animals in Japan: Clonal Dissemination of Multidrug-Resistant Extended-Spectrum β-Lactamase-Producing Klebsiella pneumoniae. Front. Microbiol. 2016, 7, 1021. [Google Scholar] [CrossRef]
- Moerer, M.; Merle, R.; Bäumer, W. A Cross-Sectional Study of Veterinarians in Germany on the Impact of the TÄHAV Amendment 2018 on Antimicrobial Use and Development of Antimicrobial Resistance in Dogs and Cats. Antibiotics 2022, 11, 484. [Google Scholar] [CrossRef] [PubMed]
- Schlemmer, A. All Creatures Great and Small: The Impact of the COVID-19 Pandemic on Veterinary Medicine. Available online: https://cedar.wwu.edu/wwu_honors/580 (accessed on 7 August 2024).
- Hardefeldt, L.; Hur, B.; Verspoor, K.; Baldwin, T.; Bailey, K.E.; Scarborough, R.; Richards, S.; Billman-Jacobe, H.; Browning, G.F.; Gilkerson, J. Use of cefovecin in dogs and cats attending first-opinion veterinary practices in Australia. Vet. Rec. 2020, 187, e95. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Oh, J.Y.; Sum, S.; Park, H.M. Prevalence and antimicrobial resistance of Klebsiella species isolated from clinically ill companion animals. J. Vet. Sci. 2021, 22, e17. [Google Scholar] [CrossRef]
- Kang, C.-I.; Song, J.-H. Antimicrobial resistance in Asia: Current epidemiology and clinical implications. Infect. Chemother. 2013, 45, 22–31. [Google Scholar] [CrossRef]
- Marques, C.; Menezes, J.; Belas, A.; Aboim, C.; Cavaco-Silva, P.; Trigueiro, G.; Telo Gama, L.; Pomba, C. Klebsiella pneumoniae causing urinary tract infections in companion animals and humans: Population structure, antimicrobial resistance and virulence genes. J. Antimicrob. Chemother. 2019, 74, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Darwich, L.; Seminati, C.; Burballa, A.; Nieto, A.; Durán, I.; Tarradas, N.; Molina-López, R.A. Antimicrobial susceptibility of bacterial isolates from urinary tract infections in companion animals in Spain. Vet. Rec. 2021, 188, e60. [Google Scholar] [CrossRef]
- Feuer, L.; Frenzer, S.K.; Merle, R.; Leistner, R.; Wolfgang, B.; Bethe, A.; Lübke-Becker, A.; Klein, B.; Bartel, A. Prevalence of MRSA in canine and feline clinical samples from one third of veterinary practices in Germany from 2019–2021. J. Antimicrob. Chemother. 2024, 13, dkae225. [Google Scholar] [CrossRef]
- Urban-Chmiel, R.; Marek, A.; Stępień-Pyśniak, D.; Wieczorek, K.; Dec, M.; Nowaczek, A.; Osek, J. Antibiotic Resistance in Bacteria—A Review. Antibiotics 2022, 11, 1079. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, L.; Dai, H.; Zhang, H.; Song, Y.; An, Q.; Wang, J.; Xia, Z. Multidrug-Resistant Klebsiella pneumoniae Complex From Clinical Dogs and Cats in China: Molecular Characteristics, Phylogroups, and Hypervirulence-Associated Determinants. Front. Vet. Sci. 2022, 9, 816415. [Google Scholar] [CrossRef]
- Marques, C.; Belas, A.; Aboim, C.; Cavaco-Silva, P.; Trigueiro, G.; Gama, L.T.; Pomba, C. Evidence of Sharing of Klebsiella pneumoniae Strains between Healthy Companion Animals and Cohabiting Humans. J. Clin. Microbiol. 2019, 57, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.M.; Fernandes, M.R.; Sellera, F.P.; Cerdeira, L.; Medeiros, L.K.G.; Garino, F.; Azevedo, S.S.; Lincopan, N. Multidrug-resistant CTX-M-15-producing Klebsiella pneumoniae ST231 associated with infection and persistent colonization of dog. Diagn. Microbiol. Infect. Dis. 2018, 92, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Maeyama, Y.; Taniguchi, Y.; Hayashi, W.; Ohsaki, Y.; Osaka, S.; Koide, S.; Tamai, K.; Nagano, Y.; Arakawa, Y.; Nagano, N. Prevalence of ESBL/AmpC genes and specific clones among the third-generation cephalosporin-resistant Enterobacteriaceae from canine and feline clinical specimens in Japan. Vet. Microbiol. 2018, 216, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Santajit, S.; Indrawattana, N. Mechanisms of Antimicrobial Resistance in ESKAPE Pathogens. BioMed Res. Int. 2016, 2016, 2475067. [Google Scholar] [CrossRef]
- Chen, C.-M.; Tang, H.-L.; Chiou, C.-S.; Tung, K.-C.; Lu, M.-C.; Lai, Y.-C. Colonization dynamics of Klebsiella pneumoniae in the pet animals and human owners in a single household. Vet. Microbiol. 2021, 256, 109050. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).